ABSTRACT
The purpose of this study is to examine the feasibility of single-incision laparoscopic percutaneous extraperitoneal closure (LPEC) for incarcerated inguinal hernia (IIH) repair. 6 single-incision LPEC procedures were performed for IIH repair and 60 procedures were performed for reducible inguinal hernia (RIH) in the same period of time in one hospital. The laparoscope and one pair of grasping forceps were placed through the same umbilical incision. In IIH repair, the herniated organ was gently pulled using the grasping forceps with external manual pressure. If it was difficult to reduce the herniated organ with one pair of forceps, another pair of forceps were inserted through a multi-channel port without extending the umbilical incidion. Using the LPEC needle, the hernia orifice was closed extraperitoneally. We performed a retrospective analysis to compare the outcomes of single-incision LPEC for IIH repair or reducible inguinal hernia. All procedures were completed by single-incision without open conversion. A multi-channel port with another pair of forceps was needed in three cases. The operation time and the length of stay were significantly longer with IIH repair than with RIH repair. There were no major complications and there was no evidence of early recurrence in any patient. In conclusion, single-incision LPEC with a multi-channel port is feasible and safe for IIH repair.
Key Words: pediatrics, incarcerated inguinal hernia, laparoscopic percutaneous extraperitoneal closure, reduced port surgery
INTRODUCTION
There are numerous techniques for laparoscopic inguinal herniorrhaphy. Laparoscopic percutaneous extraperitoneal closure (LPEC), as introduced by Takehara et al.,1) is one of the most simple and reliable methods in children. To further reduce invasiveness and achieve better cosmetic results, our group introduced single-incision LPEC (SILPEC), and we have previously reported its safety and feasibility.2) In this technique, the hernia orifice is percutaneously closed by suturing, under laparoscopic assistance using a pair of grasping forceps inserted through the same umbilical incision as the laparoscope. However, there are still several challenges to performing SILPEC for incarcerated inguinal hernia (IIH) repair. In IIH repair, it may be necessary to make an additional incision for reduction, and surgical procedures may be needed to repair the damaged herniated organ. Furthermore, the safety and feasibility of SILPEC for IIH repair are still unclear.
In this report, we performed a retrospective analysis to compare the outcomes of SILPEC for IIH repair or reducible inguinal hernia in the same period of time in one hospital. We present our preliminary results and review the literature about laparoscopic IIH repair.
PATIENTS AND METHODS
Patients
We reviewed 66 patients who underwent SILPEC for inguinal hernia repair at our hospital between April 2014 and November 2014. Presurgical manual reduction of the herniated organs was unsuccessful in six of these patients. Sixty patients with a reducible inguinal hernia and four patients with an IIH containing an ovary or omentum underwent elective surgery. Two patients with an IIH containing the intestine underwent emergency surgery soon after an unsuccessful manual reduction procedure. This study was approved by the Ethics Committee at our hospital.
Surgical procedures
Regardless of the herniated organs, all surgical procedures were started using the same technique, which was described by our group in a previous report.2) Under general anesthesia, the patients were placed in a supine position. Through a 1.0–1.5 cm vertical transumbilical incision, a 3 mm port was placed using an open technique for a 3 mm, 30° laparoscope. The abdomen was insufflated to 8–10 mmHg. One pair of 3 mm grasping forceps was inserted through the same transumbilical incision as the laparoscope, with a different entrance.
In IIH repair, the herniated organ was gently pulled using the grasping forceps under external manual pressure. If it was difficult to reduce the hernia using this technique, a wound retractor (Alexis Wound Retractor XS; Applied Medical, Rancho Santa Margarita, CA) was inserted through the umbilicus with remaining the same skin incision and only extending the fascia incision, and a silicon cap (Free Access; TOP Corporation, Tokyo, Japan) was mounted for use as a multi-channel port. Another pair of forceps was inserted through the multi-channel port. The herniated organ and the rim of the hernia orifice were pulled using both pairs of grasping forceps. If the herniated organ adhered to the hernia sac, an energy device was used to dissect the hernia. After successful reduction, the viability and mechanical damage of the reduced organ were assessed laparoscopically.
