Abstract
Objective
Test the effect of exposure to the U.S. Food and Drug Administration’s proposed graphic images with text warning statements for cigarette packages on implicit and explicit attitudes toward smoking.
Design and methods
A two-session web-based study was conducted with 2192 young adults 18–25 years old. During session one, demographics, smoking behavior, and baseline implicit and explicit attitudes were assessed. Session two, completed on average 18 days later, contained random assignment to viewing one of three sets of cigarette packages, graphic images with text warnings, text warnings only, or current U.S Surgeon General’s text warnings. Participants then completed post-exposure measures of implicit and explicit attitudes. ANCOVAs tested the effect of condition on the outcomes, controlling for baseline attitudes.
Results
Smokers who viewed packages with graphic images plus text warnings demonstrated more negative implicit attitudes compared to smokers in the other conditions (p=.004). For the entire sample, explicit attitudes were more negative for those who viewed graphic images plus text warnings compared to those who viewed current U.S. Surgeon General’s text warnings (p=.014), but there was no difference compared to those who viewed text-only warnings.
Conclusion
Graphic health warnings on cigarette packages can influence young adult smokers’ implicit attitudes toward smoking.
Keywords: implicit attitude, explicit attitude, graphic warning labels, young adults, smoking
Introduction
One component of comprehensive tobacco control programs is requiring warning labels on cigarette packages, and the U.S. has lagged behind many parts of the world in terms of labeling regulations (Hammond, 2012). The small text warnings currently used in the U.S. have been shown to produce low levels of awareness and poor recall (Fischer, Richards, & Krugman, 1989). The Family Smoking Prevention and Tobacco Control Act of 2009 aimed to change this by requiring that large, health warning labels that include a graphic image and text message appear on tobacco packages (Deyton, Sharfstein, & Hamburg, 2010). However, the implementation of the new warning labels was stopped by the U.S. District Court for the District of Columbia, which ruled in favor of the tobacco industry stating that the evidence of the effectiveness of graphic warning labels was insufficient to justify an encroachment on the tobacco companies’ right to free commercial speech (R. J. Reynolds Tobacco Co., et al. v. Hamburg, et al., 2011). Despite this ruling, research from around the world has demonstrated that graphic health warnings are effective in changing smokers’ self-reported explicit beliefs and attitudes and intentions to quit smoking (Borland et al., 2009; Hammond et al., 2007; Hammond, Fong, McDonald, Brown, & Cameron, 2004; Hammond, Fong, McDonald, Cameron, & Brown, 2003; White, Webster, & Wakefield, 2008; Yong et al., 2014). The study conducted to inform the U.S. Food and Drug Administration’s (FDA) selection of the final graphic warnings utilized self-reported emotional and cognitive reactions, recall, beliefs about the health risks of smoking, and intention to quit as outcomes, which are all explicit measures (Nonnemaker, Choiniere, Farrelly, Kamyab, & Davis, 2015). One small experimental study reported that exposure to the graphic warning labels that were high in emotional reactivity reduced the electrophysiological brain response to smoking cues (Wang, Lowen, Romer, Giorno, & Langleben, 2015), but other recent studies on the impact of the FDA’s final proposed graphic warnings have relied on self-reported explicit outcome measures (Cameron, Pepper, & Brewer, 2013; Cantrell et al., 2013; Hammond, Reid, Driezen, & Boudreau, 2013; Mays et al., 2014; Nonnemaker et al., 2015; Villanti, Cantrell, Pearson, Vallone, & Rath, 2014).
However, changing explicit cognitions alone may not be sufficient to influence smokers’ behavior. Instead, studies of dual process models have shown that both conscious, controlled, reflective processes (such as explicit attitudes) and automatic associations that may be beyond conscious awareness (such as implicit attitudes) are important predictors of addictive behaviors like cigarette smoking (Wiers & Stacy, 2006). Explicit measures of attitudes, in which individuals directly report their evaluations of a target behavior by responding to survey questions, cannot detect attitudes that are outside of conscious awareness, and they may also underestimate positive attitudes for socially undesirable behaviors, such as smoking. In contrast, implicit attitudes, measured with a computer-based task that records reaction times to stimuli, reflect more automatic evaluative associations with smoking.
Prior studies have examined the role of implicit attitudes measured with the Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998) in predicting smoking behavior. Some previous work found that smokers had negative implicit attitudes toward smoking leading to questions about the relevance of the IAT for smoking behavior (Swanson, Swanson, & Greenwald, 2001). However, smokers have been found to have positive attitudes on the IAT when the IAT is personalized (De Houwer, Custers, & De Clercq, 2006). Moreover, implicit attitudes measured on-line with the IAT have been shown to prospectively predict both smoking onset and smoking cessation over and above explicit measures (Chassin, Presson, Sherman, Seo, & Macy, 2010; Sherman, Chassin, Presson, Seo, & Macy, 2009). One study demonstrated that implicit attitudes were transmitted intergenerationally from parents to their adolescent children, and those implicit attitudes, in turn, predicted smoking onset 18 months later (Sherman et al., 2009). A second study showed that, among adult smokers, those with more negative implicit attitudes toward smoking at baseline were more likely to quit smoking 18 months later (Chassin et al., 2010).
