Abstract
Objective
To compare and evaluate the safety and efficacy of holmium laser enucleation of the prostate (HoLEP) and simple prostatectomy for large prostate burdens, as discussion and debate continue about the optimal surgical intervention for this common pathology.
Materials and methods
A systematic search was conducted for studies comparing HoLEP with simple prostatectomy [open (OP), robot-assisted, laparoscopic] using a sensitive strategy and in accordance with Cochrane collaboration guidelines. Primary parameters of interest were objective measurements including maximum urinary flow rate (Qmax) and post-void residual urine volume (PVR), and subjective outcomes including International Prostate Symptom Score (IPSS) and quality of life (QoL). Secondary outcomes of interest included volume of tissue retrieved, catheterisation time, hospital stay, blood loss and serum sodium decrease. Data on baseline characteristics and complications were also collected. Where possible, comparable data were combined and meta-analysis was conducted.
Results
In all, 310 articles were identified and after screening abstracts (114) and full manuscripts (14), three randomised studies (263 patients) were included, which met our pre-defined inclusion criteria. All these compared HoLEP with OP. The mean transrectal ultrasonography (TRUS) volume was 113.9 mL in the HoLEP group and 119.4 mL in the OP group. There was no statistically significant difference in Qmax, PVR, IPSS and QoL at 12 and 24 months between the two interventions. OP was associated with a significantly shorter operative time (P = 0.01) and greater tissue retrieved (P < 0.001). However, with HoLEP there was significantly less blood loss (P < 0.001), patients had a shorter hospital stay (P = 0.03), and were catheterised for significantly fewer hours (P = 0.01). There were no significant differences in the total number of complications recorded amongst HoLEP and OP (P = 0.80).
Conclusion
The results of the meta-analysis have shown that HoLEP and OP possess similar overall efficacy profiles for both objective and subjective disease status outcome measures. This review shows these improvements persist to at least the 24 month follow-up point. Further randomised studies are warranted to fully determine the optimal surgical intervention for large prostate burdens.
Abbreviations: OP, open prostatectomy; HoLEP, holmium enucleation of the prostate; LASP, laparoscopic simple prostatectomy; MeSH, Medical Subject heading; Qmax, maximum urinary flow rate; PVR, post-void residual urine volume; QoL, quality of life; RASP, robot-assisted simple prostatectomy; RCT, randomised controlled trial; WMD, weighted mean difference
Keywords: HoLEP, Holmium, Lasers, Prostatectomy, BPH
Introduction
BPH is a condition, which affects ≈28% of men aged >70 years [1]. The progressive nature of this disease has been confirmed by landmark studies, such as the Olmstedt County Study [2] and Baltimore Longitudinal Study of Aging [3]. The search for the optimal surgical treatment for large prostate burdens (>80 mL) is unremitting and remains the subject of continued conjecture and debate [4]. Before the advent of endoscopic approaches, simple open prostatectomy (OP) surgery was the prerogative and still is the only option in certain developing countries [5]. Despite a decline in the number of open procedures carried out each year in western countries, it remains a core component of the urologist’s therapeutic arsenal [6].
Holmium laser enucleation of the prostate (HoLEP) is an efficient, laser-based, transurethral alternative, which is both minimally invasive and has been cited as ‘size independent’ [7]. Its application has achieved diffusion across centres worldwide with 10-year outcome data now available. While there has been increased attention towards the efficacy of HoLEP vs its endourological alternatives such as TURP and photo-selective vapourisation of the prostate, formal evaluation of HoLEP compared with simple prostatectomy [OP, laparoscopic simple prostatectomy (LASP), and robot-assisted simple prostatectomy (RASP)] remains under reported.
The objective of the present study was to systematically review the evidence and compare the efficacy and safety between HoLEP and simple prostatectomy.
Materials and methods
A systematic search was conducted according to Cochrane Collaboration guidelines and the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist [8]. The search strategy was devised to retrieve studies from electronic databases including Medline, Web of Science, Embase, and the Cochrane Central Register of Registered Trials (CENTRAL), and Scopus. The search was performed on 24 May 2015.
