Abstract
Objective:
To assess the effect of adding acupuncture to standard swallowing training for patients with dysphagia after stroke.
Design:
Single-blind randomized controlled trial.
Setting:
Inpatient and outpatient clinics.
Subjects:
A total of 124 patients with dysphagia after stroke were randomly divided into two groups: acupuncture and control.
Interventions:
The acupuncture group received standard swallowing training and acupuncture treatment. In comparison, the control group only received standard swallowing training. Participants in both groups received six days of therapy per week for a four-week period.
Main measures:
The primary outcome measures included the Standardized Swallowing Assessment and the Dysphagia Outcome Severity Scale. The secondary outcome measures included the Modified Barthel Index and Swallowing-Related Quality of Life, which were assessed before and after the four-week therapy period.
Results:
A total of 120 dysphagic subjects completed the study (60 in acupuncture group and 60 in control group). Significant differences existed in the Standardized Swallowing Assessment, Dysphagia Outcome Severity Scale, Modified Barthel Index, and Swallowing-Related Quality of Life scores of each group after the treatment (P < 0.01). After the four-week treatment, the Standardized Swallowing Assessment (mean difference − 2.9; 95% confidence interval (CI) – 5.0 to − 0.81; P < 0.01), Dysphagia Outcome Severity Scale (mean difference 2.3; 95% CI 0.7 to 1.2; P < 0.01), Modified Barthel Index (mean difference 17.2; 95% CI 2.6 to 9.3; P < 0.05) and Swallowing-Related Quality of Life scores (mean difference 31.4; 95% CI 3.2 to 11.4; P < 0.01) showed more significant improvement in the acupuncture group than the control group.
Conclusions:
Acupuncture combined with the standard swallowing training may be beneficial for dysphagic patients after stroke.
Keywords: Dysphagia, stroke, acupuncture, swallowing training
Introduction
Dysphagia is a common impairment following stroke; it presents in about 45%−65% of patients after acute stroke1, 2 and 11%−13% of patients cannot recover swallowing function after six months.3, 4 The presence of dysphagia has been associated with an increased risk of pneumonia, dehydration, dystrophia, recurrent stroke, prolonged length of stay in hospital, and mortality, leading to a poor prognosis.5 Previous studies have suggested that untreated dysphagia delays functional recovery and better swallowing function is closely related with a better quality of life (QOL).4 Therefore, early identification and treatment of dysphagia is critical for patients after stroke.
In recent years, many studies have focused on earlier dysphagia diagnosis using bedside or instrumental tests, therapeutic measures (formal swallowing therapy, acupuncture, drug therapy, and stimulation), and dietary management (percutaneous endoscopic gastrostomy, nasogastric tube feeding, oral intake, and dietary modification).6–8 Effective rehabilitation is believed to shorten the course of this impairment, lighten the burden for both patients and society, and reduce the mortality rate.9–11 A review by Cochrane from 201212 concluded that insufficient data remains related to swallowing therapy effects on functional outcome and death in dysphagic patients with either acute or subacute stroke, but behavioral interventions and acupuncture can reduce dysphagia. The standard swallowing training includes the most basic and traditional methods, involving compensation strategies such as postural adjustment or diet modification, strengthening weak oropharyngeal musculature through oral exercise, following oropharyngeal swallowing maneuvers to augment impaired anatomy, heightening sensory input through thermal-tactile stimulation, and developing a feeding-swallowing training program.13 Each exercise works from a different aspect to significantly improve swallowing function.
Acupuncture is an effective, simple, inexpensive, and primary medical intervention. It has been widely used as a primary medical intervention in China and elsewhere in East Asia for many years, and continues to be a standard complementary therapy after stroke in that region. Needles are inserted into acupoints to achieve a “de qi” reaction, where the patient perceives an ache or heaviness in the area surrounding the needle. Although it has gained increased attention, arguments still remain about its effectiveness. While large numbers of articles have shown the effectiveness of acupuncture for treating dysphagia after stroke, some conclusions are unreliable owing to their poor design.14, 15 For example, a review by Cochrane from 200816 concluded not enough evidence was available to show a therapeutic effect of acupuncture for dysphagia after acute stroke; high quality and large-scale randomized controlled trials were necessary.