Given the importance of implicit attitudes in predicting smoking behavior, a potentially important goal for tobacco control is the implementation of interventions that change implicit attitudes. For example, a recent study demonstrated the utility of a web-based intervention in influencing the implicit attitudes of adult smokers (Macy, Chassin, Presson, & Sherman, 2015). In the current study, we tested whether exposure to the FDA’s final proposed set of nine graphic warning labels on cigarette packages similarly influenced implicit attitudes toward smoking. Exposure to graphic images may differentially affect implicit versus explicit outcomes because indirect, non-verbal outcomes such as implicit attitudes have been shown to be influenced by different types of information than more explicit, self-reported outcomes (McConnell & Rydell, 2014). The only other published study to use an implicit outcome measure found no effect of exposure to graphic warning labels, but that study included only two of the FDA warning labels among a diverse set of 15 labels (Süssenbach, Niemeier, & Glock, 2013).
We tested the effects of exposure to the nine FDA graphic warning labels among a racially and ethnically diverse sample of young adults. Young adulthood is a unique and important age period in terms of smoking behavior because onset, increases in consumption, and cessation attempts are all occurring during this time. Moreover, individuals who experiment or smoke at low levels during adolescence often transition to regular smoking as young adults (Husten, 2007). Furthermore, young adults are more prone to impulsive and risky decision making than adults as they generally lack vital regulatory mechanisms until their mid-twenties (Albert & Steinberg, 2011; Casey, Jones, & Hare, 2008; Spear, 2009; Steinberg, 2010) thus making them at increased risk for smoking onset. Because this age period is marked by brain maturation, the importance of understanding implicit and explicit processes during young adulthood is amplified. Therefore, we collected young adults’ baseline implicit and explicit attitudes toward smoking in one session, randomly assigned them to exposure to images of cigarette packages with the FDA’s proposed graphic images plus text warnings, text warnings only, or the current U.S. Surgeon General’s text warnings, and then measured post-exposure implicit and explicit attitudes in a follow-up session. Finally, it is important to know if the proposed warning labels are more effective for some subgroups than others, so we tested whether the effects of exposure to the cigarette packages on attitudes differed by smoking status, gender, and race/ethnicity.
Method
Sample
Participants were recruited into the study from a nationally representative online panel of adults (Research Now). Because this panel was limited in numbers of African American and Hispanic smokers, study participants were also recruited from additional online opt-in panels through Research Now. Participants were eligible for the study if they were 18 to 25 years old and identified as either white, African American, or Hispanic, and members of these demographic subgroups were targeted for recruitment. Potential participants were contacted by email and asked to participate in a two-session online study about health messages. Of the 9537 individuals who responded to the email invitation, 4357 met the eligibility criteria (age 18 to 25 and white, African American, or Hispanic race/ethnicity) and completed the first session. Of these participants, 2835 (65.1%) were retained in session two. Compared to those who were lost to follow-up, those who were retained were more likely to be older, t(3004.11) = 2.31; p = .021, white, χ2(2, n=4357) = 64.81; p < .001, non-smoking, χ2(1, n=4003) = 40.79; p < .001, to have more negative baseline implicit attitudes toward smoking, t(3952) = 2.39; p = .017, and to have more negative baseline explicit attitudes toward smoking, t(2979.50) = 3.47; p = .001, but there was no gender difference, χ2(1, n=4357) = 0.18; p = .669.
In addition to those lost to follow-up, 237 participants were excluded because of inconsistencies in reported smoking behavior, 60 were excluded because they reported being distracted at least three-fourths of the time during either session one or two, 88 were excluded because of missing data, 181 were excluded because they made too many errors on the IAT (more than 40% errors in any one of the critical blocks or more than 30% errors overall) during either session one or two, and 77 were excluded because of inconsistencies between their session one and session two smoking behavior. Thus, the final sample eligible for analyses was 2192.
Procedure
Data were obtained from two web-based sessions. Participants were informed that the study was about health messages in general rather than graphic warnings about smoking in particular. During session one, participants reported demographic characteristics, answered questions about their smoking-related behaviors and explicit attitudes, and completed an IAT to measure their implicit attitude toward smoking. One week after completing session one, participants received an email invitation to complete session two. The median time interval between sessions was 18 days, as most participants completed session 2 several days after receiving the invitation.