Specific search terms included, but were not limited to: ‘holmium’, ‘enucleation’, ‘laser surgery’, ‘open prostatectomy’, ‘laparoscopy’, ‘minimally invasive’, ‘robotic’, ‘benign prostate hyperplasia’, and ‘lower urinary tract symptoms’. Medical Subject heading (MeSH) phrases included: ‘prostatectomy’ [MeSH], ‘laser therapy’ [MeSH], ‘laparoscopy’ [MeSH], ‘robotic surgical procedures’ [MeSH], ‘prostatic hyperplasia’ [MeSH]. Phrases were combined using Boolean operators (‘AND’, ‘OR’) to augment the search. References from suitable studies were also hand searched.
Data extraction and analysis
The pre-defined inclusion criteria were for randomised controlled trials (RCTs) comparing HoLEP with any form of simple prostatectomy. The list of potentially relevant studies generated by the search was reviewed by two of the authors independently (P.J. and O.A.). The extraction of data from selected studies was performed in the same manner.
Data on baseline characteristics and complications were also collected.
Outcome measures
Primary outcomes were maximum urinary flow rate (Qmax) and post-void residual urine volume (PVR), and subjective outcomes included IPSS and quality of life (QoL).
Secondary outcomes of interest included: operative time, volume of prostate tissue retrieved, drop in haemoglobin and serum sodium levels, catheterisation time, hospital stay, and complications. Complications were grouped according to their estimated Clavien–Dindo system grade, as none of the studies implemented a formal tool for classifying complications [9]. The Martin Criteria, a validated tool for accurate and comprehensive reporting of surgical complications, was also incorporated into our evaluation [10]. Articles were analysed and labelled with a level of evidence in accordance with the Oxford Centre for Evidence Based Medicine (CEBM) [11].
Where possible, comparable data were combined and meta-analysis was performed using Cochrane software Review Manager version 5.3. Results for continuous outcomes were displayed as the mean difference with 95% CIs, where P < 0.05 was considered to indicate statistical significance. Heterogeneity was analysed using a chi-squared test and with the I2 test where I2 values of 75%, 50% and 25% correspond to high, medium and low levels of heterogeneity, respectively.
Results
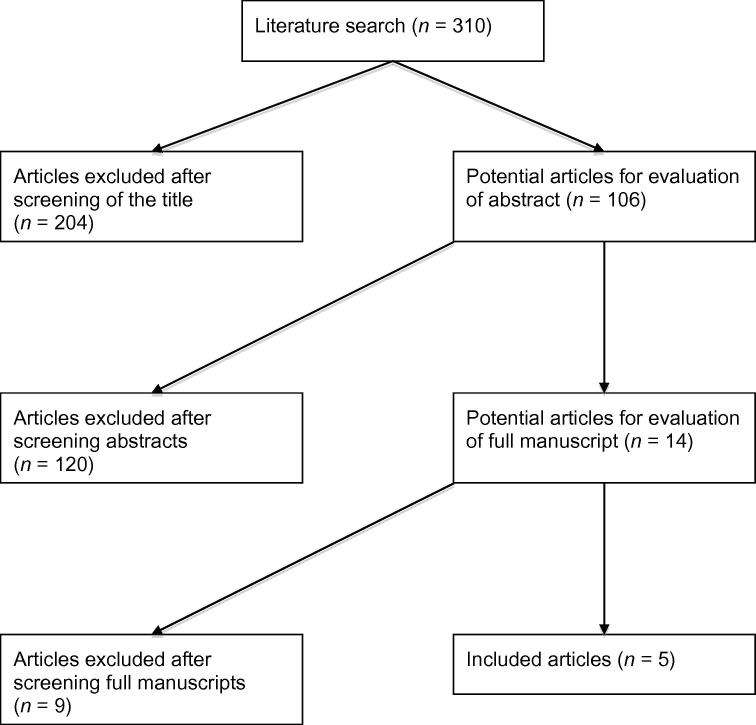
In all, 310 articles were screened, from which five publications were identified, which met our pre-defined inclusion criteria (Fig. 1) [12], [13], [14], [15], [16]. Three studies were duplicate publications of the same trial [14], [15], [16]. This resulted in a total of three trials to analyse. Each trial compared HoLEP with OP. No studies were identified, which compared HoLEP with LASP or RASP.
Figure 1.
PRISMA flowchart of literature search.
