Abstract
Objective
To prospectively compare the outcome of standard mini-percutaneous nephrolithotomy (SmPCNL) versus tubeless mini-percutaneous nephrolithotomy (TmPCNL) as primary treatments of renal stones.
Patients and methods
In all, 80 patients with a solitary radio-opaque renal stone and candidates for PCNL were selected. The patients were randomly divided into two groups of 40, one group treated with SmPCNL and the other with TmPCNL. Patients and stone characters, as well as operative and postoperative data of both groups were compared and statistically analysed.
Results
There was no significant difference between the two groups for patient demographics and stone characteristics. There was no statistically significant difference between the two groups for the mean operative time, mean postoperative drop in haemoglobin, mean postoperative urine leakage, mean hospital stay, and stone-free rate. The mean (SD) postoperative dose of analgesia was statistically significantly higher in the SmPCNL group compared with the TmPCNL group, at 112.5 (48.03) versus 48.8 (43.5) mg, respectively.
Conclusion
Both procedures are safe and effective for managing renal stones, without any significant difference between the two procedures; however, the postoperative analgesic requirement is significantly higher in SmPCNL.
Abbreviations: BMI, body mass index; PCNL, percutaneous nephrolithotomy; SmPCNL, standard mini-percutaneous nephrolithotomy; TmPCNL, tubeless mini-percutaneous nephrolithotomy; ESWL, extracorporeal shockwave lithotripsy; RIRS, retrograde intrarenal surgery
Keywords: Mini-percutaneous nephrolithotomy, Tubeless percutaneous nephrolithotomy, Renal stones, Nephrostomy tube
Introduction
Renal stone disease is a persistent medical disorder with a recurrence rate of ≈50%, and consequently has a significant influence on health-related quality of life [1], [2]. Technological advances in minimally invasive surgery, e.g., extracorporeal shockwave lithotripsy (ESWL), retrograde intrarenal surgery (RIRS), and percutaneous nephrolithotomy (PCNL), have improved the efficacy and outcome of renal stone management [1], [3]. PCNL is now considered the ‘gold standard’ treatment for managing simple and complex renal stones, with a success rate of >90% [1], [4], [5]. Many modifications and refinements of the standard PCNL have been developed to decrease morbidity, analgesic requirement, and hospital stay; such as the use of a smaller working sheath and nephroscope (mini-PCNL), omitting the use of a nephrostomy tube (tubeless PCNL), sealing of the nephrostomy tract with haemostatic materials, and PCNL under regional anaesthesia [3], [4], [6].
Despite the importance of the nephrostomy tube at the end of the PCNL procedure for the drainage of the pelvicalyceal system, tamponading of the renal access tract and in allowing for a ‘second look’ if needed, there are several side-effects, such as prolonged hospital stay and pain or discomfort that are related to the size of the nephrostomy tube used [7], [5], [8].
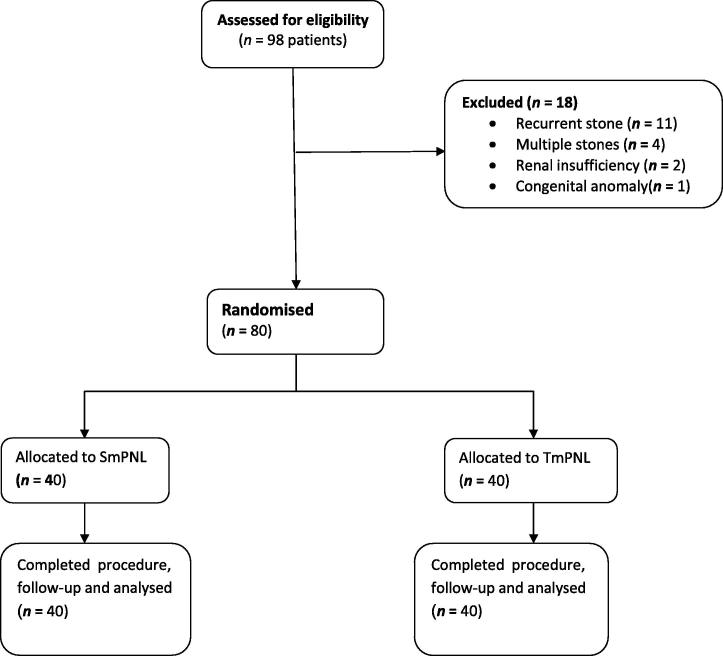
In the present study, we evaluated the tubeless mini-PCNL by comparing two groups of patients who underwent mini-PCNL, in one group we kept the nephrostomy tube, i.e., standard mini-percutaneous nephrolithotomy (SmPCNL), and in the other group the technique was tubeless mini-percutaneous nephrolithotomy (TmPCNL) (see Fig. 1).
