Abstract
Introduction
Trauma center care has been associated with improved mortality. It is not known if access to trauma center care is also associated with reduced readmissions. We hypothesized that receiving treatment at a trauma center would be associated with improved care and therefore would be associated with reduced readmission rates.
Methods
We conducted a retrospective analysis of all hospital visits in California using the Office of Statewide Health Planning and Development Database from 2007–2008. All hospital admissions and emergency department visits associated with injury were longitudinally linked. Regions were categorized by whether or not they had trauma centers. We excluded all patients younger than 18 years of age. We performed univariate and multivariate regression analyses to determine if readmissions were associated with patient characteristics, length of stay for initial hospitalization, trauma center access, and triage patterns.
Results
A total of 211,504 patients were included in the analysis. Of these, 5,094 (2%) died during the index hospitalization. Of those who survived their initial hospitalization, 79,123 (38%) experienced one or more readmissions to any hospital within one year. The majority of these were one-time readmissions (62%) but 38% experienced multiple readmissions. Over 67% of readmissions were unplanned and 8% of readmissions were for a trauma. After controlling for patient variables known to be associated with readmissions, primary triage to a trauma center was associated with a lower odds of readmission (OR 0.89, p<0.001). The effect of transport to a trauma center remained significantly associated with decreased odds of readmission at one year (OR 0.96, p<0.001).
Conclusion
Readmissions after injury are common and are often unscheduled. While patient factors play a role in this, care at a trauma center is also associated with decreased odds for re-admission, even when controlling for severity of injury. This suggests that the benefits of trauma center care extend beyond improvements in mortality to improved long-term outcomes.
Keywords: Trauma, Triage, Readmissions, Outcomes
Introduction
Trauma center care is associated with improved mortality for severely-injured patients.1,2 However, the use of mortality as the only metric to assess the benefit of trauma systems may not fully capture the value that trauma systems afford the population. Non-fatal outcomes are increasingly being used as measurements of healthcare system performance. One of these metrics, the hospital readmission rate, is directly tied to reimbursement for certain conditions. The Centers for Medicare & Medicaid Services (CMS) began using readmission rates as a publicly reported quality indicator in 2012. As required by the Affordable Care Act and the Hospital Readmissions Reduction Program, CMS reduces payments to inpatient prospective payment system (IPPS) hospitals with excess readmissions for condition such as pneumonia, myocardial infarction, and heart failure.
There has been a recent focus on factors associated with readmission after trauma. 3–6 However, most of the work has focused on patient-level risk factors associated with unplanned readmissions in a specific cohort (e.g. elderly patients) rather than readmissions as a quality metric to evaluate trauma center care. Readmission rates have not been used to measure the value of trauma system care nor have they been applied to trauma hospitals in the United States. To evaluate whether trauma center care is associated with decreased readmission rates, we used a population-based longitudinal database of all patients admitted to all non-federal, acute care hospitals in California. We hypothesized that readmission rates would be lower for patients who were treated in trauma centers versus non-trauma centers.
METHODS
Data source and linkage
Non-public data for all hospital discharges (Patient Discharge Data, PDD) and Emergency Department (ED) visits in the state of California were obtained from the California’s Office of Statewide Health Planning and Development Database (OSHPD)7 for the period between January 1, 2007, and December 31, 2008. These years were selected as mortality data in OSHPD was available through 2009. Mortality was determined using the linked ED and PDD/Vital Statistics data provided by OSHPD. This comprehensive dataset allowed us to capture all readmissions to any hospital such that an admission to a different hospital after the initial discharge would be captured. Information on hospital characteristics was derived from the OSPHD State Utilization Data File of Hospitals. Trauma center status was confirmed manually for each hospital for each year by comparing to California Emergency Medical Information System (CEMSIS) data and individual hospitals’ websites.
