ABSTRACT
OBJECTIVE
To describe the prevalence of common mental disorders in Brazilian adolescent students, according to geographical macro-regions, school type, sex, and age.
METHODS
We evaluated 74,589 adolescents who participated in the Cardiovascular Risk Study in Adolescents (ERICA), a cross-sectional, national, school-based study conducted in 2013-2014 in cities with more than 100,000 inhabitants. A self-administered questionnaire and an electronic data collector were employed. The presence of common mental disorders was assessed using the General Health Questionnaire (GHQ-12). We estimated prevalence and 95% confidence intervals of common mental disorders by sex, age, and school type, in Brazil and in the macro-regions, considering the sample design.
RESULTS
The prevalence of common mental disorders was of 30.0% (95%CI 29.2-30.8), being higher among girls (38.4%; 95%CI 37.1-39.7) when compared to boys (21.6%; 95%CI 20.5-22.8), and among adolescents who were from 15 to 17 years old (33.6%; 95%CI 32.2-35.0) compared to those aged between 12 and 14 years (26.7%; 95%CI 25.8-27.6). The prevalence of common mental disorders increased with age for both sexes, always higher in girls (ranging from 28.1% at 12 years to 44.1% at 17 years) than in boys (ranging from 18.5% at 12 years to 27.7% at 17 years). We did not observe any significant difference by macro-region or school type. Stratified analyses showed higher prevalence of common mental disorders among girls aged from 15 to 17 years of private schools in the North region (53.1; 95%CI 46.8-59.4).
CONCLUSIONS
The high prevalence of common mental disorders among adolescents and the fact that the symptoms are often vague mean these disorders are not so easily identified by school administrators or even by health services. The results of this study can help the proposition of more specific prevention and control measures, focused on highest risk subgroups.
Keywords: Adolescent; Mental Disorders, epidemiology; Prevalence; Mental Health; Cross-Sectional Studies
INTRODUCTION
In recent decades, the patterns of physical and mental illness in children and adolescents have changed considerably. The prevalence of emotional and conduct problems is around 10.0%-20.0%, representing a significant burden of disease, which causes loss in school life and in family and social relationships for these children and adolescents 1 . In addition, mental health problems are highly persistent, causing a significant portion of these individuals to have some impairment in adult life 21 .
A study on the global burden of disease in adolescents and young people aged between 10 and 24 years showed that, worldwide, the three leading causes of years of life lost due to disability in this age group are, respectively, neuropsychiatric disorders (45.0%), unintentional injuries (12.0%) and infectious and parasitic diseases (10.0%) 9 .
In Brazil, a population-based study (Sao Paulo Megacity Mental Health Study) 29 , showed that the average age for the onset of psychiatric disorders is earlier for anxiety disorders (13 years old) and impulse control disorders (14 years old), when compared with substance abuse disorders (24 years old) and mood disorders (36 years old). Another population-based study, conducted in four cities in four regions of Brazil (Southeast, Midwest, Northeast and North) 22 , assessed the prevalence of psychiatric disorders in 1,676 children and adolescents aged from six to 16 years, who attended elementary school, from the second to the sixth year. The overall prevalence for the presence of at least one psychiatric disorder was 13.1%, similar to values found in other population-based studies around the world 3 , 19 .
About 90.0% of mental disorders are non-psychotic disorders 30 . Such disorders due to their high prevalence in the general population (20.0%-30.0%), are usually called common mental disorders (CMD), mainly characterized by the presence of symptoms of depression and anxiety, and various nonspecific and somatic complaints 8 . CMD affect individuals in different age groups and, when present in children and adolescents, may be early and less specific manifestations of more serious mental disorders, also impairing the social relationships and school performance of this population 21 . Early identification of CMD and its main risk factors can contribute to specific interventions and a better prognosis.
In Brazil, some studies evaluated the prevalence and risk factors for CMD in the adult population 13 - 15 , 25 . However, the literature on CMD in adolescents is scarce. We have only identified one cross-sectional, population-based study, conducted among adolescents aged from 15 to 18 years from Pelotas, RS, Southern Brazil, whose CMD prevalence was of 28.8% and the main associated factors were low maternal education, smoking, sedentary behavior, and body image dissatisfaction 23 .
This study aimed to describe the prevalence of common mental disorders in the population of Brazilian adolescent students, according to region, school type, and sociodemographic characteristics.
