Abstract
Zoonotic influenza A viruses constantly pose a health threat to humans as novel strains occasionally emerge from the avian population to cause human infections. Many past epidemic as well as pandemic strains have originated from avian species. While most viruses are restricted to their primary hosts, zoonotic strains can sometimes arise from mutations or reassortment, leading them to acquire the capability to escape host species barrier and successfully infect a new host. Phylogenetic analyses and genetic markers are useful in tracing the origins of zoonotic infections, but there are still no effective means to identify high risk strains prior to an outbreak. Here we show that distinct host tropism protein signatures can be used to identify possible zoonotic strains in avian species which have the potential to cause human infections. We have discovered that influenza A viruses can now be classified into avian, human, or zoonotic strains based on their host tropism protein signatures. Analysis of all influenza A viruses with complete proteome using the host tropism prediction system, based on machine learning classifications of avian and human viral proteins has uncovered distinct signatures of zoonotic strains as mosaics of avian and human viral proteins. This is in contrast with typical avian or human strains where they show mostly avian or human viral proteins in their signatures respectively. Moreover, we have found that zoonotic strains from the same influenza outbreaks carry similar host tropism protein signatures characteristic of a common ancestry. Our results demonstrate that the distinct host tropism protein signature in zoonotic strains may prove useful in influenza surveillance to rapidly identify potential high risk strains circulating in avian species, which may grant us the foresight in anticipating an impending influenza outbreak.
Introduction
Influenza A viruses remain a public health threat with annual recurrence of seasonal influenza viruses in addition to sporadic avian influenza outbreaks in human population as well as rare, but formidable pandemic events. While most viruses are restricted to their primary hosts, zoonotic strains can sometimes arise through mutations or reassortment events, leading them to acquire the capability to escape host species barrier and successfully infect a new host [1]. The devastating consequences resulting from these zoonotic strains are evident from the highly pathogenic H5N1 outbreaks in Asia and Africa [2,3], as well as the H7N9 outbreak in China [4,5], which carried high rates of morbidity and mortality. Zoonotic strains are therefore a serious concern and it would be prudent to identify these strains prior to an outbreak for appropriate measures to be taken.
Current influenza surveillance focuses on surveillance, detection and response following influenza outbreak [6]. Virus strains are rapidly identified and characterized antigenically as well as genetically, with phylogenetic analyses performed to trace the origins of the infections [7]. Mutations on notable species-associated genetic markers are sometimes identified to further characterize the adaptation of the virus strain from avian to mammalian hosts [8,9]. However, most of these host switch events are unique and the genetic markers may not be applied to novel strains of different subtypes. Furthermore, efficient transmission and adaptation of avian viruses to humans is a complex process involving many factors. Even with the intensive research on influenza viruses, we are still no closer to predicting zoonotic strains having the ability to cause outbreaks in human population.
As opposed to commonly used approaches focusing on molecular adaptations of interspecies transmission, we adopted a systemic approach which considers the contribution of 11 influenza virus proteins to look for host tropism protein signatures prevalent in avian, human, and zoonotic strains. In this study, we utilized an influenza host tropism prediction system to obtain independent host tropism predictions of 11 influenza virus proteins (HA, M1, M2, NA, NP, NS1, NS2, PA, PB1, PB1-F2, and PB2) [10], the results of which were concatenated to provide an overview of the underlying host tropism protein signatures for influenza virus strains. Host tropism protein signature is herein defined as an influenza viral proteome profile of 11 independent avian or human protein predictions classified by the host tropism prediction system. We thus sought out to investigate the host tropism protein signatures of all influenza A virus strains, and to examine differences in the signatures of avian, human and zoonotic strains.
Methods
Influenza protein sequences
Protein sequences of influenza A virus strains were obtained from Influenza Research Database (http://www.fludb.org) [11]. The initial dataset consists of 331,748 protein sequences of HA, M1, M2, NA, NP, NS1, NS2, PA, PB1, PB1-F2, and PB2 from 61,559 strains. Virus strains with invalid protein sequences, incomplete proteome, and sequence discrepancy were next removed. Furthermore, we observed that prediction accuracies decrease for protein sequences that are of incomplete length (S2 Fig), justifying the exclusion of these sequences from further analyses. The full host tropism protein signature analysis thus involves 12,624 avian and human-isolated strains with 11 complete full-length protein sequences.
A crucial step in this study involved identifying confirmed zoonotic influenza virus strains isolated from human patients during influenza outbreaks. We have identified a total of 126 confirmed zoonotic strains as well as a further 346 avian strains isolated from the corresponding zoonotic outbreaks as suspected zoonotic strains (Table 1, S1 Dataset). These zoonotic strains were identified based on published literature on zoonotic or avian influenza outbreaks [4,12–32], United States Center for Disease Control and Prevention (CDC) reports [33–37], as well as World Health Organization (WHO) reports [38–43].