Hospitalizations associated with a primary diagnosis of injury were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes (see “Inclusion/Exclusion Criteria” below for more information). These admissions were linked to ED visits and other hospitalizations using patient-specific record linkage numbers. The operating assumption was that any ED visit or hospitalization that preceded or followed the index admission date by 2 days was likely associated with the same injury event, as has previously been done.8 The time span of two days was selected as there are some transfer processes from rural areas which may take longer than 24 hours.
Injury severity scores (ISS) were derived using a publicly-available Stata program for Injury Classification (ICDPIC) which uses ICD-9-CM diagnosis codes.9 Mechanisms of injury were determined using principal E-codes.
Inclusion/Exclusion Criteria
We included all patients ≥18 years of age with a hospital admission listing a primary diagnosis consistent with trauma (ICD9-CM 800.00 to 959.0, excluding 905 to 909; and 910 to 924, and 930 to 939).10 Patients were excluded if the primary diagnosis was listed as a burn injury, if the index admission was listed as “elective,” or if admission was not to a general acute care hospital (e.g. psychiatric health facility). We also excluded cases where it would have been impossible to link or determine the order of subsequent hospital visits (e.g. patient records without record-linkage numbers or dates of service).
Analysis
The primary outcome was the all-cause readmission rate. Unadjusted analyses were performed to compare patients who experienced at least one readmission within one year vs. patients who were not readmitted in order to describe the population. Analyses to determine the association between trauma center care and readmissions were performed on those patients who survived for the entire year after injury. The primary reason for this was to isolate the effect on trauma survivors, because the mortality benefit of trauma center care has already been established. Furthermore, death serves as a competing outcome for readmission rates which would bias results. Patients were categorized as to whether the index admission for trauma occurred at a Level I or II trauma center or not. “Primary Triage” was defined as a patient who was directly transported from the field to a Level I or II trauma center.” Secondary triage” was defined as a patient who first visited a non-Level I/II trauma center, but was subsequently transferred to a Level I/II trauma center. Patients were further categorizes as receiving “No Trauma Center Care” (never taken or transferred to a Level I/II trauma center) and “Trauma Center Care” (either primary or secondary triage). Access to care was determined by whether the patient lived in a local emergency services region that had a Level I or II trauma center or not.
Categorical data were compared using chi square analysis. Continuous data were compared using Student’s T-test for data satisfying normality assumptions and Wilcoxon rank sum was used for nonparametric data. Logistic regression was performed to determine whether trauma center care was associated with readmissions while controlling for known confounders including demographics, number of comorbidities, injury severity, length of initial hospital stay, and access to trauma center care. These variables were selected due to their significance in univariate analysis and a priori determined clinical relevance. All statistical analysis was performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC).
Results
A total of 211,504 patients met inclusion criteria. Of these, 79,123 (38%) experienced one or more readmissions within one year. Characteristics of patients who were readmitted were different from those who were not in all measures. (Table 1) Patients who experienced a readmission were older (65% were aged ≥65 vs. 40%, p<0.001) and more often female (70% vs. 63%, p<0.001). Patients who were readmitted had more severe injuries (12% vs. 10% with ISS>15, p<0.001), and were more often injured by a fall mechanism of injury (67% vs. 48%, p<0.001) for their first admission. Outcomes also differed for the cohort of patients who were readmitted vs. those who were not; specifically, one-year mortality rates for readmitted patients were approximately twice that of non-readmitted patients (20% vs. 9%, p<0.001) and per-patient one-year healthcare costs were almost 3 times as high ($49,510 vs. $17,040; p<0.001).
Table 1.