Figure 1.
Study flow chart.
Patients and methods
Between May 2012 and June 2014, 80 patients with a solitary radio-opaque renal stone, and candidates for PCNL were included in the study. All patients were selected from the outpatient clinic of the Urology Department at Benha University Hospital, Egypt. Patients with multiple stones, previous surgery, endoscopic manoeuvres or SWL in the same kidney, congenital anomalies, coagulopathy, or renal insufficiency were not included in the study. All patients were evaluated by a full clinical history, serum creatinine, blood urea nitrogen, bleeding profile, urine culture, and radiological investigations in the form spiral CT.
The patients fulfilling the criteria of the study were divided randomly into two groups of 40 using a simple randomisation method of sealed envelopes before the procedure. The first group of patients were treated by SmPCNL and the second group underwent TmPCNL.
All procedures were performed with the patient supine under general anaesthesia. Cystoscopy was used to insert a 6-F open-tip ureteric catheter; a percutaneous puncture of the desired calyx was made under fluoroscopic guidance using an 18-G puncture needle after the injection of contrast media into the ureteric catheter to identify the pelvicalyceal system. Once the position of the needle was confirmed in the desired calyx a 0.09-cm (0.035″) J-tip guidewire was inserted into the collecting system or down the ureter under image control, the needle was then retracted and a 14-F Teflon dilator was inserted over the guidewire in a screw manner. A 14-F Amplatz sheath was inserted over the dilator and then the dilator was removed leaving the sheath in place. Using a 9.5-F Karl Storz semi-rigid 6° short ureteroscope, the stone was identified and disintegrated by pneumatic lithotripsy. The fragments were removed with stone forceps or Zero Tip™ baskets. At the end of the procedure, the pelvicalyceal system was examined, both endoscopically and radiographically, for any residual fragments or perforations. In the SmPCNL group, a 14-F nephrostomy tube was inserted and fixed to the skin and clamped for 4 h; while in the TmPCNL patients the site of the tract was closed using deep 1/0 suture.
All perioperative complications and need for analgesia were observed and recorded. A plain abdominal radiograph of the kidneys, ureters and bladder was taken in all patients 1 day after the procedures, and the nephrostomy tube was removed after confirmation of the absence of residual fragments and the ureteric catheter removed 1 day later if there was no leakage in the patients in the SmPCNL group. While in the TmPCNL group, the ureteric catheter was removed 24–72 h postoperatively, if there was no urinary leakage, then the patients were discharged and followed-up to ascertain stone-free rates.
Data were collected, tabulated, and statistically analysed and compared using SPSS software version 17. The data are expressed as the mean (SD) and number and percentage according to the type of data. The independent-samples t-test and chi-square test were used in the statistical comparison of the two groups and P values were estimated, with a P < 0.05 considered to indicate statistical significance.
The details of each procedure, and possible re-treatment, shift to another treatment, or complications had been explained to all patients. Written informed consent was signed by all patients, and the consent and study protocol were approved by the Institutional Ethics Committee.
