ABSTRACT
Vulnerable communities in Malaysia have been facing issues of accessibility and availability for pediatric cardiac services for years due to long waiting times, high costs and a lack of pediatric cardiothoracic surgeons. To ease this situation, the government has allocated a certain amount of funds, introduced through the Pediatric Cardiothoracic Program (PCP), in which the patients are transported to the Narayana Health Institute of Cardiac Science (NH) in India to receive a heart operation following an eligibility check at MediAssist4U Sdn Bhd in Selangor, Malaysia, a facility appointed by the NH. This study aimed to determine the demographic incidence of congenital heart diseases of patients in this program and to evaluate the outcome of the program in association with post-operative mortality rate and the beneficial factors of the program. In this study, 241 patients who participated in this program from August 2008 to September 2012 were reviewed. Fisher’s exact tests were applied to calculate p-values of categorical data. Out of 241, 11 patients were rejected because of their poor health condition for flight transportation to India, leaving 230 patients for analysis. The majority of patients were 1 to 4 years of age (57.8%), Malays (61.7%), from families of monthly household income less than RM 1,500 (86.5%) and with primary school-educated parents (86.5%). Patients could apply from any government hospital in Malaysia, but 34.8% of the patients were from the state of Johor. The region (Peninsular Malaysia and East Malaysia) of patients seeking pediatric cardiac services was significantly associated with race (p<0.001), low household income (p<0.001) and low education background of parents (p=0.004). The associations between the age group and diagnosis group (p=0.010) and between duration of hospitalization and outcome of medical management (p=0.013) were significant. Post-operative mortality rate was 1.7% (95% confidence interval, 0.5–4.4). In conclusion, the patients and the government were considered to have benefited from the PCP.
Key Words: Congenital Heart Disease, Pediatric Care Services, Pediatric Heart Program, Telemedicine, Malaysia
INTRODUCTION
According to Health Indicator 2007 by the Malaysian Department of Statistics, there were about 500,000 child deliveries in Malaysia in a year. Incidences of congenital heart disease (CHD) is estimated about 5,000 per year, of which two thirds will require a surgical intervention. Hence the number of children requiring surgery each year is about 2,000 to 3,000, which presents a unique challenge.1-4)
Currently, only the National Heart Institute and 2 other private hospitals are performing complex pediatric cardiothoracic surgeries. For certain cases, the waiting time is unacceptably long. The shortage of local pediatric cardiothoracic surgeons also compounds this delay. Due to high cost of cardiothoracic surgery in private hospitals, access to such services is limited for ordinary Malaysians. Consequently, some children have expired while waiting their turn for surgery.5-8)
To address these issues, the Cabinet of Malaysia have decided that the government will bear the cost of cardiothoracic surgery for poor Malaysian children undergoing surgery at Narayana Health Institute of Cardiac Sciences (NH), Bangalore, through the Medical Aid Fund, locally known as ‘Tabung Bantuan Perubatan’.5,6,9-11) The program was named the Pediatric Cardiothoracic Program (PCP), and started in 2008.
A world renowned hospital for cardiology and cardiothoracic services for adult and children12-17) afflicted with heart diseases, the NH has the capacity and capability to treat both local and international patients, as well as perform simple to complex surgeries using advanced, high tech equipment along with their skilled specialists, paramedics and supporting clinical and non-clinical personnel.18-20) A discounted rate that is much lower than those charged by Malaysian private hospitals has been offered by the NH to perform cardiothoracic surgeries for poor Malaysian children.5,6,21)
The government allocated a total of RM 2 million (USD 512,000) biannually for this program but additional will be provided if it surplus. Eligible can obtain the medical aid fund for the medical management and the number of patient enrollment is not limited for this program. The government only pays about RM 14,900 (USD 4,030) for the packaged services regardless of type of surgery, type of medication and duration of hospitalization, flight ticket, visa and other miscellaneous issues.6)
MediAssist4U Pvt. Ltd. (M4U) was appointed by the NH as the local agent and facilitator for the purpose of facilitating the surgery of children suffering from CHD at NH, on a non-profit basis. Prior to traveling to India, the patients are seen and counselled by M4U.6) The clinic uses its teleconferencing facilities for tele-consultation with the NH, tele-ECG and tele-echocardiography for diagnostic purposes.11,22) Once approved by the NH through the videoconferencing session, M4U makes all the required arrangements to enable the selected patients to travel to India for surgery. M4U also makes arrangements for the patients' parents or guardians to accompany them.23,24)
The purpose of this study is to study demographics characteristics of patients with CHD who sought operations at the NH, and further to evaluate the outcome of the program based on post-operative mortality.
