Abstract
Background
Rate of torque development (RTD) measures the ability of a muscle to produce torque quickly. Decreased quadriceps RTD may impair performance of sporting tasks after surgery. Currently, little is known about variations in quadriceps RTD between ACL reconstructed and non-injured limbs.
Purpose
To determine the differences in RTD of the quadriceps, the rate and timing of knee extensor moment (KEM) development, and knee flexion excursion during running following ACL reconstruction with patellar tendon autograft.
Study Design
Cross-Sectional
Methods
Twenty-one (11 females) subjects 6-months post-ACL reconstruction with patellar tendon autograft. (Median±IQR) age 18±4 years, mass 68.18±13.64 kg, height 1.74±0.11 m. Subjects performed four, 5-second maximal voluntary isometric strength trials of both limbs on an isokinetic dynamometer. RTD was calculated as the mean slope of the torque-time curve between 20 – 80% of total time to peak torque. Then, subjects underwent 3-D motion analysis while running on an instrumented treadmill at a self-selected running speed (mean 2.68 ± 0.28 m/s). Rate of knee extensor moment (RKEM) was calculated as the mean slope of the moment curve between 10–30% of stance phase. Between-limb comparisons were determined with a paired t-test for peak KEM, RKEM, knee flexion excursion during 10–30% of stance, and time to generate KEM.
Results
Deficits in peak rate of quadriceps torque development existed both isometrically (RTD 257.56 vs. 569.11 Nm/s, p<0.001) and dynamically (RKEM 16.47 vs. 22.38 Nm/kg*m*s, p<0.001) in the reconstructed limb. The reconstructed limb also generated a KEM later in the stance phase (11.37 vs. 9.61 % stance, p<0.001) and underwent less knee flexion excursion (15.5 vs. 19.8°, p<0.001) than the non-injured limb.
Conclusions
Following ACL reconstruction with patellar tendon autograft, patients have lower RTD and RKEM in the reconstructed limb. Deviations in RTD and the timing of the KEM can change the way the knee is loaded and potentially increases injury risk and future development of post-traumatic osteoarthritis.
Clinical Relevance
Deficits in RTD affect the ability of the limb to generate sufficient KEM at the appropriate time during dynamic tasks. Rehabilitation should consider exercises designed to improve RTD and prepare the limb for the demands of sport performance.
Key Terms: knee extensor moment, running, loading, excursion
Introduction
Over 250,000 anterior cruciate ligament (ACL) tears occur annually15, 26. Surgical reconstruction requires a lengthy period of post-operative rehabilitation, after which between 37 – 56% of individuals do not return to sport7, 8, 27. While the reasons for this are multi-factorial, one limiting factor is the incomplete return of quadriceps strength, which may persist for up to 4 years following surgery9, 21, 24, 31, 32, 35, 43. Decisions on readiness to return-to-sport following an ACL reconstruction are made, in part, by comparing the operative limb to the non-operative limb for symmetry in quadriceps strength, function, and mechanics23, 27, 28, 38, 42. While measurements of peak quadriceps strength have proven valuable, they typically do not reflect how the quadriceps functions during critical times of dynamic activity. Non-contact ACL tears occur quickly (<50 ms), while the quadriceps requires >300 ms to reach peak torque production2, 41. For this reason, alternative methods to measure quadriceps function are needed that capture the quadriceps ability to generate force quickly.
Measuring rate of torque development (RTD) of the quadriceps instead of peak strength has been proposed as one potential method to assess how quickly the muscle can generate force2, 6. Additionally, examining differences in early and late-phase RTD may provide insight as to whether reductions in RTD are due to neural or muscle physiology changes3. To date, few studies have focused on this variable following ACL reconstruction. One study found diminished RTD following an ACL reconstruction despite a full recovery of peak maximum isometric quadriceps strength6. While informative, this study used a leg press machine with the subjects performing an isometric contraction. This testing method does not isolate the quadriceps as the hip extensors and ankle plantar flexors can contribute to the torque produced. More recently, Jordan et al. (2014) used isometric knee extension to determine quadriceps RTD in 8 elite alpine ski racers after ACL reconstruction and found that RTD and peak torque were impaired in the reconstructed limb more than 2 years after surgery20. While informative, the small and highly specific sample limits the study’s generalizability. Thus, a need remains to define quadriceps RTD following an ACL reconstruction in a wider population.
Since the quadriceps are the primary active stabilizers of the knee joint during dynamic tasks10, its ability to generate force during these tasks could lend important insights into the altered mechanics often observed after ACL reconstruction that potentially predispose the patient to post-traumatic osteoarthritis5, 19. Little is known of quadriceps RTD during dynamic functional tasks such as running. Due to the timing demands of dynamic tasks, these activities require that muscles generate torque rapidly for safe and optimal performance4, 37. For this reason, RTD may be a suitable measurement of quadriceps function and reflect the ability of the quadriceps to generate torque during functional and sports tasks.
