Abstract
Objective
To estimate selected direct medical care costs of children with chronic pancreatitis (CP) and acute recurrent pancreatitis (ARP).
Methods
We performed a cross-sectional study of data from INSPPIRE (International Study Group of Pediatric Pancreatitis: In search for a cuRE), a multinational registry of children with ARP or CP. We determined health care utilization and estimated costs of hospitalizations, surgical and endoscopic procedures, and medications in our study population. Health care utilization data were obtained from all subjects enrolled in the study, and costs were calculated using national United States costs.
Results
We included 224 subjects (median age 12.7 years), 42% of whom had CP. Mean number of hospitalizations, including for surgery and endoscopic retrograde cholangiopancreatography (ERCP), was 2.3/person/year, costing an estimated average $38,755/person/year. Including outpatient medications, estimated total mean cost was $40,589/person/year. Subjects utilizing surgical procedures or ERCP incurred mean annual costs of $42,951/person and $12,035/person, respectively. Estimated annual costs of pancreatic enzyme replacement therapy, diabetic medications, and pain medications were $4,114, $1,761, and $614 per person, respectively. In an exploratory analysis, patients with the following characteristics appear to accrue higher costs than those without them: more frequent ARP attacks/year, reported constant or episodic pain, family history of pancreatic cancer, and use of pain medication.
Conclusions
ARP and CP are uncommon childhood conditions. The severe burden of disease associated with these conditions and their chronicity results in high healthcare utilization and costs. Interventions that reduce the need for hospitalization could lower costs for these children and their families.
Keywords: healthcare costs, quality of life, pain, hospitalization, economic
Introduction
In recent years, the number of children with acute pancreatitis (AP) has increased to approximately 1 in 10,000, an incidence less than but approaching that reported in adults (~1–5:10, 000), depending on the population described (1–7). Most children with AP have a single episode that resolves without complications, but a subset develops acute recurrent pancreatitis (ARP) or chronic pancreatitis (CP) (8). This group experiences recurrent episodes of pancreatitis with increased risk of complications. No epidemiological studies have focused on children, but overall ARP is reported in 15–35 % of children following an AP (1, 2, 4, 9) and as ≤ 0.5 per 100,000 in adult studies with younger populations (<34 years (10) and <25 years (11)). Despite modest incidence rates, ARP and CP are associated with significant disease burden. Children with these diseases experience frequent abdominal pain, emergency room visits and hospitalizations, and they undergo numerous endoscopic and surgical procedures (12, 13).
In adults, the high burden of disease associated with CP leads to a disproportionately high cost of medical care (14). The sources of these costs include hospitalization, complications of CP (including endocrine and exocrine insufficiency), and pain management. Adult patients with AP also incur substantial costs, estimated at $2 billion yearly in the United States (US) (15). A recent study reported an increased incidence of AP, length of stay and higher charges in children hospitalized for AP (16). The direct medical costs of pancreatitis of children with ARP and CP have not been analyzed, but are expected to be high.
In this study, we examined selected direct medical costs of ARP and CP in children enrolled in the INternational Study Group of Pediatric Pancreatitis: In search for a cuRE (INSPPIRE) registry at baseline. These direct costs include those of hospitalizations, procedures, and medications. These costs further define the burden of ARP and CP in children.
Methods
Study population
The design and implementation of the INSPPIRE registry has been described previously (17). In brief, the consortium collects data on the demographics, presentation, risk factors, diagnosis, and management of children with ARP or CP. For the current work, we included health care utilization data from subjects with ARP or CP enrolled at baseline at all sites, including 2 Canadian, 1 Israeli, 1 Australian, and 12 US Centers, since we considered utilization of treatments to be similar across countries. We applied only US national healthcare cost data, so that the costs would be uniform and comparable. This method is frequently used when determining care costs across international clinical trials (18). The consensus definition of ARP and CP in children have been published previously (8). We used data from subjects enrolled between August 2012 and March, 2014.
Patient and physician questionnaires employed in the INSPPIRE database have been described (17). Patient questionnaires queried emergency department visits, hospitalizations, and medication used for pain. Physicians utilized interactions with the patient and review of the medical record (test results, hospitalizations, imaging results and reports) to complete the questionnaires. Results were recorded in REDCap™ (Research Electronic Data Capture, Vanderbilt University) System database (19) to allow secure electronic capture of the data.
All centers had permission from their Institutional Review Boards or the equivalent for their country to proceed. Consent was obtained from the parents of subjects <18 years of age and from subjects themselves if ≥18; children gave assent at the age specified by the local Institutional Review Board.
Healthcare utilization
We estimated utilization and mean costs of i) total hospitalizations due to ARP or CP, including for operations or endoscopic procedures (endoscopic retrograde cholangiopancreatography (ERCP)), ii) ARP or CP-associated operations, and iii) ARP or CP-associated ERCP procedures reported for each patient at enrollment in INSPPIRE. In addition, we also estimated the cost of ARP or CP-associated medications (pancreatic enzymes, diabetes medications, corticosteroids, and pain medications) in our study population.