MATERIALS AND METHODS
This study was conducted at M4U, a diagnostic center which evaluates the cardiac function of each patient prior to being referred to the NH for medical management. Data were collected from all patients potentially eligible for the surgery at the NH during the period from August 2008 to September 2012. The study subjects were 241 pediatric patients with cardiac-related problems who were referred from government hospitals in Malaysia, 11 of which were rejected as their health condition was too poor to board the plane to seek cardiac care in India. The remaining 230 patients were analyzed in this study. The medical records were collected using Clinical Management System software (MedexOne Global Pvt. Ltd., Kuala Lumpur) and also by reviewing patients’ medical files for details of the surgery.
Background factors which were taken into consideration were race, monthly household income and parents’ education background, while the outcome was accounted via referral from government hospitals, diagnosis group, duration of hospitalization and post-operative mortality. They were followed up for 24 months as a matter of routine. This information has been routinely collected to evaluate the PCP. This study was ethically approved by M4U.
The difference in the categorical data were examined by Fisher’s exact test, with 95% confidence intervals calculated based on a binomial distribution. Statistical Package for Social Science (SPSS) version 22.0 (IBM, Chicago, IL) was used for the calculation.
RESULTS
Socio-demographics characteristic of patients treated in Pediatric Cardiothoracic Program patients, August 2008 to September 2012.
The majority of the pediatric patients (53.9%) were male (Table 1). During the enrollment period, 52.5% of males and 64.2% of females were aged 1 to 4 years, for 57.8% of the total. Half of the patients (61.7%) were Malays followed by others (14.8%) which composed of mix minority ethnics group, and the least was made up by Chinese (10.4%). Most (86.5%) patients were from low income group with monthly household incomes of less than RM 1,500 (approximately $420). More than four fifths (86.5%) of the patients’ parents had not completed secondary education.
Table 1.
Socio-demographics characteristic of patients treated in Pediatric Cardiothoracic Program, August 2008 to September 2012
| Characteristics | Male | Female | Total | |||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |||
| Total | 124 | (100) | 106 | (100) | 230 | (100) | ||
| Age | ||||||||
| < 1 | 17 | (13.7) | 12 | (11.3) | 29 | (12.6) | ||
| 1 – 4 | 65 | (52.5) | 68 | (64.2) | 133 | (57.8) | ||
| 5 – 9 | 22 | (17.7) | 17 | (16.0) | 39 | (17.0) | ||
| 10 – 14 | 20 | (16.1) | 9 | (8.5) | 29 | (12.6) | ||
| Race | ||||||||
| Malay | 74 | (59.7) | 68 | (64.1) | 142 | (61.7) | ||
| Chinese | 15 | (12.1) | 9 | (8.5) | 24 | (10.4) | ||
| Indian | 14 | (11.3) | 16 | (15.1) | 30 | (13.0) | ||
| Others | 21 | (16.9) | 13 | (12.3) | 34 | (14.8) | ||
| Monthly household income a | ||||||||
| < RM 1,500 (< USD 420) | 106 | (85.5) | 93 | (87.7) | 199 | (86.5) | ||
| RM 1,500 – RM 3,000 (USD 420 - USD 840) | 18 | (14.5) | 13 | (12.3) | 31 | (13.5) | ||
| Parents’ education background | ||||||||
| Primary education | 106 | (85.5) | 93 | (87.7) | 199 | (86.5) | ||
| Secondary education | 14 | (11.3) | 12 | (11.3) | 26 | (11.3) | ||
| Tertiary education | 4 | (3.2) | 1 | (1.0) | 5 | (2.2) | ||
a Based on the data from Economic Planning Unit, Prime Minister’s Department of Malaysia, household income < RM1,500 is categorized as low income group.