While the knee extensor moment is a surrogate measure of all forces across the knee, the contribution of the quadriceps are one of the largest modifiable components45. Therefore, determining the RTD of the knee extensor moment may provide insight into how the quadriceps function during dynamic activity. Moreover, little is known regarding the differences in timing of the knee extensor moment. Alterations in the onset of the knee extensor moment could modify the loading pattern in the knee joint during early stance. Impaired RTD could potentially delay the timing of the knee extensor moment and result in altered knee mechanics. Reduced knee flexion angle during early stance phase has been reported in walking, but this relationship was not seen in running14, 30. To date, knee flexion excursion, defined as the difference between maximum and minimum knee flexion angle during stance phase, has been relatively understudied during running and may affect the ability of the quadriceps to stabilize the knee joint and attenuate shock during higher-level tasks4, 13, 19.
Therefore, the purpose of this study was to determine if there are reductions in RTD of the quadriceps, determine between-limb differences in the rate and timing of the knee extensor moment (KEM) development, and determine between-limb differences in sagittal plane knee mechanics following an ACL reconstruction. We hypothesized that the reconstructed limb would have a lower RTD, lower rate of KEM, and decreased knee flexion excursion.
Methods
Subjects
Following a protocol approval by the university institutional review board, twenty-one recreational athletes (11 females, 10 males, age 18±4 years, mass 68.18±13.64 kg, height 1.74±0.11 m) (median±IQR) with a reconstructed ACL using a patellar tendon autograft provided their written informed consent. The subjects reported an average pre-surgery Tegner Activity Scale Rating of 9±1. An a priori power analysis based on previously published data (Jordan et al., 2015) (α=0.05, β=0.90) revealed a need for a minimum of 11 subjects for adequate statistical power to detect a 300 Nm/s difference in RTD. All participants were tested 6 months following surgery, after having completed rehabilitation, and were cleared to return to sport by a physician. Concurrent meniscus repair or meniscectomy may have been performed at time of reconstruction, but potential subjects were excluded if total knee dislocation occurred at time of injury. All ACL reconstructions were performed by 1 of 2 surgeons from the same orthopedic practice. Each subject used a standardized rehabilitation protocol, with a 4–6 week period of reduced weightbearing for those who underwent concurrent meniscectomy. Return to sport decisions were made based on performance of a battery of functional testing including hop testing, Y balance test, and strength within 80% of non-operative limb.
Rate of Torque Development
Subjects performed four, 5-second maximal voluntary isometric knee extension strength trials of both the operative and non-operative limb using a Biodex System 3 isokinetic dynamometer with a sampling rate of 30 Hz (Biodex Medical Systems, Inc., Shirley, NY, USA). An initial practice trial was allowed for each limb to familiarize the subject with the task and device. Subjects were securely situated in the dynamometer using shoulder, lap, and thigh straps to ensure joint motion did not influence the isometric contraction. All trials were performed with the knee at 90° and the hip at 85° of flexion. Maximal verbal encouragement was provided to facilitate full effort. Custom MATLAB code (MathWorks Inc., Natick, MA, USA) was used to calculate the mean slope of the torque-time curve between 20 and 80% of total time between the onset of the trial and peak torque (Figure 1). Additionally, the time-torque curve was divided into two phases: 0–100 ms (RTD1) and 100–200 ms (RTD2) to examine differences in neurological and muscular contributions to knee extensor torque, respectively (Figure 1)3. Early phase RTD (0–100 ms) is influenced by muscle fiber type, while late-phase (100–200 ms) is thought to be more influenced by neural drive1, 2, 11, 17. Data from each trial was extracted individually and a mean established for each limb for each subject.
Figure 1.