Table 1. Summary of confirmed and suspected zoonotic strains with complete proteome identified.
| Year | Subtype | Country | Avian-isolated suspected zoonotic strains | Human-isolated confirmed zoonotic strains | Reference |
|---|---|---|---|---|---|
| 1997 | H9N2 | Hong Kong | 2 | [24] | |
| 1998 | H9N2 | China | 1 | [24] | |
| 1999 | H9N2 | China | 2 | [24] | |
| 2003 | H7N7 | Netherlands | 1 | [20] | |
| H9N2 | Hong Kong | 2 | [35] | ||
| 2004 | H5N1 | Thailand | 10 | ||
| Vietnam | 14 | [35,39] | |||
| H7N3 | Canada | 1 | [18,35] | ||
| 2005 | H5N1 | Cambodia | 1 | [39,44] | |
| China | 1 | [39,44] | |||
| Indonesia | 6 | 7 | [26,39,44] | ||
| Thailand | 24 | [39,44] | |||
| Vietnam | 46 | [39,44] | |||
| 2006 | H5N1 | Egypt | 3 | 2 | [39] |
| Indonesia | 9 | 46 | [39,45] | ||
| Iraq | 1 | [39,45] | |||
| Thailand | 7 | 1 | [39] | ||
| Turkey | 3 | [29,32,46] | |||
| Vietnam | 2 | [39] | |||
| 2007 | H3N8 | Laos | 1 | [39] | |
| H5N1 | Indonesia | 2 | 10 | [39] | |
| Laos | 16 | [39] | |||
| Nigeria | 20 | [39] | |||
| Vietnam | 51 | [39] | |||
| 2008 | H3N8 | Vietnam | 1 | [39] | |
| H5N1 | Bangladesh | 1 | [39] | ||
| China | 1 | [39] | |||
| Egypt | 18 | [39] | |||
| Vietnam | 1 | [39] | |||
| H9N2 | Hong Kong | 9 | [24] | ||
| H11N9 | Vietnam | 2 | [39] | ||
| 2009 | H5N1 | Cambodia | 1 | [39] | |
| Egypt | 6 | [39] | |||
| H9N2 | Hong Kong | 4 | [47] | ||
| H12N5 | Vietnam | 1 | [39] | ||
| 2010 | H5N1 | Cambodia | 5 | 1 | [39] |
| China | 1 | [39] | |||
| Egypt | 25 | [36,39] | |||
| 2011 | H5N1 | Bangladesh | 1 | 1 | [38,39] |
| Cambodia | 6 | 4 | [38,39] | ||
| Egypt | 13 | [38,39] | |||
| 2012 | H5N1 | Cambodia | 1 | [2] | |
| H7N3 | Mexico | 1 | [37] | ||
| 2013 | H5N1 | Cambodia | 1 | 4 | [2] |
| H7N9 | China | 32 | 31 | [40,41] | |
| Hong Kong | 1 | [40] | |||
| Taiwan | 2 | [40] | |||
| H10N8 | China | 4 | [48] | ||
| 2014 | H7N9 | China | 1 | [40,41] | |
| Total | 346 | 126 |
Host tropism protein signature analysis
The host tropism protein signature analysis was performed using an influenza host tropism protein signature prediction system (http://fluleap.bic.nus.edu.sg) [10]. The host tropism prediction system consists of 11 individual protein prediction models (HA, M1, M2, NA, NP, NS1, NS2, PA, PB1, PB1-F2 and PB2) which independently predicts the host tropism of each protein given the protein sequences. Each protein prediction model was constructed using the machine learning algorithm random forest trained on datasets of avian and human protein sequences, which were transformed into machine learning feature vectors using amino acid compositions as well as physicochemical properties. Differences in the amino acid compositions and physicochemical properties between avian and human protein sequences allowed the prediction models to accurately distinguish between avian and human proteins with a minimum of 96.57% and up to 98.62% accuracy [10]. Results from the 11 individual avian or human protein predictions could therefore be combined for each influenza virus strain, characterizing its host tropism protein signature. We then analysed the signatures based on four groups of influenza viruses: typical avian and human strains circulating in avian and human hosts respectively, confirmed zoonotic strains isolated from human patients during zoonotic outbreaks and suspected zoonotic strains isolated from avian sources during zoonotic outbreaks.
We next performed hierarchical clustering on the host tropism protein signatures of suspected and confirmed zoonotic strains. The signatures comprising of avian and human predictions for each protein were represented with binary values and standardized for comparability. The clustering was performed using Ward’s minimum variance method with Euclidean distance metric [49]. Only avian-isolated suspected zoonotic strains with at least one human protein in their signatures were included.
