Abstract
Objective
Coagulation factor XI (FXI) has been shown to contribute to thrombus formation on collagen or tissue factor (TF)-coated surfaces in vitro and in vivo by enhancing thrombin generation. Whether the role of the intrinsic pathway of coagulation is restricted to the local site of thrombus formation is unknown. This study was aimed to determine whether FXI could promote both proximal and distal platelet activation and aggregate formation in the bloodstream.
Approach and Results
Pharmacological blockade of FXI activation or thrombin activity in blood did not affect local platelet adhesion, yet reduced local platelet aggregation, thrombin localization and fibrin formation on immobilized collagen and TF under shear flow, ex vivo. Downstream of the thrombus formed on immobilized collagen or collagen and 10 pM TF, platelet CD62P expression and microaggregate formation and progressive platelet consumption were significantly reduced in the presence of FXI-function blocking antibodies or a thrombin inhibitor in a shear rate- and time-dependent manner. In a non-human primate model of thrombus formation, we found that inhibition of FXI reduced single platelet consumption in the bloodstream distal to a site of thrombus formation.
Conclusions
This study demonstrates that the FXI-thrombin axis contributes to distal platelet activation and procoagulant microaggregate formation in the blood flow downstream of the site of thrombus formation. Our data highlights FXI as a novel therapeutic target for inhibiting distal thrombus formation without affecting proximal platelet adhesion.
INTRODUCTION
Platelets and coagulation factors are two essential components of hemostasis. Upon vessel injury, resting platelets are immediately recruited to the exposed extracellular matrix under shear flow, followed by platelet adhesion and activation.1 Platelet activation triggers the surface expression of CD62P (P-selectin) from α-granules, and the conversion of integrin αIIbβ3 to its active conformation, potentiating homotypic aggregate formation via fibrinogen binding. In parallel, activation of the coagulation cascade leads to thrombin generation, which cleaves fibrinogen to fibrin to stabilize the hemostatic plug. Thrombin is also able to activate platelets through protease-activated receptors (PARs) and thus accelerate the activation of both hemostatic components.
Coagulation factor XI (FXI) participates in the intrinsic pathway, whereby activated FXI (FXIa) triggers the downstream activation of factor IX (FIX), which in turn activates factor X (FX). FXa then converts prothrombin to thrombin. Thrombin can directly activate FXIa to perpetuate its own generation, thereby creating a procoagulant feedback loop of thrombin generation driven by FXI-thrombin axis.2–4 To date, however, it is not clear whether the FXI-thrombin axis facilitates platelet activation and consumption in blood flow under prothrombotic conditions.
The aim of this study was to define the role of the FXI-thrombin axis in promoting platelet activation and aggregation at the site of, and distal to, thrombus formation under shear flow. We show that inhibition of FXIIa activation of FXI or thrombin activity abrogated platelet CD62P expression and microaggregate formation under both venous and arterial shear flows downstream of the site of thrombus formation on collagen and 10 pM TF. In vivo, inhibition of FXI also reduced single platelet consumption in the bloodstream distal to a site of thrombus formation. These results provide the first evidence of a role for FXI in mediating platelet activation and platelet aggregate formation downstream of the site of thrombus formation.
RESULTS
Role of FXII and FXI in clotting times
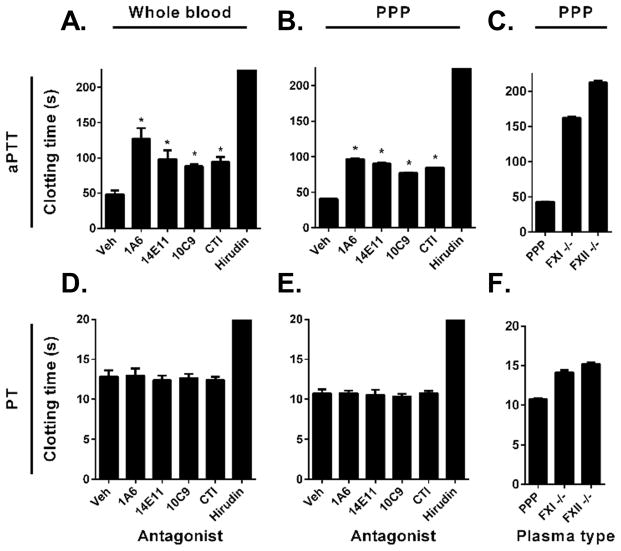
Our initial experiments were designed to evaluate the anticoagulant activity of FXI function-blocking antibodies, FXII inhibitor (CTI) and thrombin inhibitor (hirudin) in recalcified whole blood and platelet-poor plasma (Figure 1). Inhibition of FXI activation by FXIIa and FIX activation by FXIa with the function-blocking FXI-antibody (FXI-Ab 1A6) nearly tripled the aPTT in whole blood (47.8±5.6 s) to 126.9±15 s. Inhibition of FXI activation by FXIIa (FXI-Ab 14E11) or the neutralization of the FXIa active site (FXI-Ab 10C9) or inhibition of FXII activity (CTI) prolonged aPTT to 98.3±12.2 s, 87.9±3.3 s, and 94.2±6.9 s, respectively (Figure 1A). As expected, none of the inhibitors, except for the direct thrombin inhibitor (hirudin), were able to prolong PT in whole blood (Figure 1D). Similar results were seen in aPTT and PT assays using platelet-poor pooled human plasma (Figure 1B&E). Moreover, aPTTs were prolonged to 162.3±1.9 and 212.6±2.4 s using FXI- and FXII-immunodepleted plasmas, respectively (Figure 1C), while PTs were slightly prolonged to 14.1±0.3 s and 15.2±0.1 s, respectively (Figure 1F).