METHODS
This study is part of the Estudo de Riscos Cardiovasculares em Adolescentes (ERICA – Study of Cardiovascular Risk in Adolescents), a cross-sectional, national, school-based study, conducted in 2013-2014, with the objective of estimating the prevalence of metabolic syndrome, diabetes mellitus, obesity, cardiovascular risk factors, and insulin and inflammatory resistance markers in adolescents aged from 12 to 17 years, who attend schools in cities municipalities with over 100,000 inhabitants.
We assessed 74,589 adolescents in 1,247 schools of 124 Brazilian cities. The research population was stratified into 32 strata comprised of 27 state capitals and five sets of cities with more than 100,000 inhabitants in each geographical macro-region of the Country. For each geographic stratum, we selected schools with probability proportional to size and inversely proportional to the distance to the capital. The sample is representative for the group of cities with more than 100,000 inhabitants at the national, regional and state capitals level. More details on the sampling design can be found in a previous publication 28 . We excluded from the analysis, for not being considered eligible, adolescents outside the age group of 12-17 years, pregnant adolescents and those with physical or mental impairment, temporary or permanent. We have previously described the study protocol 2 .
Data were collected using a self-administered questionnaire, which was entered into the electronic data collector PDA (personal digital assistant). The questionnaire consisted of about 100 questions divided into 11 blocks: sociodemographic aspects, occupational activities, physical activity, eating habits, smoking, alcohol use, reproductive health, oral health, sleep duration, physical morbidity (self-reported) and mental health.
In this study, we analyzed the following characteristics: sex, age, school type (public or private), geographic macro-region (North, Northeast, Midwest, Southeast and South) and presence of CMD. The age variable was used categorically, considering two groups: from 12 to 14 years and from 15 to 17 years.
For the CMD evaluation, we used the General Health Questionnaire, 12-item version (GHQ-12) 6 . The scores of the individual items were coded as “missing” or “present” (0 or 1, respectively) and then summed up; adolescents with a score of three or more were classified as cases of CMD 17 . The Brazilian version, used in this study, was submitted to a validation study, using a structured psychiatric interview as the gold standard and the same criterion of three or more to establish a case of CMD. The results showed a sensitivity of 85.0%, a specificity of 79.0%, and area under the ROC (Receiver Operating Characteristics) curve of 0.87 7 .
We calculated the prevalences and 95% confidence intervals (95%CI) of CMD according to sex, age, and school type, considering the national, regional and capital levels.
The analysis was performed using the Stata 14.0 statistical package. We adjusted the distributions of the features according to the sample design, using statistical routines for complex samples. The ERICA sample is a complex one 26 , since it employs stratification and clustering in its selection stages. We calculated the sample weights using the product of the inverse of inclusion probabilities at each stage of the sample, and calibrated it considering the projection of the number of adolescents enrolled in schools located in geographic areas considered on December 31, 2013. We used a post-stratification estimator, which modifies the natural weight of the design by a calibration factor that is the ratio between the total population and the total estimated by the natural weight of the design for the post-stratum or estimated domain considered.
All participating students signed an assent form and brought the informed consent form signed by their legal guardians (when required by the local Research Ethics Committee). The study was approved by the Research Ethics Committee of the institution of the Study Coordination Center (IESC/UFRJ – Process 45/2008) and by each Brazilian state involved.
RESULTS
Of the 102,327 eligible adolescents registered in the selected schools, 74,589 (72.9%) participated in the study.
Nearly a third of adolescents from cities with more than 100,000 inhabitants in Brazil presented CMD. The prevalence was higher in the female sex and in older adolescents. The prevalence did not differ by macro-region and school type (Table 1).
Table 1. Sample size, population and prevalence of common mental disorders in cities with more than 100,000 inhabitants, according to sex, age, school type and macro-region. ERICA, Brazil, 2013-2014.
