Abstract
Background
Research supports the efficacy of intensive cognitive behavioral therapy (CBT) for the treatment of adolescent panic disorder with or without agoraphobia (PDA). However, little is known about the conditions under which intensive treatment is most effective. The current investigation examined the moderating roles of baseline fear and avoidance in the intensive treatment of adolescent PDA.
Methods
Adolescents with PDA (ages 11–17; N = 54) were randomized to either an intensive CBT treatment (n = 37) or a waitlist control condition (n = 17). PDA diagnosis, symptom severity, and number of feared and avoided situations were assessed at baseline and 6-week post-treatment/post-waitlist. Hierarchical regression analyses examined the relative contributions of treatment condition, number of baseline feared or avoided situations, and their interactions in the prediction of post-treatment/waitlist PDA symptoms.
Results
The main effect of intensive CBT on post-treatment PDA symptoms was not uniform across participants, with larger treatment effects found among participants with lower, relative to higher, baseline levels of fear and avoidance.
Conclusions
Findings help clarify which adolescents suffering with PDA may benefit most from an intensive treatment format.
Introduction
Panic disorder with or without agoraphobia (PDA) is a debilitating condition that commonly onsets in adolescence and early adulthood (Barlow, 2002; Beesdo, Knappe, & Pine, 2009; Grant et al., 2006; Kessler et al., 2012). Adolescents with PDA experience recurrent, unexpected panic attacks characterized by distressing physical and cognitive symptoms, including heart palpitations, nausea, difficulty breathing, dizziness, derealization, and fears of dying or losing control. These symptoms are associated with persistent fears that future panic attacks will occur, and are often accompanied by changes in behavior and daily routine – such as avoiding school, crowds, elevators, or exercise – to avoid the possibility of experiencing a panic attack (American Psychiatric Association, 2013), thus contributing to significant suffering and impairment in academic and social functioning (e.g. Diler et al., 2004; Kearney, Albano, Eisen, Allan, & Barlow, 1997; King & Bernstein, 2001; Masi, Favilla, Mucci, & Millepiedi, 2000). When left untreated, adolescent PDA places individuals at risk for continuing mental health concerns and reduced quality of life in adulthood (Comer et al., 2011; Merikangas et al., 2007; Pine, Cohen, Gurley, Brook, & Ma, 1998). Fortunately, cognitive behavioral therapy (CBT) has emerged as a supported treatment for adolescent PDA. Specifically, a developmental adaptation of Panic Control Treatment (PCT; Barlow, Craske, Cerny, & Klosko, 1989; Craske & Barlow, 2006), a well-established cognitive-behavioral intervention for PDA in adults, has shown considerable efficacy in the treatment of adolescent PDA (Hoffman & Mattis, 2000; Pincus, May, Whitton, Mattis & Barlow, 2010). Results of a randomized control trial (RCT) demonstrated that youth receiving the adolescent version of the treatment, PCT-A, showed significantly greater reductions in panic frequency and severity relative to youth in a waitlist control condition (Pincus et al., 2010).
Given limitations in the availability and accessibility of quality care for the majority of adolescents with PDA, specialty clinics have increasingly offered intensive treatment formats as an alternative for patients lacking local expert services (Angelosante, Pincus, Whitton, Cheron, & Pian, 2009). Intensive treatments may be more desirable than weekly treatment formats with respect to time commitment, travel requirements, and stigma-related concerns, without requiring the content of treatment to vary (Ehrenreich & Santucci, 2009). In addition, intensive treatments can be conducted during convenient times, such as summer or holiday breaks, and may allow families without easy access to evidence-based care to travel to a specialty clinic and devote a week or so to treatment (Angelosante et al., 2009).
Given preliminary support for the efficacy of intensive PCT for adults (Bitran, Morissette, Spiegel, & Barlow, 2008), PCT-A was adapted for delivery in an intensive format over eight consecutive days (Angelosante et al., 2009). A recent RCT demonstrated the efficacy of intensive PCT-A relative to a waitlist control condition, with 63% of adolescents treated with intensive PCT-A no longer meeting diagnostic criteria for PDA at post-treatment (Pincus et al., 2015). Intensive PCT-A has also been found to reduce the severity of comorbid anxiety disorder diagnoses not directly targeted during treatment (Gallo, Chan, Buzzella, Whitton & Pincus, 2012), and descriptive comparisons suggest intensive PCT-A shows comparable efficacy to weekly PCT-A (Chase, Whitton, & Pincus, 2012).