Characteristics of Patients who were Re-Admitted within 1 Year after Index Admission for Injury who Survived their Index Admission (but may not have survived the year)
| All Patients (N = 211504) | No Subsequent Admissions (N = 141494) | Patients with >=1 Admission (N = 79123) | p value | ||
|---|---|---|---|---|---|
| Demographics | |||||
| Age | 18–24 | 20112 (9.61%) | 17219 (12.38%) | 2893 (4.11%) | <0.001 |
| 25–34 | 19596 (9.36%) | 16226 (11.67%) | 3370 (4.79%) | ||
| 35–44 | 20000 (9.55%) | 15705 (11.30%) | 4295 (6.11%) | ||
| 45–54 | 24860 (11.87%) | 18327 (13.18%) | 6533 (9.29%) | ||
| 55–65 | 22629 (10.81%) | 15435 (11.10%) | 7194 (10.23%) | ||
| 65–74 | 22794 (10.89%) | 13614 (9.79%) | 9180 (13.05%) | ||
| 75–84 | 40020 (19.12%) | 21612 (15.54%) | 18408 (26.18%) | ||
| >84 | 39352 (18.80%) | 20902 (15.03%) | 18450 (26.24%) | ||
| Gender | Male | 106971 (51.09%) | 76194 (54.80%) | 30777 (43.77%) | <0.001 |
| Female | 102392 (48.91%) | 62846 (45.20%) | 39546 (56.23%) | ||
| Race | White | 136306 (65.11%) | 87006 (62.58%) | 49300 (70.11%) | <0.001 |
| Black | 13487 (6.44%) | 9392 (6.75%) | 4095 (5.82%) | ||
| Hispanic | 38507 (18.39%) | 27939 (20.09%) | 10568 (15.03%) | ||
| Asian | 11847 (5.66%) | 7920 (5.70%) | 3927 (5.58%) | ||
| Other or Unknown | 9216 (4.36%) | 6783 (4.79%) | 2433 (3.07%) | ||
| Insurance | Self-pay | 16959 (8.10%) | 14336 (10.31%) | 2623 (3.73%) | <0.001 |
| Medicare | 97877 (46.75%) | 52935 (38.07%) | 44942 (63.91%) | ||
| Medicaid | 19679 (9.40%) | 13525 (9.73%) | 6154 (8.75%) | ||
| Commercial | 51891 (24.79%) | 39715 (28.57%) | 12176 (17.31%) | ||
| Other or Unknown | 22948 (11%) | 18522 (13%) | 4426 (1%) | ||
| Injury Characteristics | |||||
| ISS | <15 | 186576 (89.12%) | 124703 (89.69%) | 61873 (87.98%) | <0.001 |
| >15 | 22787 (10.77%) | 14337 (10.13%) | 8450 (12.02%) | ||
| Mechanism | Penetrating | 12194 (5.82%) | 10020 (7.21%) | 2174 (3.09%) | <0.001 |
| Falls | 114756 (54.81%) | 67399 (48.47%) | 47357 (67.34%) | <0.001 | |
| Any MVC | 35140 (16.78%) | 26801 (19.28%) | 8339 (11.86%) | <0.001 | |
| Other | 28072 (13.41%) | 22268 (16.02%) | 5804 (8.25%) | <0.001 | |
| Missing | 19201 (9.17%) | 12552 (9.03%) | 6649 (9.45%) | 0.001 | |
| Outcomes | |||||
| Death during index admission | 5094 (2.43%) | 5073 (3.65%) | 21 (0.03%) | <0.001 | |
| 1-year mortality | 27228 (13.01%) | 13142 (9.45%) | 14086 (20.03%) | <0.001 | |
| 1-year costs | 28840.69 ± 52459.46 | 17039.72 ± 31942.98 | 49509.65 ± 71511.05 | <0.001 | |
ISS Injury Severity Score; MVC Motor Vehicle Collision
Note: percentages are for nonmissing values (?true for ISS?)
To better understand the nature of the readmissions, a descriptive analysis was conducted on patients who both survived for one year following the index admission for injury and who were admitted at least one time during that year. There were 55,638 patients who survived for one year and were readmitted, with a total of 100,375 readmission events. (Table 2) Of the readmitted patients, 62% were readmitted once, but 38% were admitted more than one time over the course of the year. Most patients (86%) were readmitted with non-trauma primary diagnoses. The majority of re-admissions were unscheduled (67%) and 55% of readmissions were to same hospital as the index admission.