Characteristics of included studies
All studies were conducted in Europe and published between 2002 and 2008. They included 263 patients, 135 and 128 underwent HoLEP and OP, respectively. The mean age of the patients was 67.6 years in the HoLEP group and 68.8 years in the OP group. The mean TRUS volume was 113.9 mL in the HoLEP group and 119.4 mL in the OP group (Table 1).
Table 1.
Study characteristics for HoLEP vs OP.
| References | Level of evidence | Country | Journal | Sample size, n | Mean (SD) age, years | Mean (SD) TRUS volume, mL |
|---|---|---|---|---|---|---|
| Naspro et al. [12] | 2 | Italy | Eur. Urol. | 41 vs 39 | 66.26 (6.55) vs 67.27 (6.27) | 113.27 (35.33) vs 124.21 (38.52) |
| Salonia et al. [13] | 2 | Italy | Urology | 34 vs 29 | 67.4 (6.7) vs 68 (6.4) | 113.8 (37.0) vs 121.0 (34.9) |
| Kuntz et al. [14], [15], [16] | 2 | Germany | J. Urol., J. Endourol., Eur. Urol. | 60 vs 60 | 69.2 (8.4) vs 71.2 (8.3) | 114.6 (21.6) vs 113.0 (19.2) |
Primary outcomes
Clinical efficacy
-
•
Qmax
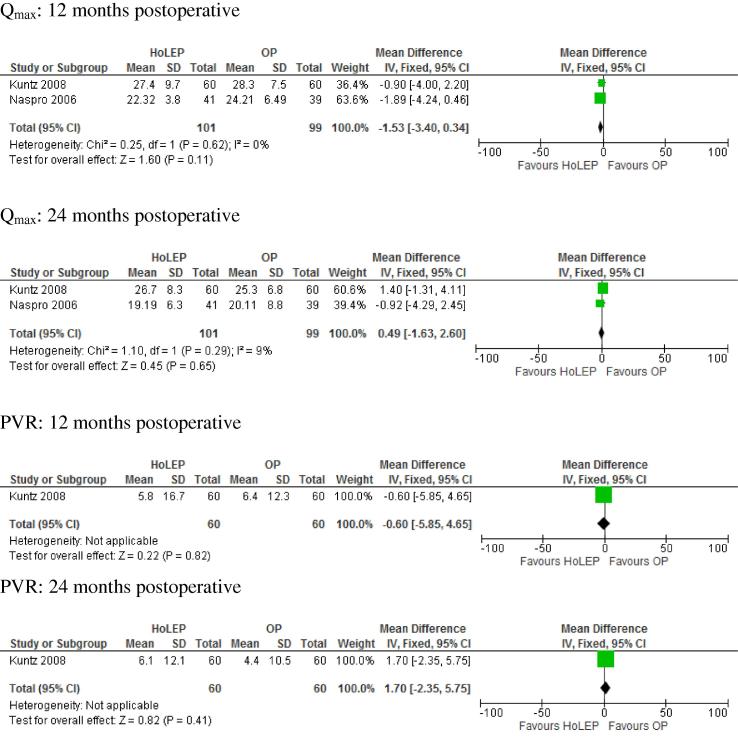
This parameter was recorded in the three studies; however, follow-up occurred in only two of these (Table 2) [12], [14], [15], [16]. Meta-analysis at 12 and 24 months showed no significant differences [12 months P = 0.11, weighted mean difference (WMD) −1.53, 95% CI −3.40 to 3.4; 24 months P = 0.65; WMD 0.49, 95% CI −1.63 to 2.6; Fig. 2).
-
•
PVR
Table 2.
Objective outcomes for HoLEP vs OP.
| Variable, mean (SD) | Naspro et al. [12] | Salonia et al. [13] | Kuntz et al. [16] |
|---|---|---|---|
| Qmax, mL/s | |||
| Before procedure | 7.83 (3.42) vs 8.32 (2.37) | 8.9 (4.2) vs 8.4 (2.4) | 3.8 (3.6) vs 3.6 (3.8) |
| At 12-month follow-up | 22.32 (3.8) vs 24.21 (6.49) | NR | 27.4 (9.7) vs 28.3 (7.5) |
| At 24-month follow-up | 19.19 (6.3) vs 20.11 (8.8) | NR | 26.7 (8.3) vs 27.4 (6.8) |
| At ⩾ 36-month follow-up | NR | NR | 27 (9.8) vs 25.3 (6.8) |
| PVR, mL | |||
| Before procedure | NR | 87.4 (83.5) vs 106.3 (71.8) | 280 (273) vs 292 (191) |
| At 12-month follow-up | NR | NR | 5.8 (16.7) vs 6.4 (12.3) |
| At 24-month follow-up | NR | NR | 1.7 (6.5) vs 2.4 (6.7) |
| At ⩾ 36-month follow-up | NR | NR | 6.1 (12.1) vs 4.4 (10.5) |
Figure 2.