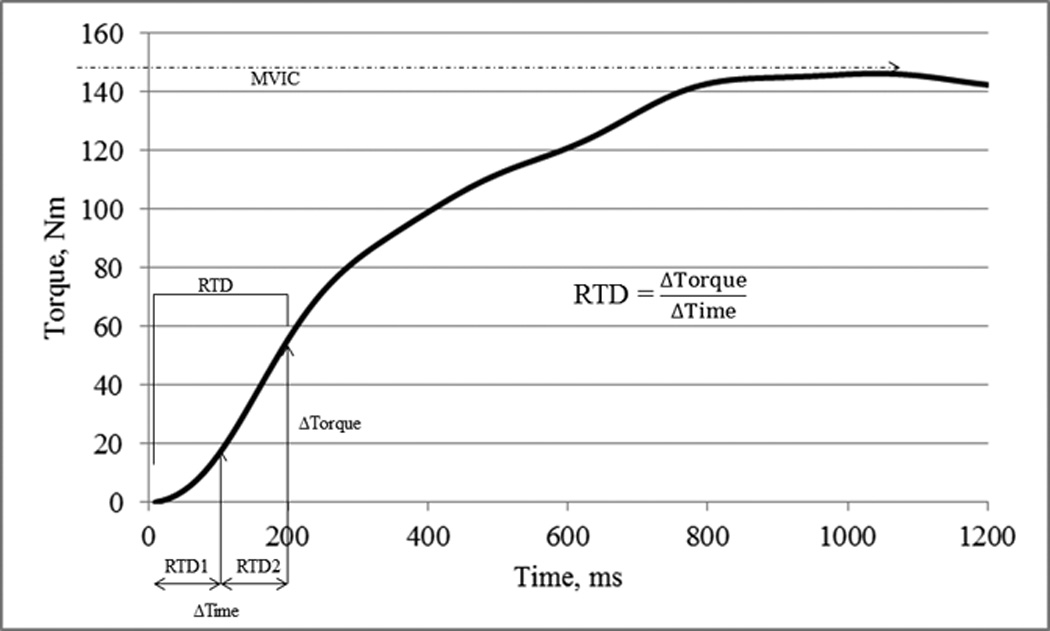
Torque-time graph from a single subject. The rate of torque development is the slope of the torque-time curve from the initiation of torque production to the respective time threshold. RTD1: 0 – 100ms, RTD2: 100 – 200 ms, RTD: 0 – 200 ms. MVIC = maximal voluntary isometric contraction.
3-D Motion Analysis
Fifty-six reflective markers were placed on the participant using a previously established configuration29: thirty-two on anatomical landmarks and twenty-four as tracking clusters. The anatomical landmarks were placed on the following locations: sternal notch, spinous process of C7, right and left superior acromion processes, posterior L5/S1, right and left superior iliac crests, right and left greater trochanters, right and left posterior superior iliac spine, right and left anterior superior iliac spines, right and left medial and lateral distal tibia, right and left medial and lateral proximal tibia, right and left medial and lateral malleoli, right and left 5th metatarsal heads, right and left 1st metatarsal head, right 2nd metatarsal head, and right and left distal foot. Tracking clusters were attached to rigid plates and secured to bilateral thigh and shank. Each plate contained 4 markers. Three tracking markers were secured to the rearfoot of each shoe to identify proximal, distal, and lateral heel locations. In order to differentiate the left and right limbs, 2 additional tracking markers were placed on the right anterior thigh and shank. All participants wore neutral running shoes (New Balance 662, New Balance Athletic Shoe Inc., Boston, MA, USA) to minimize potential alterations in mechanics due to footwear. After the participant ran a warm-up for 5 minutes, the participant ran at a self-selected test speed (2.7 ± 0.26 m/s) while marker trajectories were recorded using a 10 camera motion analysis system (Motion Analysis Corp, Santa Rosa, CA, USA) sampling at 200 Hz. Force plate data was simultaneously recorded from an instrumented Bertec treadmill (Bertec, Columbus, OH, USA) sampling at 1200 Hz.
Visual 3D software (C-motion, Germantown, MD, USA) was used to filter the data, calculate knee joint angles, and perform inverse dynamics to calculate knee joint moments. Marker trajectories were filtered at 8 Hz and the force data at 35 Hz using a fourth-order, low-pass, zero-lag Butterworth filter. The biomechanical model used has been previously described29 where angles and moments were calculated using Cardan XYZ angles referencing the distal segment to the proximal. The moments were normalized with respect to body mass and height. Custom MATLAB code was used to extract sagittal plane knee moment curves and sagittal plane knee angles. Knee moments from individual strides were analyzed for each limb in each subject. Peak KEM, percent stance of KEM onset, and rate of KEM were extracted from each stride. Percent stance of KEM onset was defined as the time percentage of the stance phase in which the KEM is greater than zero and remains above zero for the duration of the stance phase. RKEM was defined as the change in KEM divided by stance duration between 10–30% of stance, which corresponds to the most linear phase of KEM (Figure 2).
Figure 2.