Table 2.
Characteristics of Readmissions within 1 Year for those who survived (Note 55638 not the same as 79123 minus 14086=65037)
| Readmissions per patient | |
|---|---|
| Total number of patients readmitted | N=55638 |
| Number of readmissions per patient | |
| 1 | 34582 (62.16%) |
| 2 | 10911 (19.61%) |
| 3 | 5054 (9.08%) |
| >=4 | 5091 (9.15%) |
| Number of readmissions per patient | |
| 0 | 47937 (86.16%) |
| 1 | 7250 (13.03%) |
| 2 | 398 (0.72%) |
| 3 | 38 (0.07%) |
| >=4 | 15 (0.03%) |
| Readmission events (i.e. patients may have had more than one readmission) | |
| Total number of readmissions | 100375 |
| Total number of trauma readmissions (% of all readmissions) | 8093 (8.06%) |
| Mean time from discharge to readmission (days) | 104.03 ± 112.05 |
| Type of admission for all readmissions | |
| Scheduled | 32620 (32.50%) |
| Unscheduled | 67625 (67.37%) |
| Hospitalized at the Same Hospital Visited during Index Hospitalization Event | 55471 (55.26%) |
| Primary Diagnosis ICD9 Categories at all readmissions | |
| V code diagnosis (encounters not due to disease or injury) | 21255 (21.18%) |
| Injury and Poisoning | 20345 (20.27%) |
| Diseases of Circulatory System | 10970 (10.93%) |
| Diseases of the Respiratory System | 6962 (6.94%) |
| Mental Disorders | 6654 (6.63%) |
| Diseases of the Digestive System | 6217 (6.19%) |
| Diseases of the Musculoskeletal System | 5395 (5.37%) |
| Infectious and Parasitic Disease | 4192 (4.18%) |
| Symptoms, Signs, and Ill-Defined Conditions | 4176 (4.16%) |
| Diseases of the Genitourinary System | 4123 (4.11%) |
| Endocrine, Nutritional and Metabolic, and Immunity | 3257 (3.24%) |
| Diseases of Skin and Subcutaneous Tissue | 2241 (2.23%) |
| Diseases of the Nervous System and Sense Organs | 2170 (2.16%) |
| Neoplasms | 1040 (1.04%) |
| Diseases of Blood and Blood Forming Organs | 904 (0.90%) |
| Complications of Pregnancy and Childbirth | 384 (0.38%) |
| Congenital Anomalies | 51 (0.05%) |
| Unknown | 35 (0.03%) |
| Certain Conditions Originating in the Perinatal Period | 4 (0.00%) |
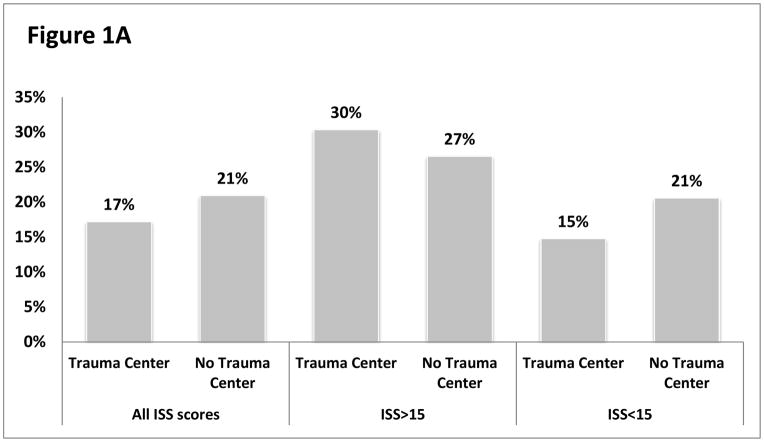
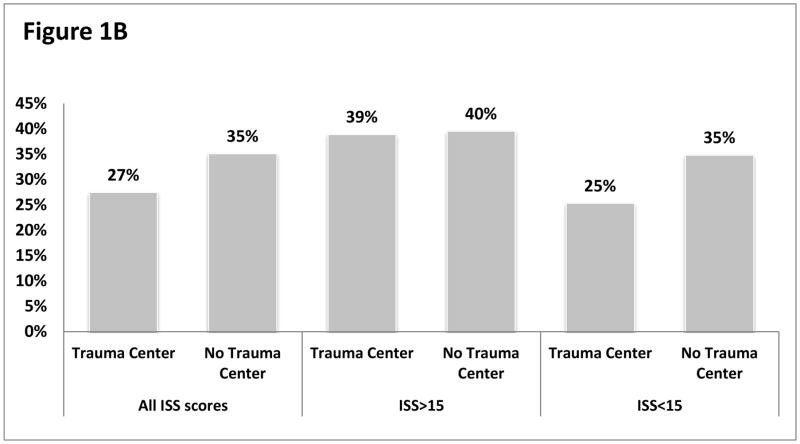
The association between readmissions and whether the patient had received care at a trauma center was evaluated for the cohort of patients who survived for one year following injury. A total of 174,318 (82.42%) survived for one year following injury and had complete data on hospital and injury characteristics. For patients with an ISS<15, readmissions were significantly lower when patients were treated at trauma centers vs. non-trauma centers at both 30 days (15% vs. 21%, p<0.001) and one year (25% vs. 35%, p<0.001). (Figures 1A&B) For patients with an ISS>15, 30-day readmissions were lower when the index hospitalization occurred at a non-trauma center (27% vs. 30%, p<0.001) and no different at one year (39% vs. 40%, p=0.818).