Despite the growing support for intensive protocols targeting adolescent PDA, as in the treatment of other anxiety problems roughly 40% of youth do not exhibit adequate symptom relief (Silverman, Pina, & Viswesvaran, 2008). Such heterogeneity in treatment response underscores the reality that CBT protocols work for many, but not all, children. Moreover, little data have emerged on the clinical characteristics of youth who are most likely to respond to various treatment formats. Identifying treatment moderators that clarify which patients are most likely to benefit from a particular treatment, such as intensive formats, is critical for informing patient-centered care (e.g., Comer & Kendall, 2013; Kazdin, 2002; Kendall & Comer, 2010).
The degree to which adolescents fear and avoid anxiety-provoking situations and stimuli are central aspects of PDA phenomenology. Gold-standard assessment measures of PDA symptoms and severity in youth (e.g. Silverman & Albano, 1997) emphasize a thorough evaluation of the extent of a child’s fear and avoidance to inform PDA diagnostic impressions and decisions about clinical severity. Moreover, in the evidence-based treatment of PDA, fear and avoidance are central treatment targets for both adults (Barlow & Craske, 2000; Craske & Barlow, 2006) and children (Pincus, Ehrenreich, Mattis, & Barlow, 2008), and are addressed through the development of a fear and avoidance hierarchy that subsequently provides a roadmap for exposures across treatment. Given the centrality of fear and avoidance in the identification and treatment of youth with PDA, it is possible that heterogeneity across children’s baseline levels of fear and avoidance are meaningfully linked to heterogeneity in treatment response. Thus, identifying whether baseline levels of fear and avoidance moderate treatment response can help clarify which youth may benefit most from intensive PCT-A.
The present study examines the moderating roles of baseline fear and avoidance on treatment response among adolescents receiving intensive PCT-A in the context of an RCT. We hypothesized that the extent of adolescents’ baseline fear and avoidance would each moderate the effect of treatment on panic severity. Given that referrals to intensive programs often follow initial treatment failures (e.g., Storch et al., 2007), and given that concentrated exposure opportunities afforded by an intensive format may be particularly effective for severe cases, we specifically hypothesized that intensive PCT-A would have a significantly greater effect on youth with higher levels of baseline fear and avoidance than on youth with more moderate levels of baseline fear and avoidance.
Method
Participants
Participating youth were enrolled in an RCT investigating the feasibility and efficacy of intensive 8-day cognitive behavioral treatment for PDA. Main outcomes for the trial are reported elsewhere (Pincus et al., 2015). Treatment was conducted at a university-based anxiety specialty clinic. Adolescents with PDA were randomly assigned to immediate intensive PCT-A or a waitlist. Exclusion criteria for the trial were: (a) schizophrenia, pervasive developmental disorder, organic brain syndrome, mental retardation, or current suicidal ideation; (b) unavailability of a caregiver to bring the adolescent to treatment; (c) refusal to accept random assignment; and (d) refusal to accept medication stabilization requirements to remain on steady doses of current medications for the duration of the study. Finally, as all procedures were delivered in English, only English-speaking participants were enrolled.
Participants in the present study were 54 adolescents between the ages of 11 and 17 (M = 15.29, SD = 1.68) with a principal diagnosis of PDA. Participant diagnostic profiles were generated following semi-structured interviews conducted with children and parents. The majority of eligible participants received a diagnosis of panic disorder with agoraphobia (N = 53); one participant was assigned a diagnosis of panic disorder without agoraphobia. Eight participants had co-principal diagnoses, including specific phobia of vomiting (N = 5), social anxiety disorder (N = 2), and major depressive disorder (N =1). Participants were predominantly Caucasian/Non-Hispanic (86.8%), and 61% were female. Annual family income for participants ranged from $25,000 to $500,000, with a mean annual income of $105,000. Nearly half of participants (46%) reported taking psychotropic medications at baseline. Reported medications included antidepressants (N =11, 20.3%), antianxiety medications (N = 3, 5.5%), or multiple medications (N = 11, 20.3%).