The hernia orifices were corrected using the same technique in all patients regardless of the presence/absence of peritoneal edema around the internal inguinal ring. A 19-gauge LPEC needle with nonabsorbable suture material was inserted into the inguinal region. Using the LPEC needle and the forceps, the hernia orifice was closed extraperitoneally with circuit suturing without leaving a peritoneal gap. Bilateral closure was performed in patients with a contralateral patent processus vaginalis.
Data analysis and statistical considerations
Data were retrieved from our institutional database and were reviewed retrospectively. The study ended at September 2015, and the status of each patient at that time was recorded. The data were compared between patients with an IIH and patients with a reducible inguinal hernia. Statistical analyses were performed using the χ2 test for categorical variables and the Mann–Whitney U test for continuous variables. Values of P < 0.05 were considered statistically significant.
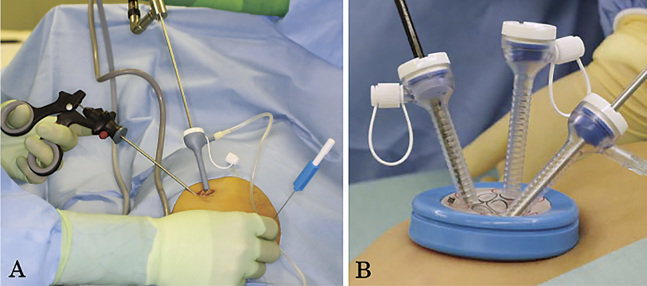
Fig. 1.
(A) The port and grasping forceps are inserted through a single transumblical incision. (B) If reduction was difficult using one pair of grasping forceps, a multi-channel port was inserted through the umbilical incision without extending the skin incision.
RESULTS
All the procedures were completed by SILPEC without conversion or requiring an additional skin incision. The characteristics of patients and complications are presented in Table 1. Reducible inguinal hernia repair and IIH repair were comparable in terms of the patients’ age, body weight, sex ratio, side of the hernia, and follow-up period. However, the operation time and the time from operation to discharge were significantly longer for IIH repair than for reducible inguinal hernia repair. There were no major complications and there was no evidence of early recurrence in any patient. The parents of all patients were satisfied with the cosmetic appearance of the resulting scar.
Table 1.
Characteristics of the patients with an inguinal hernia
| Reducible hernia n = 60 |
Incarcerated hernia n = 6 |
P-value | |
|---|---|---|---|
| Age (mo) | 54.5 (4–132) | 11 (5–104) | 0.07 |
| Body weight (kg) | 17.3 (5.8–36.4) | 8.6 (6.6–38.2) | 0.22 |
| Sex (male), n (%) | 28 (46.7%) | 3 (50%) | 0.88 |
| Side of hernia, n (%) | |||
| Unilateral | 41 (68.3%) | 3 (50.0%) | 0.39 |
| Contralateral patent processus vaginalis | 15 (25%) | 2 (33.3%) | 0.64 |
| Bilateral | 4 (6.7%) | 1 (16.7%) | 0.39 |
| Total operating time (min) | 34 (19–65) | 57 (26–75) | 0.014* |
| Pneumoperitoneum time (min) | 18 (5–52) | 43 (14–42) | 0.008* |
| Conversion, n (%) | 0 (0%) | 0 (0%) | |
| Hospital discharge (postoperative day) | 1 (1–1) | 1.5 (1–5) | < 0.001* |
| Follow-up time (mo) | 12 (10–17) | 12 (10–14) | 0.29 |
| Complications, n | |||
| Recurrence | 0 | 0 | |
| Vas transection | 0 | 0 | |
| Postoperative testicular atrophy | 0 | 0 | |
| Scrotal swelling | 0 | 1 | |
| Postoperative paresis of intestine | 0 | 2 |
Values are presented as the n (%) or median (range).