Figure 1.
Figure 1A: 30-Day All-Cause Readmissions
Figure 1B: One-Year All-Cause Readmissions
Since the higher rate of readmissions for severely-injured patients in unadjusted analysis may be related to the fact that trauma centers treat the most severely-injured patients, logistic regression to control for age, gender, comorbidities, injury severity, length of stay for the initial hospitalization, and access to trauma center care was performed. After controlling for these confounders, patients who were brought directly to a trauma center experienced lower rates of readmission at both 30 days (OR 0.89, 95% CI 0.87–0.92, p<0.001) and one year (OR 0.96, 95% CI 0.93–0.98, p=0.0008).
Discussion
Our findings demonstrate that for patients who survive their initial trauma, triage to a trauma center is associated with an 11% reduction in the adjusted 30-day odds ratio for readmission, and a 4% reduction in odds at one year. In the current healthcare environment, readmission rates have been introduced as a metric to assess the quality of care. Readmission rates after trauma have been explored as performance indicators for hospitals, 11,12 but have not been used to assess the value of trauma systems. This is the first study to show that trauma system care is associated with reduced readmissions across the injured U.S. population. The findings have significant implications for quality of care as well as for costs. For example, the one-year costs associated for patients who were readmitted within one year were almost 3 times higher compared to patients who were not admitted. Readmissions provide a new lens through which the value of trauma systems can be evaluated.
Interestingly, we also found that patients with minor injuries experienced lower readmission rates when treated at trauma centers. Rates of readmission were 6–10% higher for patients with minor injuries who were taken to non-trauma centers when compared to those taken to trauma centers. As trauma system performance has historically been measured by mortality benefits in the severely-injured, these data suggest that trauma systems benefit patients with minor injuries as well. This is relevant when considering over-triage rates and the impact it may have on costs. For example, costs associated with over-triage during the initial hospitalization may be outweighed by the decreased costs associated with lower readmission rates over time. As states consider funding for trauma institutions, these longer-term considerations should play an important role.