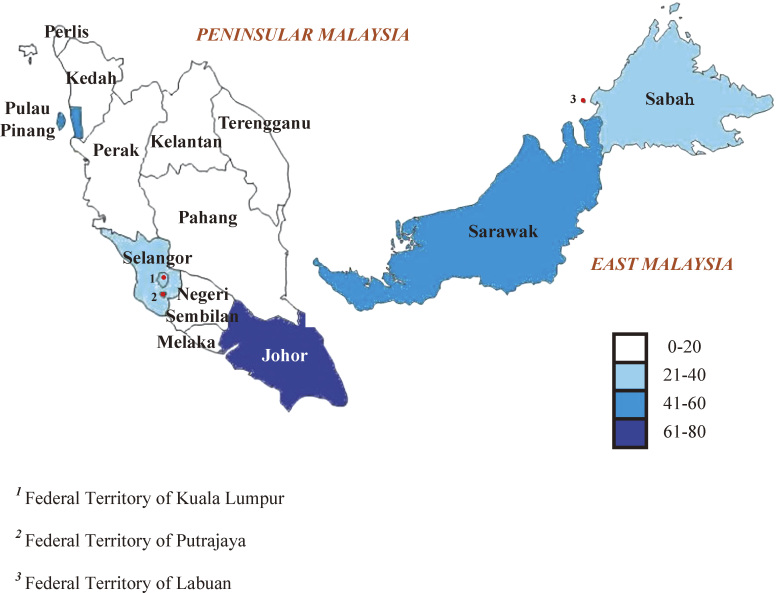
Volume of patients for Pediatric Cardiothoracic Program by state
Figure 1 explains the volume of patients for PCP by state. In Peninsular Malaysia, only 3 states, Pulau Pinang, Selangor (including the Federal Territory of Kuala Lumpur) and Johor, referred patients to M4U, while in East Malaysia both the states referred patients. Johor makes the largest proportions followed by Pulau Pinang and Sarawak; then Selangor and Sabah.
Fig. 1.
Volume of patients based on states for pediatric cardiothoracic program (PCP).
Characteristics of patients who were treated in Pediatric Cardiothoracic Program
Table 2 shows the factors associated with patient seeking cardiothoracic services in government hospitals. Among 230 patients, 149 (64.8%) sought cardiothoracic services in Peninsular Malaysia government hospitals, while 81 (35.2%) sought services in East Malaysia government hospitals. There was no significant association (p=0.129) between the region and gender. The associations of the region with age (p=0.014), race (p<0.001), monthly household income (p<0.001), and parents’ education background (p<0.005) were statistically significant.
Table 2.