Figure 1. Role of FXII and FXI in clotting times.
Recalcified whole blood (A, D), pooled human plasma (PPP; B, E) or coagulation-factor depleted plasma (C, F) was incubated with indicated FXI function blocking antibody, FXII inhibitor (CTI) or direct thrombin inhibitor (hirudin). aPTT (A–C) or PT (D–F) was recorded as described in Methods. *indicates significantly different, p < 0.05, clotting time vs. vehicle (mean±SEM).
FXIa activity promotes local fibrin formation under shear
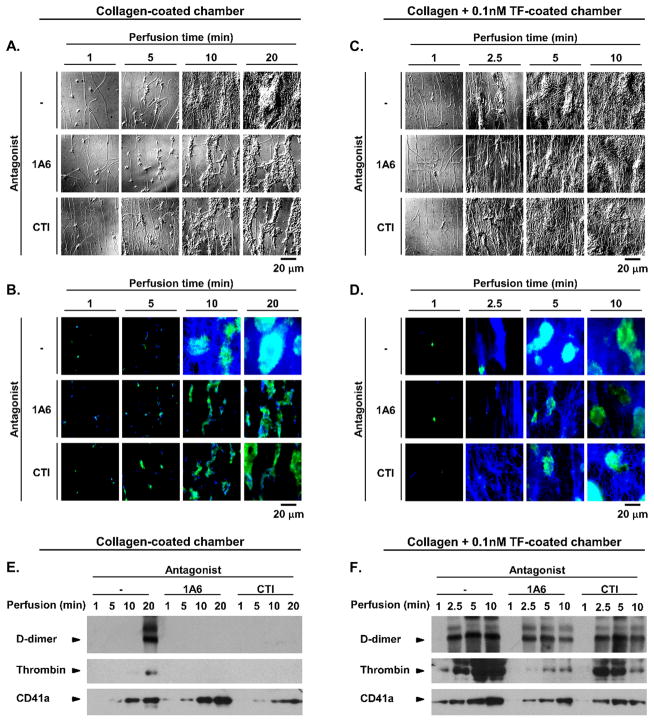
We next studied the role of FXI activation in local platelet deposition and fibrin formation under physiologically relevant shear flow conditions. Robust platelet adhesion, aggregation and fibrin formation was observed following the perfusion of recalcified whole blood over surfaces coated with collagen (Figure 2A&B). Both the rate and the extent of fibrin formation were enhanced on surfaces coated with collagen and tissue factor (TF; 0.01–0.1 nM), as visually recorded using differential interference contrast and fluorescence microscopy (Figure 2C&D and Figure IA&B in the online-only Data Supplement). TF alone (0.01–0.1 nM) yielded robust fibrin networks largely absent of platelets (Figure IA&B in the online-only Data Supplement).
Figure 2. FXIa activity promotes local fibrin formation under shear.
Recalcified whole blood was perfused over collagen (A&B) or collagen and 0.1nM TF (C&D) for indicated times at a shear rate of 300 s−1. Images of local thrombi formed at each time point in the presence of vehicle control, 50 μg/mL 1A6 or 40 μg/mL CTI were recorded using differential interference contrast (A&C) or fluorescent light microscopy (B&D) after staining for fibrin (blue) and P-selectin (green). In parallel experiments, thrombi were lysed and immunoblotted for the fibrin degradation product, D-dimer, thrombin and the platelet surface receptor, CD41a (E&F).
Inhibition of FXI activation by FXIIa and FIX activation by FXIa with FXI-Ab 1A6, or inhibition of FXIIa activity with CTI, decreased fibrin formation on collagen or surfaces coated with collagen and 0.01 nM TF or TF alone (Figure 2A&B and Figure IA&B in the online-only Data Supplement). Hirudin prevented fibrin formation on all surfaces, while CTI had no effect on surfaces coated with collagen and 0.1 nM (Figure 2C&D).