* P < 0.05
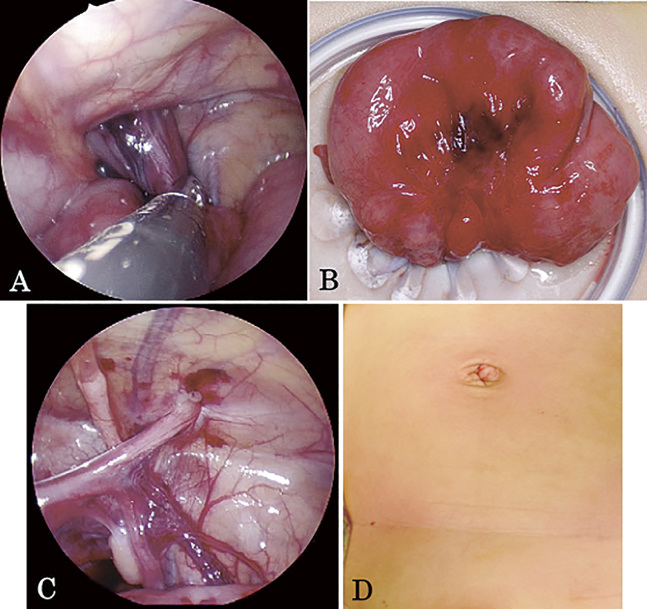
The characteristics of IIH repair are summarized in Table 2. The herniated organs were an ovary (n = 2), omentum (n = 2), sigmoid colon (n = 1), and small intestine (n = 1). In both cases of herniated ovary, the prolapsed ovary was reduced without difficulty using one pair of grasping forceps. In both cases of herniated omentum, a multi-channel port and a second pair of forceps were needed for reduction. In one of these cases in which the omentum adhered to the hernia sac, laparoscopic coagulating shears were needed for tissue dissection. In this case, the scrotum was swelling in 2 weeks after surgery. In both cases of herniated intestine, the prolapsed intestine was reduced using one pair of grasping forceps under external manual pressure to keep a laparoscopic view without disturbing bowel dilatation. Although in both of these cases the reduced intestines were congested and appeared to be nonviable, the damaged segment improved gradually in the peritoneal cavity. In the patient with a herniated small intestine, however, the intestinal serosa was injured during reduction. The wound retractor was inserted and the damaged intestine could be exteriorized and repaired without an additional skin incision. Both patients developed postoperative paresis of the intestine and oral intake started 2 days after surgery.
Table 2.
Characteristics of the individual patients with incarcerated inguinal hernia
| Case | Organ | Side | Age (mo) | Weight (kg) | Operation time (min) | Multi-channel port used | Discharge (POD) | Complication |
|---|---|---|---|---|---|---|---|---|
| 1 | Ovary | R | 5 | 7.6 | 26 | No | 1 | |
| 2 | Ovary | B | 5 | 6.6 | 47 | No | 1 | |
| 3 | Omentum | L | 57 | 20.8 | 55 | Yes | 2 | Scrotal swelling |
| 4 | Omentum | B* | 104 | 38.2 | 59 | Yes | 1 | |
| 5 | Sigmoid colon | L | 13 | 9.4 | 58 | No | 5 | Intestinal paresis |
| 6 | Small intestine | B* | 9 | 7.7 | 75 | Yes | 4 | Intestinal paresis |
POD: postoperative day; R: right; B: bilateral; L: left.
*Contralateral patent processus vaginalis was observed during the operation.
Fig. 2.
Case 6. (A) The herniated small intestine was reduced using one pair of grasping forceps and external manual pressure. (B) The herniated intestine was exteriorized and the injured serosa was repaired. (C) The hernia orifice was closed without leaving a peritoneal gap. (D) The parents of the patient were satisfied with the cosmetic appearance of the resulting scar.