Results
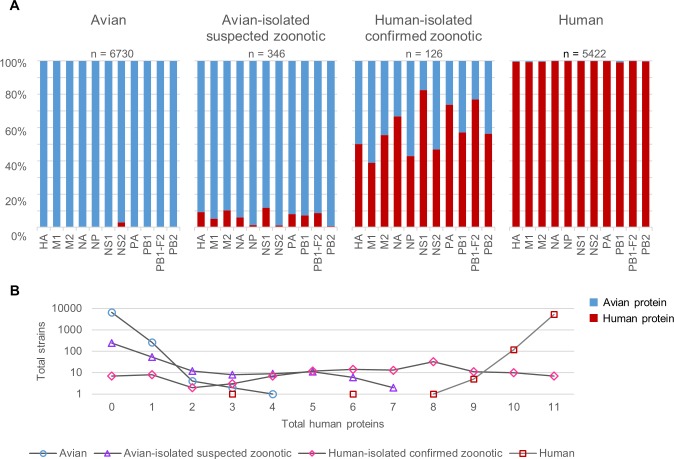
Analysis of the host tropism protein signatures show reveal indeed, there are distinct signatures between avian, human and zoonotic strains. Almost all avian strains display a unanimous signature of entirely avian proteins (Fig 1A). The percentage of avian to human predictions for each protein exceeds 99% except for NS2, where 3% of the predictions are human proteins (Fig 2A). Merely 3.86% of the avian strains have one human protein while the remaining 0.10% have at most two to four human proteins in their signatures (Fig 2B). These findings suggest that most circulating avian strains carry only avian proteins, thus rendering most of them incapable of crossing the host species barrier to freely infect a new secondary host.
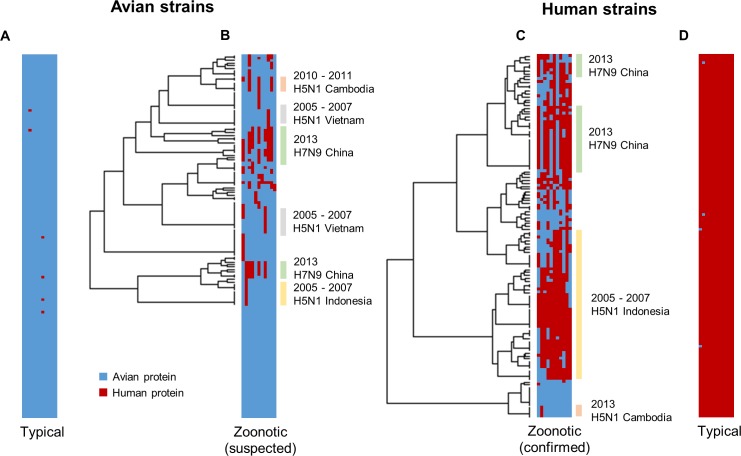
Fig 1. Host tropism protein signatures of avian, human and zoonotic strains.
Each row in the bar represents a strain, with 11 columns depicting one of each protein prediction (HA, M1, M2, NA, NP, NS1, NS2, PA, PB1, PB1-F2, and PB2). Blue column indicates an avian protein prediction while red column indicates a human protein prediction. Only a total of 146 strains are shown in each bar to match the low number of samples in confirmed zoonotic strains, with the complete result landscape illustrated in S1 Fig. (A) Typical avian strains show almost exclusive avian predictions. (B) Suspected zoonotic strains isolated from avian species during zoonotic outbreaks show slight mosaic patterns of mixed avian and human predictions. (C) Confirmed zoonotic strains isolated from human patients during zoonotic outbreaks display prominent mosaic patterns. (D) Typical human strains with almost exclusive human predictions. Hierarchical clustering shows that zoonotic strains from the same outbreaks tend to have similar signatures, with the bars indicating strains from the zoonotic outbreaks.
Fig 2. Percentage predictions and total number of human proteins for avian, human and zoonotic strains.
(A) 100% stacked bars representing total avian and human predictions for each protein in each group. (B) Total number of human proteins in the host tropism protein signatures of each group. A logarithmic scale of base 10 was applied to total samples.
Through accumulation of mutations or acquiring new gene segments from reassortment [50], avian strains may over time evolve to harbour human proteins in their proteome, as evident from the host tropism protein signatures of avian strains isolated during zoonotic outbreaks (Fig 1B). While more than half still carry the typical avian signature of 11 avian proteins and only 15.32% have one human protein in their signatures (Fig 2B), the remaining 13.87% were observed to have a combination of between two to seven human proteins (Fig 2B). Additionally, hierarchical clustering results of suspected zoonotic strains with at least one human protein reveal that strains isolated from the same outbreaks share similar host tropism protein signatures. These findings suggest that some of these avian strains could be the possible source of zoonotic infections.
We next speculate that as these avian strains evolve to acquire more human features in their proteins, they may eventually escape their primary host species barrier and successfully infect human hosts. This can be observed in the host tropism protein signatures of confirmed zoonotic strains isolated from human hosts during outbreaks (Fig 1C), where in contrast to typical avian and human strains, these zoonotic strains clearly display a mosaic of mixed avian and human proteins. Consistent with earlier clustering results of suspected zoonotic strains, strains isolated from the same zoonotic outbreaks were clustered in the same groups (Fig 1C). This therefore strongly indicates that zoonotic strains isolated from the same outbreak exhibit similar host tropism protein signatures.