These results were confirmed by analyzing the degree of fibrin formation and platelet deposition by Western blotting following clot lysis with plasmin for the fibrin degradation product, D-dimer, and the CD41a platelet surface marker (Figure 2E&F; Figure IC in the online-only Data Supplement). Interestingly, we were able to detect thrombin in local thrombus lysates, and found that the increasing levels of clot-bound thrombin correlated with D-dimer levels. We found that inhibition of FXI activation by FXIIa with 14E11 reduced fibrin formation on collagen alone, while neither 14E11 nor the FXIa active site domain-neutralizing antibody, 10C9, affected fibrin formation on surfaces coated with collagen and 0.1 nM TF (Figure IC in the online-only Data Supplement). Control experiments using the thrombin inhibitor, hirudin, were shown to eliminate fibrin formation and the presence of clot-bound thrombin on all surfaces.
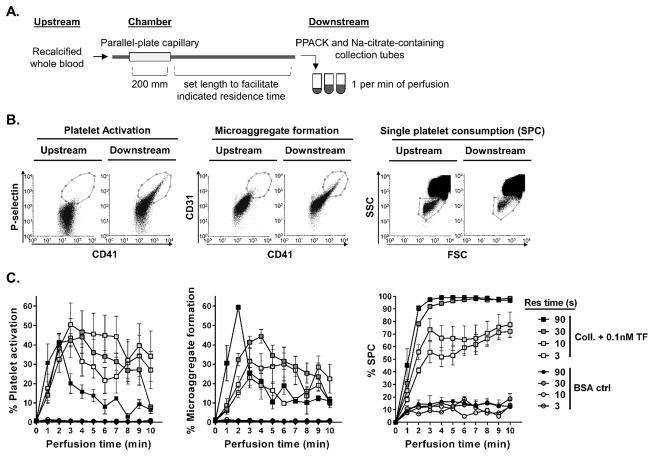
Propagation of distal platelet activation and single platelet consumption under shear in flow
We next designed a platform to determine whether local fibrin formation and thrombin generation at sites of thrombus formation promoted distal platelet activation and aggregate formation in the bloodstream. As shown in Figure 3A, a set length of tubing was added downstream of the chamber to allow platelets to react in flow for a set time (residence time) prior to being collected at 1 min intervals into tubes containing PPACK and sodium citrate. Distal single platelet consumption (reduction of single platelet population in the bloodstream), platelet activation (CD62P expression), and platelet microaggregate formation in solution (CD41a/CD31 high positive) was quantified using flow cytometry (Figure 3B). In parallel, untreated upstream samples were collected and analyzed to define the baseline parameters (time = 0 min), or stimulated with thrombin receptor activator peptide-6 (TRAP 6) to induce maximal platelet activation or microaggregate formation as a positive control (94.3±0.3% P-selectin activation, 47.6±2.4% microaggregate formation, and 77.2±3.6% single platelet consumption; mean±SEM).
Figure 3. Propagation of distal platelet activation and single platelet consumption under shear in flow.
Recalcified whole blood was perfused through a 200 mm chamber (coated with either BSA or 150 μg/mL collagen + 0.1 nM TF) before being collected downstream after indicated residence time in flow (A). Downstream samples were collected into a reaction quenching solution at 1 min intervals, immunostained and evaluated by FACS flow cytometry for percent platelet activation (CD41a+/CD62P+ events), platelet microaggregate formation (high fluorescence intensity CD41a+/CD31+ evets) and single platelet consumption (loss of single platelet population gate on FSC by SSC scatter). Representative raw FACS scatter plots (B) and quantification (C) for at least three experiments are reported (mean±SEM).
Our results show that platelet P-selectin expression, microaggregate formation and single platelet consumption increased as a function of residence time in whole blood samples downstream of chambers coated with collagen and 0.1 nM TF (Figure 3C). In contrast, an increase in platelet activation, microaggregate formation or single platelet consumption was not observed downstream of BSA-coated chambers.
At a set residence time of 30 sec, we observed an increase in platelet activation, microaggregate formation and single platelet consumption as a function of perfusion times downstream of chambers coated with collagen (Figure 4A). The inclusion of 0.01–1.0 nM TF with collagen coatings significantly increased both the rate and extent of platelet activation and microaggregate formation. It should be noted that the presence of TF dramatically increased the rate of single platelet consumption, resulting in over a 95% loss of single platelets by 8, 4 and 2 min for 0.01 nM, 0.1 nM and 1 nM TF, respectively, leading to grossly visible insoluble clot formation in flow in the distal samples. A drop in the percent of activated platelets and microaggregates was observed at these time points, reflective of the consumption of single platelets and microaggregates into downstream clots. Inhibition of platelet GPIIb-IIIa homodimer formation with eptifibatide increased circulating levels of single activated platelets and decreased microaggregate formation and single platelet consumption downstream of collagen-coated chambers. Similarly, the prevention of clot formation in solution downstream of collagen with 0.1 nM TF-coated chambers with eptifibatide resulted in a continued increase in circulating activated platelet levels beyond 4 min and attenuated both microaggregate formation and single platelet consumption, presumably sustained by fibrin agglutination (Figure 4B).