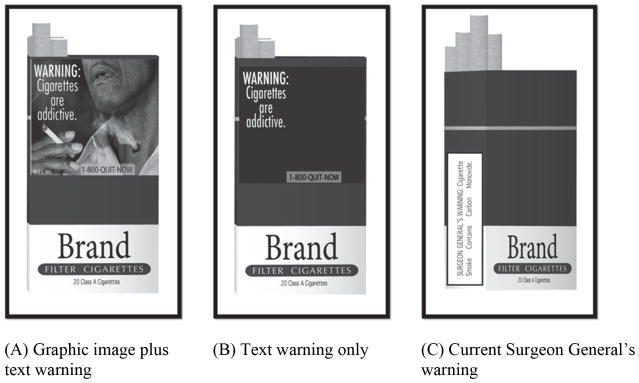
Session two started with random assignment to one of three versions of a slide-show of cigarette package images: (1) cigarette packages with the proposed FDA graphic warning labels including the text warning statements, (2) cigarette packages with labels containing only the text warning statements, and (3) cigarette packages with the current Surgeon General’s text-only warning statements on the side of the package. See Figure 1. Participants were instructed that the study was evaluating the extent to which they could remember what they saw and were encouraged to watch and pay attention, and 90% of participants responded correctly to a follow-up question about the messages they viewed. For the first two study conditions, participants viewed packages with the nine proposed warnings four times each in random order for a total of 36 exposures. For the third study condition, participants viewed packages with the four current Surgeon General’s warning statements in random order for a total of 36 exposures. In all three conditions, packages were evenly distributed between red and green colors to resemble actual cigarette packages, and the images were displayed for 6 seconds each with a screen that read “Get ready to view the next image” displayed for 3 seconds in between the images. After viewing the slide show, participants again completed an IAT and answered questions about their smoking-related explicit attitudes and behaviors.
Figure 1.
Examples of study stimuli.
Participants were paid US$13 in Research Now currency for completing session one and US$23 in Research Now currency for completing session two. The research protocol was approved by the Institutional Review Board at Indiana University, and informed consent was obtained for participation in the research.
Measures
Demographic characteristics included in the analyses were sex and race/ethnicity. Smoking status was determined by participants’ responses to two items. The first item asked participants to identify the sentence that best describes their cigarette smoking. Response options were, “I have never smoked a cigarette, not even a few puffs,” “I have smoked one cigarette or a few cigarettes ‘just to try’ but I have not smoked in the past month,” I no longer smoke but in the past I was a regular smoker,” “I smoke cigarettes but no more than one a month,” “I smoke cigarettes but no more than one a week,” “I cigarettes but no more than one a day,” and “I smoke more than one cigarette a day.” A study using an unannounced bioassay procedure supported the validity of this self-reported cigarette smoking item (Chassin, Presson, Sherman, & Edwards, 1990). The second item asked participants to report when they smoked their last cigarette. Response options ranged from, “I am smoking right now” to “More than five years ago” and included “Never.” Participants were considered non-smokers if they endorsed one of the first three options to the first item above and reported no smoking within the past month (71.1%). Participants were coded as smokers if they reported that they smoked at least one cigarette a month and had a cigarette within the last month (28.9%). Of the smokers, 45.9% were daily smokers, and 65.7% smoked less than five cigarettes per day.
At both sessions, participants completed an implicit measure of attitude toward smoking using an attitudinal IAT (Greenwald et al., 1998), which was administered online through Project Implicit’s Virtual Laboratory (Nosek, Greenwald, & Banaji, 2005). There were eight pictures that showed a scene related to smoking (a hand holding a burning a cigarette (3 pictures), a lit cigarette in an ashtray (2 pictures), someone lighting a cigarette, cigarettes lying on a table, and cigarettes and a lighter lying on a table) and eight pictures of geometric shapes (rectangle, parallelogram, triangle, pentagon, trapezoid, square, oval, and octagon). As positive and negative stimuli, we used eight adjectives with a positive meaning (excellent, fabulous, friendly, great, nice, pleasant, terrific, and wonderful) and eight adjectives with a negative meaning (awful, disgusting, dreadful, horrible, nasty, rotten, stupid, and ugly). All stimuli were presented in the center of a black screen with words displayed in green letters. The words smoking, shape, good, and bad were used for labels. The smoking and shape labels were displayed in white letters, and the good and bad labels in green letters. Participants responded by pressing the letter e (left) or the letter i (right) on the keyboard.
This version of the IAT is a dual categorization task. Participants saw the four types of stimuli: smoking pictures, shape pictures, positive words, and negative words. There were five phases to the IAT during which the labels of the stimuli assigned to the e (left) and i (right) keys were continuously displayed on the screen. The first phase was a practice phase consisting of 20 trials of good and bad words displayed in random order. Participants were instructed to match the words to the good or bad label by pressing either the e or i key. In the second phase, also consisting of 20 trials, the smoking and shape pictures were presented in random order, and participants were instructed to match the pictures to the smoking or shape label by pressing either the e or i key. The third phase contained the SMOKING + BAD task and consisted of three blocks, one of 20 trials and two of 40 trials, during which pictures and words were displayed in random order, and participants responded by pressing the appropriate key. The fourth and fifth phases were identical to the second and third, except that the response assignment for the smoking and shape pictures were reversed (e.g., the letter e instead of i), there were 40 trials in the fourth phase as opposed to 20 trials in the second phase, and the fifth phase contained the SMOKING + GOOD task. For each trial, the stimulus was displayed until the participant pressed the e or i key. If the response was correct, the next stimulus appeared. If the response was incorrect, a red X was displayed on the screen until the participant pressed the correct key. Phases three and five were used to measure implicit attitude toward smoking. To the extent that reaction times are slower during phase five when smoking pictures are paired with positive words than phase three when smoking pictures are paired with negative words, participants have more negative implicit attitudes toward smoking.