Results
Patients and stone characteristics are presented in Table 1. There were no statistically significant differences between the SmPCNL and TmPCNL groups for the age and sex of the patients. The mean (SD) age of the patients was 46.1 (18.4) years in SmPCNL group and 40.6 (11.9) years in TmPCNL group. In SmPCNL group 67.5% of patients were male and 32.5% were female, while in the TmPCNL group 77.5% were male and 22.5% were female. Also there was no statistically significant difference between the two groups for stone size, side, and location within the kidney. The mean (SD) stone size was 1.91 (0.37) cm in SmPCNL group and 1.82 (0.36) cm in TmPCNL group. In the SmPCNL group 5% of the patients were recurrent and 4% were recurrent in the TmPCNL group, and this difference was statistically nonsignificant. There was no statistically significant difference between SmPCNL and TmPCNL groups in mean body mass index (BMI), at 30.9 (5.3) versus 32.5 (7.1) kg/m2, respectively.
Table 1.
Patients’ and stone characteristics.
| Variable | SmPCNL | TmPCNL | P |
|---|---|---|---|
| Number of patients | 40 | 40 | |
| Mean (SD): | |||
| Age (years) | 46.1 (18.4) | 40.6 (11.9) | 0.12 |
| BMI (kg/m2) | 30.9 (5.3) | 32.5 (7.1) | 0.25 |
| Stone size (cm) | 1.91 (0.37) | 1.82 (0.36) | 0.24 |
| N (%): | |||
| Sex: | 0.93 | ||
| Male | 27 (67.5) | 31 (77.5) | |
| Female | 13 (32.5) | 9 (22.5) | |
| Stone side: | 0.41 | ||
| Right | 19 (47.5) | 22 (55) | |
| Left | 21 (52.2) | 18 (45) | |
| Stone location: | 0.15 | ||
| Renal pelvis | 8 (20) | 9 (22.5) | |
| Lower calyx | 25 (62.5) | 25 (62.5) | |
| Middle calyx | 5 (12.5) | 5 (12.5) | |
| Upper calyx | 2 (5) | 1 (2.5) | |
| Recurrence: | 0.57 | ||
| De novo | 35 (87.5) | 36 (90) | |
| Recurrent | 5 (12.5) | 4 (10) | |
Operative and postoperative data are presented in Table 2. There were no statistically significant differences between the SmPCNL and TmPCNL groups for mean operative time, postoperative drop in haemoglobin, postoperative leakage, and mean hospital stay. Multiple punctures were needed in six patients (15%) in SmPCNL group and nine patients in TmPCNL group, and this difference was statistically nonsignificant (75 mg of diclofenac sodium was given when indicated). The mean (SD) dose of postoperative analgesia was statistically significantly higher in the SmPCNL group compared with the TmPCNL group, at 112.5 (48.03) versus 48.8 (43.5) mg, respectively. The stone-free rate was 82.5% in the SmPCNL group versus 90% in TmPCNL group, but this difference was statistically nonsignificant.
Table 2.
Operative and postoperative data.
| Variable | SmPCNL | TmPCNL | P |
|---|---|---|---|
| Number of patients | 40 | ||
| Punctures, n (%): | 0.09 | ||
| Single puncture | 34 (85) | 31 (77.5) | |
| Multiple punctures | 6 (15) | 9 (22.5) | |
| Mean (SD): | 40 | ||
| Operative time (min) | 46.9 (18.6) | 40.6 (11.9) | 0.08 |
| Drop in haemoglobin (g%) | 0.82 (0.3) | 0.85 (0.4) | 0.64 |
| Postoperative leakage (mL) | 86 (80.02) | 105.5 (75.1) | 0.27 |
| Postoperative analgesia (mg) | 112.5 (48.03) | 48.8 (43.5) | 0.001 |
| Hospital stay (days) | 1.07 (0.27) | 1.1 (0.3) | 0.72 |
| Stone-free status, n (%): | 0.13 | ||
| Stone free | 33 (82.5) | 37 (90) | |
| Residual stone | 7 (17.5) | 3 (10) |
Discussion
PCNL has the advantage in the management of large renal stones of decreasing morbidity and hospital stay in comparison to open surgery [7].