The ratio of human to avian protein predictions increased tremendously for confirmed zoonotic strains as compared to suspected zoonotic strains, with as many as five proteins (M2, NA, NS1, PA, PB1-F2) having more than 50% human predictions (Fig 2A). Different human to avian protein prediction ratios signifies that some proteins may play more important roles than others in host switch events. It comes as no surprise that proteins with the least percentage of human predictions were M1 and NP (Fig 2A), which serve primarily structural roles within the virus [51]. Perhaps the more astonishing of which is that well-known protein determinants of host adaptation such as HA and PB2 were not among the top proteins with the most human predictions, but rather, NS1 and PB1-F2 with less characterized roles in interspecies transmission (Fig 2A).
HA has long been acknowledged as a crucial protein determinant in cross-species transmission, with the specificity for different types of sialic acid species determining binding to avian or human host receptors [52–54]. However, we observed here that only 50% of the confirmed zoonotic strains have human HA (Fig 2A), noting that it is not a requirement for a switch in receptor specificity for efficient transmission to humans, a sentiment also echoed by recent studies [1]. Similarly, the PB2 polymerase protein, especially at position 627 [9,55], has been identified as another critical determinant of host range, affecting efficient viral transcription and replication in host cells [56]. Yet only slightly more than half of the PB2 proteins in confirmed zoonotic strains were predicted as human (Fig 2A), with the other half retaining functions more similar to proteins in avian strains, the effect of which is probably compensated by other polymerase proteins.
Surprisingly, NS1 and PB1-F2 protein were predicted to be human in as much as 82.95% and 76.94% respectively of the confirmed zoonotic strains (Fig 2A), strongly supporting their major contributions in avian-to-human transmission. Despite that, both proteins are more widely known to be associated with virulence and pathogenicity [57,58], with their roles in host range restriction uncertain. Nevertheless, NS1 functions to inhibit host immune response and there are studies suggesting that efficiency in controlling interferon response can affect host range [59]. Based on the prevalence of human NS1 and PB1-F2 in confirmed zoonotic strains, our study highlights the importance of both proteins in interspecies transmission, even more so than previously thought. Future molecular studies are warranted to link the functions of both proteins with interspecies transmission.
Additionally, almost a third of confirmed zoonotic strains carry between five to ten human proteins in the signatures (Fig 2A), suggesting that an avian strain need not acquire all human proteins to be able to successfully infect humans. In fact, this further highlights the complexity of interspecies transmission, whereby it requires the contribution of more than a single protein to grant a virus the ability to escape host species barrier. We are therefore required to move on from relying heavily on single markers in determining whether an avian strain has zoonotic ability, to analysing the influenza virus strain from a systems perspective by looking at all the proteins in addition to conventional analyses.
Lastly, in comparison with typical avian strains, the reversed can be observed for human strains, with almost all showing a signature of 11 exclusive human proteins. There were only 2.19% of the human strains with one avian protein, and the remaining 0.15% with two to eight avian proteins making up the signatures (Fig 2B). In addition, the proportion of human to avian proteins for individual protein predictions were in excess of 99% for all 11 proteins (Fig 2A). Following this finding, this strongly indicates that seasonal influenza viruses circulating in humans have well adapted to human hosts, with efficient transmission between humans.
Discussion
As evident from the results, the host tropism protein signatures distinguish between avian, human and zoonotic strains based on the number of avian and human viral proteins in the signatures, though there are rare exceptions. Closer observation of the typical avian strain reveals that a very small proportion carries a human NS2 protein (Fig 2A). This could be attributed to prediction error in which the NS2 prediction model does not distinguish between avian or human NS2 proteins as well as the other protein prediction models; or it could also imply that there is less distinction between avian and human NS2 proteins as compared to other influenza proteins. A further investigation found that human NS2 proteins in avian strains are widely distributed across 43 different influenza subtypes in various avian species (S1 Table), which seems to suggest that human NS2 protein can still function well in these avian species. The NS2 or nuclear export protein (NEP), functions to mediate export of viral ribonucleoprotein (vRNP) complexes from host nucleus, as well as control viral RNA accumulation in host cells [60,61]. While it is still unclear if NS2 plays any important role in interspecies transmission of influenza virus, further sequence analysis or molecular studies can perhaps shed light to this interesting observation.
Yet another observation from the results is that proteins from the same segment show vastly different avian-to-human prediction ratios. Contrary to common presumption that proteins from the same segment should be classified similarly, there are higher number of human viral protein predictions of M2, NS1 and PB1-F2 as compared to M1, NS2 and PB1 respectively, despite being coded on the same viral segments. This however, should not be surprising as these pairs of proteins from the same segment (M1 and M2; NS1 and NS2; PB1 and PB1-F2) were not classified purely based on sequence alone, but rather, amino acid physicochemical properties of the protein sequences [10]. As such, even though they originated from the same genomic sequence, they are structurally and functionally different [1,60,62]. Indeed, a study has shown that proteins from the same segment exhibit different evolutionary rates in which both proteins respond individually to structural constraints or selective pressures [63]. Hence, mutations in the gene segment may affect only one protein resulting in a switch in host tropism but not the other. As a result, these protein pairs may play significantly different roles in interspecies transmission, hence maintain a different range of functions in different hosts, ultimately resulting in divergent avian or human classifications. This is due to the individual host tropism classification performed independently for each protein based on the amino acid physicochemical properties observed in the training dataset. Taken together, the host tropism classification of each protein should be considered independently based on the roles they play in avian-to-human transmission of influenza A viruses.