We calculated an IAT D score for each participant using a standard scoring algorithm (Greenwald, Nosek, & Banaji, 2003). As noted above, participants were flagged who made more than 40% errors in any one of the critical blocks or more than 30% errors overall. Trial latencies greater than 10,000 milliseconds or less than 400 milliseconds were eliminated, and error latencies were replaced with the block mean plus 600 milliseconds. A higher value indicated a more negative attitude toward smoking.
At both sessions, participants reported their explicit attitude toward smoking using a semantic differential measure of smoking as “nice versus awful,” “pleasant versus unpleasant,” “fun versus not fun,” “disgusting versus not disgusting,” and “sad versus not sad” (Azjen & Fishbein, 1970). Responses to the five items were averaged (α = .91 at both sessions). A higher value indicated a more negative attitude toward smoking.
At both sessions, participants responded to a question that was used to evaluate the quality of the data provided: “While you were working on this study how often did things happen to distract you?” As noted above, participants who reported that they were distracted ¾ of the time or more were excluded from analyses.
Analyses
To assess the effect of exposure to graphic warnings on cigarette packages on implicit and explicit attitudes toward smoking, analysis of covariance (ANCOVA) was conducted with post-exposure implicit and explicit attitude toward smoking as outcome variables, gender (male, female), race/ethnicity (white, African American, Hispanic), smoking status (smoker, nonsmoker), and cigarette package condition (graphic image plus text warning, text warning only, current U.S. Surgeon General’s text warning) as between subjects factors, and baseline implicit and explicit attitude toward smoking as covariates. Pairwise comparisons among the three cigarette pack conditions were tested when statistically significant main effects and interactions involving cigarette pack condition were detected.
Because of attrition and exclusion of unreliable data, to confirm the robustness of our findings yielded by ANCOVA, we used full information maximum likelihood (FIML) in Mplus version 7 to estimate saturated correlates models (Graham, 2003). The FIML procedure used data from all participants who had no missingness in the predictors even though their outcomes might have been missing. It generated parameter estimates and standard errors by “borrowing” information from the complete data to infer the missing values of the outcomes given the predictors (Enders & Bandalos, 2001; Schlomer, Bauman, & Card, 2010). In these saturated correlated models, auxiliary variables (age and parental educational attainment) were added to our hypothesized models providing additional information to reduce bias in the findings based on the assumption of missing at random. These models confirmed that the results obtained from ANCOVA using listwise deletion that are presented here were robust against potential biases due to missing data.
Results
Sample characteristics overall and by study condition are shown in Table 1. The race/ethnicity distribution of the sample reflects that of the U.S. population (U.S. Census Bureau, 2015). There were no differences in demographic characteristics or smoking status by study condition (all p-values >= .08). For the outcome measures, the mean IAT score was 0.62 (SD = .29, range −0.60 to 1.40) at session one and 0.53 (SD = .30, range −0.77 to 1.37) at session two. The mean for explicit attitudes was 4.04 (SD = 1.02, range 1 to 5) at session one and 4.16 (SD = .96, range 1 to 5) at session two.
Table 1.
Sample characteristics overall and by study condition
| Overall (n = 2192) % or mean (SD) |
Graphic Image Plus Text Warning (n = 719) % or mean (SD) |
Text Warning Only (n = 751) % or mean (SD) |
Current Surgeon General’s Warning (n = 722) % or mean (SD) |
p-value (ANOVA or chi-square) | |
|---|---|---|---|---|---|
| Age | 22.9 (2.0) | 22.9 (2.0) | 22.9 (2.0) | 23.0 (1.9) | .19 |
| Female | 46.9 | 46.7 | 45.0 | 49.0 | .30 |
| Race/ethnicity | |||||
| White | 61.6 | 61.3 | 61.4 | 62.0 | .92 |
| African American | 16.6 | 16.0 | 16.6 | 17.2 | |
| Hispanic | 21.8 | 22.7 | 22.0 | 20.8 | |
| Father has college degree | 37.8 | 38.5 | 38.5 | 36.3 | .60 |
| Mother has college degree | 39.3 | 41.7 | 39.7 | 36.6 | .13 |
| Smoker | 28.9 | 27.1 | 27.7 | 32.0 | .08 |
SD=standard deviation; ANOVA=analysis of variance.