A total of 103 adolescents were assessed in an initial phone screen. Forty-three participants were excluded because they did not meet diagnostic criteria for primary diagnosis of PDA. Three withdrew following the baseline evaluation due to unwillingness to participate in the study. (For a full CONSORT diagram detailing the flow of study participants, the interested reader is directed to Pincus et al., 2015).
Measures
Child diagnoses
The Anxiety Disorders Interview Schedule for Diagnostic and Statistical Manual of Mental Disorders IV: Child and Parent Versions (ADIS-C/P; Silverman & Albano, 1997) was administered to inform clinician-generated diagnoses. The ADIS-C/P is a semi-structured diagnostic interview that assesses DSM-IV mood, anxiety, and disruptive behavior disorders. The ADIS-C/P is the most widely used diagnostic interview in clinical research with child anxiety populations, boasting strong reliability, validity, and sensitivity to change (Grills & Ollendick, 2003; Silverman & Ollendick, 2005; Silverman, Saavedra, & Pina, 2001; Wood, Piacentini, Berman, McCracken, & Barrios, 2002). Diagnosticians at the treatment site of the present study demonstrated good interrater agreement on primary diagnoses ( = .87), and 15% of study assessments were rated by two evaluators to ensure reliability.
Fear and avoidance
The child version of ADIS-C/P was used to collect baseline data on the extent of adolescents’ fear and avoidance related to their PDA. Specifically, the Panic Disorder module of the ADIS-C includes a Fear Checklist and an Avoidance Checklist. Both checklists present situations commonly feared and/or avoided by youth with PDA, including classrooms, public transportation, elevators, etc., (total number of situations assessed = 20). When completing this checklist, the clinician inquires about whether the adolescent fears and/or avoids each of these situations due to panic. For endorsed items, adolescents rate the degree to which they fear and/or avoid that situation on a scale from 0–8, where 0 indicates no fear/avoidance, 4 indicates some fear/avoidance, and 8 signifies the greatest extent of fear/avoidance. As per ADIS-C/P administration guidelines, fear and avoidance ratings greater than or equal to 4 are considered clinically elevated. For the Fear and Avoidance Checklists, respectively, the number of all feared and avoided situations with a rating of 4 or above was summed to generate a baseline Total Number of Feared Situations and a baseline Total Number of Avoided Situations.
Panic severity
The Panic Disorder Severity Scale for Children (PDSS-C; Elkins, Pincus & Comer, 2014) is a 7-item self-report measure assessing the frequency and severity of PDA symptoms. The PDSS-C utilizes a 5-point scale (0 to 4) to assess each item, and responses to all items are summed to yield a total score ranging from 0 to 28 representing overall PDA severity. The PDSS-C demonstrates strong reliability and validity, as well as sensitivity to treatment-related change (Elkins et al., 2014).
Procedures
Potential participants and their parents completed an initial phone screen. Eligible participants completed assessments at baseline and 6-week post-waitlist/post-treatment administered by independent evaluators (IEs) who were blind to participants’ study condition. IEs and study therapists were doctoral candidates and postdoctoral fellows in clinical psychology specializing in pediatric anxiety disorders. All IEs met internal certification and reliability procedures, developed in collaboration with one of the ADIS-C/P authors. IE assessments included the administration of the ADIS-C/P, including the Fear and Avoidance Checklists from the ADIS-C panic disorder module, and the PDSS-C self-report form. Demographic information was obtained from parent report.
Eligible participants were randomly assigned to receive either immediate intensive CBT with heavy parent involvement (N = 19), immediate intensive CBT with minimal parent involvement (N = 18), or a 6-week waitlist (N = 17). Prior work (Pincus et al., 2015) found that the two active treatment conditions showed equivalent outcomes. Accordingly, data from these conditions were collapsed into a single intensive CBT condition (CBT; N = 37) compared to a 6-week waitlist condition (WL; N = 17).