Figure 4. Presence of collagen and TF promotes distal platelet consumption.
Recalcified whole blood was perfused through a 200 mm chamber (coated with either BSA, collagen or collagen + 0.01 – 1.0 nM TF) and allowed to react in flow for 30 sec (residence time) before being collected into a reaction quenching solution at 1 min intervals. Quantification of platelet activation, microaggregate formation and single platelet consumption using FACS (A) for at least five experiments are reported (mean±SEM). In parallel experiments, whole blood was pretreated with a GPIIb-IIIa inhibitor, Eptifibatide (B).
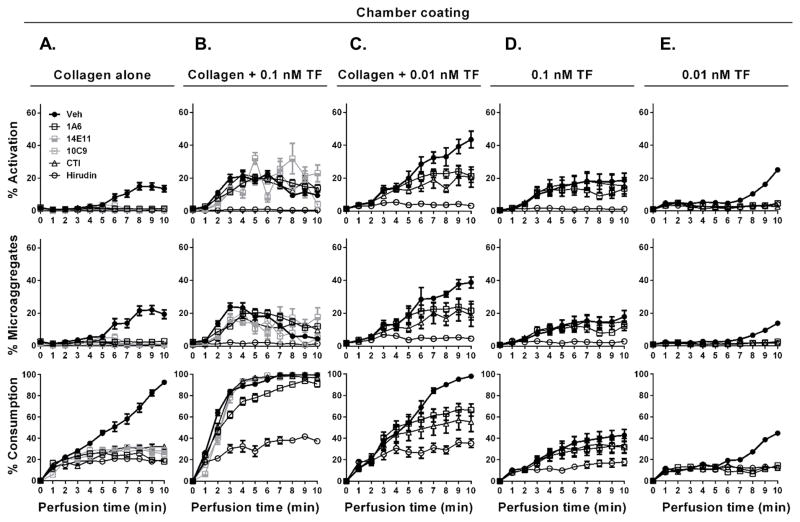
FXIa activity promotes distal platelet activation and consumption in the presence of collagen and TF
To examine the role of FXI activation in promoting distal platelet activation, whole blood was pretreated with the function-blocking FXI antibodies (1A6, 14E11 or 10C9), FXIIa inhibitor (CTI) or the thrombin inhibitor (hirudin) prior to perfusion through flow chambers coated with either collagen, TF, a combination of collagen and TF (0.01–0.1 nM), fibrinogen, thrombin, or vWF. Distal samples were collected downstream after 30 sec of residence time. We found that collagen, whether alone or in combination with TF, promoted the greatest degree of distal platelet activation and consumption as compared to TF alone, fibrinogen, thrombin or vWF (Figure 5 & Figure III in the online-only Data Supplement). Our results show that inhibition of FXIIa activation of FXI, FXIa activation of FIX and FXIa activity with 14E11, 1A6 and 10C9, respectively, or FXIIa activity with CTI eliminated platelet activation, microaggregate formation and single platelet consumption downstream of collagen-coated chambers (Figure 5A). Exposure of blood to collagen in combination with increasing concentrations of TF drastically accelerated the rate and the extent of distal platelet activation, microaggregate formation and consumption (Figure 5B&C). In contrast to collagen alone, only the FXI inhibitor 1A6 attenuated the rate of platelet consumption in the presence of higher levels TF (0.1 nM), while both 1A6 and CTI were able to significantly reduce the rate of platelet consumption in the presence of lower levels of TF (0.01 nM). Hirudin dramatically reduced the degree of distal platelet activation, microaggregate formation and single platelet consumption regardless of local TF concentration. A similar mechanism was observed when the shear rate was increased to 1000 s−1 (Figure IIB in the online-only Data Supplement). These results suggest a role for the contact activation pathway in the initial amplification of thrombin generation downstream of sites of thrombus formation under flow.
Figure 5. FXIa activity promotes distal platelet activation and consumption in the presence of collagen and low levels of TF.
Recalcified whole blood pretreated with either vehicle, 1A6, 14E11, 10C9, CTI or hirudin was perfused over chambers coated with collagen, collagen + 0.01 – 0.1 nM TF, or 0.01 – 0.1 nM TF alone at shear rate of 300 s−1. Samples were collected downstream of the chamber; distal microaggregate formation and single platelet consumption was assessed by FACS (A–E). Results (mean±SEM) from at least 4 experiments.