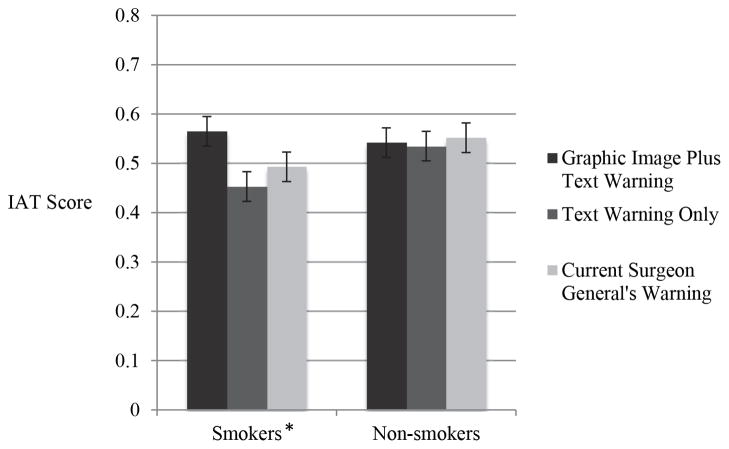
In the ANCOVA that assessed the effect of exposure to graphic warnings on implicit attitudes toward smoking, a significant main effect of cigarette package condition, F(2, 2155) = 4.69, p = .009, partial η2 = .004, indicated that implicit attitudes toward smoking were significantly more negative for those who viewed the graphic images plus text warnings (adjusted M = .55, se = .01) compared to those who viewed the text only warnings (adjusted M = .49, se = .01) but not significantly more negative compared to those who viewed the current U.S. Surgeon General’s text warnings (adjusted M = .52, se = .01). However, this main effect was qualified by a package condition by smoking status interaction, F(2, 2155) = 3.91, p = .02, partial η2 = .004, which indicated that the effect of the intervention differed by smoking status. As illustrated in Figure 2, for smokers, implicit attitudes toward smoking were more negative for participants who viewed the graphic images plus text warnings (adjusted M = .57, se = .03) compared to participants who viewed the text only warnings (adjusted M = .45, se = .02) and participants who viewed the current U.S. Surgeon General’s text warnings (adjusted M = .49, se = .02). The difference between the means was statistically significant, F(2, 2155) = 5.66, p = .004, partial η2 = .005. For non-smokers, however, there was no significant difference in implicit attitudes among the three groups, F(2, 2155) = 0.37, p = .69. Finally, there was a gender by race by smoking status by package condition interaction, F(4, 2155) = 2.37, p = .050, partial η2 = .004. Because of very small cell sizes in some subgroups, this four-way interaction was not interpretable.
Figure 2.
Implicit attitude toward smoking (IAT score) for the three study conditions by current smoking status, after controlling for baseline implicit attitude toward smoking. A higher value reflects a more negative implicit attitude toward smoking.
*Mean difference p = .004.
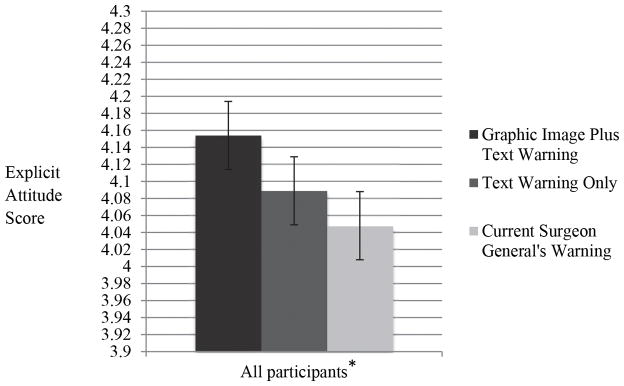
In the ANCOVA that assessed the effect of exposure to graphic warnings on explicit attitudes toward smoking, there was a main effect of cigarette package condition, F(2, 2155) = 4.27, p = .014, partial η2 = .004. As shown in Figure 3, explicit attitudes toward smoking were more negative for participants who viewed the graphic images plus text warnings (adjusted M = 4.15, se = .03) compared to participants who viewed the current U.S. Surgeon General’s text warnings (adjusted M = 4.05, se = .03), but there was no difference compared to participants who viewed the text only warnings (adjusted M = 4.09, se = .03). There were no significant interactions involving gender, race/ethnicity, or smoking status.
Figure 3.
Explicit attitude toward smoking for the three study conditions, after controlling for baseline explicit attitude toward smoking. A higher value reflects a more negative explicit attitude toward smoking.
*Mean difference p = .014.
Discussion
The current study adds to the growing literature on the effects of graphic health warnings on cigarette packages on smoking-related beliefs and attitudes. Importantly, this is one of the first studies to test the impact of graphic warnings on implicit attitudes toward smoking. In this ethnically and racially diverse sample of young adults, smokers exposed to packages with graphic images plus text warnings demonstrated more negative implicit attitudes than those exposed to packages with large text warnings only or with the current Surgeon General’s warnings on the side of the package. The only other study to use implicit attitudes as an outcome found no difference in IAT scores between smokers who saw packages with graphic warnings and smokers who saw packages with text-only warnings (Süssenbach et al., 2013). However, that study included only two of the nine FDA graphic warnings and did not control for pre-exposure implicit attitudes.
For explicit attitudes, both smokers and nonsmokers who were exposed to the packages with graphic images plus text warnings demonstrated more negative explicit attitudes compared to those exposed to packages with the current Surgeon General’s warnings. The finding that implicit attitudes were significantly more negative after exposure to graphic images plus text compared to text only, but explicit attitudes were not significantly different between these two conditions is consistent with research showing that implicit and explicit attitudes change based on different types of information (Rydell, McConnell, Mackie, & Strain, 2006). Specifically, explicit attitudes are more likely to change in response to verbal (i.e., text) information, but implicit attitudes are more likely to be affected by information presented outside of conscious awareness (i.e., images). Our findings are also consistent with a recent alcohol study that found that exposure to posters with pictorial and text information about binge drinking influenced young adults’ implicit but not explicit attitudes toward alcohol (Glock, Klapproth, & Müller, 2014). Similar to implicit methods, neuroimaging is more sensitive than self-report to the neurophysiological mechanisms underlying the effectiveness of information delivery. Recent functional magnetic resonance imaging data showed that the FDA graphic warnings that were rated higher in emotional reaction had greater neural activation in brain regions related to emotional memory (Wang, Lowen, Romer, Giorno, & Langleben, 2015).