Participants in the CBT condition received an intensive format of the manual-based PCT-A protocol, Mastery of your Anxiety and Panic for Adolescents: Riding the Wave (Pincus et al., 2008) adapted for delivery over eight consecutive days (Angelosante et al., 2009). As with standard weekly individual CBT for panic disorder, intensive treatment for adolescent PDA focused on targeting the cognitive distortions and associated behavioral avoidance related to each adolescent’s symptoms, and incorporated well-established cognitive-behavioral treatment elements, such as psychoeducation, cognitive restructuring, interoceptive and in vivo exposures. Several steps were taken to individualize the treatment within fidelity to the treatment protocol to optimally address each adolescent’s unique PDA presentation using a cognitive-behavioral approach. Specifically, therapists elicited information from each adolescent regarding the frequency, duration, and intensity of their panic symptoms; therapists and adolescents collaboratively created an individualized fear and avoidance hierarchy, which provided a guiding outline for later exposures; treatment addressed the cognitive distortions about panic particular to the adolescent; and in vivo exposures were tailored to address feared and avoided situations specific to each adolescent.
The first two days of treatment were devoted to rapport building, psychoeducation, developing an individualized fear and avoidance hierarchy, and cognitive restructuring. The third day was dedicated to practicing interoceptive exposures, and the fourth and fifth days were full-day sessions (6 to 8 hours) to allow for repeated therapist-assisted in vivo exposures, often conducted outside of the clinic to generalize treatment gains to “real life” settings. The adolescent and his or her family completed additional independent exposures over the weekend, and the final day in the clinic was devoted to review, relapse prevention, and planning for continued practice at home. Treatment included weekly 30-minute telephone check-ins for 1-month following the eighth day of treatment. These four phone calls provided a forum for therapists and youth to collaboratively plan additional home-based exposure practices, troubleshoot problems as they arose, and facilitated the gradual transfer of responsibility for treatment to the adolescent; thus, post-treatment assessments for the CBT group occurred six weeks following the initial assessment. WL participants did not receive treatment, and were also assessed six weeks following their initial assessment.
Analytic strategy
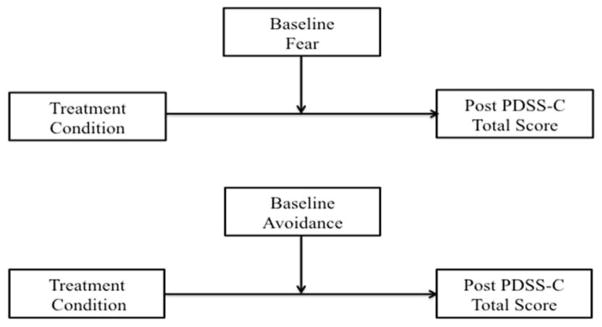
Hierarchical multiple regression analyses examined the relative contributions of treatment condition, number of baseline feared or avoided situations, and their interactions in the prediction of post-treatment PDA severity. Given that all data were normally distributed and assumptions of normality were not violated, generalized linear models were not appropriate for the present analyses. Two parallel analyses (one for baseline fear and one for baseline avoidance) were run in line with data analytic conventions for evaluating moderators (Baron & Kenny, 1986). Treatment condition (CBT vs. WL) was identified as the independent variable. As in previous analyses (Gallo, Cooper-Vince, Hardway, Pincus, & Comer, 2014), the dependent variable was PDSS-C Total Score at 6-week post-treatment/post-waitlist. Two proposed moderators were hypothesized: 1) number of Feared situations at baseline, and 2) number of Avoided situations at baseline (see Figure 1). For each model, treatment condition was entered into step 1 as a predictor of 6-week PDSS-C scores. The proposed moderator was then added as a centered predictor in step 2, and the product term of treatment condition × the proposed moderator (the interaction term) was added as a centered predictor into step 3. Significance of the interaction term in step 3, after accounting for main effects in steps 1 and 2, is interpreted as evidence of significance moderation (Comer & Kendall, 2013). Evidence of significant moderation was followed-up with post-hoc analyses comparing simple slopes at different levels of fear and avoidance to clarify the direction of each moderation effect. Specifically, simple slopes were computed for youth showing >1 SD and <1 SD beyond the mean number of feared situations in the sample (i.e., high and moderate fear subgroups, respectively) and for youth showing >1 SD and <1 SD beyond the mean number of avoided situations in the sample (i.e., high and moderate avoidance subgroups, respectively). Youth in the present sample showing <1 SD below the sample means were characterized as "moderate" rather than "low" given that all youth in the study presented with clinical levels of fear and avoidance.