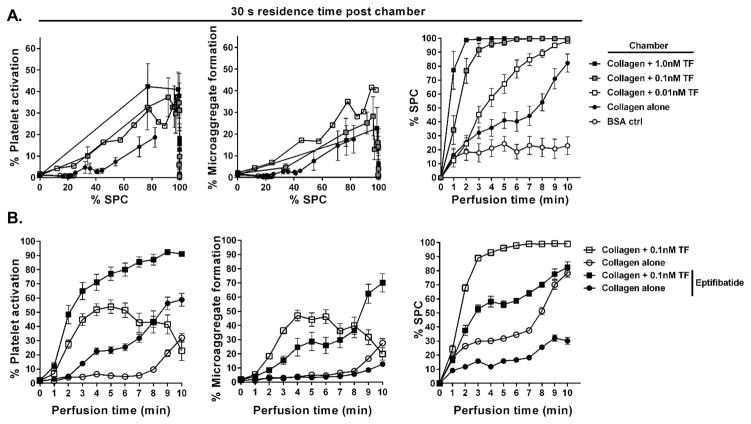
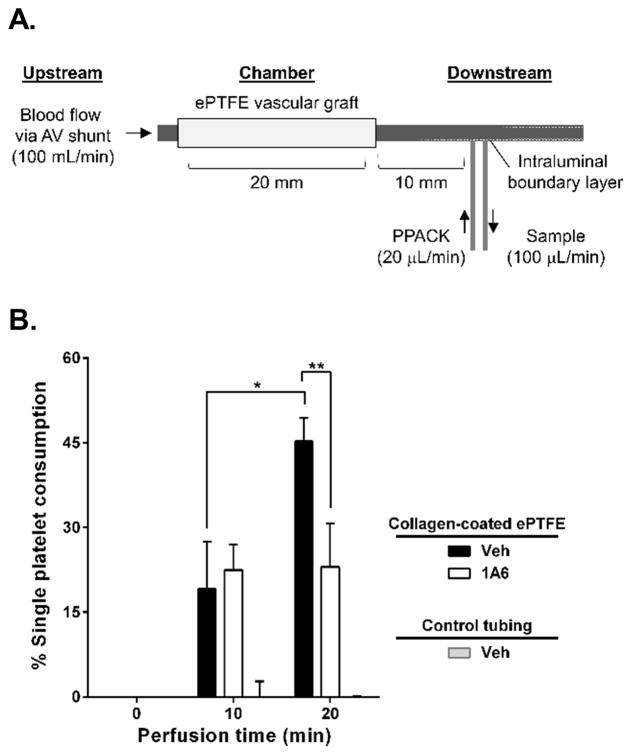
Protection of 1A6-treated baboons from collagen-initiated distal single platelet consumption
To examine the role of FXI activation in promoting distal platelet consumption in non-human primate baboon model, blood was collected distally from acutely introduced collagen-coated or control BSA-coated grafts in animals with chronic high flow arteriovenous shunts (Figure 6A). In line with the results shown in Fig 4A, exposure of blood to collagen in vivo accelerated the rate and the extent of distal single platelet consumption as compared to BSA controls. Our data demonstrates that inhibition of FXI activity with 1A6 treatment reduced distal single platelet consumption at 20 min of perfusion by fifty percent (p = 0.0180, n = 6; Figure 6B). Taken together with our previous studies demonstrating that inhibition of FXI prevented occlusion of collagen-coated grafts in a non-human primate model of thrombosis without increasing bleeding times, our data provides rationale for the development of anti-FXI therapeutics for the prevention of thrombotic distal complications.
Figure 6. Protection of 1A6-treated baboons from collagen-initiated distal single platelet consumption.
4-mm internal diameter expanded-polytetrafluoroethylene (ePTFE) vascular graft coated with collagen was deployed into a chronic high flow arteriovenous (AV) shunt in healthy baboons. In parallel, control experiments were performed with tubing alone. Samples were drawn from the intraluminal coagulation marker concentration boundary layer by a syringe pump 1 cm downstream from acutely developing thrombi. 1 mM PPACK anticoagulant was infused at 1/5th of the sample extraction rate 3 mm proximal to the sample port to prevent the sample port from occluding during the 1-hour study. Blood flow through the graft was maintained at a fixed rate of 100 mL/min for the entirety of each study by proximal clamping (A). Quantification of the six separate animal experiments for each treatment (mean±SEM) are reported (B). Significant rise in percent single platelet consumption immediately distal to collagen-coated ePTFE was seen between 10 to 20 min of perfusion in control animals (*, p = 0.0283; n = 6). 1A6-treated baboons maintained same single platelet levels at 20 min as at 10 min of perfusion (p = 0.9530; n = 6) significantly different from control at 20 min of perfusion (**, p = 0.0180; n = 6).