The placement of a nephrostomy tube is considered a standard last step in PCNL to secure haemostasis, ensuring a pre-formed tract to allow for a ‘second look’ if needed, and to maintain good drainage of the collecting system, but the tube can cause discomfort and pain, and prolong hospitalisation. To minimise the comorbidities of the nephrostomy tube, two modifications were introduced; the smaller calibre nephrostomy, i.e., mPCNL, and the tubeless technique, i.e., TmPCNL [5].
Jackman et al. [9] first reported mPCNL using 13–20 F working sheaths, and used them in adults for decreasing renal trauma and percutaneous tract size. Although this procedure affected postoperative morbidity, analgesia requirements, hospital stay, and cost, it still culminated in the placement of a nephrostomy tube, albeit smaller, which was still associated with postoperative pain, although to a lesser extent than the traditional tube.
Pietrow et al. [10] showed that the use of a smaller tube, 10 instead of 22 F, could improve comfort in the immediate postoperative period without sacrificing safety, thus giving the option to decrease the size of nephrostomy tube with proper tamponade and less postoperative pain, and may give us the advantage of not using a tube at all. From a technical point of view, the use of a smaller calibre nephrostomy reduces bleeding due to less trauma to the renal parenchyma; however, Li et al. [11] reported in their prospective study that there was no significant advantages of the mPCNL in reducing surgical trauma and associated invasiveness compared with standard PCNL.
Some urologists, such as Bellman et al. [12] decided that placement of a ureteric stent in cases of tubeless PCNL for 2–4 weeks might cause some morbidity, such as dysuria, stent migration, fever, and the need for another procedure for removal.
In our present study, we compared the effectiveness and safety of SmPCNL and TmPCNL for operative time, drop in haemoglobin, postoperative leakage, postoperative analgesia, hospital stay, and stone-free rate. In the present study, there was no statistically significant difference between the groups for the age and sex of patients, mean stone size, stone side and location, and BMI; this minimised the effect of any of them on the outcomes of the procedures, and this was matched with many studies where the preoperative characters of the randomised groups were homogenously distributed between the two study groups [13], [14].
The mean operative time was longer in the SmPCNL group than in the TmPCNL group [mean (SD) 46.9 (18.6) versus 40.6 (11.9) min, respectively] but this difference was statistically nonsignificant. In the Khairy Salem et al. [13] paediatric study, there was no statistically significant difference in operative time between the SmPCNL and TmPCNL groups, while Ni et al. [7] reported that tubeless PCNL had a reduced operative time versus standard PCNL.
For the mean postoperative drop in haemoglobin, there was a nonsignificant difference between the two groups in the present study [mean (SD) 0.82 (0.3) for SmPCNL versus 0.85 (0.4) g% for TmPCNL]. In the study of Kara et al. [15] there was no significant difference in the haematocrit values in both groups of elderly patients (3.9% for TmPCNL versus 3.2% for SmPCNL) and in the study of Khairy Salem et al. [13] there was no need for blood transfusion during or after the operation due to insignificant blood loss, and according to haemoglobin and haematocrit levels postoperatively. In the study of Shoma et al. [16], the postoperative drop in haemoglobin, the development of perinephric haematoma, and postoperative significant haematuria did not decrease with the placemat of nephrostomy tube, they reason that haemostasis after PCNL is related to the nature of the haemostatic power of the body rather than placement of the nephrostomy tube, unless there is a significant trauma or coagulopathy.
There was no statistically significant difference between the two groups for postoperative urinary leakage. In the Khairy Salem et al. [13] study, there was urine leakage in one patient in the SmPCNL group, but in the TmPCNL group urine leakage occurred in five patients (after removal of the ureteric catheter), but stopped spontaneously within 12–24 h. In the study of Kara et al. [15] none of the patients in totally (tubeless and stentless) TmPCNL group had the evidence of perinephric urinary collection on postoperative renal ultrasonography; however, Bilen et al. [14] in their study, showed that the complication rate in general was higher for TmPCNL.