These findings have important implications for future development of warning labels on cigarette packages. First, the young adults in this study who were exposed to packages with the current small Surgeon General’s warning on the side demonstrated significantly more positive implicit and explicit attitudes toward smoking compared to smokers who viewed the packages with graphic images plus text warnings. This is consistent with prior research demonstrating the ineffectiveness of the warning labels currently in use in the U.S. (Fischer et al., 1989). Second, because a goal of placing graphic health warnings on cigarette packages is to motivate smokers to quit, it is noteworthy that smokers exposed to the graphic images plus text warnings demonstrated significantly more negative implicit attitudes toward smoking. Given that dual process models suggest that influencing both implicit and explicit processes is necessary for behavior change (Wiers & Stacy, 2006), these findings are promising for the potential for graphic health warnings to impact smoking behavior among U.S. young adults.
An additional important finding was that there were no gender or race/ethnicity differences for explicit attitudes. Another study found that the FDA’s proposed warning labels were effective in influencing adult smokers’ explicit smoking-related outcomes across race/ethnicity and socioeconomic subpopulations (Cantrell et al., 2013). However, there was some evidence to suggest that the effect of the graphic warning labels on the implicit attitudes of smokers was moderated by demographic factors. Because of small cell sizes in some subgroups of smokers, we were unable to interpret these potential moderation effects. Future studies with large ethnically diverse samples of smokers are needed to determine whether effects on implicit attitudes differ based on race, ethnicity, or gender. It is important to know whether this set of warning labels is more effective for certain demographic subgroups to inform the development of future messages. In addition, subsequent studies should assess whether effects differ for light and intermittent versus heavy and daily smokers.
There are limitations to this study that should be considered. First, exposure to images of cigarette packages on a computer screen may not perfectly reflect the experience of viewing the warning labels on real cigarette packages in a natural setting. However, results of studies of actual cigarette packs with graphic health warnings have been similar to studies that presented stimuli online (Thrasher, Arillo-Santillan, et al., 2012; Thrasher, Carpenter, et al., 2012). Second, the current findings are based on a one-time exposure to all nine graphic warning labels. Future studies are needed to test the effect of multiple exposures over a long period of time. Indeed, a recently published protocol establishes a methodology for testing real-word exposure to cigarette package warnings over time (Brewer et al., 2015), and a study in which smokers carried packages with graphic warnings for one week found that smokers paid more attention to graphic than to text-only warnings, and that five of the nine warnings were associated with greater thoughts of health risks (McQueen et al., 2015). Third, race/ethnicity groups included in this study were limited to white, African American, and Hispanic. Fourth, this study did not test a graphic image-only condition. Such a condition would provide additional information to tease out the differential effects of text and images on implicit and explicit attitudes. Finally, the current study focused on attitudes, just one predictor of subsequent behavior. Studies of the type described by Brewer et al. (2015) that measure smoking behavior are needed to fully evaluate the effectiveness of graphic health warnings on cigarette packages. Even in countries where graphic health warnings have been in place, more data are needed to establish their utility in promoting smoking cessation. Indeed, there are strong critics of the use of fear appeals such as graphic warning labels to change health behaviors. Recent reviews of fear appeal research conclude that graphic warnings on cigarette packages might be counterproductive and induce a defensive reaction because the current warnings do nothing to address the efficacy of the smoker to change behavior (Peters, Ruiter, & Kok, 2013; Ruiter, Kessels, Peters, & Kok, 2014). One study of smoking-related images found that smokers were more likely to disengage as measured by reaction times supporting the argument that smokers have defensive reactions to high-threat information (Kessels, Ruiter, & Jansma, 2010). Thus, additional research is needed with warning labels that include messaging that goes beyond increasing fear and with behavioral outcomes.
Although there were limitations, this study also had strengths including the two-session protocol that allowed us to control for baseline attitudes in the models and the large racially and ethnically diverse sample of young adults. The most important contribution was the use of implicit attitudes as an outcome measure. The first study to use implicit attitudes to evaluate the impact of the FDA’s final proposed set of nine graphic health warnings on cigarette packages, our findings suggest that, for young adult smokers, cigarette packages with graphic images and text warnings will be the most effective in changing implicit attitudes toward smoking. Given the importance of implicit attitudes in predicting future smoking behavior, this finding is important as the U.S. continues to determine how to implement cigarette package labeling policies.
Acknowledgments
This work was supported by the National Institute on Drug Abuse of the National Institutes of Health under Grant DA013555 and a supplement to that grant from the Food and Drug Administration.
We thank Brian Nosek, Natarajan Sriram, and Project Implicit for their technical assistance and web site hosting services and Rachel Dowty for managing data collection.
Footnotes
Disclosure Statement
The authors have no financial disclosures to report.