DISCUSSION
Coagulation FXI is an intrinsic pathway enzyme with an elusive role in normal hemostasis and mounting evidence for roles in thrombosis. Clinically, FXI deficiency is associated with only mild and injury-related bleeding, whilst elevated levels of FXI are associated with an increased risk for thrombotic complications.5–7 Patients deficient in the other members of the contact pathway, namely FXII and prekallikrein, do not exhibit bleeding complications, suggesting that FXI may play a role in hemostasis through feedback activation by thrombin.8–11 Moreover, activated FXI is able to activate FIX, FX, FV, and FVIII, bind platelets and inhibit tissue factor pathway inhibitor (TFPI).12–15 FXI therefore acts to amplify thrombin via multiple pathways, providing rationale for the inhibition of FXI-mediated thrombin generation as an antithrombotic therapy design. For instance, a phase 2 clinical trial reducing FXI levels using FXI-antisense oligonucleotide demonstrated decreased incidence of deep venous thrombosis (DVT) after knee replacement surgery. While the study showed that reduction of FXI levels prevented venous thrombosis, translational approaches targeted at FXI may sacrifice the hemostatic function of FXI, increasing the risk of bleeding.16,17 Thus, a better understanding of the role of FXI in thrombosis and hemostasis is required for the rational development of agents that target specific enzymatic functions of FXI, balancing safety with efficacy.
The biophysics of thrombus formation at a site of vascular injury has been well described,18–20 in which blood flow dictates the transport kinetics of blood cells and coagulation factors to the site of injury, and thrombin generation is rate limited by the assembly and sequential activation of coagulation factors on the surface or activated platelets. Thus, the Dahmköhler number (Da), which is the ratio of the rate of reaction to the rate of transport,21 is high (Da>1). In contrast, within the bloodstream, the kinetics of platelet activation and thrombin generation are diffusion limited, as platelets in the bloodstream experience limited relative blood flow, as cells in suspension are transported by viscous forces within the bloodstream, resulting in a low Da (<1). Our study demonstrates that FXI plays a differential role in promoting thrombin generation, platelet activation and aggregate formation in the bloodstream (diffusion-limited regime) relative to the site of thrombus formation (transport-limited regime).
Previously, we have demonstrated that inhibition of FXI activation by FXIIa is protective in a non-human primate model of local thrombus formation specifically due to a decrease in local thrombin generation and fibrin formation.22–24 However, the mechanism by which the FXIa-thrombin axis may contribute to formation of platelet aggregates in flowing blood and distal microvascular occlusions under proximal procoagulant conditions has not been explored. In this study we investigated downstream changes in platelets in whole blood following passage through collagen- or collagen and TF-coated flow chambers. Our results demonstrate that local thrombus formation on immobilized collagen and TF potentiated platelet activation in the bloodstream, resulting in the rapid formation of platelet aggregates in the bloodstream, which may hold potential to occlude downstream vessels. This process of distal platelet activation was directly dependent on thrombin activity. Inhibition of FIX activation by FXIa with the FXI-Ab 1A6 was protective against distal single platelet consumption in the bloodstream both in vitro and in vivo, providing an additional role for FXI in thrombotic complications.
It has been established that the health of microvessels plays an important role in maintaining unobstructed blood flow to organs. Aging vessels are stiffer and more tortuous due to many factors including atherosclerosis plaque buildup, hypertension-driven vessel wall remodeling, smoking and diabetes, which predispose them to aberrant blood flow, platelet activation and thrombosis.25 The physical biology of the microvasculature promotes increased platelet-platelet and platelet-endothelial cell interactions.26,27 Additionally, the reduced flow rates within venules serves to increase the residence time of circulating platelets within these vascular beds. In patients, introduction of a vascular injury, such as a surgical incision during a joint replacement followed by stasis due to patient immobility post-operation, may result in a local burst of thrombin generation.28,29 Under these conditions, our findings would suggest that FXI-dependent thrombin amplification and activation of platelets potentiates platelet microaggegate formation which may then occlude the microvascular networks.
In summary, this study demonstrates that the FXI axis plays a key role in distal platelet activation and microaggregate formation in solution downstream of thrombus formation under both venous and arterial shear flow. In addition to its anticoagulant role, pharmacological targeting of FXI might be able to regulate platelet function and therefore prevent platelet-driven amplification of circulating thrombi formation in prothrombotic conditions involving direct contact pathway agonists and widespread vascular injury.
MATERIALS AND METHODS
Materials and Methods are available in the online-only Data Supplement
Supplementary Material
SIGNIFICANCE.
Hemostasis is an active process between plasma and blood cells, resulting in thrombin generation, platelet activation and fibrin formation to generate a hemostatic plug that staunches blood loss following vessel injury. While the enzymatic reactions that mediate hemostasis are orchestrated outside the lumen of the blood vessel, thrombosis results from clot formation within the blood vessel. The events that support hemostasis versus thrombosis are distinct in part due to the rheology of blood flow that differentially distributes blood components inside and outside blood vessels. We developed an ex vivo flow model to mimic a local site of vascular injury in combination with the downstream collection of blood samples to allow for the analysis of distal platelet activation, aggregation and single platelet consumption in the bloodstream. Our results provide evidence that FXI plays a role in mediating distal platelet activation and aggregate formation downstream of the site of primary thrombus formation.