| Variable | Sample | Estimated population | Prevalence (%) | 95%CI |
|---|---|---|---|---|
| Sex | ||||
| Female | 41,225 | 5,052,137 | 38.4 | 37.1-39.7 |
| Male | 33,364 | 5,095,563 | 21.6 | 20.5-22.8 |
| Age group | ||||
| 12-14 | 34,141 | 5,348,201 | 26.7 | 25.8-27.6 |
| 15-17 | 40,448 | 4,799,499 | 33.6 | 32.2-35.0 |
| School type | ||||
| Public | 58,707 | 8,382,253 | 30.0 | 29.1-31.0 |
| Private | 15,882 | 1,765,447 | 29.8 | 28.7-30.8 |
| Macro-region | ||||
| North | 15,073 | 855,362 | 31.3 | 30.0-32.5 |
| Northeast | 23,167 | 2,165,033 | 30.2 | 28.7-31.8 |
| Midwest | 9,727 | 778,010 | 31.7 | 30.4-33.0 |
| Southeast | 17,080 | 5,153,506 | 29.3 | 28.0-30.7 |
| South | 9,542 | 1,195,789 | 30.4 | 28.6-32.2 |
| Brazil | 74,589 | 10,147,700 | 30.0 | 29.2-30.8 |
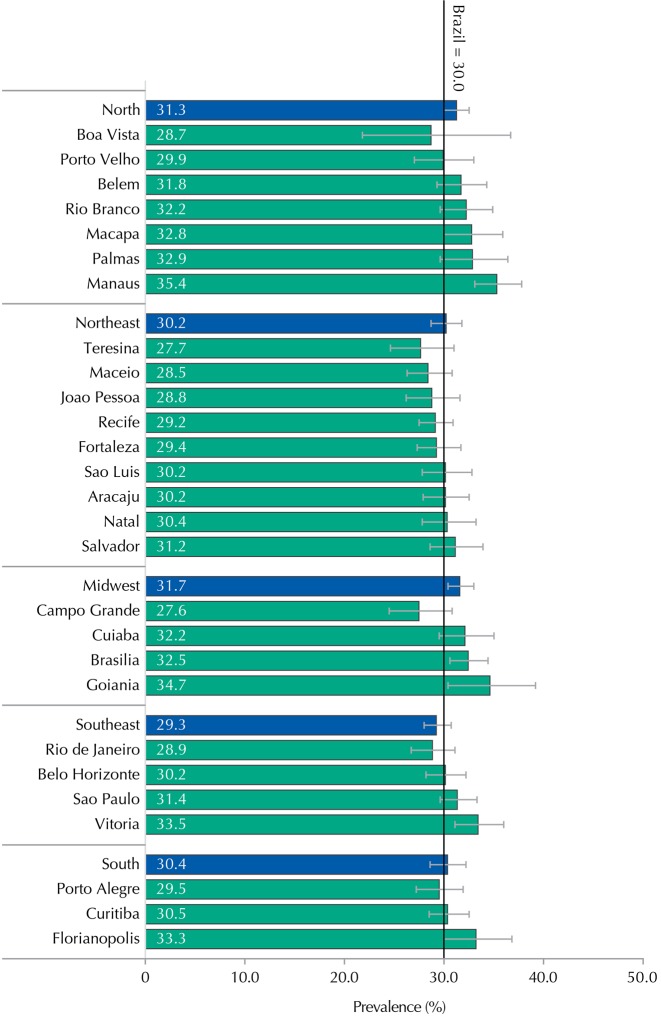
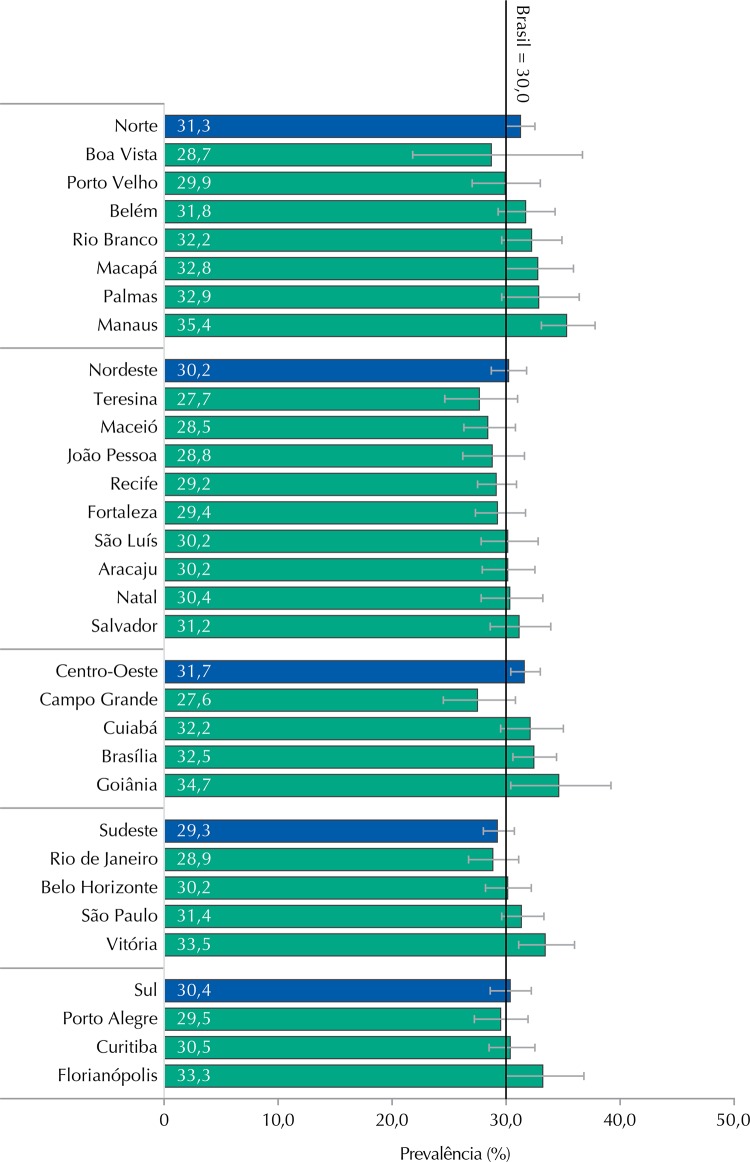
Regarding the cities, we also found no significant differences, with the highest prevalence of CMD being observed in Manaus, AM, Northern Brazil, and the lowest in Campo Grande, MS, Midwestern Brazil (Figure 1).
Figure 1. Prevalence and 95%CI of common mental health disorders in the cities with more than 100,000 inhabitants per macro-region and capitals. ERICA, Brazil, 2013-2014.
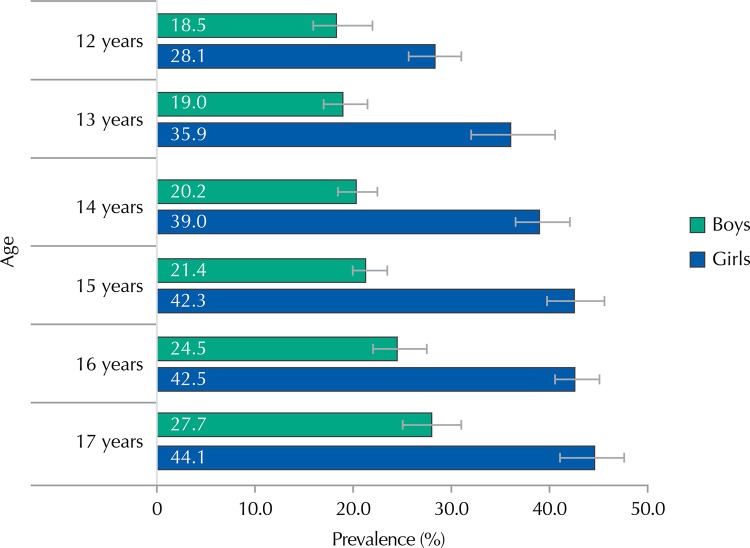
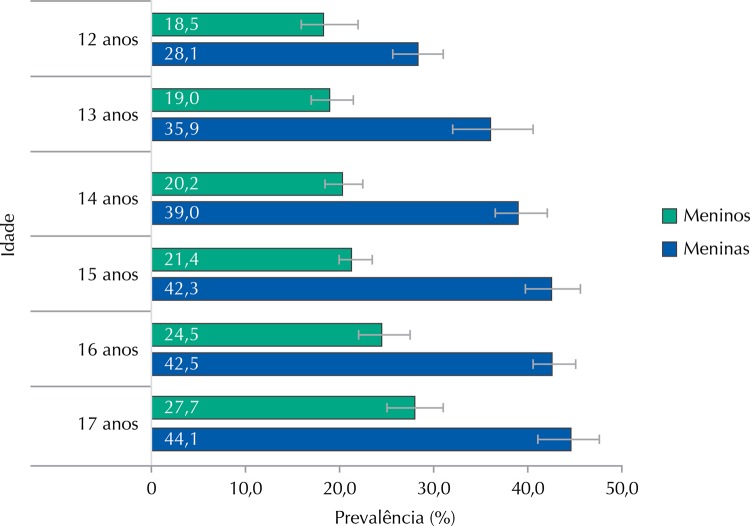
Prevalence of CMD among girls was always higher than among boys, for all age groups (Figure 2). We also observed a trend of increasing CMD prevalence as age increased.