Hospital stay plays an important role in the evaluation of a technique, in our present study it was lower in TmPCNL group; however, this difference was statistically nonsignificant. This result is similar to other published studies, such as in the study of Khairy Salem et al. [13] in which the mean (range) hospital stay was 1.7 (1–4) days in the TmPCNL group and 2.8 (3–4) days in the SmPCNL. Also, Zhong et al. [17] reported that the time for return to normal activity in the totally tubeless group was significantly lower than the standard PCNL group. In the study of Kara et al. [15], the mean of hospital stay was 1.5 days for TmPCNL and 3.2 days for SmPCNL, Bilen et al. [14] reported that the mean hospital stay was longer in SmPCNL versus the TmPCNL group (4.9 versus 3.1 days) and Etemadian et al. [18] in their study using adult instruments for PCNL showed a significant shorter hospital stay in the tubeless PCNL group.
In our present study, the postoperative analgesics requirement (diclofenac sodium) in the TmPCNL group was less than that of SmPCNL group [mean (SD) 48.8 (43.5) versus 112.5 (48.03) mg, respectively]. This is an advantageous feature of tubeless PCNL and has also been reported in other studies, such as that of Zhong et al. [17], as their overall results indicated that the tubeless PCNL group had a lesser analgesic requirement. In the study of Khairy Salem et al. [13], in the TmPCNL group the mean (range) pain score was 4.6 (3–6), with no need for i.v. analgesia (only oral and per rectum); however, in the SmPCNL group the mean (range) pain score was 5.5 (5–8), and i.v. analgesia was needed but only in four patients.
In the present study, there was no significant difference between the groups for the stone-free rate, this result is also similar to other published studies such as that of Ni et al. [7], who reported no significant differences between tubeless and standard PCNL. Khairy Salem et al. [13] reported all their patients were stone free except for one patient in the SmPCNL group and in the study of Bilen et al. [14], the stone-free rates were 91.6% in the tubeless and 78.5% in the standard PCNL groups.
In conclusion, both SmPCNL and TmPCNL are safe, effective, accepted procedures for the primary management of renal stones, with no significant difference between them; however, the need for postoperative analgesia is significantly higher in SmPCNL.
Conflict of interest
The authors declare that there is no conflict of interest.
Source of Funding
None.
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Ferakis N., Stavropoulos M. Mini percutaneous nephrolithotomy in the treatment of renal and upper ureteral stones: lessons learned from a review of the literature. Urol Ann. 2015;7:141–148. doi: 10.4103/0974-7796.152927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nalbant I., Ozturk U., Sener N.C., Dede O., Bayraktar A.M., Imamoglu M.A. The comparison of standard and tubeless percutaneous nephrolithotomy procedures. Int Braz J Urol. 2012;38:795–800. doi: 10.1590/1677-553820133806795. [DOI] [PubMed] [Google Scholar]
- 3.Yun S.I., Lee Y.H., Kim J.S., Cho S.R., Kim B.S., Kwon J.B. Comparative study between standard and totally tubeless percutaneous nephrolithotomy. Korean J Urol. 2012;53:785–789. doi: 10.4111/kju.2012.53.11.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonen M., Basaran B. Tubeless percutaneous nephrolithotomy: spinal versus general anesthesia. Urol J. 2014;11:1211–1215. [PubMed] [Google Scholar]