While most zoonotic strains carry host tropism protein signatures with a mosaic of both avian and human viral proteins, there does not appear to be a consistent pattern across all zoonotic strains. Instead, viruses isolated in specific outbreaks show similar signatures. This further highlights the complexity of interspecies transmission, where molecular changes that lead to zoonosis are unique to the outbreak events. Furthermore, although more than half of the zoonotic strains carry between five to ten human viral proteins in the signatures, the signatures of seven zoonotic strains from two separate outbreaks intriguingly contain not a single human protein prediction (S1 Dataset). Such an all-avian signature could be due to prediction error limitations, or they really are avian strains. This is akin to the continuing debate over the entirely avian origin of the deadly 1918 pandemic strain [64–68]. What molecular mechanisms that such avian strains use to overcome the species barrier is yet to be elucidated. One can only speculate that in these rare instances, a non-sequence-based characteristic hitherto not used in existing prediction tools is crucial to the zoonotic process, such as another novel undiscovered viral protein coded in the viral genome, or some host-pathogen interaction too subtle to be determinable from pure sequence analysis and prediction. Nevertheless, the mosaic pattern of host tropism protein signatures can be observed in most zoonotic strains as demonstrated with the zoonotic strains from the 2013 H7N9 outbreak in China and most of the H5N1 zoonotic strains. With increased influenza surveillance and sequencing, additional training samples would increase the accuracy in host tropism classification and hopefully provide more clues in understanding the subtleties in interspecies transmission.
A crucial task following a zoonotic outbreak is to identify the source of infection. The challenge however, is to identify infected avian species which do not exhibit any clinical symptoms, such as one faced by the H7N9 outbreak in China recently [69]. From this analysis, it is evident that we can observe the underlying host tropism protein signatures of avian-isolated suspected zoonotic strains regardless of their clinical symptoms (Fig 2B). With this, we can possibly identify high risk strains in avian species carrying a zoonotic signature of mixed avian and human proteins prior to an outbreak. This could be a useful tool when coupled with adequate influenza surveillance in avian species, providing us with the opportunity for an early alert to an impending species jump into the human population.
Overall, our findings show that the host tropism protein signature is a simplified way of examining the contribution of all proteins in an influenza virus strain. It is by no means comprehensive in itself, nor does it tell with absolute certainty if a strain will be zoonotic given a specific signature. It does however, provide an additional angle from a systemic perspective which could serve to complement traditional analyses including sequence and phylogenetic analyses for more in-depth understanding of the virus. The host tropism protein signatures would therefore be most appropriate for the monitoring of influenza virus strains in the avian population, an epidemiologically useful tool for current influenza surveillance. The capability to identify zoonotic strains that could contribute to the onset of an influenza outbreak may represent a significant advantage over these strains in which we may now possibly identify high risk strains from sequence data alone. If successful, this would allow more time in anticipation of an impending influenza outbreak to reduce public health as well as economic burden.
Supporting Information
(CSV)
Each row in the bar represents a strain, with 11 columns depicting one of each protein prediction (HA, M1, M2, NA, NP, NS1, NS2, PA, PB1, PB1-F2, and PB2). Blue column indicates an avian protein prediction while red column indicate a human protein prediction. The upper panel are avian-isolated strains while the lower panel are human-isolated strains. ZA and ZH are avian-isolated suspected zoonotic strains and human-isolated confirmed zoonotic strains from influenza outbreaks.
(PDF)
The x-axis represents prediction accuracy of up to 100%, while the y-axis represents the length of the protein. The common protein lengths are represented by the red line [70]. Prediction accuracy decreases for proteins of incomplete length.