Figure 1.
Model of proposed moderators of panic disorder severity
Results
Means and standard deviations across study variables are presented in Table 1. At baseline, no demographic or clinical group differences were noted between CBT and WL youth: age (t[52] = −1.62, p = 0.11), gender (χ2[1] = 0.14, p = 0.71), medication status (χ2 [1] = 0.01, p = 0.94), baseline PDSS-C Total scores, (t[48] = .67, p = .51), baseline numbers of feared situations (t[52] = .71, p = 0.48 ), and baseline number of avoided situations (t[52] = .45, p = 0.66). Across the full sample, baseline fear and avoidance both showed small, negative associations with post-treatment panic severity (r = −.17, p = .32, and r = −.13, p = .44, respectively). Among youth receiving CBT, baseline fear and avoidance both showed small, positive associations with post-treatment panic severity (r = .25, p = .23, and r = .32, p = .13, respectively).
Table 1.
Baseline characteristics of participants, by condition (N =54)
| Total Sample | CBT Youth (N = 37) | WL Youth (N = 17) | Significance test | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | % | N | % | N | % | ||
|
| |||||||
| Female | 33 | 61.1 | 22 | 59.5 | 11 | 64.7 | χ2 (1) = .14, p = .71 |
| Taking psychotropic medication | 25 | 46.3 | 17 | 45.9 | 8 | 47.1 | χ2 (1) = .01, p = .94 |
| M | SD | M | SD | M | SD | Significance test | |
|
|
|||||||
| Age, years | 15.29 | 1.7 | 15.04 | 1.8 | 15.82 | 1.3 | t(52) = −1.62, p = .11 |
| Baseline # feared situations | 6.42 | 4.2 | 6.70 | 4.2 | 5.82 | 4.5 | t(52) = .71, p = .48 |
| Baseline # avoided situations | 5.46 | 3.8 | 5.62 | 3.6 | 5.12 | 4.2 | t(52) = .45, p = .66 |
| Baseline PDSS-C Total | 13.46 | 5.25 | 13.82 | 5.5 | 12.77 | 4.8 | t(48) = .67, p = .51 |
Note: CBT = Youth assigned to intensive cognitive-behavioral therapy; WL = Youth assigned to waitlist control; PDSS-C = Panic Disorder Severity Scale for Children
Moderating effect of baseline fear on treatment outcome
Table 2 presents the results of the hierarchical multiple regression analysis evaluating the relative contributions of treatment condition, number of feared situations at baseline, and their interaction in the prediction of treatment outcome, as measured by the PDSS-C Total score at post-treatment/post-waitlist. In the prediction of treatment outcome, the main effect of treatment condition provided a significant contribution to the model, F(1, 37) = 11.48, p < .01, indicating significantly greater reductions in panic severity at six weeks among youth treated with intensive CBT than among youth in the WL group. Adding the main effect of baseline fear as a predictor did not improve the predictive utility of the model, Fchange(1, 36) = .09, p = .77. However, after accounting for main effects, the interaction of Treatment Condition × Fear added a significant contribution to the prediction of six week panic symptoms, Fchange(1, 35) = 4.61, p = .04, indicating that the extent of baseline fear moderates the effect of intensive CBT on panic severity.
Table 2.