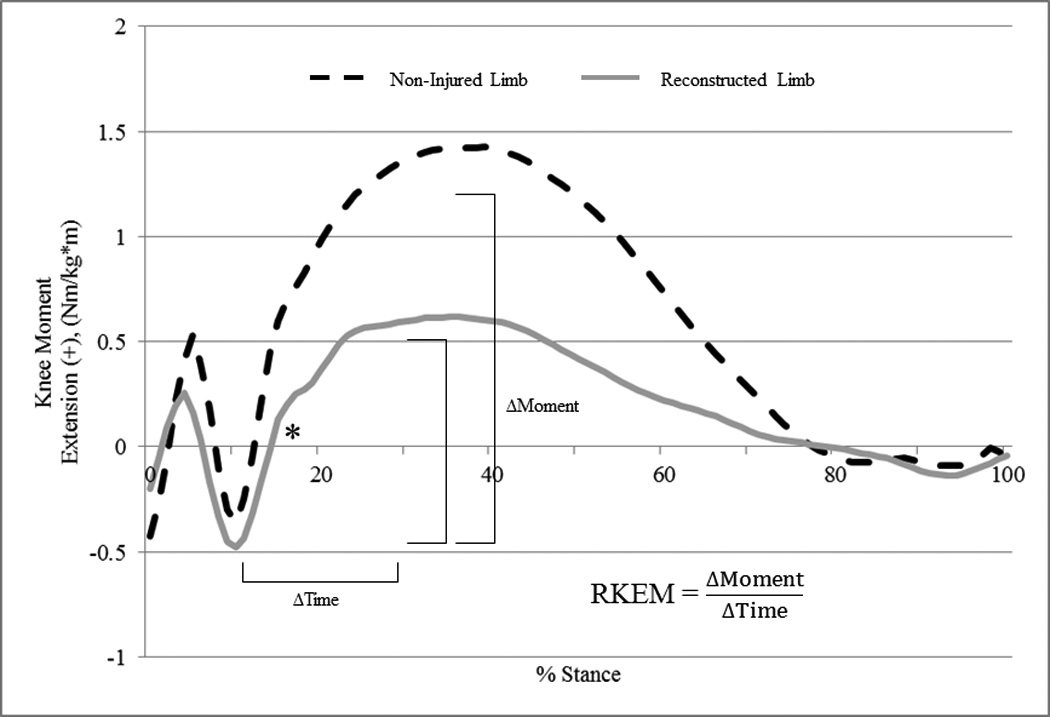
Sagittal plane knee moment from single subject demonstrating differences between ACL-reconstructed limb and non-injured limb. Rate of knee extensor moment (RKEM) is the slope of the moment-time curve between 10 – 30% of the stance phase during running. * = time, in % stance, of achievement of knee extensor moment.
Statistical Analysis
Comparisons between the operative and non-operative limb were made using SPSS (IBM Corporation, Armonk, NY, USA) software to perform two-tailed paired t-tests to compare RTDt, RTD1, RTD2, RKEM, percent stance to KEM, peak KEM, and sagittal plane knee excursion. Statistical significance was defined as p ≤ 0.05.
Results
There was a significant difference between the reconstructed limb and non-injured limb for all variables of interest (Table 1). RTD, RTD1, and RTD2 were 55%, 51%, and 57% slower, respectively, in the reconstructed limb than the non-injured limb (p<0.001) (Table 1). Additionally, the reconstructed limb demonstrated the following differences compared the injured limb: 4.5 ± 3.5° less knee flexion excursion during the stance phase of running (p<0.001), 26% reduced RKEM (p<0.001), and 15% more time to onset of KEM during stance (p<0.001) (Figure 2) (Table 1).
Table 1.
Between-Limb Comparisons: Reconstructed vs Non-Injured. Paired t-tests
| Variable | Reconstructed Limb | Non-Injured Limb | Paired T-test |
|---|---|---|---|
| RTD1 (Nm/s) | 302.40 ± 169.80 (225.11, 379.69) |
620.71 ± 223.83 (518.82, 722.60) |
<0.001* |
| RTD2 (Nm/s) | 178.10 ± 102.00 (131.67, 224.52) |
411.57 ± 141.83 (347.01, 476.13) |
<0.001* |
| RTD (Nm/s) | 257.56 ± 147.1 (190.60, 324.52) |
569.11 ± 180.68 (486.87, 651.35) |
<0.001* |
| Knee Flexion Excursion (°) | 15.5 ± 5.23 (13.12, 17.88) |
19.83 ± 4.14 (17.95, 21.71) |
<0.001* |
| Rate of KEM (Nm/kg*m*s) | 16.47 ± 5.38 (14.02, 18.92) |
22.38 ± 5.32 (19.96, 24.80) |
<0.001* |
| % stance to KEM | 11.37 ± 1.95 (10.48, 12.26) |
9.61 ± 1.59 (8.89, 10.33) |
<0.001* |
Continuous variables reported as mean ± SD. 95% CI shown in parentheses below mean ± SD.