(PDF)
(PDF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.Taubenberger JK, Kash JC (2010) Influenza virus evolution, host adaptation, and pandemic formation. Cell Host Microbe 7: 440–451. 10.1016/j.chom.2010.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (2014) Cumulative number of confirmed human cases for avian influenza A(H5N1) reported to WHO, 2003–2014. Available: http://www.who.int/influenza/human_animal_interface/EN_GIP_20140727CumulativeNumberH5N1cases.pdf?ua=1
- 3.Peiris JS, de Jong MD, Guan Y (2007) Avian influenza virus (H5N1): a threat to human health. Clin Microbiol Rev 20: 243–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y, Liang W, Yang S, Wu N, Gao H, Sheng J, et al. (2013) Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet 381: 1916–1925. 10.1016/S0140-6736(13)60903-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, et al. (2013) Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 368: 1888–1897. 10.1056/NEJMoa1304459 [DOI] [PubMed] [Google Scholar]
- 6.Heymann DL, Dixon M (2013) Infections at the animal/human interface: shifting the paradigm from emergency response to prevention at source. Curr Top Microbiol Immunol 366: 207–215. 10.1007/82_2012_285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (2014) Antigenic and genetic characteristics of zoonotic influenza viruses and development of candidate vaccine viruses for pandemic preparedness. Available: http://www.who.int/influenza/resources/documents/201009_H5_H9_VaccineVirusUpdate.pdf [PubMed]
- 8.Chen GW, Chang SC, Mok CK, Lo YL, Kung YN, Huang JH, et al. (2006) Genomic signatures of human versus avian influenza A viruses. Emerg Infect Dis 12: 1353–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steel J, Lowen AC, Mubareka S, Palese P (2009) Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog 5: e1000252 10.1371/journal.ppat.1000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eng CLP, Tong JC, Tan TW (2014) Predicting host tropism of influenza A virus proteins using random forest. BMC Med Genomics 7 Suppl 3: S1 10.1186/1755-8794-7-S3-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Squires RB, Noronha J, Hunt V, Garcia-Sastre A, Macken C, Baumgarth N, et al. (2012) Influenza research database: an integrated bioinformatics resource for influenza research and surveillance. Influenza Other Respir Viruses 6: 404–416. 10.1111/j.1750-2659.2011.00331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Q, Liu DY, Yang ZQ (2013) Characteristics of human infection with avian influenza viruses and development of new antiviral agents. Acta Pharmacol Sin 34: 1257–1269. 10.1038/aps.2013.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reperant LA, Kuiken T, Osterhaus AD (2012) Adaptive pathways of zoonotic influenza viruses: from exposure to establishment in humans. Vaccine 30: 4419–4434. 10.1016/j.vaccine.2012.04.049 [DOI] [PubMed] [Google Scholar]
- 14.Harder TC, Werner O. Avian Influenza Influenza Report. Flying Publisher; 2006. [Google Scholar]
- 15.Kalthoff D, Globig A, Beer M (2010) (Highly pathogenic) avian influenza as a zoonotic agent. Vet Microbiol 140: 237–245. 10.1016/j.vetmic.2009.08.022 [DOI] [PubMed] [Google Scholar]
- 16.Tang RB, Chen HL (2013) An overview of the recent outbreaks of the avian-origin influenza A (H7N9) virus in the human. J Chin Med Assoc 76: 245–248. 10.1016/j.jcma.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 17.Shortridge KF, Zhou NN, Guan Y, Gao P, Ito T, Kawaoka Y, et al. (1998) Characterization of avian H5N1 influenza viruses from poultry in Hong Kong. Virology 252: 331–342. [DOI] [PubMed] [Google Scholar]
- 18.Tweed SA, Skowronski DM, Davies TM, Larder A, Petric M, Lees W, et al. (2004) Human illness from avian influenza H7N3, British Columbia. Emerg Infect Dis 10: 2196–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kurtz J, Manvell RJ, Banks J (1996) Avian influenza virus isolated from a woman with conjunctivitis. Lancet 348: 901–902. [DOI] [PubMed] [Google Scholar]
- 20.Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, et al. (2004) Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363: 587–593. [DOI] [PubMed] [Google Scholar]
- 21.(2007) Avian influenza A/(H7N2) outbreak in the United Kingdom. Euro Surveill 12: E070531 070532. [PubMed] [Google Scholar]
- 22.Tiensin T, Chaitaweesub P, Songserm T, Chaisingh A, Hoonsuwan W, Buranathai C, et al. (2005) Highly pathogenic avian influenza H5N1, Thailand, 2004. Emerg Infect Dis 11: 1664–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, et al. (1999) Human infection with influenza H9N2. Lancet 354: 916–917. [DOI] [PubMed] [Google Scholar]
- 24.Butt AM, Siddique S, Idrees M, Tong Y (2010) Avian influenza A (H9N2): computational molecular analysis and phylogenetic characterization of viral surface proteins isolated between 1997 and 2009 from the human population. Virol J 7: 319 10.1186/1743-422X-7-319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Butt KM, Smith GJ, Chen H, Zhang LJ, Leung YH, Xu KM, et al. (2005) Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J Clin Microbiol 43: 5760–5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kandun IN, Wibisono H, Sedyaningsih ER, Yusharmen, Hadisoedarsuno W, Purba W, et al. (2006) Three Indonesian clusters of H5N1 virus infection in 2005. N Engl J Med 355: 2186–2194. [DOI] [PubMed] [Google Scholar]