Data on frequency of ARP- or CP-associated hospitalization and medication use were obtained from the INSPPIRE patient questionnaire, whereas data on number of surgical and ERCP procedures performed were obtained from the physician questionnaire. Patient recall for hospitalizations is stronger than less dramatic health care use such as physician visits, and may be more accurate than physicians’ recall if patients are hospitalized at more than one health care system (20, 21). Disease onset was defined as either the i) date of diagnosis of pancreatitis, or ii) date of first hospitalization due to pancreatitis, whichever occurred first. If the date of diagnosis or of first hospitalization were unavailable, the date of first onset of symptoms was used as the time when the disease began. Since data on medication dosage, frequency, and duration were rarely reported, we assumed that patients were given the recommended indication-specific dose for each reported medication for a total of one year.
Because there are no large volume data on ERCP in children, we based our calculations on adult literature (22). We assumed that all surgical procedures required hospitalization, and, to be conservative, that 56.5% of ERCP procedures were performed in inpatient setting, with the remaining performed in outpatient setting (22). We also assumed that operations or ERCP procedures performed in an inpatient setting included a physician fee for the procedure performed in addition to hospitalization cost. We assumed ERCP procedures performed in an outpatient setting included a facility fee and a physician fee for the ERCP procedure.
We assumed that the patient-reported number of ARP and CP-associated hospitalizations included hospitalizations for surgical or ERCP procedures. If a patient’s total number of surgical or ERCP procedures exceeded the patient-reported number of ARP and CP-associated hospitalizations, the number of surgical or ERCP procedures was then used to estimate a patient’s total number of hospitalizations.
Costs
We used a “bottom-up” approach to estimate mean cost of pancreatitis in children by adding together the various elements that make up the diagnosis and treatment. This commonly used approach multiplies the unit cost of a particular diagnosis and treatment by the mean amount of utilization for diagnosis and treatment to obtain the mean total cost estimate (23). We estimated 2013 U.S. mean costs (not charges) of ARP or CP-associated hospitalizations, including operations or therapeutic/diagnostic ERCP procedures, overall, and stratified these data by patient clinical characteristics to identify potential areas of high costs in INSPPIRE (Figure 1). Charges were converted to costs using the Medicare cost-to-charge ratio. We used mean costs despite the fact that costs might be skewed. This was done because health care systems prefer calculation of mean costs to plan their expenses (24). Study outcomes were expressed as the cost of surgical and ERCP procedures or ARP or CP-associated medications per person per year among those who underwent the procedure or were on the medications. We also expressed the same costs per person per year over all the subjects analyzed. This analysis provided an estimate of costs both for high users of medical resources and over the larger population of children with ARP or CP.
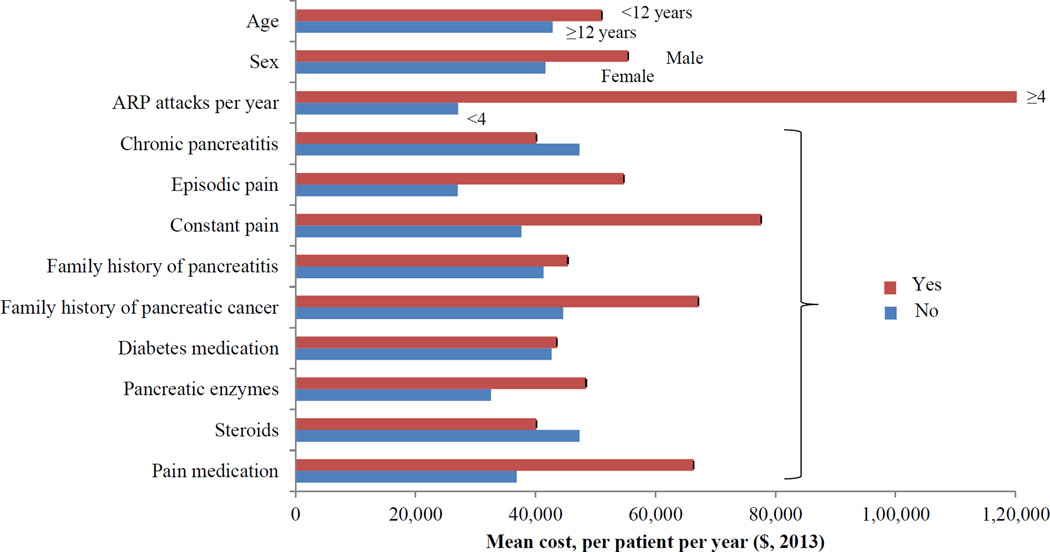
Figure 1. Total Healthcare Costs of the INSPPIRE Cohort.
Costs of hospitalization, including for surgical or ERCP procedures, and medication in INSPPIRE patient population at baseline, stratified by patient clinical characteristics (n=219)
ERCP=endoscopic retrograde cholangiopancreatography
Costs of ARP or CP- associated hospitalizations were obtained from the Healthcare Cost and Utilization Project-Kids’ Inpatient Database (HCUP-KIDs) 2012 (25) using ICD-9 codes 577.0 and 577.1 (Table 2). Costs of ARP or CP-associated surgical and ERCP procedures requiring hospitalization were also obtained from HCUP-KIDs 2012 (25) using the relevant ICD-9 codes, or from the literature (26). Physician fees for the surgical or ERCP procedure were obtained from Medicare Physician Fee Schedule 2013 (27) using CPT codes. Facility fees were obtained from the Medicare Ambulatory Surgical Center Fee Schedule 2013 (28). Medication costs were the average wholesale price using RED BOOK™ Online 2013 (29), and discounted at 17% for contract pricing. All costs were adjusted to 2013 dollars using the Consumer Price Index for medical care services (30).
