Abstract
Background:
Regional anesthesia has been the choice of preference for elective cesarean sections. This study was designed to determine whether preoperative administration of 6% hetastarch decreases the incidence of hypotension.
Materials and Methods:
This study was conducted on 50 nonlaboring American Society of Anesthesiologists class I and II women undergoing elective cesarean section. Patients were randomly divided into two groups and were preloaded either with 1000 ml Ringer's lactate (RL) or 500 ml of 6% hetastarch 30 min prior to the surgery. Spinal anesthesia was performed with patients in the left lateral position and 2 cc (10 mg) of 0.5% of bupivacaine injected into subarachnoid space. Hemodynamic variables (heart rate, noninvasive blood pressure, and SpO2) were recorded from prior to preloading until the recovery from the subarachnoid blockade.
Results:
Our study showed the incidence of hypotension to be 28% in the hetastarch group and 80% in the RL group. Rescue ephedrine requirements for the treatment of hypotension were significantly less in patients who were preloaded with 6% hetastarch prior to cesarean section. The neonatal outcome, as determined by Apgar scores was good and similar in both groups.
Conclusion:
Hence, we conclude that 6% hydroxyl ethyl starch is more effective than lactated Ringers solution and that its routine use for preloading prior to spinal anesthesia should be considered.
Keywords: Cesarean, preloading, spinal
INTRODUCTION
Cesarean section in an awake patient is undoubtedly a major test of regional anesthesia. Regional anesthesia has been the choice of preference for elective cesarean sections.[1] The operation may be lengthy, profound blockade of many nerves is required, strong visceral stimulation is present, sudden cardiovascular changes are compounded by posture, and fetal well-being may be influenced by several physiologic variable and drugs. Spinal anesthesia is perhaps the most elegant approach to this challenge with one small needle and an almost homeopathic amount of drug, the anesthesiologist can readily provide profound anesthesia and excellent. In the elective cesarean section under spinal anesthesia, hypotension has been reported in 85% of the patients. Maternal hypotension is associated with distressing symptoms such as dizziness, nausea, vomiting and may interfere with the surgical procedure and also can cause fetal bradycardia and acidosis. Hypotension results primarily from sympathetic nervous system blockade, which causes a decrease in the systemic vascular resistance and cardiac output. The systemic hypotension can cause a reduction in the uterine perfusion pressure and decrease in the placental blood flow.
Recent studies have shown that colloids, when used for preloading, are more effective in the prevention of hypotension.[2,3] Hence, we made a sincere effort to compare the efficacy of a crystalloid to that of colloids in reducing the incidence and severity of hypotension following spinal anaesthesia in the elective cesarean section.
MATERIALS AND METHODS
After Institutional Ethics Committee approval, informed and written consent was taken from all the patients. Fifty American Society of Anesthesiologists (ASA) Grades I and II pregnant women scheduled for the elective cesarean section were studied in our institutional hospitals. Patients were randomly assigned to two groups of 25 patients.
Group 1 – Patients received 1 l lactated Ringer's solution (n = 25).
Group 2 – Patients received 500 ml of 6% hetastarch solution (n = 25).