Figure 2. Prevalence (%) and 95%CI of common mental disorders in the cities with more than 100,000 inhabitants by sex and age. ERICA, Brazil, 2013-2014.
In the analysis stratified by sex, age, school type and macro-region, we observed that the highest prevalence of CMD was among girls, aged from 15 to 17 years, and from private schools in the North region. The lowest prevalence was among boys, aged from 12 to14 years, from private schools in the Southeast region (Table 2).
Table 2. Prevalence (%) and 95%CI of common mental disorders in adolescents by macro-region, according to the school type, sex and age group. ERICA, Brazil, 2013-2014.
| Variable | Brazil | Macro-region | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| North | Northeast | Midwest | South | Southeast | ||||||||
|
|
|
|
|
|
|
|||||||
| % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | |
| Public school | ||||||||||||
| Girls | ||||||||||||
| 12-14 years | 33.8 | 31.9-35.9 | 35.0 | 32.2-37.8 | 29.8 | 26.5-33.3 | 35.9 | 33.1-38.9 | 31.8 | 26.8-37.3 | 35.3 | 32.0-38.7 |
| 15-17 years | 42.3 | 40.0-44.6 | 44.9 | 43.1-46.8 | 42.5 | 40.0-45.1 | 44.7 | 42.1-47.4 | 40.7 | 36.4-45.1 | 41.7 | 37.6-46.0 |
| Boys | ||||||||||||
| 12-14 years | 20.0 | 17.9-22.2 | 18.8 | 16.9-20.8 | 23.6 | 16.1-33.1 | 19.3 | 15.5-23.7 | 23.2 | 17.5-29.9 | 18.3 | 16.2-20.6 |
| 15-17 years | 24.0 | 22.4-25.6 | 25.4 | 23.3-27.6 | 24.5 | 21.8-27.4 | 25.8 | 23.5-28.3 | 26.7 | 22.7-31.2 | 22.6 | 20.0-25.3 |
|
| ||||||||||||
| Total | 30.0 | 29.1-31.0 | 30.9 | 29.6-32.3 | 30.4 | 28.4-32.3 | 31.3 | 29.9-32.8 | 30.5 | 28.5-32.5 | 29.4 | 27.8-31.0 |
|
| ||||||||||||
| Private school | ||||||||||||
| Girls | ||||||||||||
| 12-14 years | 36.4 | 33.3-39.5 | 39.1 | 33.0-45.5 | 35.3 | 32.4-38.3 | 38.2 | 34.2-42.4 | 32.8 | 26.5-39.8 | 37.2 | 31.7-43.1 |
| 15-17 years | 46.5 | 42.6-50.5 | 53.1 | 46.8-59.4 | 47.4 | 43.8-50.9 | 44.6 | 39.4-49.9 | 42.1 | 38.0-46.3 | 46.7 | 39.7-53.9 |
| Boys | ||||||||||||
| 12-14 years | 16.3 | 14.6-18.2 | 20.4 | 15.6-26.2 | 18.1 | 15.4-21.2 | 20.0 | 14.3-27.1 | 21.5 | 15.5-29.0 | 13.0 | 11.0-15.4 |
| 15-17 years | 26.0 | 24.0-28.1 | 32.3 | 28.7-36.1 | 27.2 | 24.0-30.8 | 34.1 | 28.7-40.0 | 26.7 | 22.1-31.9 | 23.8 | 21.3-26.5 |
|
| ||||||||||||
| Total | 29.8 | 28.7-30.8 | 35.0 | 31.6-38.6 | 29.7 | 27.9-31.6 | 33.3 | 30.8-36.0 | 29.6 | 26.5-32.8 | 28.8 | 27.2-30.4 |
DISCUSSION
This is the first epidemiological study conducted in Brazil, with representation for the cities with 100,000 inhabitants or more on a national level, which evaluated mental morbidity data in adolescents.
The overall prevalence of these disorders was high, being higher among older girls (15-17 years) in private schools in the North region, followed by those from public schools in the same region. The general prevalences by macro-regions and by school type, however, showed no significant differences.