Characteristics of patients who were treated in Pediatric Cardiothoracic Program
| Characteristics | Peninsular Malaysia | East Malaysia | p – value b | ||||
|---|---|---|---|---|---|---|---|
| N | (%) | n | (%) | ||||
| Total | 149 | (100) | 81 | (100) | |||
| Gender | |||||||
| Male | 86 | (57.7) | 38 | (46.9) | 0.129 | ||
| Female | 63 | (42.3) | 43 | (53.1) | |||
| Age | |||||||
| < 1 | 25 | (16.7) | 4 | (4.9) | 0.014 | ||
| 1 – 4 | 88 | (59.1) | 45 | (55.6) | |||
| 5 – 9 | 21 | (14.1) | 18 | (22.2) | |||
| 10 – 14 | 15 | (10.1) | 14 | (17.3) | |||
| Race | |||||||
| Malay | 105 | (70.5) | 37 | (45.7) | <0.001 | ||
| Chinese | 24 | (16.1) | 0 | (0) | |||
| Indian | 18 | (12.1) | 12 | (14.8) | |||
| Others | 2 | (1.3) | 32 | (39.5) | |||
| Monthly household income a | |||||||
| < RM 1500 (< USD 420) | 121 | (81.2) | 78 | (96.3) | <0.001 | ||
| RM 1500 – RM 3000 (USD 420 - USD 840) | 28 | (18.8) | 3 | (3.7) | |||
| Parents’ education background | |||||||
| Primary education | 121 | (81.2) | 78 | (96.3) | 0.004 | ||
| Secondary education | 23 | (15.4) | 3 | (3.7) | |||
| Tertiary education | 5 | (3.4) | 0 | (0) | |||
Government hospitals: Hospital Sultan Aminah Johor Bahru, Hospital Pulau Pinang, Hospital Kuala Lumpur, and Hospital Serdang were grouped under Peninsular Malaysia, while Hospital Umum Sarawak and Hospital Likas Sabah were grouped under East Malaysia.
a Based on the data from Economic Planning Unit, Prime Minister’s Department of Malaysia, household income < RM1,500 is categorized as low income group.
b Fisher’s exact test
Diagnosis according to age group
As shown in Table 3, more than half (56.1%) of the 230 patients were diagnosed with left to right shunt defects followed by 97 patients with cyanotic defects (42.2%), and the least was 4 patients with obstructive defects (1.7%). There was a statistically significant association (p=0.010) between diagnosis category and age.
Table 3.
Diagnosis according to age group
| Age | Cyanotic | Left to right shunt | Obstructive | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | ||||
| Total | 97 | (100) | 129 | (100) | 4 | (100) | 230 | (100) | |||
| < 1 | 9 | (9.3) | 16 | (12.4) | 4 | (100.0) | 29 | (12.6) | |||
| 1 – 4 | 56 | (57.7) | 77 | (59.7) | 0 | (0.0) | 133 | (57.8) | |||
| 5 – 9 | 19 | (19.6) | 20 | (15.5) | 0 | (0.0) | 39 | (16.9) | |||
| 10 – 14 | 13 | (13.4) | 16 | (12.4) | 0 | (0.0) | 29 | (12.6) | |||
The details of diagnosis for each diagnostic category are as follows; Tetralogy of Fallot, mitral regurgitation, double outlet right ventricle, and transposition of great arteries for “Cyanotic”, ventricular septal defect and atrial septal defect for “Left to right shunt”, and coarctation of aorta, aortic stenosis, and pulmonary stenosis for “Obstructive”. Mitral regurgitation was put into cyanotic group based on the final outcome of the condition like mitral prolapse or cardiac failure which will lead to cyanosis.
A Fisher’s exact test for the 3 x 4 table was significant (p=0.010).
Outcome of medical management according to duration of hospitalization
Table 4 presents the outcomes of the medical management. There were 226 (98.3%) patients alive for 24 months after surgery. The outcome of medical management and duration of hospitalization showed statistically significant difference (p=0.013). Post-surgery, 4 patients expired (1.7%, 95% confidence interval, 0.5–4.4). In 2014, 224 (97.4%) patients were alive after medical management, which also shows statistical significance (p<0.001) in relation to medical management.
Table 4.
Outcome of medical management according to duration of hospitalization
| Duration of hospitalization (days) | Alive | Expired | |||
|---|---|---|---|---|---|
| N | (%) | n | (%) | ||
| Total | 226 | (100) | 4 | (100) | |
| Short (4–14) | 133 | (50.0) | 1 | (25.0) | |
| Middle (15–24) | 80 | (35.4) | 0 | (0.0) | |
| Long (25–34) | 33 | (14.6) | 3 | (75.0) | |
A Fisher’s exact test for the 2 × 3 table was significant (p=0.013).