Patients aged <18 years and >40 years, weighing over 100 kg, height <152 cm, with associated diabetes mellitus, pregnancy-induced hypertension, chronic hypertension, heart disease, multiple gestation, breech presentation, systolic blood pressure (SBP) <100 mm Hg and patients who have received any intravenous (IV) fluids prior to surgery. Complete blood count, coagulation profile and blood grouping were done. All patients received 10 mg of injection metoclopramide and injection ranitidine hydrochloride 50 mg IV 30 min before giving the anesthesia. Patients were explained the procedure of spinal anesthesia during the preanesthetic evaluation and informed/consent attained. Once the patient was shifted to OT, IV access was secured with an 18-gauge cannula. Monitors – electrocardiogram, noninvasive blood pressure (BP), and SpO2 probe were to be connected, and baseline heart rate (HR), SBP and diastolic BP and SpO2 were measured. Patients were randomly assigned into two groups and were preloaded either with 1000 ml Ringer's lactate (RL) or 500 ml of 6% hetastarch 30 min prior to the surgery. Patient was then put to left lateral position and under aseptic precautions spinal anesthesia was performed at the L2-3 or L3-4 interspaces. The skin was infiltrated with 2 ml of 2% local anesthetic (lignocaine). Then using a 23-gauge Quincke – Babcock needle, with the side port of the needle pointing cephalad, all subjects received 10 mg (2 cc) of 0.5% bupivacaine (H) in dextrose. Immediately after the injection the patients were positioned supine with left uterine displacement. Oxygen 5 L/min was administered using a face mask. BP was measured every min for first 10 min then, every 3 min until extraction of baby and 5 min thereafter until the end of surgery. Definition – hypotension is defined as a SBP <100 mm Hg and <80% of the baseline BP. The baseline BP was determined by calculating the mean of three BP measurements taken preoperatively before fluid loading was given. Hypotension was treated with IV boluses of 5 mg ephedrine, and additional rapid infusion bolus of ephedrine treatment was repeated every 2 min if hypotension persisted or recurred. The maximum height of the block was assessed by a pinprick. All other drugs were given and their doses, the amount of additional IV fluids given before delivery were recorded. The incidence and timing of nausea and/or vomiting were monitored. The interval between spinal injection delivery and the uterine incision-delivery interval will be noted. Following delivery, the neonatal outcome was assessed using the Apgar score. Patients were monitored till the recovery from the spinal anesthesia.
Statistical analysis
A number of patients in each group was decided as per statistician's advice with pilot study results. Both these groups were compared and statistically analyzed using Student's t-test and significance evaluated by P value. Repeated – measures analysis of variance were used to compare measurements of BP and pulse over time. P < 0.05 considered as statistically significant. Statistical analysis carried out using MedCalc Statistical software version 11.0 (MedCalc software, Buba, Belgium).
RESULTS
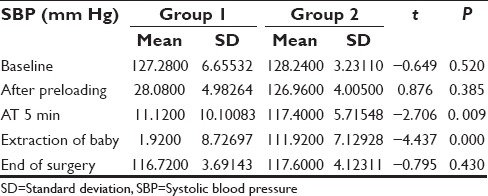
In our study, we included 50 ASA I and II pregnant patients who were scheduled for the elective cesarean section under spinal anesthesia. Both groups were similar with respect to age, height, weight, gestational age and the upper level of the spinal blockade [Table 1]. Both groups had similar preinduction SBP and HR. However, after spinal anesthesia there was a significant difference in SBP from 5 min to the extraction of the baby. The Group 1 (RL) had a mean ranging from 111.1200 to 101.9200 and the Group 2 (6% hetastarch) had a mean range of 117.4000–111.9200 during this period. The minimum SBP was significantly lower in Group 1 at the time of extraction of the baby when compared to Group 2 [Figures 1–3]. While the HR was higher in Group 1 during the extraction of the baby (between 8 and 10 min) following spinal anesthesia [Tables 2–4]. The incidence of hypotension was significantly higher in Group 1 (RL) than in Group 2 (hetastarch). Eighty percent of the patients in Group 1 had developed hypotension while only 28% of the patients developed in Group 2 [Table 5]. Hypotension was treated with repeated boluses of 5 mg of ephedrine. Despite a significant difference in the incidence and severity of hypotension in the Group 1 (RL), the neonatal outcome was uniformly good in both groups [Table 6]. No adverse reactions to hetastarch occurred in this study while a small group developed nausea and vomiting in both the groups 10 min after the induction of spinal anesthesia [Table 7].
Table 1.
Inter group comparison of nonparametric data
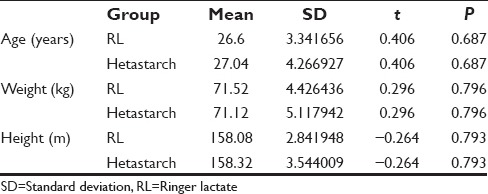
Figure 1.
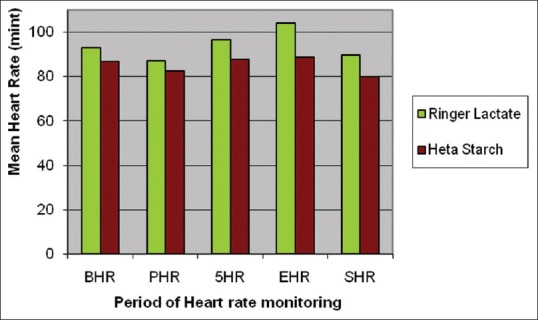
Comparison of heart rate
Figure 3.