Hierarchical regression examining moderating role of baseline feared situations in predicting treatment response (N = 54)
| Variable Entered | B | SE(B) | β | t |
|---|---|---|---|---|
| Step 1. | ||||
| Treatment condition (CBT vs. WL) | 6.62 | 1.95 | .49 | 3.39** |
| Step 2. | ||||
| Treatment Condition | 6.47 | 2.05 | .48 | 3.16** |
| Baseline Fear | −.07 | .23 | −.05 | −.30 |
| Step 3. | ||||
| Treatment Condition | 5.91 | 1.97 | .44 | 3.01** |
| Baseline Fear | 1.27 | .66 | .83 | 1.92 |
| Treatment Condition × Baseline Fear | −.97 | .45 | −.94 | −2.15* |
Note:
p < .05,
p < .01
To probe the direction of this moderation effect, post-hoc analyses compared simple slopes among high (n = 11) and moderate (n = 10) fear youth – defined as those with fear scores one standard deviation above and below the sample mean, respectively. The effect of treatment condition on 6-week PDSS-C scores was significant among moderate fear youth (B = 20, SE = 4.12, β = .93, p < .01), whereas there was no condition effect on 6-week PDSS-C scores among high fear youth (B = 2.20, SE = 4.63, β = .19, p = .65).
Moderating effect of baseline avoidance on treatment outcome
Hierarchical regression procedures examined the moderating effect of baseline avoidance on treatment outcome (see Table 3). As with baseline fear analyses, results indicated a main effect of Treatment Condition in step 1, F(1, 37) = 11.48, p < .01. Adding the main effect of baseline avoidance as a predictor in step 2 did not add a significant contribution to the prediction of 6-week panic severity, Fchange(1, 36) = .07, p = .79. However, after accounting for main effects, the interaction of Treatment Condition × Avoidance significantly contributed to the prediction of post-treatment panic symptoms, Fchange(1, 36) = 5.51, p = .03, indicating that the extent of baseline avoidance also moderates the effect of intensive CBT on panic severity.
Table 3.
Hierarchical regression examining moderating role of baseline avoided situations in predicting treatment response (N = 54)
| Variable Entered | B | SE(B) | β | t |
|---|---|---|---|---|
| Step 1. | ||||
| Treatment condition (CBT vs. WL) | 6.62 | 1.95 | .49 | 3.39** |
| Step 2. | ||||
| Treatment Condition | 6.52 | 2.01 | .48 | 3.24** |
| Baseline Avoidance | −.07 | .26 | −.04 | −.26 |
| Step 3. | ||||
| Treatment Condition | 6.41 | 2.00 | .47 | 3.38** |
| Baseline Avoidance | 1.59 | .75 | .92 | 2.13* |
| Treatment Condition × Baseline Avoidance | −1.14 | .49 | −1.01 | −2.35* |
Note:
p < .05,
p < .01
Post-hoc analyses compared simple slopes among high (n = 9) and moderate (n = 10) avoidance youth – defined as those with avoidance scores one standard deviation above and below the sample mean, respectively). Similar to the baseline fear analyses, the effect of treatment condition on 6-week PDSS-C scores was significant among moderate avoidance youth, (B = 17.53, SE = 4.69, β = .86, p = .01), whereas there was no condition effect on 6-week PDSS-C scores among high avoidance youth (B = 1.75, SE = 5.12, β = .15, p = .75).
Discussion
Intensive treatment formats may play a crucial role in the expansion of evidence-based treatment options for anxiety-disordered youth (Ollendick, 2014). Data on intensive treatment formats for adolescent PDA have been encouraging (Chase et al., 2012; Gallo et al., 2013; Pincus et al. 2015), but despite the great value of identifying treatment moderators for informing patient-centered care (see Comer & Kendall, 2013; Kazdin, 2002), research has yet to evaluate which adolescents are most likely to benefit from this promising treatment format.
The present findings offer the first data-based portrait of presenting clinical characteristics in the context of response to intensive treatment for adolescent PDA. Within the present RCT, the main effect of intensive treatment on post-treatment panic symptoms was not uniform across participants. Indeed, treatment effects were moderated by the extent of baseline fear and avoidance, with treatment effects stronger among adolescents with more moderate, relative to higher, levels of fear and avoidance. These results suggest that data on baseline fear and avoidance can provide compelling prognostic information regarding the conditions under which intensive treatment for adolescent PDA is most effective.