- 27.Gilsdorf A, Boxall N, Gasimov V, Agayev I, Mammadzade F, Ursu P, et al. (2006) Two clusters of human infection with influenza A/H5N1 virus in the Republic of Azerbaijan, February-March 2006. Euro Surveill 11: 122–126. [PubMed] [Google Scholar]
- 28.Yang JR, Kuo CY, Huang HY, Wu FT, Huang YL, Cheng CY, et al. (2015) Characterization of influenza A (H7N9) viruses isolated from human cases imported into Taiwan. PLoS ONE 10: e0119792 10.1371/journal.pone.0119792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ceyhan M, Yildirim I, Ferraris O, Bouscambert-Duchamp M, Frobert E, Uyar N, et al. (2010) Serosurveillance study on transmission of H5N1 virus during a 2006 avian influenza epidemic. Epidemiol Infect 138: 1274–1280. 10.1017/S095026880999166X [DOI] [PubMed] [Google Scholar]
- 30.To KK, Song W, Lau SY, Que TL, Lung DC, Hung IF, et al. (2014) Unique reassortant of influenza A(H7N9) virus associated with severe disease emerging in Hong Kong. J Infect 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arzey GG, Kirkland PD, Arzey KE, Frost M, Maywood P, Conaty S, et al. (2012) Influenza virus A (H10N7) in chickens and poultry abattoir workers, Australia. Emerg Infect Dis 18: 814–816. 10.3201/eid1805.111852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oner AF, Bay A, Arslan S, Akdeniz H, Sahin HA, Cesur Y, et al. (2006) Avian influenza A (H5N1) infection in eastern Turkey in 2006. N Engl J Med 355: 2179–2185. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (1997) Isolation of avian influenza A(H5N1) viruses from humans—Hong Kong, May-December 1997. MMWR Morb Mortal Wkly Rep 46: 1204–1207. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (2003) Update: influenza activity—United States and worldwide, 2002–03 season, and composition of the 2003–04 influenza vaccine. MMWR Morb Mortal Wkly Rep 52: 516–521. [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention (2004) Update: influenza activity—United States and worldwide, 2003–04 season, and composition of the 2004–05 influenza vaccine. MMWR Morb Mortal Wkly Rep 53: 547–552. [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (2010) Influenza activity—United States and worldwide, June 13-September 25, 2010. MMWR Morb Mortal Wkly Rep 59: 1270–1273. [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention (2012) Notes from the field: Highly pathogenic avian influenza A (H7N3) virus infection in two poultry workers—Jalisco, Mexico, July 2012. MMWR Morb Mortal Wkly Rep 61: 726–727. [PubMed] [Google Scholar]
- 38.World Health Organization (2011) Weekly epidemiological report. Available: http://www.who.int/wer/2011/wer8643.pdf?ua=1
- 39.World Health Organization (2011) Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO, 2003–2011. Available: http://www.who.int/influenza/human_animal_interface/EN_GIP_LatestCumulativeNumberH5N1cases.pdf
- 40.World Health Organization (2013) Overview of the emergence and characteristics of the avian influenza A(H7N9) virus. Available: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/WHO_H7N9_review_31May13.pdf?ua=1
- 41.World Health Organization (2013) China—WHO Joint Mission on Human Infection with Avian Influenza A(H7N9) Virus. Available: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/ChinaH7N9JointMissionReport2013.pdf
- 42.World Health Organization (2014) Confirmed human cases of avian influenza A(H7N9) reported to WHO Report 13. Available: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/13_ReportWebH7N9Number_20140221.pdf?ua=1
- 43.World Health Organization (2015) H5N1 research issues. Available: http://www.who.int/influenza/human_animal_interface/avian_influenza/h5n1_research/en/
- 44.World Health Organization (2005) Avian influenza: assessing the pandemic threat. Available: http://whqlibdoc.who.int/hq/2005/WHO_CDS_2005.29.pdf
- 45.(2006) Avian influenza H5N1 detected in poultry in Nigeria, further human cases reported in Iraq, Indonesia and China. Euro Surveill 11: E060209 060201. [PubMed] [Google Scholar]
- 46.(2006) Avian influenza in Turkey: 21 confirmed human cases. Euro Surveill 11: E060119 060111. [PubMed] [Google Scholar]
- 47.World Health Organization (2010) Antigenic and genetic characteristics of influenza A(H5N1) and influenza A(H9N2) viruses and candidate vaccine viruses developed for potential use in human vaccines. Available: http://www.who.int/influenza/resources/documents/201009_H5_H9_VaccineVirusUpdate.pdf [PubMed]
- 48.World Health Organization (2014) Avian influenza A (H10N8). Available: http://www.wpro.who.int/china/mediacentre/factsheets/h10n8/en/