Although we do not have mental health data of Brazilian adolescents with national representation, the overall prevalence of CMD found in ERICA (30.0%) was similar to that observed in a population-based study conducted among adolescents aged from 15 to 18 years living in Pelotas, a medium-sized city in Southern Brazil (28.8%) 23 . The higher prevalence of CMD in girls (38.4%) when compared to boys (21.6%) found in this study is also consistent with the findings of the Pelotas study, in which the prevalence of CMD among girls was 37.2% and among boys was 19.9%. A Brazilian study, conducted in four cities of four regions of Brazil (North, Northeast, Midwest and Southeast) found an overall prevalence of 13.1% (in the last 12 months) for at least one psychiatric disorder 22 . This prevalence is much lower than the one found in our study and probably reflects some differences between the two studies, namely: 1) the ERICA study used a screening instrument for mental disorders (GHQ-12), while the study by Paula et al. 22 applied a tool for psychiatric disorders diagnosis (Schedule for Affective Disorders and Schizophrenia for School-Age Children – K-SADS-PL); 2) in ERICA, the age group of participants was 12-17 years, while in the study by Paula et al., participants were aged between six and 16 years; and 3) ERICA is a study with national representativeness, conducted among 75,000 students, while in the study by Paula et al., the sample remained restricted to only four cities. In addition, the study by Paula et al. observed a higher prevalence (18.5%) of psychiatric disorders (any disorder) in the city located in the Midwest region. In this study we found differences not really significant in CMD prevalence by macro-regions, with it being slightly higher only in the Midwest and North regions.
Comparisons with international studies are even more difficult, due to differences in methods, in types of disorders and in age groups employed in the studies. However, a review of the results from population-based surveys conducted in different parts of the world shows that, despite the substantial variation in the results, approximately one quarter of adolescents experienced some mental disorder in the previous year and a third during their lifetimes 18 . Studies have also been consistent in pointing higher prevalence of anxiety and mood disorders among girls, while boys have higher rates of behavior and conduct disorders 19 , 20 , 24 ,varying according to income and countries’ development . Conduct disorders, communications disorders, and pervasive developmental disorders are more common in the early stage of childhood, while in adolescence conduct disorders and depression prevail 20 , 24 .
Studies show a higher prevalence of disorders among adolescents living in disadvantaged countries or regions; however, the findings are inconsistent, likely reflecting differences in the used methods. Giel et al. 5 (1981) found a prevalence of mental disorders ranging from 12.0% to 29.0% in children and adolescents aged from five to 15 years in four countries with low or average income (Sudan, Philippines, Colombia and India). A study conducted in Oman, in Arabia, with 5,409 adolescents and young adults of both sexes, aged between 14 and 23 years, found a prevalence of 20.0% for at least one psychiatric diagnosis, according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), and 32.7% for mild mental disorders (any disorder in the last 12 months) 11 . Thabet and Vostanis 27 (1998) reported a 21.0% prevalence of anxiety symptoms and related disorders among children living in the Gaza Strip, comparable to data found by Kashani and Orvaschel 12 (1990) in the population of children and adolescents of USA. In India, a recent meta-analysis on the prevalence of mental disorders in children and adolescents showed that among schoolchildren from five to 15 years, the prevalence of psychiatric disorders was 23.3% 16 . These prevalence rates are lower than those found in this study that used an instrument for CMD assessment and non-psychiatric diagnoses, like the studies mentioned above.
This is the first study that evaluated data of physical and mental health of in adolescent students, with representation for cities with more than 100,000 inhabitants, for Brazil, macro-regions, and state capitals. CMD were evaluated by standardized instrument and validated for the population of children and adolescents 4 , allowing comparisons with national and international studies. However, we should consider that the GHQ-12 is a screening instrument sensitive to recent psychological changes, leading to a greater number of false positives, with transient symptoms of psychological disorders, thus overestimating the prevalence of CMD. In addition, more detailed socioeconomic information was not included in the analysis and it should be considered in future ones.
Mental disorders have emerged as major challenges health services must face. Often, before the formal diagnosis of a psychiatric disorder, it is already possible to find evidence of psychic suffering in adolescents during clinical practice. Therefore, early identification of CMD and its main risk factors can help proposals for preventive and more specific control measures over the entire adolescent development process.