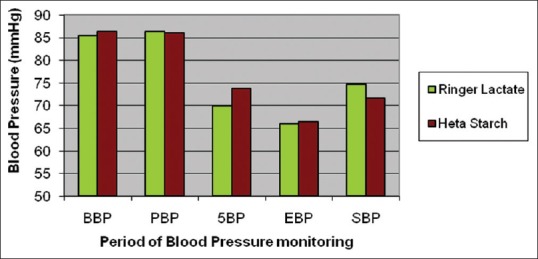
Comparison of diastolic blood pressure
Table 2.
Inter group comparison of HR
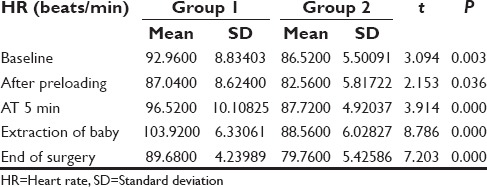
Table 4.
Inter group comparison of DBP
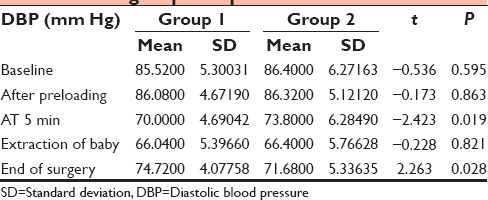
Table 5.
Incidence of hypotension
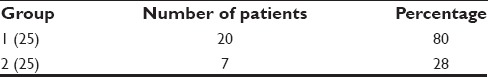
Table 6.
Adverse reactions
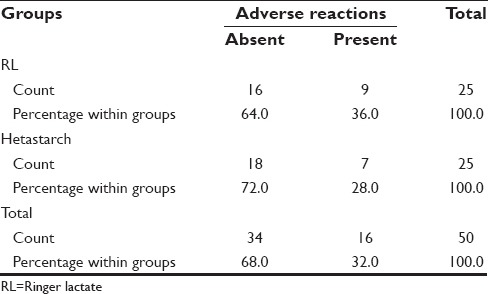
Table 7.
Inter group comparison in neonatal outcome
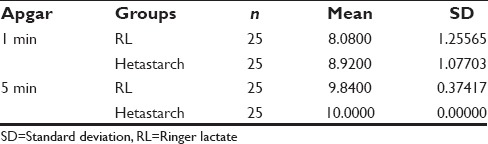
Figure 2.
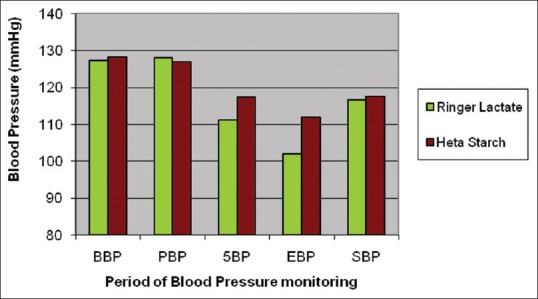
Comparison of systolic blood pressure
Table 3.
Inter group comparison of SBP
DISCUSSION
For cesarean section, spinal anesthesia is the preferred regional anesthesia.[1] For delivery only, a single–shot spinal subarachnoid block can be induced rapidly and is a more practical choice. In elective cesarean section under spinal anesthesia hypotension has been reported in as many as 85% of the patients. Prior to spinal anesthesia preloading is recommended to reduce the incidence of hypotension.
Hypotension develops as the result of various factors such as;
The level at which the block was performed
The level of anesthesia
Age of patient
Condition of the patient and hemodynamic status.