RTD1 = Quadriceps rate of torque development 0 – 100 ms.
RTD2 = Quadriceps rate of torque development 100 – 200 ms.
RTD = Quadriceps rate of torque development 0 – 200 ms.
KEM = Knee Extensor Moment during running.
% stance to KEM = Time (in % of stance) to achievement of KEM
Significant at α=0.05.
Discussion
The purpose of this study was to determine the between limb differences in RTD of the quadriceps and the knee extensor moment during running following an ACLR with patellar tendon autograft. We found that the reconstructed limb had a significantly lower RTD of the quadriceps as compared to the non-reconstructed limb. Differences between limbs were also seen during running with decreased rate of knee extensor moment, and delayed time to generation of knee extensor moment in the reconstructed limb. These results suggest that alterations in quadriceps functional abilities persist in both the static and dynamic RTD condition, which could have implications for long term joint health and return to sport readiness.
The reduction in RTD of the quadriceps is consistent with previous reports that showed decreased quadriceps RTD up to 2 years after surgery6, 20, 22. The percent reduction was greater in our findings (55% reduction between limbs) compared to those found in previous studies (28% and 29% reduction between limbs) at 6 months after surgery and 23% reduction 2 years after surgery6, 20, 22. However, direct comparisons between this work and others are not fully possible due to the use of an isometric leg press machine to determine RTD in the previous study6. This measurement may have included contributions from the hip extensors and ankle plantar flexors, potentially depressing the full impact of reduced quadriceps RTD6. Another possible factor is the type of athlete used in the study. For example, previous studies used professional athletes while we included recreational athletes. Despite differences in the methodology and patient populations, all of these studies have reported impairment in the RTD at the time of return to sport, supporting its use to measure patient functional progress. In fact, a recent report has found that quadriceps RTD collected at 3 months post-surgery correlated with the patients’ self-reported knee function18. Thus, future work should consider the use of RTD as part of return to sport testing for athletes following an ACL reconstruction.
Our results demonstrate significant reductions in both early (RTD1) and late-phase (RTD2) quadriceps RTD. Two potential contributors to RTD are neural drive and intrinsic contractile properties of the muscle1–3, 16. For example RTD1 is believed to be more dependent upon contractile properties of muscle such as the myosin-heavy chain composition of type IIa and IIx fibers11, 17. In support of this, a moderate relationship has been reported between voluntary RTD and twitch-evoked RTD, suggesting that muscle fiber-type composition contributes to the ability of muscle to generate torque within the first 40ms of contraction3. Previous work has found that RTD2 is influenced more by neural drive via increased motor unit firing rate, which is believed to increase force summation and lead to more rapid development of isometric force1, 2. Another study showed that increases in RTD can occur even after peak isometric force is attained12. Previous findings link increases in maximal isometric strength through resistance training with increases in RTD 150–250ms after onset of muscle contraction, which overlaps with RTD2 in our sample2, 16. Since most dynamic movements require torque production within shorter time frames of 50–150ms, early phase RTD may be of greater interest41. Heavy resistance training has been demonstrated to improve both early and late-phase RTD through increased neural drive, motor unit firing, and increased muscle strength2, 16, 44. Thus, interventions targeted at improving muscle force during earlier phases of quadriceps contraction may improve impairments in quadriceps RTD overall.
We have also extended the findings of deficits in RTD to dynamic activities such as running. We have found that both the onset of the knee extensor moment and the rate of the knee extensor moment (RKEM) are delayed in the ACL reconstructed limb (Figure 2). The delay in the onset of the knee extensor moment reduces the time available for the quadriceps to generate an extensor moment to control knee flexion and absorb the knee load. Similarly, impaired RKEM demonstrates additional reductions in the ability of the quadriceps to generate an extensor moment. Interestingly, the delayed time to develop the knee extensor moment occurs during the period of the initial impact peak. Previous work by Radin et al., (1991) has shown that a lack of quadriceps contraction at heel strike resulted in higher impact forces in humans, a loading mechanism that led to joint damage in an animal model36. The reduced rate of knee extensor moment possibly further impairs load attenuation. These findings support previous work linking reduced knee extensor strength and altered gait pattern as possible contributors to accelerated development of post-traumatic osteoarthritis4, 19. However, further research is needed to define whether these factors contribute greater risk for injury and decrements in long-term joint health.