- 5.Yuan H., Zheng S., Liu L., Han P., Wang J., Wei Q. The efficacy and safety of tubeless percutaneous nephrolithotomy: a systematic review and meta-analysis. Urol Res. 2011;39:401–410. doi: 10.1007/s00240-010-0355-5. [DOI] [PubMed] [Google Scholar]
- 6.Sung Y.M., Choo S.W., Jeon S.S., Shin S.W., Park K.B., Do Y.S. The “mini-perc” technique of percutaneous nephrolithotomy with a 14-Fr peel-away sheath: 3-year results in 72 patients. Korean J Radiol. 2006;7:50–56. doi: 10.3348/kjr.2006.7.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ni S., Qiyin C., Tao W., Liu L., Jiang H., Hu H. Tubeless percutaneous nephrolithotomy is associated with less pain and shorter hospitalization compared with standard or small bore drainage. Urology. 2011;77:1293–1298. doi: 10.1016/j.urology.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 8.Isac W., Rizkala E., Liu X., Noble M., Monga M. Tubeless percutaneous nephrolithotomy: outcomes with expanded indications. Int Braz J Urol. 2014;40:204–211. doi: 10.1590/S1677-5538.IBJU.2014.02.10. [DOI] [PubMed] [Google Scholar]
- 9.Jackman S.V., Hedican S.P., Peters C.A., Docimo S.G. Percutaneous nephrolithotomy in infants and preschool age children: experience with a new technique. Urology. 1998;52:697–701. doi: 10.1016/s0090-4295(98)00315-x. [DOI] [PubMed] [Google Scholar]
- 10.Pietrow P.K., Auge B.K., Lallas C.D., Santa-Cruz R.W., Newman G.E., Albala D.M. Pain after percutaneous nephrolithotomy: impact of nephrostomy tube size. J Endourol. 2003;17:411–414. doi: 10.1089/089277903767923218. [DOI] [PubMed] [Google Scholar]
- 11.Li L.Y., Gao X., Yang M., Li J.F., Zhang H.B., Xu W.F. Does a smaller tract in percutaneous nephrolithotomy contribute to less invasiveness? A prospective comparative study. Urology. 2010;75:56–61. doi: 10.1016/j.urology.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Bellman G.C., Davidoff R., Candela J., Gerspach J., Kurtz S., Stout L. Tubeless percutaneous renal surgery. J Urol. 1997;157:1578–1582. [PubMed] [Google Scholar]
- 13.Khairy Salem H., Morsi H.A., Omran A., Daw M.A. Tubeless percutaneous nephrolithotomy in children. J Pediatr Urol. 2007;3:235–238. doi: 10.1016/j.jpurol.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 14.Bilen C.Y., Gunay M., Ozden E., Inci K., Sarikaya S., Tekgul S. Tubeless mini percutaneous nephrolithotomy in infants and preschool children: a preliminary report. J Urol. 2010;184:2498–2502. doi: 10.1016/j.juro.2010.08.039. [DOI] [PubMed] [Google Scholar]
- 15.Kara C., Resorlu B., Bayindir M., Unsal A. A randomized comparison of totally tubeless and standard percutaneous nephrolithotomy in elderly patients. Urology. 2010;76:289–293. doi: 10.1016/j.urology.2009.11.077. [DOI] [PubMed] [Google Scholar]
- 16.Shoma A.M., Elshal A.M. Nephrostomy tube placement after percutaneous nephrolithotomy: critical evaluation through a prospective randomized study. Urology. 2012;79:771–776. doi: 10.1016/j.urology.2011.09.042. [DOI] [PubMed] [Google Scholar]
- 17.Zhong Q., Zheng C., Mo J., Piao Y., Zhou Y., Jiang Q. Total tubeless versus standard percutaneous nephrolithotomy: a meta-analysis. J Endourol. 2013;27:420–426. doi: 10.1089/end.2012.0421. [DOI] [PubMed] [Google Scholar]
- 18.Etemadian M., Soleimani M.J., Haghighi R., Zeighami M.R., Najimi N. Does bleeding during percutaneous nephrolithotomy necessitate keeping the nephrostomy tube? A randomized controlled clinical trial. Urol J. 2011;8:21–26. [PubMed] [Google Scholar]