Table 2.
Cost estimates for hospitalization, procedures, or medications related to pancreatitis in INSPIRRE at baseline (n=219), in 2013 US dollars
| Hospitalization or Procedure | Cost per unit |
Number of hospitalizations or procedures |
Reference | |
| n | % | |||
| ARP/CP hospitalizations | $14,913 | 1,200 | (18) | |
| Surgical therapies | 86 | (18) | ||
| Cholecystectomy | $13,047 | 35 | 40.6% | (18) |
| Celiac nerve block | $10,330 | 3 | 3.5% | (18) |
| Cyst/pseudocyst operation (with drainage) | $21,736 | 7 | 8.1% | (18) |
| Puestow procedure | $68,820 | 12 | 5.5% | (18) |
| Partial removal of pancreas | $37,887 | 1 | 0.5% | (18) |
| Complete removal of pancreas with islet autotransplantation | $195,5902 | 28 | 14.0% | (18,19) |
| ERCP procedures1 | 198 | |||
| Biliary sphincterotomy | $9,567 | 38 | 19.2% | (18, 20, 21) |
| Pancreatic sphincterotomy | $9,567 | 63 | 31.8% | (18, 20, 21) |
| Bile duct stenting | $11,862 | 11 | 5.6% | (18, 20, 21) |
| Pancreatic duct stenting | $10,500 | 58 | 29.3% | (18, 20, 21) |
| Pancreatic duct stone removal | $8,037 | 28 | 14.1% | (18, 20, 21) |
| Medication type (n, percent) | Cost per patient per year3 |
Cost per patient per year overall4 |
||
| Pancreatic enzymes (74, 33.9%) | $4,114 | $1,306 | ||
| Diabetes medication (17, 7.6%) | $1,761 | $201 | ||
| Steroids (5, 2.3%) | $91 | $2 | ||
| Pain medication (87, 39.9%) | $614 | $219 | ||
ARP=acute recurrent pancreatitis; CP=chronic pancreatitis; ERCP=endoscopic retrograde cholangiopancreatography; HCUP KID=Healthcare Cost and Utilization Project Kids’ Inpatient Database
Costs for ERCP were calculated assuming that 56.5% of total ERCPs were performed in hospital, and the remaining in an outpatient setting (17); inpatient ERCP included hospitalization costs (HCUP-KID) (18), and physician fee for procedure (20); outpatient ERCP included facility fee of $1,501 (21)
Estimated cost of complete removal of pancreas=$90,239 (20); estimated cost of islet autotransplantation=$105,051 (19)
Among those taking specified medication
Among all INSPPIRE patients
Exploratory analysis of difference in costs
We calculated the mean frequency and mean cost of hospitalization per person per year for selected patient characteristics. We chose not to perform statistical analysis of risk factors because of small sample size and variation in the source of the different utilization variables in our survey questions. Patient characteristics which could potentially affect hospitalization costs included socio-demographic factors (age and sex), frequency of ARP attacks, presence of CP, presence of pain (episodic or constant), family history of CP or ARP, family history of pancreatic cancer, and use of certain medications, including diabetes medication, pancreatic enzymes, and pain medication.
Results
Cohort
We analyzed data of the 224 INSPPIRE subjects enrolled at the time of study. Median age of our study population was 12.7 years (mean = 12.2 years; range 1.8–23.7 years). Among these patients, 218 (97%) were reported as ever having ARP. Out of 180 responders, 76 (42%) reported having CP. Eleven subjects were indeterminate (clarity of ARP vs. CP was not established). Median disease duration was 3.0 years (mean=4.1 years, range=0–19.7 years), and the majority of patients (~97%) had been hospitalized at least once due to ARP or CP over their duration of disease (Table 1).
Table 1.
Population and clinical characteristics of pediatric patient population in INSPPIRE at baseline
| Characteristic | Overall (n=224) | |||
|---|---|---|---|---|
| n | Median | Mean | Range or %1 | |
| Age, (year) | 12.7 | 12.2 | 1.8–23.7 | |
| Male/Female | 88/136 | 44% | ||
| Disease duration,(year) | 3.0 | 4.1 | 0.03–19.7 | |
| Ever had additional ARP attacks | 218 | 97% | ||
| Number of ARP attacks per person per year, | 2.0 | 3.9 | 0.06–84.2 | |
| Hospitalization for ARP | ||||
| Initial hospitalization for ARP | 211 | 97% | ||
| Number of additional hospitalizations for ARP | 3.0 | 5.0 | 0–30 | |
| Number of hospitalization for ARP per person per year | 1.4 | 2.4 | 0–28 | |
| Had surgical therapy | 60 | 27% | ||
| Had ERCP | 95 | 43% | ||
| Potential predictors of hospitalization costs | ||||
| Had chronic pancreatitis | 76 | 42% | ||
| Experienced episodic pain | 143 | 88% | ||
| Experienced constant pain | 43 | 27% | ||
| Family history of ARP/CP | 80 | 44% | ||
| Family history of pancreatic cancer | 24 | 14% | ||
| Diabetes medication | 15 | 7% | ||
| Pancreatic enzymes | 71 | 36% | ||
| Pain medication | 80 | 41% | ||
ARP=acute recurrent pancreatitis; CP=chronic pancreatitis; ERCP=endoscopic retrograde cholangiopancreatography
Percentages are out of total number of responders for each question, which may be fewer than the total n=224
Total costs
The mean number of annual hospitalizations including for surgical and ERCP procedures in the INSPPIRE patient population was 2.3 per person, costing an estimated average of $38,755 per person per year. Including medications (pancreatic enzyme, diabetes medication, steroids, and pain medication), the estimated mean cost across our study population was $40,589 per person per year.