References
- Ajzen I, Fishbein M. The predictions of behavior from attitudinal and normative variables. Journal of Experimental Social Psychology. 1970;6:466–487. doi: 10.1016/0022-1031(70)90057-0. [DOI] [Google Scholar]
- Albert D, Steinberg L. Judgment and decision making in adolescence. Journal of Research on Adolescence. 2011;21:211–224. doi: 10.1111/j.1532-7795.2010.00724.x. [DOI] [Google Scholar]
- Borland R, Wilson N, Fong GT, Hammond D, Cummings KM, Yong HH, McNeill A. Impact of graphic and text warnings on cigarette packs: Findings from four countries over five years. Tobacco Control. 2009;18:358–364. doi: 10.1136/tc.2008.028043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Hall MG, Lee JGL, Peebles K, Noar SM, Ribisl KM. Testing warning messages on smokers’ cigarette packages: A standardised protocol. Tobacco Control. 2015 doi: 10.1136/tobaccocontrol-2014-051661. Published Online First 6 January 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron LD, Pepper JK, Brewer NT. Responses of young adults to graphic warning labels for cigarette packages. Tobacco Control. 2013 doi: 10.1136/tobaccocontrol-2012-050645. Published Online First 26 April 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantrell J, Vallone DM, Thrasher JF, Nagler RH, Feirman SP, Muenz LR, Viswanath K. Impact of tobacco-related health warning labels across socioeconomic, race and ethnic groups: Results from a randomized web-based experiment. Plos One. 2013;8:e52206. doi: 10.1371/journal.pone.0052206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Annals of the New York Academy of Sciences. 2008;1124:111–126. doi: 10.1196/annals.1440.010. doi:org/10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Presson C, Sherman SJ, Edwards D. The natural history of cigarette smoking: Predicting young adult smoking outcomes from adolescent smoking patterns. Health Psychology. 1990;9:701–716. doi: 10.1037/0278-6133.27.6.819. [DOI] [PubMed] [Google Scholar]
- Chassin L, Presson C, Sherman SJ, Seo DC, Macy JT. Implicit and explicit attitudes predict smoking cessation: Moderating effects of experienced failures of control over smoking and plans to quit. Psychology of Addictive Behaviors. 2010;24:670–679. doi: 10.1037/a0021722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Houwer J, Custers R, De Clercq A. Do smokers have a negative implicit attitude toward smoking? Cognition and Emotion. 2006;20:1274–1284. doi: 10.1080/02699930500484506. [DOI] [Google Scholar]
- Deyton L, Sharfstein J, Hamburg M. Tobacco product regulation: A public health approach. New England Journal of Medicine. 2010;362:1753–1756. doi: 10.1056/NEJMp1004152. [DOI] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [PubMed] [Google Scholar]
- Fischer PM, Richards EJB, Krugman DM. Recall and eye tracking study of adolescents viewing tobacco advertisements. Journal of the American Medical Association. 1989;261:84–89. doi: 10.1001/jama.1989.03420010094040. [DOI] [PubMed] [Google Scholar]
- Glock S, Klapproth F, Müller BCN. Promoting responsible drinking? A mass media campaign affects implicit but not explicit alcohol-related cognitions and attitudes. British Journal of Health Psychology. 2014 doi: 10.1111/bjhp.12130. Published Online First: 22 December 2014. [DOI] [PubMed] [Google Scholar]
- Graham JW. Adding missing-data-relevant variables to FIML-based structural equation models. Structural Equation Modeling. 2003;10:80–100. doi: 10.1207/S15328007SEM1001_4. [DOI] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The Implicit Association Test. Journal of Personality and Social Psychology. 1998;74:1464–1480. doi: 10.1037/0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Hammond D, Fong GT, Borland R, Cummings KM, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: Findings from the International Tobacco Control Four Country Study. American Journal of Preventive Medicine. 2007;32:202–209. doi: 10.1016/j.amepre.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: Evidence from Canadian smokers. American Journal of Public Health. 2004;94:1442–1445. doi: 10.2105/AJPH.94.8.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Fong GT, McDonald PW, Cameron R, Brown KS. Impact of the graphic Canadian warning labels on adult smoking behavior. Tobacco Control. 2003;12:391–395. doi: 10.1136/tc.12.4.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D. Tobacco packaging and labeling policies under the U.S. Tobacco Control Act: Research needs and priorities. Nicotine and Tobacco Research. 2012;14:62–74. doi: 10.1093/ntr/ntr182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Reid JL, Driezen P, Boudreau C. Pictorial health warnings on cigarette packs in the United States: An experimental evaluation of the proposed FDA warnings. Nicotine and Tobacco Research. 2013;15:93–102. doi: 10.1093/ntr/nts094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husten C. Smoking cessation in young adults. American Journal of Public Health. 2007;97:1354–1356. doi: 10.2105/AJPH.2007.117358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels LTE, Ruiter RAC, Jansma BM. Increased attention but more efficient disengagement: Neuroscientific evidence for defensive processing of threatening health information. Health Psychology. 2010;29:346–354. doi: 10.1037/a0019372. [DOI] [PubMed] [Google Scholar]