Acknowledgments
We thank C. Puy, S. Baker-Groberg, J. Pang, and K. Rees for insightful comments and technical assistance.
SOURCES OF FUNDING
This work was supported by grants from the National Institutes of Health (R01HL101972, R01GM116184 and R01HL047014), an Oregon Clinical and Translational Research Institute grant (UL1TR000128) and the Oregon Health and Science University School of Medicine MD/PhD program. O.J.T. McCarty is an American Heart Association Established Investigator (13EIA12630000). A. Itakura is a Bayer International Fellow.
NONSTANDARD ABBREVIATIONS AND ACRONYMS
- FXI
Coagulation factor XI
- FXIa
Activated coagulation factor XI
- FXII
Coagulation factor XII
- FXIIa
Activated coagulation factor XII
- TF
Tissue factor
- CD62P
P-selectin
- CTI
Corn trypsin inhibitor
- aPTT
Activated partial thromboplastin time
- PT
Prothrombin time
- FACS
Fluorescence-activated cell sorting
Footnotes
DISCLOSURES
A. Gruber, E.I. Tucker, and the Oregon Health & Science University have a significant financial interest in Aronora Inc., a company that may have a commercial interest in the results of this research. This potential conflict of interest has been reviewed and managed by the Oregon Health & Science University Conflict of Interest in Research Committee. C. Gerdes and R. Vetter are employees of Bayer Pharma AG. The remaining authors declare no competing financial interests.
References
- 1.Andrews RK, Berndt MC. Platelet physiology and thrombosis. Thromb Res. 2004;114(5–6):447–453. doi: 10.1016/j.thromres.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 2.Oliver JA, Monroe DM, Roberts HR, Hoffman M. Thrombin Activates Factor XI on Activated Platelets in the Absence of Factor XII. Arterioscler Thromb Vasc Biol. 1999;19(1):170–177. doi: 10.1161/01.atv.19.1.170. [DOI] [PubMed] [Google Scholar]
- 3.Kravtsov DV, Matafonov A, Tucker EI, et al. Factor XI contributes to thrombin generation in the absence of factor XII. Blood. 2009;114(2):452–458. doi: 10.1182/blood-2009-02-203604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maas C, Meijers JCM, Marquart JA, et al. Activated factor V is a cofactor for the activation of factor XI by thrombin in plasma. Proc Natl Acad Sci U S A. 2010;107(20):9083–9087. doi: 10.1073/pnas.1004741107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salomon O, Steinberg DM, Seligshon U. Variable bleeding manifestations characterize different types of surgery in patients with severe factor XI deficiency enabling parsimonious use of replacement therapy. Haemoph Off J World Fed Hemoph. 2006;12(5):490–493. doi: 10.1111/j.1365-2516.2006.01304.x. [DOI] [PubMed] [Google Scholar]
- 6.Meijers JCM, Tekelenburg WLH, Bouma BN, Bertina RM, Rosendaal FR. High Levels of Coagulation Factor XI as a Risk Factor for Venous Thrombosis. N Engl J Med. 2000;342(10):696–701. doi: 10.1056/NEJM200003093421004. [DOI] [PubMed] [Google Scholar]
- 7.Lavigne G, Mercier E, Queré I, Dauzat M, Gris J-C. Thrombophilic families with inheritably associated high levels of coagulation factors VIII, IX and XI. J Thromb Haemost. 2003;1(10):2134–2139. doi: 10.1046/j.1538-7836.2003.00410.x. [DOI] [PubMed] [Google Scholar]
- 8.Gailani D, Renné T. The intrinsic pathway of coagulation: a target for treating thromboembolic disease? J Thromb Haemost. 2007;5(6):1106–1112. doi: 10.1111/j.1538-7836.2007.02446.x. [DOI] [PubMed] [Google Scholar]
- 9.Renné T, Gailani D. Role of Factor XII in hemostasis and thrombosis: clinical implications. Expert Rev Cardiovasc Ther. 2007;5(4):733–741. doi: 10.1586/14779072.5.4.733. [DOI] [PubMed] [Google Scholar]
- 10.Naito K, Fujikawa K. Activation of human blood coagulation factor XI independent of factor XII. Factor XI is activated by thrombin and factor XIa in the presence of negatively charged surfaces. J Biol Chem. 1991;266(12):7353–7358. [PubMed] [Google Scholar]
- 11.Gailani D, Broze GJ. Factor XI activation in a revised model of blood coagulation. Science. 1991;253(5022):909–912. doi: 10.1126/science.1652157. [DOI] [PubMed] [Google Scholar]