Thus, we designed a randomized controlled trial of Combined Swallowing Training and Acupuncture Methods, aiming to find its effect on dysphagia after acute stroke. We hypothesized that effects of acupuncture following standard swallowing training would be synergistic as compared with standard swallowing training. Our study assessed if adding acupuncture to standard swallowing training could improve dysphagic stroke patients in China.
Materials and methods
Patient characteristics
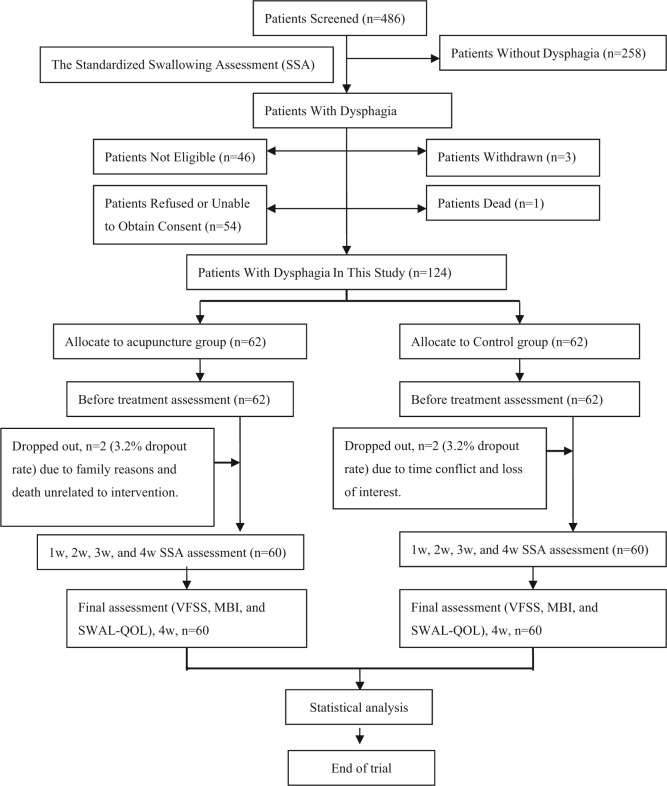
This prospective study included 62 patients in the acupuncture group (27 women and 35 men, median age 65.3 years) and 62 patients in the control group (26 women and 36 men, median age 66.1 years). The age and gender distribution, previous medical history, etiology, and severity of dysphagia were similar between the two groups. Details of attrition are shown in Figure 1. Four subjects dropped out (two in the acupuncture group and two in the control group) owing to time conflict, family reasons, or loss of interest, and one patient died because of illness (unrelated to intervention) before completing the study. All clinical parameters were shown in Table 1.
Figure 1.
Flow diagram for patient screening in this study.
MBI: Modified Barthel Index; SWAL-QOL: Swallowing-Related Quality of Life; VFSS: video fluoroscopic swallowing study.
Table 1.
General characteristics of the subjects.