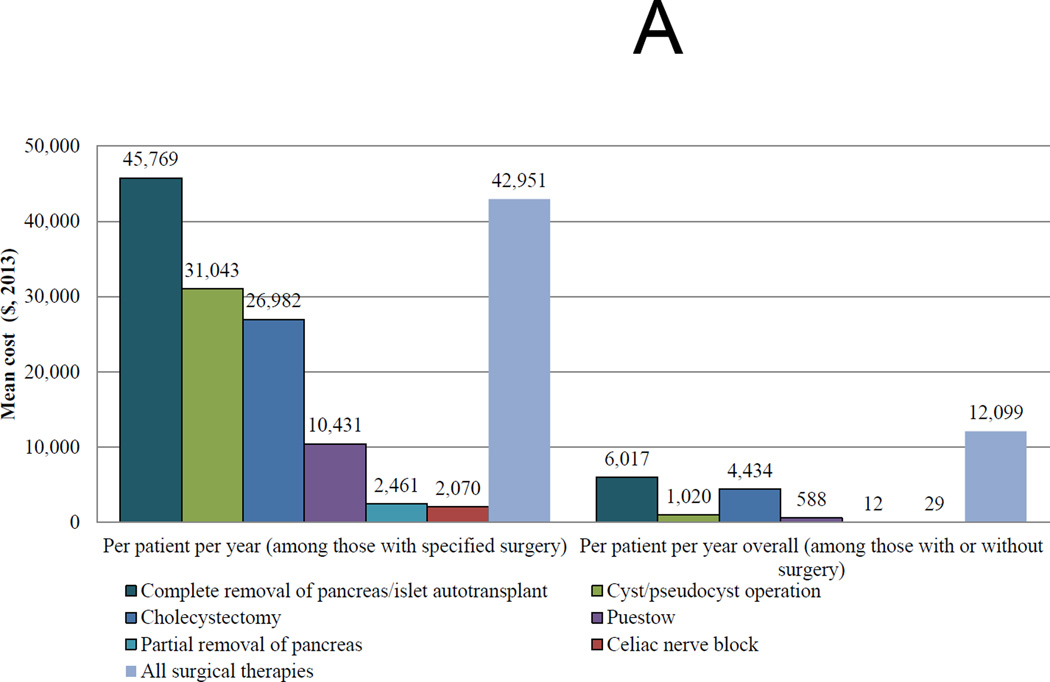
Costs of surgical therapy
Among 219 subjects on whom data on surgical therapies were available, 60 (28%) patients had 86 surgical therapies across their duration of disease (Tables 1 and 2). The most common operations were cholecystectomy and total pancreatectomy with islet autotransplantation (TPIAT) (Table 2).
Estimated mean costs of surgical procedures was $42,951 per person per year among those who had any surgical procedure, and $12,099 per person per year overall in our study population (Figure 2A, solid black bars). Across disease duration, patients who underwent TPIAT had the highest surgical cost per person per year ($45,769). Patients who underwent cyst/pseudocyst operation, cholecystectomy, or Puestow procedure (pancreaticojejunostomy) had surgery costs ranging from $10,431 to $31,043. Patients who underwent partial removal of the pancreas or had a celiac nerve block had the lowest surgical cost per person per year (<$2,500). Across our study population, TPIAT also had the highest cost per person per year ($6,017). The remaining subjects had total mean costs per operation type ranging $12–$4,434 per person per year overall.
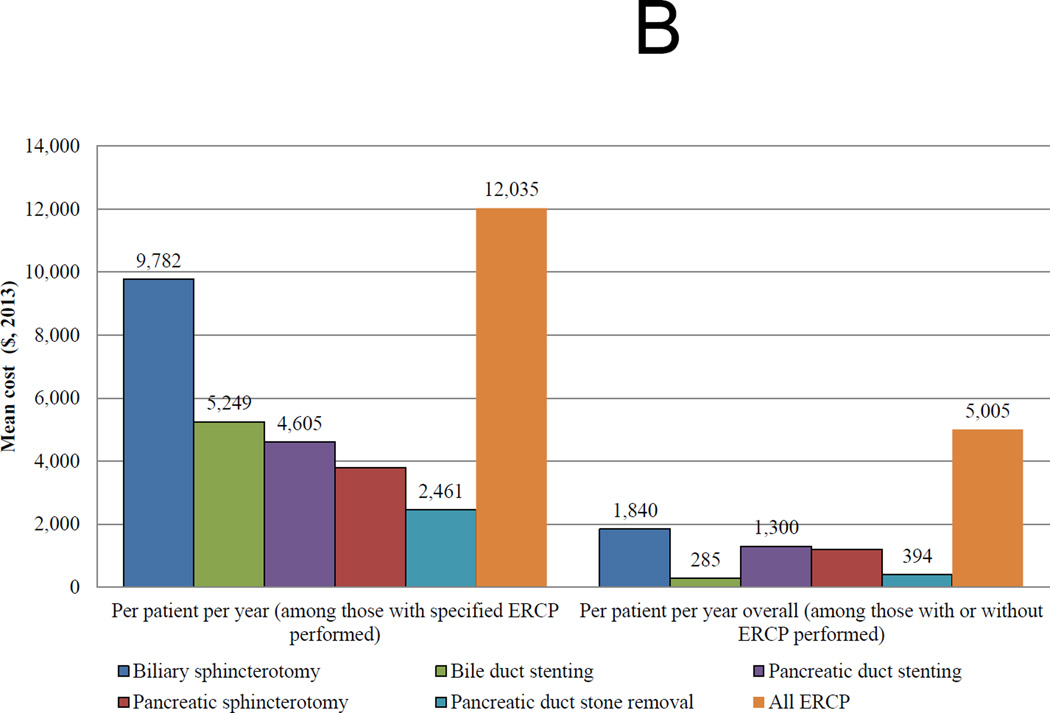
Figure 2. Costs of Surgical and Endoscopic Interventions in the INSPPIRE Cohort.