Since BP can be described as product of cardiac output and total peripheral vascular resistance, the usual management has been directed towards one or the other of these two factors: The use of peripheral vasoconstrictors to increase the total peripheral resistance or the use of drugs with inotropic or chronotropic cardiac action to augment the output of the heart. Another method of increasing cardiac output is to augment the venous return by the temporary expansion of blood volume.[4] Many authorities suggest that crystalloid preloading is not effective in reducing the incidence of hypotension after spinal anesthesia.[5,6,7] As much as 75% of the infused volume diffuses into the interstitial spaces, and it's efficacy in expanding plasma volume is only transient. Large volumes of crystalloid can also decrease the oxygen-carrying capacity and is associated with the increased risk of pulmonary and peripheral edema,[8,9] has been demonstrated that colloid may be superior for volume preloading[10,11] by sustaining an increased blood volume, cardiac output due to a longer intravascular half-life. Six percent hetastarch has a half-life of 17 days, but this is misleading because its oncotic properties disappear after 24 h. It causes 150% volume expansion. In our study, patients receiving 6% hetastarch had a lower incidence of hypotension when compared with those who received lactated Ringers solution. Our study showed the incidence of hypotension to be 28% in the hetastarch group and 80% in the RL group. This is consistent with the findings of others who compared colloids and crystalloid fluid administration prior to spinal anesthesia.[12] However, after spinal anesthesia there was a significant difference in SBP from 5 min to the extraction of the baby. The Group 1 (RL) had a mean ranging from 111.1200 to 101.9200 and the Group 2 (6% hetastarch) had a mean range of 117.4000–111.9200 during this period. The minimum SBP was significantly lower in Group 1 at the time of extraction of the baby when compared to Group 2, while the HR was higher in Group 1 during the extraction of the baby (between 8 and 10 min) following spinal anesthesia. In our study, the number of boluses of ephedrine 5 mg IV required to maintain the SBP above 100 mm Hg was more for LR group while the hetastarch group hardly required vasopressor support. This is consistent with other studies.[11] In our study, the mean HR was consistently high in the lactated Ringers group than in 6% hetastarch group. Colloids are known to cause anaphylactoid reactions, and hemodynamic instability is an important feature of this reaction along with the rash and bronchospasm. However, in our study no patients developed any such adverse reaction. Our study showed that colloid offset hypotension and hypovolemia more effectively than crystalloids in patients scheduled for elective cesarean section.[13]
In another study conducted on pregnant women scheduled for elective cesarean section in a tertiary hospital in Nigeria, patients were randomized into two groups to receive either 1000 ml of crystalloid/colloid (750/250 ml) combination or 500 ml colloid IV fluid preloaded before spinal anesthesia. In first 10 min, crystalloid-colloid combination showed better efficacy in hypotension prophylaxis over the colloid only regime. Beyond 10 min, the combination had no advantage.[14] In another study, crystalloid prehydration seems to be of little use and current focus is on timing of administration of fluids and use of colloids. It was proved that phenylephrine was proved to be as good as ephedrine for maintaining BP and a more liberal use of this drug were justified.[15] In another study, it was concluded a combination of preventive methods decreased the occurrence of hypotension following spinal anesthesia to an acceptable level.[16] In one another study combination of colloid cohydration and phenylephrine infusion initiated at 60 µg/min maintained maternal hemodynamics and neonatal well-being during cesarean deliveries requiring minimum interventions by anesthesiologist.[17] In another study, hydroxyethyl starch 6% 500 ml before administration of spinal anesthesia and ephedrine 15 mg IV bolus right after spinal anesthesia was effective in preventing hypotension during cesarean section.[18]
CONCLUSION
Preloading the pregnant patients who received spinal anesthesia for elective cesarean section with either 1000 ml of crystalloid (lactated Ringers solution) or 500 ml of colloid (6% hetastarch) showed: Colloid to be more effective in prevention of hypotension than crystalloid. Six percent hydroxyethyl starch offset the hypotension and hypovolemia more effectively than lactated Ringers solution in patients scheduled for the elective cesarean section under spinal anesthesia. It is also relatively free of side effects.