| Characteristics | Acupuncture group (n = 62) | Control group (n = 62) | P value |
|---|---|---|---|
| Age (years, mean ± SD) | 65.3 ± 14.2 | 66.1 ± 14.3 | 0.76 |
| Gender (men/women) | 35/27 | 36/26 | 0.85 |
| Previous medical history, N (%) | |||
| Hypertension | 51 (82.3) | 54 (87.1) | 0.46 |
| Diabetes | 43 (69.4) | 39 (62.9) | 0.45 |
| Hyperlipidemia | 46 (74.2) | 40 (64.5) | 0.24 |
| Atrial fibrillation | 38 (61.3) | 35 (56.5) | 0.58 |
| Etiology, N (%) | |||
| Cerebral infarction | 43 (69.4) | 42 (67.7) | 0.85 |
| Cerebral hemorrhage | 17 (27.4) | 19 (30.6) | 0.69 |
| Subarachnoid hemorrhage | 2 (3.2) | 1 (1.6) | 0.56 |
| Location of lesion, N (%) | |||
| Basal ganglia or thalamus | 48 (77.4) | 46 (74.2) | 0.68 |
| MCA territories | 10 (16.1) | 13 (21.0) | 0.49 |
| Brainstem | 4 (6.5) | 3 (4.8) | 0.70 |
| Side of lesion, N (%) | |||
| Right | 35 (56.5) | 37 (59.7) | 0.72 |
| Left | 24 (38.7) | 23 (37.1) | 0.85 |
| Both | 3 (4.8) | 2 (3.2) | 0.65 |
| Days from onset (mean ±SD) | 9.3 ± 2.3 | 8.7 ± 2.5 | 0.59 |
| The Dysphagia Outcome Severity Scale (DOSS) | 1.8 (0.7) | 1.6 (0.6) | 0.71 |
| The stage of dysphagia, N (%) | |||
| Oral stage | 33 (53.2) | 35 (56.5) | 0.81 |
| Pharyngeal phase | 37 (59.6) | 34 (54.8) | 0.71 |
| Esophageal phase | 12 (19.4) | 14 (22.6) | 0.65 |
MCA: middle cerebral artery; SD: standard deviation.
P>0.05 vs. control group.
Clinical data
This study was a randomized, single-blind clinical trial that contained two parallel arms. A total of 124 patients who developed dysphagia after stroke were admitted to the Departments of Neurology and Physical Medicine and Rehabilitation, Hubei Xinhua Hospital in Wuhan, China. All participants were diagnosed17 between June 2012 and May 2014.
Inclusion criteria included a primary diagnosis of stroke by magnetic resonance imaging or computerized tomography scans. A video fluoroscopic swallowing study (VFSS) identified dysphagia and then severity at the time of participation (between four and 12 days after stroke) was rated using the Dysphagia Outcome Severity Scale (DOSS). Patients ranged between 40 and 80 years of age. Assessments were based on their ability to follow instructions and engage in study procedures as well as their ability to give informed consent.
Exclusion criteria included the presence of serious diseases of the liver, kidney, hematological system, or endocrine system, psychiatric disorders, severe cognitive impairment, severe aphasia, or other diseases that potentially impaired swallowing function, such as head and neck tumors, esophageal neoplasms, craniocerebral injury, myasthenia gravis, and Guillain-Barre syndrome.
Subjects were randomly selected and divided into two groups by randomly numbered tables. Patients in the acupuncture group (n = 62) were subjected to swallowing training and acupuncture treatment; those in the control group (n = 62) only received swallowing training. Evaluators and statisticians were blinded throughout the study period. All investigators were trained to ensure strict adherence to study protocol.
Ethics
This study was reviewed and approved by the Ethics Committee of Hubei Xinhua Hospital in Wuhan, China (2012007). All patients provided written informed consent before enrollment in the study.
Measurements
Interventions
Standard swallowing training
This process was used to improve patient dysphagia. Functional training was applied to the feeding and swallowing organs (lip, cheek, tongue, soft palate, pharynx, throat, and esophageal sphincter). This included active or passive exercise of the oral, facial, and lingual muscles, sensory stimuli, and some specialized methods such as the Mendelsohn maneuver, supraglottic and superglottic maneuvers, swallowing efforts, and the Shaker exercise.18 Feeding–swallowing training occurred in a quiet room, where patients were placed in a safe and appropriate position as per their medical conditions and personal preference. They were instructed to swallow boluses of an appropriate volume of different consistencies.
Patients were treated with standard swallowing training according to information obtained from their VFSS tests. These training regimens were adjusted based on patient swallowing function. Each patient had one-on-one treatment for 30 minutes per session. A training intervention consisted of 24 sessions six times a week for four weeks. Standard swallowing training was performed by qualified and experienced speech–language therapists.