- 49.Ward JH (1963) Hierarchical Grouping to Optimize an Objective Function. Journal of the American Statistical Association 58: 236. [Google Scholar]
- 50.Richard M, de Graaf M, Herfst S (2014) Avian influenza A viruses: from zoonosis to pandemic. Future Virol 9: 513–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nayak DP, Balogun RA, Yamada H, Zhou ZH, Barman S (2009) Influenza virus morphogenesis and budding. Virus Res 143: 147–161. 10.1016/j.virusres.2009.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kobasa D, Kawaoka Y (2005) Emerging influenza viruses: past and present. Curr Mol Med 5: 791–803. [DOI] [PubMed] [Google Scholar]
- 53.Matrosovich MN, Gambaryan AS, Teneberg S, Piskarev VE, Yamnikova SS, Lvov DK, et al. (1997) Avian influenza A viruses differ from human viruses by recognition of sialyloligosaccharides and gangliosides and by a higher conservation of the HA receptor-binding site. Virology 233: 224–234. [DOI] [PubMed] [Google Scholar]
- 54.Rogers GN, Paulson JC (1983) Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127: 361–373. [DOI] [PubMed] [Google Scholar]
- 55.Subbarao EK, London W, Murphy BR (1993) A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J Virol 67: 1761–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Naffakh N, Tomoiu A, Rameix-Welti MA, van der Werf S (2008) Host restriction of avian influenza viruses at the level of the ribonucleoproteins. Annu Rev Microbiol 62: 403–424. 10.1146/annurev.micro.62.081307.162746 [DOI] [PubMed] [Google Scholar]
- 57.Ayllon J, Garcia-Sastre A (2015) The NS1 protein: a multitasking virulence factor. Curr Top Microbiol Immunol 386: 73–107. 10.1007/82_2014_400 [DOI] [PubMed] [Google Scholar]
- 58.Krumbholz A, Philipps A, Oehring H, Schwarzer K, Eitner A, Wutzler P, et al. (2011) Current knowledge on PB1-F2 of influenza A viruses. Med Microbiol Immunol 200: 69–75. 10.1007/s00430-010-0176-8 [DOI] [PubMed] [Google Scholar]
- 59.Cauldwell AV, Long JS, Moncorge O, Barclay WS (2014) Viral determinants of influenza A host range. J Gen Virol 95: 1193–1210. 10.1099/vir.0.062836-0 [DOI] [PubMed] [Google Scholar]
- 60.Paterson D, Fodor E (2012) Emerging roles for the influenza A virus nuclear export protein (NEP). PLoS Pathog 8: e1003019 10.1371/journal.ppat.1003019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.O'Neill RE, Talon J, Palese P (1998) The influenza virus NEP (NS2 protein) mediates the nuclear export of viral ribonucleoproteins. EMBO J 17: 288–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hale BG, Randall RE, Ortin J, Jackson D (2008) The multifunctional NS1 protein of influenza A viruses. J Gen Virol 89: 2359–2376. 10.1099/vir.0.2008/004606-0 [DOI] [PubMed] [Google Scholar]
- 63.Ito T, Gorman OT, Kawaoka Y, Bean WJ, Webster RG (1991) Evolutionary analysis of the influenza A virus M gene with comparison of the M1 and M2 proteins. J Virol 65: 5491–5498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Antonovics J, Hood ME, Baker CH (2006) Molecular virology: was the 1918 flu avian in origin? Nature 440: E9; discussion E9-10. [DOI] [PubMed] [Google Scholar]
- 65.Gibbs MJ, Gibbs AJ (2006) Molecular virology: was the 1918 pandemic caused by a bird flu? Nature 440: E8; discussion E9-10. [DOI] [PubMed] [Google Scholar]
- 66.Reid AH, Taubenberger JK (2003) The origin of the 1918 pandemic influenza virus: a continuing enigma. J Gen Virol 84: 2285–2292. [DOI] [PubMed] [Google Scholar]
- 67.Taubenberger JK (2006) The origin and virulence of the 1918 "Spanish" influenza virus. Proc Am Philos Soc 150: 86–112. [PMC free article] [PubMed] [Google Scholar]
- 68.Vana G, Westover KM (2008) Origin of the 1918 Spanish influenza virus: a comparative genomic analysis. Mol Phylogenet Evol 47: 1100–1110. 10.1016/j.ympev.2008.02.003 [DOI] [PubMed] [Google Scholar]
- 69.Pantin-Jackwood MJ, Miller PJ, Spackman E, Swayne DE, Susta L, Costa-Hurtado M, et al. (2014) Role of poultry in the spread of novel H7N9 influenza virus in China. J Virol 88: 5381–5390. 10.1128/JVI.03689-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Krug RM, Fodor E. The virus genome and its replication In: Webster RG, Braciale TJ, Monto AS, Lamb RA, editors. Textbook of influenza. Wiley; 2013. pp. 58 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(CSV)
Each row in the bar represents a strain, with 11 columns depicting one of each protein prediction (HA, M1, M2, NA, NP, NS1, NS2, PA, PB1, PB1-F2, and PB2). Blue column indicates an avian protein prediction while red column indicate a human protein prediction. The upper panel are avian-isolated strains while the lower panel are human-isolated strains. ZA and ZH are avian-isolated suspected zoonotic strains and human-isolated confirmed zoonotic strains from influenza outbreaks.
(PDF)
The x-axis represents prediction accuracy of up to 100%, while the y-axis represents the length of the protein. The common protein lengths are represented by the red line [70]. Prediction accuracy decreases for proteins of incomplete length.
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.