One difficulty in studying between-limb differences in a population with a unilateral injury lies in accounting for the physiological changes that occur in the non-injured limb while the injured limb recovers. Studies can be designed to partially control for this by including a healthy control group. While comparing to a control group highlights absolute differences after ACL reconstruction, the between-limb comparison gives us a relative difference within the individual, which is important in running. In a cyclic activity like running, motion of one limb can affect motion in the other as both limbs are engaged in the activity and asymmetries may contribute to unequal forces and movement patterns. Between-limb mechanical asymmetries have been reported in dynamic activities post-ACL reconstruction including running30, jumping33, and cutting25. Also, between-limb differences, especially in sagittal plane knee moments, present during jump landings after initial ACL reconstruction were predictive of second ACL injury34. Additionally, decisions regarding return-to-sport are often based upon normalizing between-limb differences23, 27, 28, 38, 42. Thus, between-limb differences help to give the clinician an understanding of the relative difference between the limbs, which can have implications for future injury risk and ability to return to sport safely.
There are limitations to the findings of this study. First, the data were collected 6 months post-ACL reconstruction. Although the findings reported in this paper are consistent with RTD reduction at 1 and 2 year post-reconstruction, the findings related to RKEM and the timing of the knee extensor moment cannot be generalized to individuals greater than 6 months after reconstruction. Additionally, this study included only subjects that underwent a reconstruction using a patellar tendon autograft. While the effects of graft type on RTD have not been established, the procedure to harvest the patellar tendon graft may impair the quadriceps of an ipsilateral bone-patellar-bone autograft differently than an allograft and hamstring graft. Due to pain and structural changes in the patella in harvesting an ipsilateral patellar tendon graft, ACL reconstructions utilizing a contralateral patellar tendon autograft have demonstrated improved between limb symmetry for quadriceps strength and knee range of motion39, 40. These findings indicate that the graft harvest site may play a role in torque production of the quadriceps independent of the presence of an ACL reconstruction.
Future studies should examine the relationship between RTD and knee mechanics during running and sport-specific tasks such as landing and cutting. Additionally, investigating the mechanics of dynamic sporting activities in an ACL-reconstructed group with normal RTD compared to a group with impaired RTD would provide better clarity to the role of RTD of the quadriceps in functional and sporting activities. Impairments in quadriceps RTD have been reported as long as 2 years post-reconstruction, however the expected time course and chronicity of impaired quadriceps RTD is unknown20. Additional knowledge of the expected duration of and the impact of reduced RTD on performance and mechanics will aid clinicians and researchers in addressing this impairment.
Conclusion
We have shown that the RTD of the quadriceps, rate and timing of knee extensor moment, and knee flexion excursion do not normalize between limbs after 6 months following ACL reconstruction with patellar tendon autograft and may be a contributing factor to unsuccessful return to sport and long-term joint health. These results suggest that additional attention should be paid to restoring normal RTD and between-limb gait mechanics prior to clearing a patient to return to sport participation.
What is known about the subject
Up to 56% of individuals do not return to sport after undergoing an ACL reconstruction. While low return-to-sport rates are multi-factorial, limited restoration of quadriceps strength is believed to be a contributing factor. RTD has been proposed as a novel method to assess how quickly a muscle can generate force and may provide more insight into quadriceps function after ACL reconstruction. To date, though, impaired quadriceps RTD following an ACL reconstruction is not well-defined and has only been investigated during isometric contractions.
What this study adds to existing knowledge
This study describes the novel findings of decreased rate of torque development both isometrically and during running. These between-limb differences highlight areas for further attention during rehabilitation in order to restore normal quadriceps function and normalize running gait prior to return-to-sport.
Acknowledgment
The authors acknowledge Anne Schmitz, PhD, for her assistance with data processing.