Acupuncture treatment
The nape, scalp, and tongue acupuncture were conducted by an acupuncturist using Traditional Chinese Medicine (TCM) theory. The TCM theory believes the core of disease onset is the disruption of “qi”, specifically “vital energies” of the body. Stroke patients were divided into three syndrome patterns based on TCM:19 phlegm turbidity syndrome; blood stasis syndrome due to qi stagnation; and the liver–kidney yin deficiency syndrome. The phlegm turbidity syndrome is a pathological change characterized by impaired diffusion and the down bearing of lung qi owing to phlegm-dampness obstruction. The blood stasis syndrome owing to qi stagnation is a pathological change in which a long-standing or severe qi stagnation impedes blood flow; this condition is characterized by the coexistence of qi stagnation and blood stasis. The liver–kidney yin deficiency syndrome is a pathological change in which insufficient yin (liver and kidney fluid) fails to nourish the related body constituents and organs, giving rise to deficiency-fire symptoms. The main acupoints were fengchi (GB 20, unilateral), jiaji (C2-C4) (EX-B2, bilateral), lianquan (CV 23, unilateral), jiajianquan (left CV 23 and right CV 23, bilateral), and baihui (GV 20, unilateral), and the combination acupoints were lieque (LV 07, bilateral), fenglong (ST 40, bilateral), sanyinjiao (SP 06, bilateral), jinjin and yuye (Z- 20, unilateral), taixi (K 103, bilateral), and zhaohai (K 106, bilateral). The main acupoints were used in all patients (Figures 2, 3, and 4, available online). The originally prescribed acupuncture treatment points were made according to the disease state. Points were added or subtracted based on patient presentation. Empirical acupuncture treatment, involving the use of multiple needles in various locations, was also used to complement the original treatment paradigm.
Patients laid supine on a massage table or sat in a comfortable chair with their arms and legs exposed. The skin on the acupuncture points was prepared with 70% ethyl alcohol. One-time-use disposable sterile steel needles(0.20–0.25 × 25–75 mm) were inserted into acupuncture points. The depth of insertion at each point was between 10–30 mm, except for points on Z-20 and GV20, which were between 5–10 mm. After insertion, acupuncture needles were manually manipulated to obtain the de qi sensation. The de qi sensation is defined as the acupuncturist feeling the muscle twitch response and the patient feeling an ache or heaviness in the area surrounding the needle. The needles remained in place for 30 minutes. After 30 minutes of treatment, needles were manually manipulated again before removal. An average of 16.2 needles (range 12–23) were used during each acupuncture session for each patient. Acupuncture was performed after swallowing training for 24 sessions, which comprised of sessions six times a week for a period of four weeks.
All patients were given general medication, supportive mental health treatment (i.e. psychotherapy and health education), and standard swallowing training. All acupuncturists had high standards of education and experience. Care was available for any possible sequelae that may occur. Each patient had usual access to their primary physician and acupuncturist. Patients were informed and explained of all intervention sessions.
Outcome measurement
The standardized swallowing assessment (SSA)20 consisted of three steps. The first was the clinical examination, followed by 5 mL of water given three times to the patient. In Stage 2, if the swallowing was normal in Stage 1, 60 mL of water in a beaker was given to the patient. SSA scores ranged from 17 to 46, with a higher score indicating a decreased swallowing ability.
The DOSS rating scale21 is a relatively simple seven-point scale developed to systematically rate dysphagia severity based on the VFSS. It helped make recommendations for patient diet level, independence level, and type of nutrition. In the VFSS, 200 mg barium was added into 286 mL water to make radiopaque material (60%); rice flour was added to make a thin liquid, thick liquid, and a solid food. Patients sequentially consumed the above liquids starting at 2 mL, subsequently increasing to 5 mL, and then 10 mL. Fluoroscopy was used to image swallowing in lateral and anteroposterior projections. All patients were assessed with the DOSS, with Level 7 representing normal swallowing and Level 1 representing severe dysphagia.
The Modified Barthel Index (MBI)22 was used to provide a measurement of daily patient activities. It yielded scores up to 100, with the highest score indicating complete independence in self-care; a lower score indicated a worse level of daily patient activities.
The Swallowing-Related Quality of Life (SWAL-QOL) questionnaire was used to measure patient QOL. This self-reported questionnaire consisted of 44 items; a higher score indicated a higher QOL.23
Primary outcome measures included the SSA and the DOSS. The SSA was assessed after each week of treatment over a four-week period. The DOSS was assessed after the fourth week of treatment. Secondary outcome measures included the MBI and the SWAL-QOL, which were assessed after the fourth week of treatment. Evaluators were trained in testing procedures; a comprehensive assessment manual has been developed to ensure standardized performance.