This study, part of a larger study whose main objective is to investigate cardiovascular risk factors in adolescents, included, in addition to mental health, the measurement of a number of factors such as sociodemographic characteristics, lifestyle, referred morbidity and anthropometric and biochemical data (on a subsample). Thus, we expect that the results of this study, which show high prevalence of CMD in children and adolescents, will provide important evidence for future studies that shall evaluate common mechanisms underlying mental disorders and cardiovascular diseases; and, on a longitudinal perspective, shal investigate the role of cardiovascular disease in the occurrence and persistence of mental disorders. Such studies will allow a better understanding of this comorbidity, enabling the development of effective treatments and interventions 10 .
Footnotes
Funding: Brazilian Ministry of Health (Department of Science and Technology), Brazilian Ministry of Science and Technology (Financiadora de Estudos e Projetos [FINEP – Process 01090421]), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq – Process 565037/2010-2 and 405.009/2012-7).
REFERENCES
- 1.Belfer ML. Child and adolescent mental disorders: the magnitude of the problem across the globe. 10.1111/j.1469-7610.2007.01855.xJ Child Psychol Psychiatry. 2008;49(3):226–236. doi: 10.1111/j.1469-7610.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- 2.Bloch KV, Szklo M, Kuschnir MC, Abreu GA, Barufaldi LA, Klein CH, et al. The Study of Cardiovascular Risk in Adolescents – ERICA: rationale, design and sample characteristics of a national survey examining cardiovascular risk factor profile in Brazilian adolescents. 9410.1186/s12889-015-1442-xBMC Public Health. 2015;15(1) doi: 10.1186/s12889-015-1442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. 10.1016/j.chc.2005.06.003Child Adolesc Psychiatr Clin N Am. 2005;14(4):631–648. doi: 10.1016/j.chc.2005.06.003. vii. [DOI] [PubMed] [Google Scholar]
- 4.French DJ, Tait RJ. Measurement invariance in the General Health Questionnaire-12 in young Australian adolescents. 10.1007/s00787-004-0345-7Eur Child Adolesc Psychiatry. 2004;13(1):1–7. doi: 10.1007/s00787-004-0345-7. [DOI] [PubMed] [Google Scholar]
- 5.Giel R, Arango MV, Climent CE, Harding TW, Ibrahim HH, Ladrido-Ignacio L, et al. Childhood mental disorders in primary health care: results of observations in four developing countries: a report from the WHO collaborative Study on Strategies for Extending Mental Health Care. Pediatrics. 1981;68(5):677–683. [PubMed] [Google Scholar]
- 6.Goldberg DP. The detection of psychiatric illness by questionnaire: a technique for the identification and assessment of non-psychotic psychiatric illness. London: Oxford University Press; 1972. [Google Scholar]
- 7.Goldberg DP, Williams P. A user’s guide to the General Health Questionnaire - GHQ. Windsor: Nfer-Nelson; 1988. [Google Scholar]
- 8.Goldberg DP, Huxley PY. Common mental disorders: a bio-social model. London: Tavistock/Routledge; 1992. [Google Scholar]
- 9.Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. 10.1016/S0140-6736(11)60512-6Lancet. 2011;377(9783):2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 10.Grippo AJ, Johnson AK. Stress, depression and cardiovascular dysregulation: a review of neurobiological mechanisms and the integration of research from preclinical disease models. 10.1080/10253890802046281Stress. 2009;12(1):1–21. doi: 10.1080/10253890802046281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaju S, Al-Adawi S, Al-Kharusi H, Morsi M, Al-Riyami A. Prevalence and age-of-onset distributions of DSM IV mental disorders and their severity among school going Omani adolescents and youths: WMH-CIDI findings. 2910.1186/1753-2000-3-29Child Adolesc Psychiatry Ment Health. 2009;3(1) doi: 10.1186/1753-2000-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kashani JH, Orvaschel H. A community study of anxiety in children and adolescents. 10.1176/ajp.147.3.313Am J Psychiatry. 1990;147(3):313–318. doi: 10.1176/ajp.147.3.313. [DOI] [PubMed] [Google Scholar]
- 13.Lopes CS, Faerstein E, Chor D, Werneck GL. Higher risk of common mental disorders after experiencing physical violence in Rio de Janeiro, Brazil: the Pró-Saude Study. 10.1177/0020764007083876Int J Soc Psychiatry. 2008;54(2):112–117. doi: 10.1177/0020764007083876. [DOI] [PubMed] [Google Scholar]