Footnotes
Investigation performed at the University of Kentucky, Lexington, Kentucky, USA
References
- 1.Aagaard P, Magnusson PS, Larsson B, Kjaer M, Krustrup P. Mechanical muscle function, morphology, and fiber type in lifelong trained elderly. Med Sci Sports Exerc. 2007;39(11):1989–1996. doi: 10.1249/mss.0b013e31814fb402. PMID: 17986907. [DOI] [PubMed] [Google Scholar]
- 2.Aagaard P, Simonsen EB, Andersen JL, Magnusson P, Dyhre-Poulsen P. Increased rate of force development and neural drive of human skeletal muscle following resistance training. J Appl Physiol (1985) 2002;93(4):1318–1326. doi: 10.1152/japplphysiol.00283.2002. PMID: 12235031. [DOI] [PubMed] [Google Scholar]
- 3.Andersen LL, Aagaard P. Influence of maximal muscle strength and intrinsic muscle contractile properties on contractile rate of force development. Eur J Appl Physiol. 2006;96(1):46–52. doi: 10.1007/s00421-005-0070-z. PMID: 16249918. [DOI] [PubMed] [Google Scholar]
- 4.Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009;91(Suppl 1):95–101. doi: 10.2106/JBJS.H.01408. PMID: 19182033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. PMID: 15095819. [DOI] [PubMed] [Google Scholar]
- 6.Angelozzi M, Madama M, Corsica C, et al. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):772–780. doi: 10.2519/jospt.2012.3780. PMID: 22814219. [DOI] [PubMed] [Google Scholar]
- 7.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. doi: 10.1136/bjsports-2013-093398. PMID: 25157180. [DOI] [PubMed] [Google Scholar]
- 8.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. PMID: 21398310. [DOI] [PubMed] [Google Scholar]
- 9.Beynnon BD, Johnson RJ, Naud S, et al. Accelerated versus nonaccelerated rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind investigation evaluating knee joint laxity using roentgen stereophotogrammetric analysis. Am J Sports Med. 2011;39(12):2536–2548. doi: 10.1177/0363546511422349. PMID: 21952714. [DOI] [PubMed] [Google Scholar]
- 10.Blackburn TA, Craig E. Knee anatomy: a brief review. Phys Ther. 1980;60(12):1556–1560. doi: 10.1093/ptj/60.12.1556. PMID: 7454779. [DOI] [PubMed] [Google Scholar]
- 11.Bottinelli R, Canepari M, Pellegrino MA, Reggiani C. Force-velocity properties of human skeletal muscle fibres: myosin heavy chain isoform and temperature dependence. J Physiol. 1996;495(Pt 2):573–586. doi: 10.1113/jphysiol.1996.sp021617. PMID: 8887767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buller AJ, Lewis DM. The rate of tension development in isometric tetanic contractions of mammalian fast and slow skeletal muscle. J Physiol. 1965;176:337–354. doi: 10.1113/jphysiol.1965.sp007554. PMID: 14288512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeVita P, Hortobagyi T, Barrier J. Gait biomechanics are not normal after anterior cruciate ligament reconstruction and accelerated rehabilitation. Med Sci Sports Exerc. 1998;30(10):1481–1488. doi: 10.1097/00005768-199810000-00003. PMID: 9789847. [DOI] [PubMed] [Google Scholar]
- 14.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. PMID: 23562809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79(10):1556–1576. doi: 10.2106/00004623-199710000-00014. PMID: 9378743. [DOI] [PubMed] [Google Scholar]
- 16.Hakkinen K, Alen M, Komi PV. Changes in isometric force- and relaxation-time, electromyographic and muscle fibre characteristics of human skeletal muscle during strength training and detraining. Acta Physiol Scand. 1985;125(4):573–585. doi: 10.1111/j.1748-1716.1985.tb07760.x. PMID: 4091001. [DOI] [PubMed] [Google Scholar]
- 17.Harridge SD, Bottinelli R, Canepari M, et al. Whole-muscle and single-fibre contractile properties and myosin heavy chain isoforms in humans. Pflugers Arch. 1996;432(5):913–920. doi: 10.1007/s004240050215. PMID: 8772143. [DOI] [PubMed] [Google Scholar]
- 18.Hsieh CJ, Indelicato PA, Moser MW, Vandenborne K, Chmielewski TL. Speed, not magnitude, of knee extensor torque production is associated with self-reported knee function early after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014 doi: 10.1007/s00167-014-3168-1. PMID: 25026933. [DOI] [PubMed] [Google Scholar]
- 19.Ingersoll CD, Grindstaff TL, Pietrosimone BG, Hart JM. Neuromuscular consequences of anterior cruciate ligament injury. Clin Sports Med. 2008;27(3):383–404. vii. doi: 10.1016/j.csm.2008.03.004. PMID: 18503874. [DOI] [PubMed] [Google Scholar]
- 20.Jordan MJ, Aagaard P, Herzog W. Rapid hamstrings/quadriceps strength in ACL-reconstructed elite Alpine ski racers. Med Sci Sports Exerc. 2015;47(1):109–119. doi: 10.1249/MSS.0000000000000375. PMID: 24824771. [DOI] [PubMed] [Google Scholar]
- 21.Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC. Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med. 2010;38(3):455–463. doi: 10.1177/0363546509350914. PMID: 20051501. [DOI] [PubMed] [Google Scholar]