Adverse events
Adverse events of acupuncture included pain, dizziness, bleeding, aggravation, hematoma and infection, and discomfort. Adverse events of swallowing training included discomfort and aggravation.
Physicians recorded any unexpected and unintended responses. In addition, they recorded reasons for missing outcome assessments or treatment sessions.
Sample size calculation
Based on data from previous trials, the respective mean and standard deviation (SD) of SSA scores were 24.8 ± 4.6 in the control group and 18.6 ± 4.1 in the treatment group.24 A sample-size calculation was conducted using study size software version 3.0 (CreoStat HB, Frolunda, Sweden), with a type I error of 5% (α = 0.05) and 80% power (β = 0.2). In total, 55 patients were required to show statistical differences between the arms. A targeted sample size of 124 participants was established, which allowed for a 10% drop-out rate.
Statistical analysis
Descriptive statistics were expressed as a mean ±SD. The normality test was done and it met assumptions for the t-test. The SSA, the DOSS, the MBI, and the SWAL-QOL scores were assessed among the two groups at baseline and then after treatment. The scores were compared using student and paired t-tests. Statistical analyses were performed using SPSS software version 18.0 (SPSS Inc, Chicago, IL, USA), and the statistical significance was P < 0.05.
Results
The SSA
There was no difference between the groups either at baseline or one week after treatment in assessment of swallowing function with SSA (P > 0.05). After four weeks of treatment, the SSA scores (mean difference, 2.9; 95% confidence interval (CI): 5 to 0.81; P < 0.01) in the acupuncture group were significantly lower than those in the control group (Figure 5, available online).
The DOSS, the MBI, and the SWAL-QOL
Significant differences were seen in the DOSS, the MBI, and the SWAL-QOL scores in each group after treatment (P < 0.01). After four weeks of treatment, the DOSS (mean difference, 2.3; 95% CI: 0.7 to 1.2; P < 0.01), the MBI (mean difference, 17.2; 95% CI: 2.6 to 9.3; P < 0.05), and the SWAL-QOL scores (mean difference 31.4; 95% CI: 3.2 to 11.4; P < 0.01) were more significantly improved in the acupuncture group than the control group (Table 2).
Table 2.
Comparison of DOSS, MBI, and SWAL-QOL scores between two groups.
| Acupuncture group Mean (SD) |
Control group Mean (SD) |
|||
|---|---|---|---|---|
| Before treatment | 4 weeks after treatment | Before treatment | 4 weeks after treatment | |
| DOSS scores | 1.8 (0.7) | 5.8 (1.3)∆▲ | 1.6 (0.6) | 3.7 (1.1)* |
| MBI scores | 52.3 (15.7) | 88.2 (11.1)∆# | 53.1 (16.3) | 71.0 (12.3)* |
| SWAL-QOL scores | 94.8 (17.9) | 197.1 (19.3)∆▲ | 95.2 (18.6) | 165.1 (19.9)∆ |
MBI: Modified Barthel Index; SWAL-QOL: Swallowing-Related Quality of Life; DOSS:Dysphagia Outcome Severity Scale.
P < 0.05 or ∆P < 0.01 vs before treatment; #P < 0.05 or ▲P < 0.01 vs. control group.
Adverse reactions
The type and number of adverse reactions in the acupuncture group included the following: discomfort (seven patients), hematoma (two patients), and severe pain (one patient), which were related to edema. In comparison, adverse reactions reported in the control group included discomfort (five patients), which was related to swallowing training. Points on Z-20 caused severe pain; points on CV 23, L-CV 23 and R-CV 23 caused a hematoma. All the adverse reactions were shown in Table 3.
Table 3.
Comparison of adverse events between two groups.
| Acupuncture group (n=60) | Control group (n=60) | P value | |
|---|---|---|---|
| Pain N (%) | 1 (1.7) | 0 | 0.32 |
| Hematoma N (%) | 2 (3.3) | 0 | 0.15 |
| Discomfort N (%) | 7 (11.7) | 5 (8.4) | 0.54 |
P > 0.05 vs. control group.