- Macy JT, Chassin L, Presson CC, Sherman JW. Changing implicit attitudes toward smoking: results from a web-based approach-avoidance practice intervention. Journal of Behavioral Medicine. 2015;38:143–152. doi: 10.1007/s10865-014-9585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays D, Turner MM, Zhao X, Evans WD, Luta G, Tercyak KP. Framing pictorial cigarette warning labels to motivate young smokers to quit. Nicotine & Tobacco Research. 2014 doi: 10.1093/ntr/ntu164. Published Online First 20 August 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell AR, Rydell RJ. The Systems of Evaluation Model: A dual-systems approach to attitudes. In: Sherman JW, Gawronski B, Trope Y, editors. Dual Process Theories of the Social Mind. New York: Guilford; 2014. pp. 204–217. [Google Scholar]
- McQueen A, Kreuter MW, Boyum S, Thompson VS, Caburnay CA, Waters EA, Fu Q. Reactions to FDA-proposed graphic warning labels affixed to U.S. smokers’ cigarette packs. Nicotine and Tobacco Research. 2015;17:784–795. doi: 10.1093/ntr/ntu339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonnemaker JM, Choiniere CJ, Farrelly MC, Kamyab K, Davis KC. Reactions to graphic health warnings in the United States. Health Education Research. 2015;30:46–56. doi: 10.1093/her/cyu036. [DOI] [PubMed] [Google Scholar]
- Nosek BA, Greenwald AG, Banaji MR. Understanding and using the Implicit Association Test: II. Method variables and construct validity. Personality and Social Psychology Bulletin. 2005;31:166–180. doi: 10.1177/0146167204271418. [DOI] [PubMed] [Google Scholar]
- Peters G-JY, Ruiter RAC, Kok G. Threatening communication: A critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychology Review. 2013;7(Supplement 1):S8–S31. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiter RAC, Kessels LTE, Peters GJY, Kok G. Sixty years of fear appeal research: Current state of the evidence. International Journal of Psychology. 2014;49:63–70. doi: 10.1002/ijop.12042. [DOI] [PubMed] [Google Scholar]
- Rydell RJ, McConnell AR, Mackie DM, Strain LM. Of two minds: Forming and changing valence-inconsistent implicit and explicit attitudes. Psychological Science. 2006;71:954–958. doi: 10.1111/j.1467-9280.2006.01811.x. [DOI] [PubMed] [Google Scholar]
- R. J. Reynolds Tobacco Co., et al. v. Hamburg, et al., 823 F. Supp. 2d 36 (D.D.C 2011).
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010;57:1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Sherman SJ, Chassin L, Presson C, Seo DC, Macy J. The intergenerational transmission of implicit and explicit attitudes toward smoking: Predicting adolescent smoking initiation. Journal of Experimental Social Psychology. 2009;45:313–319. doi: 10.1016/j.jesp.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP. The Behavioral Neuroscience of Adolescence. New York: Norton; 2009. [Google Scholar]
- Steinberg L. A dual systems model of adolescent risk-taking. Developmental Psychobiology. 2010;52:216–224. doi: 10.1002/dev.20445. [DOI] [PubMed] [Google Scholar]
- Süssenbach P, Niemeier S, Glock S. Effects of and attention to graphic labels on cigarette packages. Psychology and Health. 2013;28:1192–1206. doi: 10.1080/08870446.2013.799161. [DOI] [PubMed] [Google Scholar]
- Swanson JE, Swanson E, Greenwald AG. Using the Implicit Association Test to investigate attitude-behaviour consistency for stigmatised behaviour. Cognition and Emotion. 2001;15:207–230. doi: 10.1080/0269993004200060. [DOI] [Google Scholar]
- Thrasher JF, Arillo-Santillan E, Villalobos V, Perez-Hernandez R, Hammond D, Carter J, Regalado-Piñeda J. Can pictorial warning labels on cigarette packages address smoking-related health disparities? Field experiments in Mexico to assess pictorial warning label content. Cancer Causes and Control. 2012;23(Suppl 1):69–80. doi: 10.1007/s10552-012-9899-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Carpenter MJ, Andrews JO, Gray KM, Albert AJ, Navarro A, Cummings KM. Cigarette warning label policy alternatives and smoking-related health disparities. American Journal of Preventive Medicine. 2012;43:590–600. doi: 10.1016/j.amepre.2012.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. State and County QuickFacts. 2015 Jun 8; Retreived from http://quickfacts.census.gov/qfd/states/00000.html.
- Villanti AC, Cantrell J, Pearson JL, Vallone DM, Rath JM. Perceptions and perceived impact of graphic cigarette health warning labels on smoking behavior among U.S. young adults. Nicotine and Tobacco Research. 2014;16:469–77. doi: 10.1093/ntr/ntt176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang A-L, Lowen SB, Romer D, Giorno M, Langleben DD. Emotional reaction facilitates the brain and behavioural impact of graphic cigarette warning labels in smokers. Tobacco Control. 2015 doi: 10.1136/tobaccocontrol-2014-051993. Published Online First: 6 January 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviours? Addiction. 2008;103:1562–1571. doi: 10.1111/j.1360-0443.2008.02294.x. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Stacy AW. Handbook of implicit cognition and addiction. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Yong HH, Borland R, Thrasher JF, Thompson ME, Nagelhout GE, Fong GT, Cummings KM. Mediational pathways of the impact of cigarette warning labels on quit attempts. Health Psychology. 2014;33:1410–1420. doi: 10.1037/hea0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]