Hence, we conclude that the routine use of colloids-6% hydroxyl ethyl starch as the choice for preloading prior to spinal anesthesia in order to maintain the hemodynamic stability of the parturient perioperatively.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Bridenbaugh PO, Greene NM, Brull SJ. Spinal (subarachnoid) neural blockade. In: Cousins MJ, Bridenbaugh PO, editors. Neural Blockade in Clinical Anesthesia and Management of Pain. 3rd ed. Philadelphia: Lippincott-Raven Publishers; 1998. pp. 203–42. [Google Scholar]
- 2.Wollman SB, Marx GF. Acute hydration for prevention of hypotension of spinal anesthesia in parturients. Anesthesiology. 1968;29:374–80. doi: 10.1097/00000542-196803000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Sathe LL, Shah BN. Spinal preloading-colloids vs crystalloids. Bull Intensive Crit Care. 1996;3:4–15. [Google Scholar]
- 4.Graves CL, Underwood PS, Klein RL, Kim YI. Intravenous fluid administration as therapy for hypotension secondary to spinal anesthesia. Anesth Analg. 1968;47:548–56. [PubMed] [Google Scholar]
- 5.Levinson G. Clinical Procedures in Anesthesia and Intensive Care. Philadelphia: Lippincott-Raven Publishers; 1992. Spinal anesthesia; pp. 645–60. [Google Scholar]
- 6.Rout CC, Akoojee SS, Rocke DA, Gouws E. Rapid administration of crystalloid preload does not decrease the incidence of hypotension after spinal anaesthesia for elective caesarean section. Br J Anaesth. 1992;68:394–7. doi: 10.1093/bja/68.4.394. [DOI] [PubMed] [Google Scholar]
- 7.Gajraj NM, Victory RA, Pace NA, Van Elstraete AC, Wallace DH. Comparison of an ephedrine infusion with crystalloid administration for prevention of hypotension during spinal anesthesia. Anesth Analg. 1993;76:1023–6. doi: 10.1213/00000539-199305000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Cyna AM, Andrew M, Emmett RS, Middleton P, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section (Review) Cochrane Collab. 2009;1:1–212. doi: 10.1002/14651858.CD002251.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Mathru M, Rao TL, Kartha RK, Shanmugham M, Jacobs HK. Intravenous albumin administration for prevention of spinal hypotension during cesarean section. Anesth Analg. 1980;59:655–8. [PubMed] [Google Scholar]
- 10.Ueyama H, He YL, Tanigami H, Mashimo T, Yoshiya I. Effects of crystalloid and colloid preload on blood volume in the parturient undergoing spinal anesthesia for elective Cesarean section. Anesthesiology. 1999;91:1571–6. doi: 10.1097/00000542-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Riley ET, Cohen SE. Prevention of hypotension after spinal anaesthesia for caesarean section: Six percent hetastarch versus lactated Ringers solution. Anesth Analg. 1995;81:838–42. doi: 10.1097/00000539-199510000-00031. [DOI] [PubMed] [Google Scholar]
- 12.Sharma SK, Gajraj NM, Sidawi JE. Prevention of hypotension during spinal anesthesia: A comparison of intravascular administration of hetastarch versus lactated Ringer's solution. Anesth Analg. 1997;84:111–4. doi: 10.1097/00000539-199701000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Teoh WH, Sia AT. Colloid preload versus coload for spinal anesthesia for cesarean delivery: The effects on maternal cardiac output. Anesth Analg. 2009;108:1592–8. doi: 10.1213/ane.0b013e31819e016d. [DOI] [PubMed] [Google Scholar]
- 14.Idehen HO, Amadasun FE, Ekwere IT. Comparison of intravenous colloid and colloid-crystalloid combination in hypotension prophylaxis during spinal anesthesia for cesarean section. Niger J Clin Pract. 2014;17:309–13. doi: 10.4103/1119-3077.130231. [DOI] [PubMed] [Google Scholar]
- 15.Mitra JK, Roy J, Bhattacharyya P, Yunus M, Lyngdoh NM. Changing trends in the management of hypotension following spinal anesthesia in cesarean section. J Postgrad Med. 2013;59:121–6. doi: 10.4103/0022-3859.113840. [DOI] [PubMed] [Google Scholar]
- 16.Jabalameli M, Soltani HA, Hashemi J, Behdad S, Soleimani B. Prevention of post-spinal hypotension using crystalloid, colloid and ephedrine with three different combinations: A double blind randomized study. Adv Biomed Res. 2012;1:36. doi: 10.4103/2277-9175.100129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sen I, Hirachan R, Bhardwaj N, Jain K, Suri V, Kumar P. Colloid cohydration and variable rate phenylephrine infusion effectively prevents postspinal hypotension in elective Cesarean deliveries. J Anaesthesiol Clin Pharmacol. 2013;29:348–55. doi: 10.4103/0970-9185.117106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salman OH, Yehia AH. Randomised double blind comparison of intravenous ephedrine and hydroxyethyl starch six% for spinal induced hypotension in elective cesarean section. Ain Shams J Anaesthesiol. 2014;7:221–5. [Google Scholar]