Discussion
In this study, SSA scores were compared between two groups; no significant difference existed in swallowing function before or after a week of treatment. However, significant differences in SSA scores were found at the second, third, and fourth week, indicating that the traditional Chinese acupuncture in combination with standard swallowing training could improve swallowing function recovery. This was most prominent after one week of treatment. After four weeks of treatment, significant improvement was observed in patients from the acupuncture group as compared with the control group regarding swallowing function, daily activities, and QOL. The MBI showed average pre- and post-score increases >10 points. The feeding section on this scale accounted only for feeding and swallowing, suggesting significantly increased independence in other areas. Zhang et al.25 found that acupuncture together with conventional rehabilitation might positively affect dysphagia after stroke. In the current study, acupuncture treatment was adopted in combination with swallowing training, which demonstrated a better outcome than swallowing training alone; this was consistent with results of Zhang et al.25 Similarly, Zhou et al.15 found a more preferable therapeutic outcome, when combining acupuncture at the nape point with swallowing training as compared with different acupuncture sites.
According to TCM, three acupuncture points used at the same time (nape, scalp, and tongue) could “dredge the brain”, “activate the collaterals”, “enliven the mind”, and “open the orifice”. As per dysphagia treatment, acupuncture not only stimulated the muscles related to swallowing activity; it also systematically up-tuned brain function through activation of the peripheral muscles. Some studies have suggested that acupuncture improved recovery of swallowing function. However, owing to their poor design, further studies are necessary. Subsequent studies should have a large sample size, and multiple study center locations to identify their reliability.16, 26, 27 Thus far, acupuncture has been demonstrated to be a safe, effective, and inexpensive treatment without severely unfavorable outcomes; adverse effects that have been present could be subsequently improved.28, 29 In the current study, only one patient complained of severe pain and two patients were observed to have localized edema; all had mild symptoms and improved rapidly in a few hours.
The central nervous system clearly showed flexibility and resilience. Rehabilitation treatment assisted in constructing new motor projection areas and aroused resting synapses to transmit nerve impulses, restoring movement.29–31 Many types of rehabilitation methods, such as bedside exercises, standard swallowing training, and neuromuscular electrical, thermal, and chemical stimulation, are used for patients suffering from dysphagia after stroke. Swallowing training can improve swallowing physiology and improve safety and tolerance, leading patients towards a less-restrictive diet.5 Swallowing training has been regarded as an effective rehabilitation method and is widely used in clinical settings. Currently, swallowing training has been adopted as a basic rehabilitation method, with other therapeutic methods used as adjuvant treatments. Since every single treatment has its own limitations, growing evidence showed that a combination of acupuncture and swallowing training was a promising treatment option in neurorehabilitation, better than single intervention therapy for dysphagia.32, 33
Our study found that the DOSS results correlated well with SSA scores. The VFSS assessment needed to be performed under radiation, and thus was not suitable for repeated tests within a short time period. SSA instead of a VFSS should be used if repeated assessment must be done in the short term to adjust therapy. The current study dynamically observed the recovery of swallowing function after stroke; it explored effective time, duration, and effective peak time, consequently helping to design rehabilitation strategy in clinical practices.
The current study had several limitations. A lack of an acupuncture control group might be the most significant flaw; establishment of a sham acupuncture control group would not meet requirements of the ethics committee. Low compliance did not allow us to set up a sham acupuncture control group. Although this study was not a double-blinded trial, the evaluator and statistical analyzers were blinded to reduce the bias and ensure the quality of this experiment. Most patients had spontaneous recovery of swallowing function; however, this group could not be excluded. In the current study, the small sample size and lack of multicenter involvement, along with short-term evaluation and follow-up, were factors impeding assessment of the long-term therapeutic effect and experiment consistency. Hence, there is room for improvement in future studies.
The current study was performed to explore a characteristic, standard, canonical, feasible, and easy-operated scheme to facilitate recovery of swallowing function in patients with dysphagia after stroke. We found that acupuncture in combination with swallowing training for patients with dysphagia after stroke was a therapeutic effect observed in the joint rehabilitation treatment.