DISCUSSION
This study showed that the largest proportion (61.7%) of patients was Malays, understandable as they are the most populous race in Malaysia. Those aged 1–4 years (57.8%) were the largest proportion among all age groups. This was due to good medical outcomes after medical management, as most of the pediatric cardiothoracic surgery were best done when the patient was still young, as they could enjoy the benefit of the repair at an early age.
Majority of patients were from Peninsular Malaysia (64.8%), but from only 3 states and 1 Federal Territory. The patients from East Malaysia were from both states. In Malaysia, there are 132 governmental hospitals and medical care for CHD is almost free. But currently only 7 government hospitals, 5 in Peninsular Malaysia and 2 in East Malaysia, are capable of providing almost comprehensive pediatric cardiac services; complicated cases were referred to National Heart Institute. Parents prefer to go to high-level hospitals directly, rather than being referred by government hospital primary care physicians to the one with a pediatric cardiologist. Thus parents have to travel to government hospitals which might be located outside of their area of residence or state to seek pediatric cardiac services for their children which makes accessibility and availability a great issue. Since PCP is first of its kind in Malaysia, thus some pediatric cardiologists are unsure of the success of this program. These were likely the reason that patients came from limited area. Subjects of the study came from families with low monthly household incomes and poor education of parents, a vulnerable group in Malaysia.10) Pediatric cardiac services in National Heart Institute offers subsidies for them through certain funds, but the waiting time is unacceptably long, especially for complex cases. Due to the high cost of pediatric cardiac services in private hospitals and not being covered by medical insurance, parents opt out this option.5,6) Lack of finances and poor knowledge regarding the health condition of their children creates an environment for parents to be dependent on government hospitals.
The diagnosis of pediatric cardiac diseases had a strong association with age (p=0.010). Capability to diagnose and treat at early age reduces the frequency of complications, improving the quality of life of the child.9) Children are less worried about health than adults; in other words, they are mentally stronger. Hence, the post-surgery recovery occurs at a faster pace.5) Almost 56.1% of patients are diagnosed with left to right shunt and it is of utmost importance to repair it as soon as possible, because if the shunt becomes right to left, it complicates the repairing process or in some cases it may be beyond repair.
The outcome of the medical management had a significant association with the duration of hospitalization (p=0.013); longer stays had a worse prognosis. Out of 230 subjects, 4 (1.7%) patients expired after post-operation. In 2014, all the patients’ parents were contacted to inquire about the status of their children, which found another 2 (0.9%) out of the 226 patients expired in the course 24 months after operation.
The price offered for PCP is much cheaper compared to the United States where the estimated cost for an average infant with any CHD is about USD 23,000, and much higher in case of severe CHD.25) In the event of the expiry of a patient, the NH along with M4U make arrangements to bring the deceased back to Malaysia with no additional cost the government or parents.6) Through PCP, the government save great amount of resources as the cost is 10 fold higher in Malaysia. Therefore, neither the patients’ parents nor the government are financially burdened by this issue. The patients had shorter duration of hospitalization, and the overall mortality rate was 2.6%, which lower than in the United States (4.6%) and the United Kingdom (4.0%).26,27)
Post PCP feedback from the patients’ parents was good; in addition to being happy with the medical management provided to the children and the hospitality of medical professionals and medical staffs towards them and their children, they also can see their children being equal as other normal children as well. With the power of technology, distance is not an issue with the usage of telemedicine, consequently allowing ordinary doctors to do extraordinary things.
Although the National Heart Institute has grown tremendously and the government is working to set up 6 regional cardiac centers to provide complex pediatric care service, still the backlog of patients and long waiting times for medical management is ongoing and this should not be a burden borne by the patients.
There were several limitations to this study. Firstly, the study was conducted with a small sample size, thus the respondents cannot be assumed to be representatives of the whole of patients with CHD. Secondly, the patients in this study were from 5 states and 1 Federal Territory out of 13 states and 3 Federal Territories, hence hindering the ability of the study to provide a clear picture of CHD cases in Malaysia.