Comparisons of objective outcomes.
PVR follow-up data were available for one study (Table 2). (12 months P = 0.82, WMD −0.60, 95% CI −5.85 to 4.65; 24 months P = 0.41, WMD 1.7, 95% CI –2.35 to 5.75; Fig. 2) [14], [15], [16]. This revealed no significant difference between HoLEP and OP.
-
•
IPSS
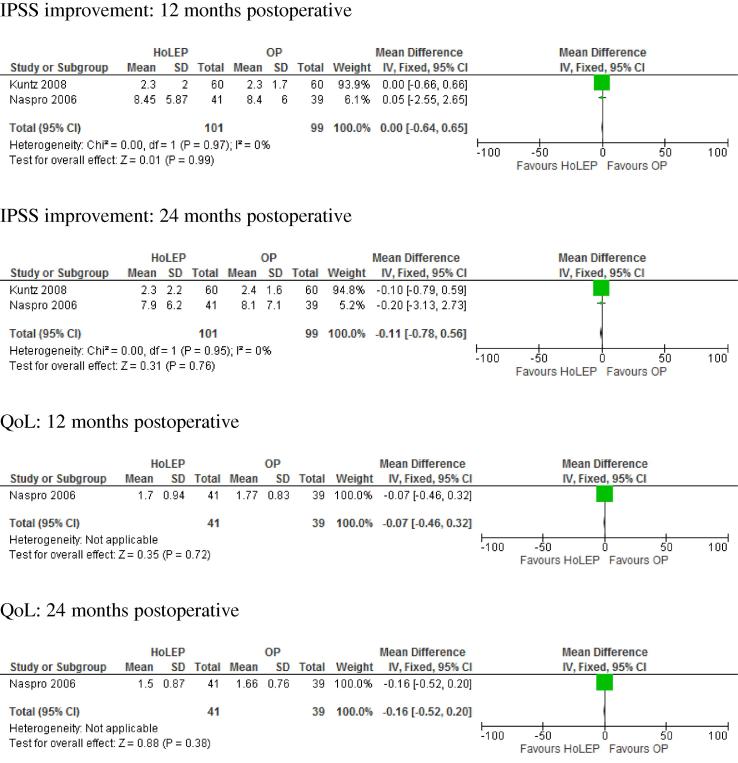
Data on IPSS were retrieved from all studies; however, follow-up data were only available for two of the studies (Table 3) [12], [14], [15], [16]. Meta-analysis of the 12 and 24 month IPSS revealed no significant differences at 12 or 24 months postoperatively (12 months P = 0.99, WMD 0.00, 95% CI −0.64 to 0.65; 24 months P = 0.76, WMD −0.11, 95% CI −0.78 to 0.56; Fig. 3).
-
•
QoL
Table 3.
Subjective outcomes for HoLEP vs OP.
| Variable, mean (SD) | Naspro et al. [12] | Salonia et al. [13] | Kuntz et al. [16] |
|---|---|---|---|
| IPSS | |||
| Before procedure | 20.11 (5.84) vs 21.6 (3.24) | 19.6 (7) vs 21.6 (3.5) | 22.1 (3.3) vs 21 (3.6) |
| At 12-month follow-up | 8.45 (5.87) vs 8.4 (6) | NR | 2.3 (2) vs 2.3 (1.7) |
| At 24-month follow-up | 7.9 (6.2) vs 8.1 (7.1) | NR | 2.3 (2.2) vs 2.4 (1.6) |
| At ⩾ 36-month follow-up | NR | NR | 3 (3.1) vs 2.8 (1.6) |
| QoL | |||
| Before procedure | 4.07 (0.93) vs 4.44 (0.96) | 4.6 (1) vs 4.4 (1) | NR |
| At 12-month follow-up | 1.7 (0.94) vs 1.77 (0.83) | NR | NR |
| At 24-month follow-up | 1.5 (0.87) vs 1.66 (0.76) | NR | |
| At ⩾ 36-month follow-up | NR | NR | |
Figure 3.