Clinical message.
The consecutive four-week treatment of acupuncture combined with standard swallowing training could effectively improve swallowing function, activities of daily living, and the quality of life in patients with dysphagia after stroke. This result may provide a better rehabilitation treatment for dysphagia after stroke.
(Registration number: ChiCTR-10R-14005249)
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Contributors: Wenguang Xia: Conception and design, clinical studies, manuscript preparation, and guarantor of integrity of entire study.
Chanjuan Zheng: Literature research, clinical studies, and data acquisition.
Suiqiang Zhu: Conception, clinical studies, and manuscript editing.
Zhouping Tang: Data analysis and statistical analysis.
Conflict of interest: The authors declare that they have no competing interests.
Funding: This study was supported by a grant from Hubei province health department of China [NO.JX5B36].
References
- 1. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Arch Phys Med Rehabil 1998; 79: 14–19. [DOI] [PubMed] [Google Scholar]
- 2. Smithard DG, O’Neill PA, Park C, et al. Can bedside assessment reliably exclude aspiration following acute stroke? Age Ageing 1998; 27: 99–106. [DOI] [PubMed] [Google Scholar]
- 3. Nakajima M, Inatomi Y, Yonehara T, Hashimoto Y, Hirano T. Acquisition of oral intake in severely dysphagic patients with acute stroke: A single-center, observational study involving a database of 4972 consecutive stroke patients. J Neurol Sci 2012; 323: 56–60. [DOI] [PubMed] [Google Scholar]
- 4. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005; 36: 2756–2763. [DOI] [PubMed] [Google Scholar]
- 5. González-Fernández M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after Stroke: An overview. Curr Phys Med Rehabil Rep 2013; 1: 187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Daniels SK, Anderson JA, Willson PC. Valid items for screening dysphagia risk in patients with stroke: A systematic review. Stroke 2012; 43: 892–897. [DOI] [PubMed] [Google Scholar]
- 7. Martino R. Screening and clinical assessment of oropharyngeal dysphagia. Nestle Nutr Inst Workshop Ser 2012; 72: 53–56. [DOI] [PubMed] [Google Scholar]
- 8. Prosiegel M, Riecker A, Weinert M, et al. [Management of dysphagic patients with acute stroke] in German. Nervenarzt 2012; 83: 1590–1599. [DOI] [PubMed] [Google Scholar]
- 9. McMicken BL, Muzzy CL. Functional outcomes of standard dysphagia treatment in first time documented stroke patients. Disabil Rehabil 2009; 31: 806–817. [DOI] [PubMed] [Google Scholar]
- 10. Han DS, Pan SL, Chen SY, Lie SK, Lien IN, Wang TG. Predictors of long-term survival after stroke in Taiwan. J Rehabil Med 2008; 40: 844–849. [DOI] [PubMed] [Google Scholar]
- 11. Kind A, Anderson P, Hind J, Robbins J, Smith M. Omission of dysphagia therapies in hospital discharge communications. Dysphagia 2011; 26: 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Geeganage C, Beavan J, Ellender S, Bath PM. Interventions for dysphagia and nutritional support in acute and subacute-stroke. Cochrane Database Syst Rev 2012; 17(10): CD000323. [DOI] [PubMed] [Google Scholar]
- 13. Kiger M, Brown CS, Watkins L. Dysphagia management: an analysis of patient outcomes using VitalStim therapy compared to traditional swallow therapy. Dysphagia 2006; 21: 243–253. [DOI] [PubMed] [Google Scholar]
- 14. Shi X, Yang Z, Zhang C, et al. Clinical observations on acupuncture treatment of pseudobulbar palsy—a report of 325 cases. J Tradit Chin Med 1999; 19: 27–31. [PubMed] [Google Scholar]