In conclusion, the PCP has benefited patients from the vulnerable group for 5 years. PCP has also overcome the situation where parents of children, especially from the vulnerable group, will not beg for pediatric care services, and this has served as the gateway for them to obtain help. Hence, the government should continue this program to benefit the citizens, especially those from vulnerable and middle income group, while waiting for our own set up to be up and running.
ACKNOWLEDGEMENTS
We wish to thank the coordinators and other staff who helped us in data collection, and all patients and parents, pediatric cardiologists, doctors, nurses, supporting clinical and non-clinical personnel and all those who were part of the PCP.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interests.
REFERENCES
- 1).Health Informatics Centre Planning and Development Division. Indicators for monitoring and evaluation of strategy health for all. In: Heath Indicator 2007. pp.54, 2007, Ministry of Health Malaysia. http://www.moh.gov.my/images/gallery/publications/md/hi/hi_2007.pdf (assessed on November 5, 2014).
- 2).Health Informatics Centre Planning and Development Division. Health facts 2007. 2008, Ministry of Health Malaysia. http://www2.moh.gov.my/images/gallery/stats/heal_fact/ health_facts_2007.pdf (assessed on November 5, 2014).
- 3).Health Informatics Centre Planning and Development Division. Annual report 2007. pp.75–76, 2008, Ministry of Health Malaysia. http://www.moh.gov.my/images/gallery/ publications/md/ar/2007-2.pdf (assessed on November 5, 2014).
- 4).Wong SL, Muhammad IHI. Where and why 5000 children in Malaysia are dying every year? In: Under Five Death in Malaysia 1993–2003. pp.20–46, 2008, Ministry of Health Malaysia. http://www.crc.gov.my/wp-ontent/uploads/documents/report/StudyOnUnder5 DeathsinMsia_1993–2003.pdf (assessed on February 14, 2015).
- 5).Sharifah AIM. Paediatric cardiac surgery with limited resources. Malaysia J Paediatr Child Health, 2011; 17: 34.
- 6).Medical Development Division. Guidelines on the management of children with congenital heart diseases for cardiothoracic surgery in Narayana Hrudayalaya Institute of cardiac sciences (NH), Bangalore, India. 2007, Ministry of Health Malaysia. http://www2.moh.gov.my/attachments/1909 (assessed on November 28, 2014).
- 7).Adeeb SM, Leman H, Sallehuddin A, Yakub A, Awang Y, Alwi, M. Coarctation of aorta repair at the National Heart Institute (1983–1994). Med J Malaysia, 2004; 59: 11–14. [PubMed]
- 8).Indra G, Terrence T, Fon EN, Thian LS. Clinical characteristics and mortality risk prediction in critically ill children in Malaysian Borneo, Singapore Med J, 2014; 55: 261–265. [DOI] [PMC free article] [PubMed]
- 9).Goh AY, Abdel LMA, Lum LC, Abu BMN. Outcome of children with different accessibility to tertiary pediatric intensive care in a developing country: a prospective cohort study. Intensive Care Med, 2003; 29: 97–102. [DOI] [PubMed]
- 10).Department of Statistics Malaysia. Report on Household Income Expenditure Survey in Malaysia 2009/10. pp.1–23, 2011, Government of Malaysia. http://catalog.ihsn.org/ index.php/catalog/5430/download/65754 (assessed on January 21, 2015).
- 11).Sangeeta S, Ira AP, Steven AK, Helen K, Susan H, Gary LS, Wyman WL. Screening fetal echocardiography by telemedicine: Efficacy and community acceptance. J Am Soc Echocardiogr, 2003; 16: 202–208. [DOI] [PubMed]
- 12).Aladeen MA, Weaam FJT, Ayad AH, Rasha MA, Hazar NR, Luke F. Narayana Hrudayalaya cardiac care hospital for the poor: Leadership case study analysis and key lessons for Jordan. Eur Sci J, 2014; 10: 474–484.