Comparisons of subjective outcomes.
Two studies recorded QoL data (143 patients) [12], [13]. Of them, only one reported QoL in the follow-up (Table 3) [2]. This did not show any significant difference at 12 and 24 months (12 months P = 0.72, WMD −0.07, 95% CI −0.46 to 0.32; 24 months P = 0.38, WMD −0.16, 95% CI −0.52 to 0.2; Fig. 3).
Secondary outcomes
-
•
Operative time
The operative time for OP was significantly shorter than for HoLEP (P = 0.01; WMD 24.86, 95% CI 5.8–43.92).
-
•
Tissue retrieved
For the volume of tissue retrieved, the results from the meta-analysis favoured OP, as this technique retrieved significantly greater volumes of tissue compared to HoLEP (P < 0.001; WMD −13.16, 95% CI −20.31 to −6.00) (Table 4) .
-
•
Decrease in haemoglobin
Table 4.
Assumed Clavien–Dindo grading of reported complications.
| Complication | Clavien–Dindo Grade | Procedure, n (%) |
|
|---|---|---|---|
| HoLEP | OP | ||
| UTI | I | – | – |
| Dysuria | I | 28 | 16 |
| Bladder mucosal injury (superficial) | I | 3 | – |
| Transitory urge incontinence | I | 19 | 23 |
| Stress incontinence | I | 1 | 1 |
| AUR | II | 8 | 5 |
| Urosepsis | II | – | – |
| Bleeding requiring blood transfusion | II | 3 | 11 |
| Bladder neck stenosis | IIIb | – | 2 |
| Urethral stricture | IIIb | 2 | 2 |
| Surgical intervention for bleeding | IIIb | 1 | – |
| Capsular perforation | IIIb | – | – |
| Myocardial infarction | IVa | – | 1 |
| Death | V | – | 1 |
| Total, n/N (%) | 65/101 (64.3) | 62/99 (62.6) | |
AUR, acute urinary retention.
Two studies provided data on haemoglobin loss. Meta-analysis showed HoLEP to result in a significantly smaller drop in haemoglobin (P < 0.001; WMD −0.95, 95% CI −1.35 to −0.56) [12], [14], [15], [16] (Table 4).
-
•
Decrease in serum sodium
One study supplied a decrease in serum sodium data, which showed no significant difference (P = 0.13; WMD −0.5, 95% CI −0.15 to 1.15) [14], [15], [16].
-
•
Catheterisation time
Two studies reported catheterisation time in hours and meta-analysis showed it to be significantly shorter in HoLEP (P = 0.01; WMD −117.36, 95% CI −208.11 to −26.62) [13], [14], [15], [16]. Naspro et al. [12] measured catheterisation time in days and the results also favoured HoLEP over OP (P < 0.001; WMD −2.60, 95% CI −2.96 to −2.24).
-
•
Hospital stay duration
For the two studies that reported the duration of hospital stay in hours, it was significantly less for HoLEP vs OP (P = 0.03; WMD −123.85, 95% CI −236.55 to −11.16) [13], [14], [15], [16]. Naspro et al. [12] reported hospital stay in days, with no significant difference found (P = 0.11; WMD −2.73, 95% CI −6.11 to 0.65).
Complications
There were no significant differences in the total number of complications recorded amongst HoLEP and OP (P = 0.80). The commonest Clavien–Dindo Grade I complication in the HoLEP group was dysuria (27.7%) and in the OP group it was transitory urge incontinence (23.2%) (Table 4). In the sub-analysis of complications according to Clavien–Dindo Grade, the only statistically significant difference was seen amongst Grade II complications, where the results of the meta-analysis favoured HoLEP (P = 0.02; WMD 0.35, 95% CI 0.15–0.82). For Grade I complications, the results favoured OP; however, this was not statistically significant. For Grade III, IV and V complications, the trend in results favoured HoLEP, but again this superiority was not statistically significant. There was one death in the OP group, with none in the HoLEP group.
Discussion
The results of the present meta-analysis suggest that HoLEP and OP possess similar overall efficacy profiles for both objective and subjective disease status outcome measures. The present review shows these improvements persist to at least the 24-month follow-up point. However, in the perioperative period, patients undergoing HoLEP spend significantly fewer hours in hospital and are catheterised for a significantly shorter period.