There were other interesting observations from the readmitted population. As would be expected, all-cause readmissions are more common for older adults. Patients older than the age of 75 comprised almost half of the readmitted population. This likely represents some background activity of readmissions experienced by older adults due to comorbid illnesses. However, it would not be unreasonable to expect that injury further contributes to that burden. For example, Fawcett et al. evaluated patient factors associated with readmissions in the older adult population and found that cardiac conditions and anemia were commonly associated with readmissions after trauma in Washington.6 It may be that the combination of injury and cardiac conditions creates fertile ground for further deterioration. The current study design did not permit us to compare the injured older adult population to non-injured adults to determine the degree that an injury might contribute to re-hospitalization, but it is the subject of future work.
One aspect of the analysis we were not able to take in account was socioeconomic status. This was due to limitations with the data and characteristics of the readmitted population. The database does not contain information on employment or income. Proxies for socioeconomic status, such as race and insurance status, were collinear with the demographics of the readmitted population. That is, the readmitted cohort consisted mainly of white Medicare patients who sustained a fall mechanism of injury. Adding income level, level of education, or other markers of socioeconomic status would have further clarified factors associated with readmission.
The 30-day and one-year readmission rates observed in the current study (19% for 30-day and 32% for one year) are higher than some previous reports. These differences are likely due to study design and patient population. One of the previous reports represented a single-center study and reported 30-day readmission rates of 4%.5 This likely reflects an underestimate because many patients do not return to the center where they were originally hospitalized. In our study, only 55% of readmissions occurred in the same hospital as the index admission. Two other population-based studies from the United States report 30-day readmission rates of 8–14%.3,6 These studies also do not represent a complete picture. Both focused on the older adult population and one evaluated only unplanned readmissions. Unplanned readmissions comprised the majority (67%), but not all, of our population. Other differences between these studies and the current one may be further explained by regional variations in readmission rates, as has been shown for medical conditions.13
This is a retrospective study derived from administrative data. This limits the ability to obtain important clinical variables that could be important for analysis including physiology and functional status. As a result, there may be important clinical differences between patients treated at trauma centers and non-trauma centers that may contribute to the observed results. We are also unable to determine which hospital processes may be associated with a trauma center benefit, as there are no data on protocols or services employed.
This is the first population-based analysis to assess the whether trauma systems are associated with reduced readmissions in the United States. The findings indicate that the benefits of trauma center care extend beyond improvements in mortality to reduced readmissions after trauma. These benefits are experienced for patients regardless of injury severity of injury, and may serve as complementary metric to assess the value of trauma systems to the U.S. population.
Table 3.
Factors associated with the odds ratio of being readmitted, for those who survive for 30 days and 1 year
| Readmitted in 30 days | Readmitted in one year | |||
|---|---|---|---|---|
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Age (years) | 1.02 (1.02 – 1.02) | <.0001 | 1.02 (1.02 – 1.02) | <.0001 |
| Female gender (vs male) | 1.00 (0.97 – 1.02) | 0.8533 | 1.02 (0.99 – 1.04) | 0.1448 |
| Number comorbidities | 1.11 (1.10 – 1.12) | <.0001 | 1.23 (1.22 – 1.24) | <.0001 |
| Injury severity score (ISS>15 vs ISS<15) | 0.75 (0.73 – 0.78) | <.0001 | 1.32 (1.27 – 1.37) | <.0001 |
| Length for stay for index hospitalization | 1.07 (1.07 – 1.07) | <.0001 | 1.07 (1.07 – 1.07) | <.0001 |
| Trauma center access (vs not) | 0.99 (0.95 – 1.02) | 0.501 | 1.07 (1.04 – 1.11) | <.0001 |
| Triage Pattern (vs no trauma center care) | ||||
| Primary | 0.89 (0.87 – 0.92) | <.0001 | 0.96 (0.93 – 0.98) | 0.0008 |
| Secondary | 0.95 (0.89 – 1.02) | 0.1573 | 0.94 (0.89 – 1.00) | 0.0597 |
OR Odds Ratio; ISS Injury Severity Score
Acknowledgments
Funding/Support: Dr. Staudenmayer is supported by NIH/NIA 1K08AG04442801A1. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies.
Footnotes
Study Type: Economic/Decision
Level of Evidence: Level IV
Conflict of Interest Disclosures: No other authors reported disclosures.