DISCUSSION
Although there are numerous techniques for laparoscopic inguinal herniorrhaphy, we previously reported that SILPEC produced excellent cosmetic outcomes.2) Furthermore, we consider that SILPEC is one of the most reliable methods because of the use of surefire sutures to completely enclose the hernia orifice without leaving a peritoneal gap, independent of any division of the distal sac.
The comparative studies of laparoscopic incarcerated inguinal hernia (unsuccessful preoperative manual reduction) repair in children were reviewed (Table 3).3-9) Kaya et al. reported that the laparoscopic approach is easier than an open approach because intraabdominal carbon dioxide insufflation widens the internal inguinal ring, which facilitates reduction.9) Esposito et al. reported three advantages of the laparoscopic approach: edematous cord structures are not touched, the reduction is performed under direct vison, and it is possible to inspect the herniated organ.5) To date, however, there have been only one reports regarding reduced port surgery for IIH repair. Zhou et al. reported an approach using two intraumbilical incisions in which the anterolateral part of the internal inguinal ring was cut if reduction was difficult with one pair of forceps.3) However, at least two pairs of forceps are needed to fully confirm whether or not the incarcerated organ is reducible. Furthermore, to avoid recurrence, it is important to keep the hernia orifice without injuring the peritoneum around the inguinal ring. On the assumption that the greatest extent of reduction is made possible by pulling the herniated organ and dilating the rim of the hernia using two pairs of forceps without cutting the inguinal ring, we used a wound retractor and a silicon cap for a multi-channel port if the reduction was difficult with one pair of forceps.
Table 3.
The comparative studies of laparoscopic incarcerated inguinal hernia (unsuccessful preoperative manual reduction) repair in children
| Zhou X | Mishra PK | Esposito C | Chan KW | Shalaby R | Kaya M | |
|---|---|---|---|---|---|---|
| (2014) | (2014) | (2013) | (2011) | (2007) | (2006) | |
| n=17 | n=4 | n=25 | n=5 | n=80 | n=29 | |
| Age (mo) | 15 (8–30) | NA | 18 (1–96) | 22 (4–144) | NA | 10 (0.8–84) |
| Sex (male), n (%) | 15 (88.2%) | NA | 15 (60%) | NA | NA | 23 (79%) |
| Side of hernia (right), n (%) | 11 (73%) | NA | 19 (76%) | NA | NA | 20 (69%) |
| Contralateral patent processus vaginalis | 2 (13%) | NA | NA | 1 (20%) | NA | NA |
| Organ | bowl and ovary | bowl (n=3), appendix(n=1) | ovary (n=9), bowl (n=9) | bowl (n=3), omentum(n=1) | bowl and ovary | bowl and ovary |
| omentum(n=5), appendix (n=2) | Meckel diverticulum (n=1) | |||||
| Necrosis of herniated organ, n (organ) | 0 | 1 (appendix) | 0 | 1 (Meckel diverticulum) | 0 | 0 |
| The number of ports | 1–2(transumblical) | 3 | 3 | 3 | 2 | 3 |
| Total operating time (min) | 30 (25–40) | NA | 30 (18–41) | 90 (20–145) | NA | NA |
| Conversion, n (%) | 0 | 0 | 0 | 0 | 0 | 0 |
| Major Complications | none | NA | reccurence (n=1) | none | none | none |
Values are presented as the n (%) or median (range).