A. Mean costs of surgical therapies in INSPPIRE at baseline, stratified by type of surgery (n=219)
B. Mean costs of ERCP in INSPPIRE at baseline, stratified by type of ERCP (n=219)
ERCP= endoscopic retrograde cholangiopancreatography
Costs of ERCP
Among 219 subjects on whom data on surgical therapies were available, 95 (43%) patients had 198 ERCP procedures across their duration of disease (Tables 1 and 2). Ninety-six percent of ERCP were done for therapeutic purposes. The most common ERCP procedures performed were pancreatic sphincterotomy and pancreatic duct stenting (Table 2). We were unable to delineate whether sphincterotomy or stenting or stone removal were done separately or concurrently during the same session.
Estimated mean cost of ERCP procedures was $12,035 per person per year among those who had any procedure, and $5,005 per person per year for all patients (Figure 2B, solid black bars). Across disease duration, patients who underwent biliary sphincterotomy had the highest ERCP cost per person per year ($9,782). Patients who underwent ERCP procedures for other reasons had ERCP costs ranging from $2,461–$5,249. Across our study population, biliary sphincterotomy, pancreatic duct stenting, and pancreatic sphincterotomy had ERCP cost ranging from $1,185–$1,840 per person per year overall, while bile duct stenting and duct stone removal cost <$400 per person per year overall.
Costs of medication
In our study population, between 30–40% of patients were on pancreatic enzyme or pain medications, and <10% took steroids or diabetes medication (Table 2). Those taking pancreatic enzymes had the highest estimated medication cost per person per year ($4,114), followed by those on diabetes medication ($1,761), then those on pain medication ($614), and lastly those on corticosteroids ($91).
Exploratory analysis of potential high-costs areas
We estimated per person per year costs of ARP or CP-associated hospitalizations, as well as medications, stratified by patients’ clinical characteristics to provide better understanding of total costs (Figure 1). Patients with the following characteristics accrued higher costs (at least 50% more) than those without them including: more frequent ARP or CP attacks per year (≥4 attacks), reported constant or episodic pain, positive family history of pancreatic cancer, and use of pain medication. Other demographic or clinical characteristics also did not appear to be associated with higher costs.
Discussion
ARP and CP represent uncommon conditions in children, but they are accompanied by large disease burdens, including pain, emergency room visits and recurrent hospitalizations (12, 13). These medical complications are costly as we estimated an average annual cost of $40,589/child for ARP or CP in our population. Assuming an incidence of 0.5/100,000/year for CP (10, 11), and a US population of 313.9 million, > 1500 children will present with CP in the US in the next year (similar data are not available for ARP). By extrapolating these costs from the INSPPIRE registry, pediatric CP alone may result in an estimated $64 million cost to the US healthcare system per year. This estimate is similar to the previously reported $52 million per year hospitalization costs in the US for pediatric acute pancreatitis (15). Importantly, pediatric acute pancreatitis is usually a single event, while children with CP will continue to accrue higher lifetime costs as a result of repeated hospitalizations, procedures, and ongoing need for medical or surgical therapy.
In our study, children who had surgical and endoscopic procedures had the highest estimated health care costs, with surgical procedures costing $42,951/person/year and ERCP costing $12,035/person/year. Our results are similar to but expand on those of Pant et al who reported a higher disease burden and hospital costs using Nationwide Kids’ Inpatient Database (median $24,000 for CP vs. $16,000 for non-CP admissions) in children with CP (13).
Children who had TPIAT had the highest healthcare costs in our study population. Although TPIAT is a costly procedure, it may result in lower lifetime costs in CP and ARP by reducing pain and improving the quality of life (31–33). A study of TPIAT for adults with minimal change chronic pancreatitis demonstrated decreased mean annual admissions, endoscopy, imaging, and narcotic use one year after TPIAT (33). Furthermore, early surgery for CP in adults may reduce the risk of pancreatic insufficiency and the need for further intervention (34). This study did not factor in the costs for TPIAT, but calculated the costs for hospitalizations and complications of CP and emphasized cost savings if these were reduced. The ongoing ESCAPE study (Early surgery versus optimal current step-up practice for chronic pancreatitis), a randomized controlled, parallel, superiority multicenter study of early pancreatic surgery versus surgery after exhausting medical and endoscopic interventions, may help answer these questions, at least for adults (35).