- 22.Knezevic OM, Mirkov DM, Kadija M, Nedeljkovic A, Jaric S. Asymmetries in explosive strength following anterior cruciate ligament reconstruction. Knee. 2014;21(6):1039–1045. doi: 10.1016/j.knee.2014.07.021. PMID: 25112209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. PMID: 15049718. [DOI] [PubMed] [Google Scholar]
- 24.Lautamies R, Harilainen A, Kettunen J, Sandelin J, Kujala UM. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):1009–1016. doi: 10.1007/s00167-008-0598-7. PMID: 18712355. [DOI] [PubMed] [Google Scholar]
- 25.Lee SP, Chow JW, Tillman MD. Persons with reconstructed ACL exhibit altered knee mechanics during high-speed maneuvers. Int J Sports Med. 2014;35(6):528–533. doi: 10.1055/s-0033-1358466. PMID: 24408765. [DOI] [PubMed] [Google Scholar]
- 26.Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: A 10-year study. Knee. 2006;13(3):184–188. doi: 10.1016/j.knee.2006.01.005. PMID: 16603363. [DOI] [PubMed] [Google Scholar]
- 27.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. doi: 10.2519/jospt.2006.2222. PMID: 16776488. [DOI] [PubMed] [Google Scholar]
- 28.Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377–387. doi: 10.2519/jospt.2011.3547. PMID: 21289456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noehren B, Sanchez Z, Cunningham T, McKeon PO. The effect of pain on hip and knee kinematics during running in females with chronic patellofemoral pain. Gait Posture. 2012;36(3):596–599. doi: 10.1016/j.gaitpost.2012.05.023. PMID: 22749951. [DOI] [PubMed] [Google Scholar]
- 30.Noehren B, Wilson H, Miller C, Lattermann C. Long-term gait deviations in anterior cruciate ligament-reconstructed females. Med Sci Sports Exerc. 2013;45(7):1340–1347. doi: 10.1249/MSS.0b013e318285c6b6. PMID: 23568090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oiestad BE, Holm I, Gunderson R, Myklebust G, Risberg MA. Quadriceps muscle weakness after anterior cruciate ligament reconstruction: a risk factor for knee osteoarthritis? Arthritis Care Res (Hoboken) 2010;62(12):1706–1714. doi: 10.1002/acr.20299. PMID: 20662041. [DOI] [PubMed] [Google Scholar]
- 32.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27(3):405–424. vii–ix. doi: 10.1016/j.csm.2008.02.001. PMID: 18503875. [DOI] [PubMed] [Google Scholar]
- 33.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258–262. doi: 10.1097/JSM.0b013e31804c77ea. PMID: 17620778. [DOI] [PubMed] [Google Scholar]
- 34.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. PMID: 20702858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134(10):1417–1428. doi: 10.1007/s00402-014-1992-x. PMID: 25091127. [DOI] [PubMed] [Google Scholar]
- 36.Radin EL, Yang KH, Riegger C, Kish VL, O'Connor JJ. Relationship between lower limb dynamics and knee joint pain. J Orthop Res. 1991;9(3):398–405. doi: 10.1002/jor.1100090312. PMID: 2010844. [DOI] [PubMed] [Google Scholar]
- 37.Rouis M, Coudrat L, Jaafar H, et al. Assessment of isokinetic knee strength in elite young female basketball players: correlation with vertical jump. J Sports Med Phys Fitness. 2014 PMID: 25373468. [PubMed] [Google Scholar]
- 38.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. doi: 10.2519/jospt.2012.4194. PMID: 22813542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shelbourne KD, Beck MB, Gray T. Anterior cruciate ligament reconstruction with contralateral autogenous patellar tendon graft: evaluation of donor site strength and subjective results. Am J Sports Med. 2015;43(3):648–653. doi: 10.1177/0363546514560877. PMID: 25520302. [DOI] [PubMed] [Google Scholar]
- 40.Shelbourne KD, Urch SE. Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med. 2000;28(5):651–658. doi: 10.1177/03635465000280050501. PMID: 11032219. [DOI] [PubMed] [Google Scholar]
- 41.Stone MH, Sands WA, Carlock J, et al. The importance of isometric maximum strength and peak rate-of-force development in sprint cycling. J Strength Cond Res. 2004;18(4):878–884. doi: 10.1519/14874.1. PMID: 15574097. [DOI] [PubMed] [Google Scholar]
- 42.Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1798–1805. doi: 10.1007/s00167-011-1669-8. PMID: 21932078. [DOI] [PubMed] [Google Scholar]
- 43.Tourville TW, Jarrell KM, Naud S, Slauterbeck JR, Johnson RJ, Beynnon BD. Relationship between isokinetic strength and tibiofemoral joint space width changes after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(2):302–311. doi: 10.1177/0363546513510672. PMID: 24275860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Cutsem M, Duchateau J, Hainaut K. Changes in single motor unit behaviour contribute to the increase in contraction speed after dynamic training in humans. J Physiol. 1998;513(Pt 1):295–305. doi: 10.1111/j.1469-7793.1998.295by.x. PMID: 9782179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Winter DA. Biomechanics and Motor Control of Human Movement. 3rd ed. Hoboken, NJ, USA: John Wiley & Sons; 2005. [Google Scholar]