Efficacy and safety
While OP retrieves greater tissue volumes and carries the advantage of a shorter operative time, it is associated with a significantly greater drop in haemoglobin. Elshal et al. [17] reported that 24.5% of patients had required a blood transfusion after OP in a retrospective analysis of 163 patients at their institution. Such are the haemostatic advantages associated with HoLEP, Tyson et al. [18] determined it to be a safe alternative to TURP for patients on oral anticoagulation therapy.
The lower volumes of tissue retrieved by HoLEP may well be confounded by the effects of tissue vapourisation [19], which has been estimated to equate to an ≈10% tissue loss. Elkoushy et al. [19] recently published findings from a single-centre large series of 1216 HoLEP procedures conducted between 1998 and 2013, and recorded a re-operation-free probability of 95% at 10 years.
Complications
There were no differences in the total number of complications between the two interventions. This lack of difference in the overall complication rate may be compounded by insufficient power amongst the included studies. Across the studies, the mean rating according to Martin Criteria was 4.3/10 (Table 5). Reasons for a low score included poor evidence of risk stratification and poor indication of the method used in the studies. None of the included studies used a grading system to classify the severity of complications. Of note, Salonia et al. [13] did not report on complications at all. None of the studies recorded sexual function as an outcome measure, an important marker of disease burden and a strong determinant for patient choice of intervention. None of the studies included in the present review provided data on re-intervention for symptom recurrence.
Table 5.
Martin Criteria.
| Martin Criteria | Naspro et al. [12] | Salonia et al. [13] | Kuntz et al. [16] |
|---|---|---|---|
| Method of accruing data defined | Yes | No | Yes |
| Duration of follow-up indicated | Yes | No | Yes |
| Outpatient information included | Yes | No | Yes |
| Definitions of complications provided | Yes | No | No |
| Mortality rate and causes of death listed | No | No | Yes |
| Morbidity rate and total complications indicated | Partially | No | Yes |
| Procedure-specific complications included | Yes | No | Yes |
| Severity grade used | No | No | No |
| Length-of-stay data | Yes | Yes | Yes |
| Risk factors included in the analysis | No | No | No |
| Total criteria, n | 5 | 1 | 7 |
Cost efficacy
With the heavy economic burden of healthcare, the net cost of a surgical procedure is an important consideration. Salonia et al. [13] compared the perioperative costs for OP vs HoLEP ($3556.3 vs $2919.4). Overall, there was a percentage net cost saving of 9.6% in favour of HoLEP. HoLEP may yield financial advantages for an institution over time, especially given the potential use of the holmium: yttrium aluminium garnet (YAG) laser as a lithotripter and cost savings achieved through shorter length of stays. However, the cost burden of the initial set up is high [6]. This, as well as the specialist training required has already proved to be a barrier to the implementation of laser therapies across less developed countries [6].
Learning curve
Dialogue continues amongst urologists about the true learning curve associated with HoLEP [20]. Gilling et al. [21] have advised dissemination of formal mentorship programmes, which should incorporate elements of focused preparation, observation in theatre, and formal supervision. These tutored courses are typically only delivered by specialist centres and made possible through financial support from companies marketing HoLEP technology. Lack of such didactic opportunities has led to many surgeons adopting a self-taught method for HoLEP, which is thought to be one of the principle reasons the learning curve has been reported by many as protracted. Vincent et al. [22] have proposed that mentorship initiatives can allow the HoLEP technique to be learnt safely after 10 cases.
Strengths and limitations of the review
The main limitation of the present review was the small number of included studies. However, these were all RCTs and each with a low overall risk of bias. A further limitation is the time at which these studies were performed, which was as early as 2002. Given HoLEP was still evolving at this time and associated with a steeper learning curve compared with now, the recorded HoLEP outcomes are likely to be limited accordingly. For example, advances in morcellation technique(s) have resulted in shorter operative times. Such technology was not available for Kuntz et al. [14] at the beginning of their study; therefore the enucleated adenoma was resected using traditional techniques. Unfortunately, Kuntz et al. do not state after how many cases the morcellator was introduced. This represents the major technical difference across the studies. Moreover, information on technical points is limited across the three studies. Each study referenced the surgical technique for HoLEP described by Gilling et al. [23], [24]; however, the authors of the respective studies have provided little additional information thereafter. Only Naspro et al. [12] commented that they adopted the traditional transvesical approach for OP, the other two studies did not mention any details on it at all.