As in other studies of healthcare costs of pancreatitis, pain is likely a major driver of many of the high costs of caring for these children. Pain is frequently the immediate cause of admission, surgical intervention, and endoscopic intervention for children with ARP or CP. In the North American Pancreatitis Study-2 (NAPS2) cohort, >90% of 414 patients with CP had been admitted to the hospital for pain at least once (36). In NAPS2, patients with constant pain had ≥10 hospitalizations for pain over their lifetime, compared with ≤2 for those with intermittent pain. Also in that study, 45% of adults with constant pain used “pain medication” regularly, compared with 22.3% of those with intermittent pain. Burden of pain in children with CP is not well-studied. In a previous study, over 80% of children with CP reported some form of pain within the previous year (12). Therefore, we expect that pain control in the ARP or CP population may result in significant reduction of economic costs. Head-to-head trials of interventions to reduce pain in children (both endoscopic and surgical) and trials to examine optimal timing of surgical procedures (similar to ESCAPE) would allow more effective and, thus, less costly care of children with these conditions.
Our study has several limitations. Since healthcare utilization data in our study population was acquired retrospectively, some therapies and hospitalizations may be omitted. Study physicians at each site reviewed subject charts to extract as much data as possible, but data on some episodes may not have been available. Self-reported data on medication use in our survey often lacked information on dose and treatment duration, thus necessitating some dose standardizing assumptions on our part when estimating medication costs. We were unable to separate whether sphincterotomy or stenting or stone removal were done separately or concurrently at one session. Similarly, we were only able to address the selected direct costs of ARP or CP. We were unable to include other imaging costs (magnetic resonance cholangiopancreatography [MRCP], magnetic resonance imaging [MRI], computed tomography. and endoscopic ultrasound), as the INSPPIRE registry did not include the full extent of imaging studies used in each subject at the time of data analysis. The INSPPIRE population may not be representative of the care of all children with ARP or CP because it consists of referral centers, with one center performing the majority of the TPIAT operations. Further, we did not account for cost differentials that are likely present between sites. Prospective data collection with larger number of patients accounting for all costs would be more representative of the actual cost of ARP and CP in children.
In addition to the direct costs of ARP or CP in children, we expect that the indirect economic costs would likely be high. Parents lose substantial time at work caring for children during exacerbations, both those requiring hospitalization and those that do not. Medical costs and travel expenses to tertiary medical centers may not be reimbursed by health insurance and would add to cost. Among adults with CP, the ability to work declines as the disease progresses (37, 38). It is possible that parental work also declines as their child’s pancreatitis progresses (39). Social and psychological costs are even harder to quantify, but may be substantial and lifelong. Structured interviews of adults with CP have described significant impact on their physical, psychological, and social functioning (40). In adults with non-alcoholic pancreatitis, depression is common (41). Most concerning is the evidence of the negative effects of pain duration on cognitive performance in CP (42). Taken together, the life-long economic impact of ARP or CP in children may be far greater than reflected in the direct costs of medical care described by our data.
Conclusions
ARP and CP are uncommon in the pediatric age group, but because of high disease burden, they are associated with high healthcare costs. Studies that improve our knowledge of these disorders and enhance our outpatient pain management strategies may reduce the need for hospitalizations, lower healthcare costs and improve quality of life of these children and their families.
What is known/What is new.
What is known about this subject?
Acute recurrent and chronic pancreatitis are uncommon in children.
Children with these conditions have a substantial burden of disease, with many hospitalizations, procedures, and pain.
What are the new findings?
Children with acute recurrent and chronic pancreatitis have high healthcare costs, resulting in a total conservative estimate of US costs of $60–70 million/year.
Highest estimated costs are for hospitalization, surgical and radiographic procedures, and medications.
Strategies to reduce hospitalization would reduce healthcare costs for acute recurrent and chronic pancreatitis.
Acknowledgments
Conflicts of interest and sources of funding: This work was supported by NIH DK096327 (AU); UL1 TR000442 (CTSA); T32 DK007762 (DU). Conflicts reported: Editor, Journal Pediatric Gastroenterology and Nutrition (MH), Editorial Board, Practical Gastroenterology (JP), speaker’s bureau for Medical Education Resources, Inc. (JP), Consultant, Abbvie Inc. for exocrine pancreatic function testing (AU). No relevant conflicts: SJS, MB, SZH, MA, BB, HD, PRD, DSF, SDF, CEG, MJG, TG, RH, SK, VDM, MEL, NEN, CYO, DT, SLW, MW, DU; DP, EV, KL, BF, DS, KK, VS, NP, CG, SR, EG, TH, TP, RS, VB, LN, CT, KC. The sponsors of this study (NIDDK) did not participate in the study design, collection of data, writing of the report, or the decision to submit this manuscript for publication.
Roles
The concept for the manuscript was developed by MBH, RH, AU, and SJS, with all authors contributing at a face-to-face meeting and online. The first draft was written by SJS, LW, and JT. The manuscript was reviewed, edited, and the final version approved by MBH, RH, BB, MB, PRD, DSF, SDF, CEG, MJG, TG, SZH, SK, VDM, MEL, CYO, JFP, DT, SLW, MW, DU, and AU.