- 15. Zhou XM, Li XZ, Gu BL. [Clinical research on post-stroke dysphagia treated with nape acupuncture and rehabilitation training] in Chinese. Zhongguo Zhen Jiu 2013; 33: 587–590. [PubMed] [Google Scholar]
- 16. Xie Y, Wang L, He J, Wu T. Acupuncture for dysphagia in acute stroke. Cochrane Database Syst Rev 2008; 16(3): CD006076. [DOI] [PubMed] [Google Scholar]
- 17. Bülow M, Speyer R, Baijens L, Woisard V, Ekberg O. Neuromuscular electrical stimulation (NMES) in stroke patients with oral and pharyngeal dysfunction. Dysphagia 2008; 23: 302–309. [DOI] [PubMed] [Google Scholar]
- 18. Clark HM. Specificity of training in the lingual musculature. J Speech Lang Hear Res 2012; 55: 657–667. [DOI] [PubMed] [Google Scholar]
- 19. Seki T, Iwasaki K, Arai H, et al. Acupuncture for dysphagia in poststroke patients: A videofluoroscopic study. J Am Geriatr Soc 2005; 53: 1083–1084. [DOI] [PubMed] [Google Scholar]
- 20. Smithard DG, O’Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke 1996; 27: 1200–1204. [DOI] [PubMed] [Google Scholar]
- 21. O’Neil KH, Purdy M, Falk J, Gallo L. The Dysphagia Outcome and Severity Scale. Dysphagia 1999; 14: 139–145. [DOI] [PubMed] [Google Scholar]
- 22. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 1989; 42: 703–709. [DOI] [PubMed] [Google Scholar]
- 23. McHorney CA, Bricker DE, Kramer AE, et al. The SWAL-QOL outcomes tool for oropharyngeal dysphagia in adults: I. Conceptual foundation and item development. Dysphagia 2000; 15: 115–121. [DOI] [PubMed] [Google Scholar]
- 24. Xia W, Zheng C, Lei Q, et al. Treatment of post-stroke dysphagia by vitalstim therapy coupled with conventional swallowing training. J Huazhong Univ Sci Technolog Med Sci 2011; 31: 73–76. [DOI] [PubMed] [Google Scholar]
- 25. Zhang JH, Wang D, Liu M. Overview of systematic reviews and meta-analyses of acupuncture for stroke. Neuroepidemiology 2014; 42: 50–58. [DOI] [PubMed] [Google Scholar]
- 26. Long YB, Wu XP. A meta-analysis of the efficacy of acupuncture in treating dysphagia in patients with a stroke. Acupunct Med 2012; 30: 291–297. [DOI] [PubMed] [Google Scholar]
- 27. He J, Zheng M, He CQ, et al. [Systematic assessment of acupoint stimulating therapy for deglutition disorders after apoplexy] in Chinese. Zhongguo Zhen Jiu 2009; 29: 66–71. [PubMed] [Google Scholar]
- 28. Zhao XF, Du Y, Liu PG, Wang S. Acupuncture for stroke: evidence of effectiveness, safety, and cost from systematic reviews. Top Stroke Rehabil 2012; 19: 226–233. [DOI] [PubMed] [Google Scholar]
- 29. Barritt AW, Smithard DG. Role of cerebral cortex plasticity in the recovery of swallowing function following dysphagic stroke. Dysphagia 2009; 24: 83–90. [DOI] [PubMed] [Google Scholar]
- 30. Robbins J, Butler SG, Daniels SK, et al. Swallowing and dysphagia rehabilitation: translating principles of neural plasticity into clinically oriented evidence. J Speech Lang Hear Res 2008; 51: S276–300. [DOI] [PubMed] [Google Scholar]
- 31. Kang JH, Park RY, Lee SJ, Kim JY, Yoon SR, Jung KI. The effect of bedside exercise program on stroke patients with Dysphagia. Ann Rehabil Med 2012; 36: 512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lee KW, Kim SB, Lee JH, Lee SJ, Ri JW, Park JG. The effect of early neuromuscular electrical stimulation therapy in acute/subacute ischemic stroke patients with Dysphagia. Ann Rehabil Med 2014; 38: 153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xu SB, Huang B, Zhang CY, et al. Effectiveness of strengthened stimulation during acupuncture for the treatment of Bell palsy: A randomized controlled trial. CMAJ 2013; 185: 473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.