- 13).Khanna, Tarun, Kasturi VR, Merlina Mn. Narayana Hrudayalaya Heart Hospital: Cardiac Care for the Poor (A). In: Harvard Business School Case Study. pp.78–101, 2005, Harvard Business School.
- 14).Khanna, Tarun, Tanya B. Narayana Hrudayalaya Heart Hospital: Cardiac Care for the Poor (B). In: Harvard Business Supplement. pp.402–407, 2011, Harvard Business School.
- 15).Richman BD, Udayakumar K, Mitchell W, Schulman KA. Lessons from India in Organizational Innovation: A Tale of Two Heart Hospitals. Health Affairs, 2008; 27: 1260–1270. [DOI] [PubMed]
- 16).Prabakar K, Sunita M. Case study: Healthcare for All: Narayana Hrudayalaya, Bangalore. In: Growing Inclusive Markets. pp.4–15, 2007, United Nations Development Programme. http://growinginclusivemarkets.org/media/cases/India_Narayana_2008.pdf. (assessed on March 21, 2015).
- 17).International partnership for innovative healthcare delivery. Narayana Health. In: International Partnership for Innovative Healthcare Delivery. pp.1–10, 2013, Innovation in Health. http://innovationsinhealthcare.org/Narayana%20profile%202013.pdf (assessed on March 21, 2015).
- 18).Geeta A. The Henry Ford of Heart Surgery. In: The Wall Street Journal. 2009, The Wall Street. http://www.wsj.com/articles/SB125875892887958111 (assessed on March 21, 2015).
- 19).Chris M. ‘Production line’ heart surgery. In: BBC News (Delhi). 2010, BBC News. http://www.bbc.com/news/health-10837726 (assessed on March 21, 2015).
- 20).Neelima MB. The World’s Largest Heart Factory. In: Forbes India, 2009, Forbes. http://forbesindia.com/article/beyond-business/the-worlds-largest-heart-factory/1442/1 (assessed on March 21, 2015).
- 21).Knowledge @ Wharton. Narayana Hrudayalaya: A Model for Accessible, Affordable Health Care? In: Innovation. 2010, University of Pennsylvania. http://knowledge.wharton.upenn.edu/article/narayana-hrudayalaya-a-model-for-accessible-affordable-health-care/ (assessed on March 21, 2015).
- 22).Weatherburn G. The design of specialist paediatric cardiology telemedicine services to meet the needs of patients. J Telemed Telecare, 2010; 16: 211–214. [DOI] [PubMed]
- 23).Krishnan A, Fuska M, Dixon R, Sable CA. The evolution of pediatric tele-echocardiography: 15-year experience of over 10,000 transmissions. Telemed J E Health, 2014; 20: 681–686. [DOI] [PubMed]
- 24).Maheshwari S, Animasahun BA, Njokanma OF. International patients with congenital heart disease: what brings them to India? Indian Heart J, 2012; 64: 50–53. [DOI] [PMC free article] [PubMed]
- 25).Boulet SL, Grosse SD, Riehle-Colarusso T, Correa VA. Health care costs of congenital heart defects. In: Congenital Heart Defects: From Origin to Treatment, edited by Wyszynski DF, Correa VA and Graham TP. pp.493–501, 2010, New York: Oxford University Press, Inc.
- 26).Welke KF, Diggs BS, Karamlou T, Ungerleider RM. Comparison of pediatric cardiac surgical mortality rates from national administrative data to cotemporary clinical standards. Ann Thorac Surgery, 2009; 87: 216–222. [DOI] [PubMed]
- 27).Brown KL, Crowe S, Franklin R, McLean A, Cunningham D, Barron D, Tsang V, Pagel C, Utley M. Trends in 30-day mortality rate and case mix for paediatric cardiac surgery in the UK between 2000 and 2010. Open Heart, 2015; 2: e000157. [DOI] [PMC free article] [PubMed]