References
- 1.Lopez JM. The changing incidence of acute pancreatitis in children: A single-institution perspective. J Pediatr. 2002;140:622–624. doi: 10.1067/mpd.2002.123880. [DOI] [PubMed] [Google Scholar]
- 2.Werlin SL, Kugathasan S, Frautschy BC. Pancreatitis in children. J Pediatr Gastroenterol Nutr. 2003;37:591–595. doi: 10.1097/00005176-200311000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Nydegger A, Heine RG, Ranuh R, et al. Changing incidence of acute pancreatitis: 10-year experience at the Royal Children’s Hospital, Melbourne. J Gastroenterol Hepatol. 2007;22:1313–1316. doi: 10.1111/j.1440-1746.2007.04936.x. [DOI] [PubMed] [Google Scholar]
- 4.Sanchez-Ramirez CA, Larrosa-Haro A, Flores-Martinez S, et al. Acute and recurrent pancreatitis in children: etiological factors. Acta Paediatr. 2007;96:534–537. doi: 10.1111/j.1651-2227.2007.00225.x. [DOI] [PubMed] [Google Scholar]
- 5.Park A, Latif SU, Shah AU, et al. Changing referral trends of acute pancreatitis in children: A 12-year single-center analysis. J Pediatr Gastroenterol Nutr. 2009;49:316–322. doi: 10.1097/MPG.0b013e31818d7db3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morinville VD, Barmada MM, Lowe ME. Increasing incidence of acute pancreatitis at an American pediatric tertiary care center. Pancreas. 2010;39:5–8. doi: 10.1097/MPA.0b013e3181baac47. [DOI] [PubMed] [Google Scholar]
- 7.Yadav D, Lowenfels AB. The Epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013:1252–1261. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morinville VD, Husain SZ, Bai H, et al. Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr. 2012;55:261–265. doi: 10.1097/MPG.0b013e31824f1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pezzilli R, Morselli-Labate AM, Castellano E, et al. Acute pancreatitis in children. An Italian multicenter study. Dig Liver Dis. 2002;34:343–348. doi: 10.1016/s1590-8658(02)80128-1. [DOI] [PubMed] [Google Scholar]
- 10.Yadav D, Timmons L, Benson JT, et al. Incidence, prevalence, and survival of chronic pancreatitis: A population-based study. Am J Gastroenterol. 2011;106:2192–2199. doi: 10.1038/ajg.2011.328. [DOI] [PubMed] [Google Scholar]
- 11.Spanier B, Bruno MJ, Dijkgraaf MG. Incidence and mortality of acute and chronic pancreatitis in the Netherlands: A nationwide record-linked cohort study for the years 1995–2005. World J Gastroenterol. 2013;19:3018–3026. doi: 10.3748/wjg.v19.i20.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwarzenberg SJ, Bellin M, Husain SZ, et al. Pediatric chronic pancreatitis is associated with genetic risk factors and substantial disease burden: A cross-sectional study. J Pediatr. 2015;166:890–896. doi: 10.1016/j.jpeds.2014.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pant C, Sferra TJ. Emergency department visits and hospitalizations in children with chronic pancreatitis in the United States. J Pediatr Gastroenterol Nutr. doi: 10.1097/MPG.0000000000000890. in press. [DOI] [PubMed] [Google Scholar]
- 14.Hall TC, Garcea G, Webb MA, et al. The socio-economic impact of chronic pancreatitis: a systematic review. J Evaluation Clin Pract. 2014;20:203–207. doi: 10.1111/jep.12117. [DOI] [PubMed] [Google Scholar]
- 15.Fagenholz PJ, Fernandez-del Castillo C, Harris NS, et al. Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas. 2007;35:302–307. doi: 10.1097/MPA.0b013e3180cac24b. [DOI] [PubMed] [Google Scholar]
- 16.Pant C, Deshpande A, Olyaee M, et al. Epidemiology of acute pancreatitis in hospitalized children in the United States from 2000–2009. PLoS One. 2014;9:e95552. doi: 10.1371/journal.pone.0095552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morinville VD, Lowe ME, Ahuja M, et al. Design and implementation of INSPPIRE (International Study group of Pediatric Pancreatitis In Search for a cuRE) J Pediatr Gastroenterol Nutr. 2014;59:360–364. doi: 10.1097/MPG.0000000000000417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reed SD, Anstrom KJ, Bakhai A, et al. Conducting economic evaluations alongside multinational clinical trials: toward a research consensus. Am Heart J. 2005;149:434–443. doi: 10.1016/j.ahj.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (Redcap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marshall SF, Deapen D, Allen M, et al. Validating California teachers study self-reports of recent hospitalization: comparison with California hospital discharge data. Am J Epidemiol. 2003;158:1012–1020. doi: 10.1093/aje/kwg256. [DOI] [PubMed] [Google Scholar]
- 21.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63:217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 22.Coelho-Prabhu N, Shah ND, Van Houten H, et al. Endoscopic retrograde cholangiopancreatography: utilisation and outcomes in a 10-year population-based cohort. BMJ Open [Internet] 2013;3 doi: 10.1136/bmjopen-2013-002689. http://www.ncbi.nlm.nih.gov/pubmed/23793659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Segal Joel E. Cost-of-Illness Studies –A Primer. January, 2006. [6.18.2015];RTI International RTI-UNC Center of Excellence in health Promotion Economics. https://www.rti.org/pubs/coi_primer.pdf,
- 24.Ramsey S, Willke R, Briggs A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: The ISPOR RCT-CEA Task Force report. Value Health. 2005;8:521–533. doi: 10.1111/j.1524-4733.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- 25.HCUP Kids’ Inpatient Database (NIS) Healthcare Cost and Utilization Project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2012. [2014 Oct 8]. http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=4655173A801AD88C&Form=SelRSTR&JS=Y&Action=>>Next>>&_RSTR= [Google Scholar]
- 26.Beckwith J, Nyman JA, Flanagan B, et al. A health economic analysis of clinical islet transplantation. Clin Transplant. 2012;26:23–33. doi: 10.1111/j.1399-0012.2011.01411.x. [DOI] [PubMed] [Google Scholar]
- 27.Medical Fees on CMS.gov. http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.