A recent matched pair analysis of 92 HoLEP and 91 transvesical OP procedures, published by Elshal et al. [25] has confirmed many of the advantages of HoLEP identified by these early randomised studies. The authors reported a median hospital stay of 2 days in the HoLEP group vs 9 days in the OP group (P < 0.001).
No studies were identified, which compared HoLEP with minimally invasive simple prostatectomy (LASP/RASP). Although clinical equipoise persists for OP and HoLEP, randomisation of open vs minimally invasive therapies is difficult to justify and is likely the principal reason the number of RCTs identified in this review was low. For the same reasons, it is likely to remain this way in the future. Whether the urology community settles with this or goes on to carry out formal randomisation of RASP or LASP vs OP for large prostate burdens remains to be determined. The method itself of true blunt enucleation performed during HoLEP is comparable to that of OP using finger enucleation. However, it carries the advantages of augmented visual control of bleeding allowing for fewer complications and overall shorter hospital stay.
The present review was strengthened through its systematic approach and using methodology based on Cochrane review standards. Indeed, we think this is the first systematic review to compare simple OP and HoLEP.
Further randomised studies are warranted to fully determine the optimal surgical intervention for large prostate burdens. These should be conducted in accordance with the Consolidated Standards of Reporting Trials (CONSORT) statement and standardised grading of complications [26].
Conclusion
OP and HoLEP are both effective and durable surgical interventions for the treatment of LUTS secondary to BPH. Given the clinically relevant advantages associated with HoLEP, such as shorter catheterisation time and hospital stay, the ascendance of this viable laser therapy is likely to continue amongst the urology community. Nonetheless, over a century in clinical practice, OP remains a valuable intervention in the urologist’s armamentarium. However, with growing economic pressures and the evolution of minimally invasive therapies, its presence will potentially fade.
Conflicts of interest
None declared.
Source of funding
None.
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Girman C.J., Jacobsen S.J., Guess H.A., Oesterling J.E., Chute C.G., Panser L.A. Natural history of prostatism: relationship among symptoms, prostate volume and peak urinary flow rate. J. Urol. 1995;153:1510–1515. doi: 10.1016/s0022-5347(01)67448-2. [DOI] [PubMed] [Google Scholar]
- 2.Rhodes T., Girman C.J., Jacobsen D.J., Roberts R.O., Lieber M.M., Jacobsen S.J. Longitudinal prostate volume in a community-based sample: 7-year follow up in the Olmsted County Study of urinary symptoms and health status among men. J. Urol. 2000;163:249. (abstract 1105) [Google Scholar]
- 3.Wright E.J., Fang J., Metter E.J. Prostate-specific antigen predicts the long-term risk of prostate enlargement: results from the Baltimore Longitudinal Study of Aging. J Urol. 2002;167:2484–2488. doi: 10.1016/s0022-5347(05)65010-0. [DOI] [PubMed] [Google Scholar]
- 4.Kuntz R.M., Lehrich K., Ahyai S. Does perioperative outcome of transurethral holmium laser enucleation of the prostate depend on prostate size? J. Endourol. 2004;18:183–188. doi: 10.1089/089277904322959842. [DOI] [PubMed] [Google Scholar]
- 5.Suardi N., Gallina A., Salonia A., Briganti A., Cestari A., Guazzoni G. Open prostatectomy and the evolution of HoLEP in the management of benign prostatic hyperplasia. Minerva. Urol. Nefrol. 2009;61:301–308. [PubMed] [Google Scholar]
- 6.Tubaro A., de Nunzio C. The current role of open surgery in BPH. EAU-EBU Update Series. 2006;4:191–201. [Google Scholar]
- 7.Elzayat E.A., Habib E.I., Elhilali M.M. Holmium laser enucleation of the prostate: a size-independent new “gold standard”. Urology. 2005;66(Suppl.):108–113. doi: 10.1016/j.urology.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 9.Dindo D., Demartines N., Clavien P.A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin R.C., 2nd, Brennan M.F., Jaques D.P. Quality of complication reporting in the surgical literature. Ann. Surg. 2002;235:803–813. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. Available at: <http://www.cebm.net/index.aspx?o=5653>. Accessed October 2015.