Role of the Sponsors: NA
Disclaimer: The views expressed in this article do not reflect positions of Stanford University, or the University of California, San Francisco.
Author Contributions: Dr. Hsia and Feng Lin had full access to all of the data in the study. Dr. Staudenmayer and Feng Lin take responsibility for the accuracy of the data analysis.
Study concept and design: Staudenmayer and Hsia.
Acquisition of data: Hsia.
Analysis and interpretation of data: Staudenmayer, Lin, Spain, Weiser, Hsia
Drafting of the manuscript: Staudenmayer.
Critical revision of the manuscript for important intellectual content: Staudenmayer, Spain, Hsia, Maggio, Weiser.
Statistical analysis: Staudenmayer, Lin, Hsia.
Obtained funding: Hsia.
Administrative, technical, or material support: Hsia.
Study supervision: Hsia.
References
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 2.Mullins RJ, Veum-Stone J, Helfand M, Zimmer-Gembeck M, Hedges JR, Southard PA, Trunkey DD. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. Jama. 1994 Jun 22–29;271(24):1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 3.Spector WD, Mutter R, Owens P, Limcangco R. Thirty-day, all-cause readmissions for elderly patients who have an injury-related inpatient stay. Med Care. 2012 Oct;50(10):863–869. doi: 10.1097/MLR.0b013e31825f2840. [DOI] [PubMed] [Google Scholar]
- 4.Morris DS, Rohrbach J, Rogers M, Thanka Sundaram LM, Sonnad S, Pascual J, Sarani B, Reilly P, Sims C. The surgical revolving door: risk factors for hospital readmission. J Surg Res. 2011 Oct;170(2):297–301. doi: 10.1016/j.jss.2011.04.049. [DOI] [PubMed] [Google Scholar]
- 5.Morris DS, Rohrbach J, Sundaram LM, Sonnad S, Sarani B, Pascual J, Reilly P, Schwab CW, Sims C. Early hospital readmission in the trauma population: are the risk factors different? Injury. 2014 Jan;45(1):56–60. doi: 10.1016/j.injury.2013.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fawcett VJ, Flynn-O’Brien KT, Shorter Z, Davidson GH, Bulger E, Rivara FP, Arbabi S. Risk factors for unplanned readmissions in older adult trauma patients in Washington State: a competing risk analysis. J Am Coll Surg. 2015 Mar;220(3):330–338. doi: 10.1016/j.jamcollsurg.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Accessed February 1, 2013];Office of Statewide Health Planning and Development (OSHPD) web site. http://www.oshpd.ca.gov/
- 8.Staudenmayer K, Lin F, Mackersie R, Spain D, Hsia R. Variability in California triage from 2005 to 2009: a population-based longitudinal study of severely injured patients. J Trauma Acute Care Surg. 2014 Apr;76(4):1041–1047. doi: 10.1097/TA.0000000000000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark D, Osler T, Hahn D. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Boston College Department of Economics; 2010. [Google Scholar]
- 10.Resources for Optimal Care of the Injured Patient. Chicago: American College of Surgeons; 2006. [PubMed] [Google Scholar]
- 11.Moore L, Stelfox HT, Turgeon AF, Nathens AB, Lavoie A, Bourgeois G, Lapointe J. Derivation and validation of a quality indicator for 30-day unplanned hospital readmission to evaluate trauma care. J Trauma Acute Care Surg. 2014 May;76(5):1310–1316. doi: 10.1097/TA.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 12.Moore L, Stelfox HT, Turgeon AF, Nathens AB, Lavoie A, Emond M, Bourgeois G, Neveu X. Derivation and Validation of a Quality Indicator of Acute Care Length of Stay to Evaluate Trauma Care. Ann Surg. 2014 Apr 16; doi: 10.1097/SLA.0000000000000648. [DOI] [PubMed] [Google Scholar]
- 13.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011 Dec 15;365(24):2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]