- 28.Medicare Ambulatory Surgical Center Fee Schedule 2013. [8/2014]; http://www.cms.gov/center/Provider-Type/Ambulatory-Surgical-Centers_ASC-Center.html.
- 29.Montvale, NY: Thomson Reuters; Online at http://www.redbook.com/redbook/awp/ Truven Health Analytics 2013, and RED BOOK, Physicians’ Desk Reference Inc. [Google Scholar]
- 30.Crawford M, Church J, Rippy D, editors. Bureau of Labor Statistics, U.S. Department of Labor. [8/2014];CPI Detailed Report Data for January 2013. :1–221. http://www.bls.gov/cpi/cpi_dr.htm.
- 31.Garcea G, Pollard CA, Illouz S, et al. Patient satisfaction and cost-effectiveness following total pancreatectomy with islet cell transplantation for chronic pancreatitis. Pancreas. 2013;42:322–328. doi: 10.1097/MPA.0b013e318264d027. [DOI] [PubMed] [Google Scholar]
- 32.Bellin MD, Freeman ML, Schwarzenberg SJ, Dunn TB, Beilman GJ, Vickers SM, et al. Quality of life improves for pediatric patients after total pancreatectomy and islet autotransplant for chronic pancreatitis. Clin Gastroenterol Hepatol. 2011;9:793–799. doi: 10.1016/j.cgh.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson GC, Ahmad SA, Schauer DP, et al. Cost-effectiveness of total pancreatectomy and islet cell autotransplantation for the treatment of minimal change chronic pancreatitis. J Gastrointest Surg. 2015;19:46–55. doi: 10.1007/s11605-014-2612-3. [DOI] [PubMed] [Google Scholar]
- 34.Yang CJ, Bliss LA, Schapira EF, et al. Systematic review of early surgery for chronic pancreatitis: Impact on pain, pancreatic function, and re-intervention. J Gastrointest Surg. 2014;18:1863–1869. doi: 10.1007/s11605-014-2571-8. [DOI] [PubMed] [Google Scholar]
- 35.Ali UA, Issa Y, Bruno MJ, et al. Early surgery versus optimal current step-up practice for chronic pancreatitis (ESCAPE): design and rationale of a randomized trial. BMC Gastroenterology. 2013;13:49–63. doi: 10.1186/1471-230X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mullady DK, Yadav D, Amann ST, O'Connell MR, Barmada MM, Elta GH, et al. Type of pain, pain-associated complications, quality of life, disability and resource utilisation in chronic pancreatitis: A prospective cohort study. Gut. 2011;60:77–84. doi: 10.1136/gut.2010.213835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wehler M, Reulbach U, Nichterlein R, et al. Health-related quality of life in chronic pancreatitis: a psychometric assessment. Scan J Gastro. 2003;38:1083–1089. doi: 10.1080/00365520310005956. [DOI] [PubMed] [Google Scholar]
- 38.Lankisch PG, Lohr-Happe A, Otto J, Creutzfeldt W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion. 1993;54:148–155. doi: 10.1159/000201029. [DOI] [PubMed] [Google Scholar]
- 39.Zan H, Scharff RL. The heterogeneity in financial and time burden of caregiving to children wit chronic conditions. Matern Child Health J. 2014;19:615–625. doi: 10.1007/s10995-014-1547-3. [DOI] [PubMed] [Google Scholar]
- 40.Fitzsimmons D, Kahl S, Butturini G, et al. Symptoms and quality of life in chronic pancreatitis assessed by structured interview and the EORTC QLQ-C30 and QLQ-PAN26. Am J Gastroenterol. 2005;100:918–926. doi: 10.1111/j.1572-0241.2005.40859.x. [DOI] [PubMed] [Google Scholar]
- 41.Balliet WE, Edwards-Hampton S, Borckardt JJ, et al. Depressive symptoms, pain, and quality of life among patients with nonalcohol-related chronic pancreatitis. Pain Res Treat. 2012 doi: 10.1155/2012/978646. article ID 978646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jongsma MLS, Postma SAE, Souren P, et al. Neurodegenerative properties of chronic pain: Cognitive decline in patients with chronic pancreatitis. PLoS One. 2011;6:e23363. doi: 10.1371/journal.pone.0023363. [DOI] [PMC free article] [PubMed] [Google Scholar]