- 12.Naspro R., Suardi N., Salonia A., Scattoni V., Guazzoni G., Colombo R. Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24-month follow-up. Eur. Urol. 2006;50:563–568. doi: 10.1016/j.eururo.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Salonia A., Suardi N., Naspro R., Mazzoccoli B., Zanni G., Gallina A. Holmium laser enucleation versus open prostatectomy for benign prostatic hyperplasia: an inpatient cost analysis. Urology. 2006;68:302–306. doi: 10.1016/j.urology.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Kuntz R., Lehrich K. Transurethral holmium laser enucleation versus transvesical open enucleation for prostate adenoma greater than 100 gm.: a randomized prospective trial of 120 patients. J. Urol. 2002;168:1465–1469. doi: 10.1016/S0022-5347(05)64475-8. [DOI] [PubMed] [Google Scholar]
- 15.Kuntz R., Lehrich K., Ahyai S. Transurethral holmium laser enucleation of the prostate compared with transvesical open prostatectomy: 18-month follow-up of a randomized trial. J. Endourol. 2004;18:189–191. doi: 10.1089/089277904322959851. [DOI] [PubMed] [Google Scholar]
- 16.Kuntz R.M., Lehrich K., Ahyai S.A. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur. Urol. 2008;53:160–166. doi: 10.1016/j.eururo.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 17.Elshal A.M., El-Nahas A.R., Barakat T.S., Elsaadany M.M., El-Hefnawy A.S. Transvesical open prostatectomy for benign prostatic hyperplasia in the era of minimally invasive surgery: perioperative outcomes of a contemporary series. Arab. J. Urol. 2013;11:362–368. doi: 10.1016/j.aju.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tyson M.D., Lerner L.B. Safety of holmium laser enucleation of the prostate in anticoagulated patients. J. Endourol. 2009;23:1343–1346. doi: 10.1089/end.2009.0013. [DOI] [PubMed] [Google Scholar]
- 19.Elkoushy M.A., Elshal A.M., Elhilali M.M. Reoperation after holmium laser enucleation of the prostate for management of benign prostatic hyperplasia: assessment of risk factors with time to event analysis. J. Endourol. 2015;29:797–804. doi: 10.1089/end.2015.0060. [DOI] [PubMed] [Google Scholar]
- 20.Robert G., Cornu J.N., Fourmarier M., Saussine C., Descazeaud A., Azzouzi A.R. Multicentre prospective evaluation of the learning curve of holmium laser enucleation of the prostate (HoLEP) BJU Int. 2015 doi: 10.1111/bju.13124. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 21.Gilling P.J. Editorial Comment on Holmium laser enucleation of prostate: outcome and complications of self-taught learning curve. Urology. 2009;73:1048–1049. doi: 10.1016/j.urology.2008.12.052. [DOI] [PubMed] [Google Scholar]
- 22.Vincent M.W., Gilling P.J. HoLEP has come of age. World J. Urol. 2015;33:487–493. doi: 10.1007/s00345-014-1443-x. [DOI] [PubMed] [Google Scholar]
- 23.Gilling P.J., Cass C.B., Cresswell M.D., Fraundorfer M.R. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology. 1996;47:48–51. doi: 10.1016/s0090-4295(99)80381-1. [DOI] [PubMed] [Google Scholar]
- 24.Tan A.H., Gilling P.J. Holmium laser prostatectomy: current techniques. Urology. 2002;60:152–156. doi: 10.1016/s0090-4295(02)01648-5. [DOI] [PubMed] [Google Scholar]
- 25.Elshal A.M., Mekkawy R., Laymon M., Barakat T.S., Elsaadany M.M., El-Assmy A. Holmium laser enucleation of the prostate for treatment for large-sized benign prostate hyperplasia; is it a realistic endourologic alternative in developing country? World J. Urol. 2015 doi: 10.1007/s00345-015-1639-8. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 26.Moher D. CONSORT: an evolving tool to help improve the quality of reports of randomized controlled trials. Consolidated standards of reporting trials. JAMA. 1998;279:1489–1491. doi: 10.1001/jama.279.18.1489. [DOI] [PubMed] [Google Scholar]