- 14.Lopes CS, Moraes CL, Junger WL, Werneck GL, Ponce de Leon AC, Faerstein E. Direct and indirect exposure to violence and psychological distress among civil servants in Rio de Janeiro, Brazil: a prospective cohort study. 10910.1186/s12888-015-0487-9BMC Psychiatry. 2015;15(1) doi: 10.1186/s12888-015-0487-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ludermir AB, Araújo TV, Valongueiro SA, Lewis G. Common mental disorders in late pregnancy in women who wanted or attempted an abortion. 10.1017/S003329170999184XPsychol Med. 2010;40(9):1467–1473. doi: 10.1017/S003329170999184X. [DOI] [PubMed] [Google Scholar]
- 16.Malhotra S, Patra BN. Prevalence of child and adolescent psychiatric disorders in India: a systematic review and meta-analysis. 2210.1186/1753-2000-8-22Child Adolesc Psychiatry Ment Health. 2014;8(1) doi: 10.1186/1753-2000-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mari JJ, Williams P. A comparison of the validity of two psychiatric screening questionnaires (GHQ-12 and SRQ-20) in Brazil, using Relative Operating Characteristic (ROC) analysis. Psychol Med. 1985;15(3):651–659. doi: 10.1017/s0033291700031500. [DOI] [PubMed] [Google Scholar]
- 18.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. 10.1542/peds.2008-2598Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Navarro-Pardo E, Meléndez Moral JC, Sales Galan A, Sancerni Beitia MD. Desarrollo infantil y adolescente: trastornos mentales más frecuentes en función de la edad y el género. Psicothema. 2012;24(3):377–383. [PubMed] [Google Scholar]
- 21.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. 10.1016/S0140-6736(07)60368-7Lancet. 2007;369(9569):1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 22.Paula CS, Bordin IA, Mari JJ, Velasque L, Rohde LA, Coutinho ES. The mental health care gap among children and adolescents: data from an epidemiological survey from four Brazilian regions. e8824110.1371/journal.pone.0088241PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0088241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pinheiro KAT, Horta BL, Pinheiro RT, Horta LL, Terres NG, Silva RA. Common mental disorders in adolescents: a population based cross-sectional study. 10.1590/S1516-44462006005000040Rev Bras Psiquiatr. 2007;29(3):241–245. doi: 10.1590/s1516-44462006005000040. [DOI] [PubMed] [Google Scholar]
- 24.Ravens-Sieberer U, Wille N, Erhart M, Bettge S, Wittchen HU, Rothenberger A, et al. Prevalence of mental health problems among children and adolescents in Germany: results of the BELLA study within the National Health Interview and Examination Survey. 10.1007/s00787-008-1003-2Eur Child Adolesc Psychiatry. 2008;17(Suppl 1):22–33. doi: 10.1007/s00787-008-1003-2. [DOI] [PubMed] [Google Scholar]
- 25.Rocha SV, Almeida MMG, Araújo TM, Virtuoso JS., Júnior Prevalence of common mental disorders among the residents of urban areas in Feira de Santana, Bahia. 10.1590/S1415-790X2010000400008Rev Bras Epidemiol. 2010;13(4):630–640. doi: 10.1590/s1415-790x2010000400008. [DOI] [PubMed] [Google Scholar]
- 26.Skinner CJ, Holt D, Smith TMF. Analysis of complex surveys. Chichester: John Wiley and Sons; 1989. [Google Scholar]
- 27.Thabet AA, Vostanis P. Social adversities and anxiety disorders in the Gaza Strip. 10.1136/adc.78.5.439Arch Dis Child. 1998;78(5):439–442. doi: 10.1136/adc.78.5.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vasconcellos MTL, Silva PLN, Szklo M, Kuschnir MCC, Klein CH, Abreu GA, et al. Sampling design for the Study of Cardiovascular Risks in Adolescents (ERICA) 10.1590/0102-311X00043214Cad Saude Publica. 2015;31(5):921–930. doi: 10.1590/0102-311X00043214. [DOI] [PubMed] [Google Scholar]
- 29.Viana MC, Andrade LH. Lifetime prevalence, age and gender distribution and age-of-onset of psychiatric disorders in the São Paulo Metropolitan Area, Brazil: results from the São Paulo Megacity Mental Health Survey. 10.1016/j.rbp.2012.03.001Rev Bras Psiquiatr. 2012;34(3):249–260. doi: 10.1016/j.rbp.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization . Towards a common language for functioning disability and health – ICF. Geneva: World Health Organization; 2002. [Google Scholar]