NA: not available
This report includes six cases of IIH repair by SILPEC. All of the procedures were completed without conversion or making an additional skin incision. We could reduce all of the ovaries and intestines using only one pair of grasping forceps and external manual pressure. The ovaries, in particular, were reduced relatively easily. Takehara et al. reported the efficacy of LPEC for irreducible ovarian hernias, and found that 78.6% (11/14) of cases could be corrected by laparoscopic methods only.10) In our report, both cases of herniated omentum were difficult to reduce with one pair of forceps, and required a multi-channel port. The herniated omentum sometimes adheres to the distal sac, and it is important to deal with such cases appropriately in order to prevent scrotal swelling. IIH containing intestinal tissue is a good indication for laparoscopic repair because the herniated intestine, although it may seem nonviable, might recover some time after reduction under laparoscopic inspection. Our technique using a wound retractor allowed us to exteriorize the damaged intestine without making an additional skin incision, because the pediatric abdominal wall is flexible and many intestinal IIHs occur during infancy. In the previous literatures, however, the herniated gangrenous organs which could be reduced laparoscopicsally were only appendix and Meckel diverticulum.4,6) Future studies should examine whether it is possible to reduce gangrenous and swollen bowel tissue using laparoscopic procedures only.
Sngle-incision LPEC with a multi-channel port is a potentially safe and feasible procedure for IIH repair. There were no major complications and no evidence of recurrence in the early postoperative period. However, a larger number of patients and a longer follow-up time are needed to confirm the advantages and the disadvantages of this technique.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
REFERENCES
- 1).Takehara H, Yakabe S, Kameoka K. Laparoscopic percutaneous extraperitoneal closure for inguinal hernia in children: clinical outcome of 972 repairs done in 3 pediatric surgical institutions. J Pediatr Surg, 2006; 41: 1999–2003. [DOI] [PubMed]
- 2).Uchida H, Kawashima H, Goto C, Sato K, Yoshida M, Takazawa S, Iwanaka T. Inguinal hernia repair in children using single-incision laparoscopic-assisted percutaneous extraperitoneal closure. J Pediatr Surg, 2010; 45: 2386–2389. [DOI] [PubMed]
- 3).Zhou X, Peng L, Sha Y, Song D. Transumbilical endoscopic surgery for incarcerated inguinal hernias in infants and children. J Pediatr Surg, 2014; 49: 214–217. [DOI] [PubMed]
- 4).Mishra PK, Burnand K, Minocha A, Mathur AB, Kulkarni MS, Tsang T. Incarcerated inguinal hernia management in children: ‘a comparison of the open and laparoscopic approach’. Pediatr Surg Int, 2014; 30: 621–624. [DOI] [PubMed]
- 5).Esposito C, Turial S, Alicchio F, Enders J, Castagnetti M, Krause K, Settimi A, Schier F. Laparoscopic repair of incarcerated inguinal hernia. A safe and effective procedure to adopt in children. Hernia, 2013; 17: 235–239. [DOI] [PubMed]
- 6).Chan KW, Lee KH, Tam YH, Sihoe JD, Cheung ST, Mou JW. Laparoscopic inguinal hernia repair by the hook method in emergency setting in children presenting with incarcerated inguinal hernia. J Pediatr Surg, 2011; 46: 1970–1973. [DOI] [PubMed]
- 7).Nah SA, Giacomello L, Eaton S, de Coppi P, Curry JI, Drake DP, Kiely EM, Pierro A. Surgical repair of incarcerated inguinal hernia in children: laparoscopic or open? Eur J Pediatr Surg, 2011; 21: 8–11. [DOI] [PubMed]
- 8).Shalaby R, Shams AM, Mohamed S, el-Leathy M, Ibrahem M, Alsaed G. Two-trocar needlescopic approach to incarcerated inguinal hernia in children. J Pediatr Surg, 2007; 42: 1259–1262. [DOI] [PubMed]
- 9).Kaya M, Hückstedt T, Schier F. Laparoscopic approach to incarcerated inguinal hernia in children. J Pediatr Surg, 2006; 41: 567–569. [DOI] [PubMed]
- 10).Takehara H, Hanaoka J, Arakawa Y. Laparoscopic strategy for inguinal ovarian hernias in children: when to operate for irreducible ovary. J Laparoendosc Adv Surg Tech A, 2009; 19: 129–131. [DOI] [PubMed]