- 12.Matafonov A, Cheng Q, Geng Y, et al. Evidence for factor IX-independent roles for factor XIa in blood coagulation. J Thromb Haemost. 2013;11(12):2118–2127. doi: 10.1111/jth.12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whelihan MF, Orfeo T, Gissel MT, Mann KG. Coagulation procofactor activation by factor XIa. J Thromb Haemost. 2010;8(7):1532–1539. doi: 10.1111/j.1538-7836.2010.03899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White-Adams TC, Berny MA, Tucker EI, et al. Identification of coagulation factor XI as a ligand for platelet apolipoprotein E receptor 2 (ApoER2) Arterioscler Thromb Vasc Biol. 2009;29(10):1602–1607. doi: 10.1161/ATVBAHA.109.187393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puy C, Tucker EI, Matafonov A, et al. Activated factor XI increases the procoagulant activity of the extrinsic pathway by inactivating tissue factor pathway inhibitor. Blood. 2015;125(9):1488–1496. doi: 10.1182/blood-2014-10-604587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang H, Löwenberg EC, Crosby JR, et al. Inhibition of the intrinsic coagulation pathway factor XI by antisense oligonucleotides: a novel antithrombotic strategy with lowered bleeding risk. Blood. 2010;116(22):4684–4692. doi: 10.1182/blood-2010-04-277798. [DOI] [PubMed] [Google Scholar]
- 17.Büller HR, Bethune C, Bhanot S, et al. Factor XI antisense oligonucleotide for prevention of venous thrombosis. N Engl J Med. 2015;372(3):232–240. doi: 10.1056/NEJMoa1405760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colace TV, Tormoen GW, McCarty OJ, Diamond SL. Microfluidics and Coagulation Biology. Annu Rev Biomed Eng. 2013;15:283–303. doi: 10.1146/annurev-bioeng-071812-152406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stalker TJ, Welsh JD, Tomaiuolo M, et al. A systems approach to hemostasis: 3. Thrombus consolidation regulates intrathrombus solute transport and local thrombin activity. Blood. 2014;124(11):1824–1831. doi: 10.1182/blood-2014-01-550319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomaiuolo M, Stalker TJ, Welsh JD, Diamond SL, Sinno T, Brass LF. A systems approach to hemostasis: 2. Computational analysis of molecular transport in the thrombus microenvironment. Blood. 2014;124(11):1816–1823. doi: 10.1182/blood-2014-01-550343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCarty OJ, Ku D, Sugimoto M, King MR, Cosemans JMEM, Neeves KB. Dimensional analysis and scaling relevant to flow models of thrombus formation. J Thromb Haemost. 2016 doi: 10.1111/jth.13241. in Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng Q, Tucker EI, Pine MS, et al. A role for factor XIIa-mediated factor XI activation in thrombus formation in vivo. Blood. 2010;116(19):3981–3989. doi: 10.1182/blood-2010-02-270918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tucker EI, Marzec UM, White TC, et al. Prevention of vascular graft occlusion and thrombus-associated thrombin generation by inhibition of factor XI. Blood. 2009;113(4):936–944. doi: 10.1182/blood-2008-06-163675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leung PY, Hurst S, Berny-Lang MA, et al. Inhibition of Factor XII-mediated activation of factor XI provides protection against experimental acute ischemic stroke in mice. Transl Stroke Res. 2012;3(3):381–389. doi: 10.1007/s12975-012-0186-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chesnutt JKW, Han H-C. Tortuosity triggers platelet activation and thrombus formation in microvessels. J Biomech Eng. 2011;133(12):121004–11. doi: 10.1115/1.4005478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang J, Bergeron AL, Yu Q, et al. Platelet aggregation and activation under complex Patterns of Shear Stress. Thromb Haemost. 2002;88(5):817–821. [PubMed] [Google Scholar]
- 27.Casa LDC, Ku DN. Geometric design of microfluidic chambers: platelet adhesion versus accumulation. Biomed Microdevices. 2014;16(1):115–126. doi: 10.1007/s10544-013-9811-7. [DOI] [PubMed] [Google Scholar]
- 28.Wong RK, Sleep JR, Visner AJ, et al. Thrombography reveals thrombin generation potential continues to deteriorate following cardiopulmonary bypass surgery despite adequate hemostasis. J Extra Corpor Technol. 2011;43(1):19–25. [PMC free article] [PubMed] [Google Scholar]
- 29.Shen F, Kastrup CJ, Liu Y, Ismagilov RF. Threshold response of initiation of blood coagulation by tissue factor in patterned microfluidic capillaries is controlled by shear rate. Arterioscler Thromb Vasc Biol. 2008;28(11):2035–2041. doi: 10.1161/ATVBAHA.108.173930. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.