Although significant moderators of treatment response were identified, contrary to hypotheses, more moderate levels of baseline fear and avoidance predicted more favorable outcome. All participating youth presented with elevated symptoms, but the present findings suggest that intensive treatment may be best suited for youth with more moderate, relative to severe, fear and avoidance patterns. Although intensive treatments are often recommended for more severe patients who have not responded to standard weekly treatment (e.g. Storch et al., 2007), the present data suggest that in the case of adolescent PDA, prescribing intensive treatments for severe cases may be somewhat misguided. It may be that for adolescents with relatively high fear and avoidance, asking them to confront their symptoms in the condensed span of eight days may be less productive than weekly treatment formats or medication management. In contrast, the present findings suggest that adolescents with moderate degrees of fear and avoidance benefit most from intensive treatment. Given the role of intensive approaches to help overcomes barriers in the availability of expert care (see Comer & Barlow, 2014), it is encouraging that the more moderate cases, which constitute the majority of the adolescent PDA population, appear to be well served by intensive treatment alternatives to traditional weekly treatment formats.
The present analysis has several limitations. First, the study was conducted at an urban university-based outpatient clinic specializing in the treatment of anxiety disorders. As a result, although participants traveled from across the country, findings may not be fully representative of youth with PDA. Similarly, the sample was English-speaking, predominantly Caucasian, and of relatively high economic means. Given these limitations, future work is needed to examine cultural and socioeconomic variations in the extent to which fear and avoidance moderates treatment outcome. Second, many participants were concurrently taking psychotropic medications, which could have impacted symptom presentations and treatment response. However, as adolescents with PDA are five times more likely to be treated with antidepressants than adolescents without PDA, and are also more likely to be taking anxiolytic, mood stabilizing, or stimulant medications (Olfson, He, & Merikangas, 2012), restricting the trial to medication-naïve youth would have considerably limited the generalizability of findings. Third, although significant results were identified, the results of the present study may have been influenced by the sample size, and it is possible that a larger sample size may have yielded different results. Future work would do well to recruit larger sample sizes to increase the power to detect clinically significant moderators of treatment outcome for youth receiving intensive CBT for PDA. Fourth, although fear and avoidance are conceptualized throughout the literature as related but distinct predictors of PDA presentation, it is possible that fear and avoidance as presently measured did not assess distinct symptom dimensions in the present study.
As the present trial utilized a waitlist control rather than an active treatment comparison, the extent to which baseline fear and avoidance specifically moderate intensive treatment formats, as opposed to all active treatments, remains unclear. Future controlled evaluations are needed in which youth are either (a) randomly assigned to intensive or weekly formats, or (b) randomly assigned to varying sequences of intensive and weekly formats (Barlow & Comer, 2013). Finally, although we examined baseline fear and avoidance, there are a number of features of PDA that could be considered when identifying diagnostic severity (e.g., intensity of physiological panic symptoms, reliance on safety behaviors). Future work may do well to consider other features of PDA that may additionally inform the identification of sub-populations of PDA youth who would benefit from intensive treatment.
Despite the development of well-tolerated, evidence-based treatments for children’s mental health problems, serious gaps persist between treatment available in experimental settings and services broadly available in the community (Sandler et al., 2005). The present findings add to a growing body of literature suggesting that intensive treatment options at expert care facilities may be an important alternative to standard weekly care—particularly for youth presenting with more moderate severity—when local professional expertise is lacking (Comer & Barlow, 2014). Given the promising role that intensive treatment formats may play in the expansion of evidence-based care for youth, continued empirical efforts are needed to identify the benefits of intensive treatment options and to clarify for whom such formats are most effective.
Key Practitioner Message.
Intensive cognitive behavioral therapy (CBT) has shown considerable efficacy in the treatment of adolescent panic disorder (PDA). However, it is important to clarify which patients are most likely to benefit from this approach.
Considering the degree to which adolescents fear and avoid common situations and settings at baseline may inform whether a given adolescent will benefit from intensive treatment for PDA.
Results indicate that adolescents with more moderate fear and avoidance at baseline may benefit most from intensive CBT.
The present findings add to the literature suggesting that intensive treatment may be an important alternative to standard weekly care for many affected youth, particularly those presenting with more moderate severity.
Acknowledgments
Funding for this work was provided by the National Institute of Mental Health (R01 MH068277; K23 MH090247). The authors wish to thank all families who participated in this study. All authors take full responsibility for the accuracy of the data and the integrity of the data analysis.
Footnotes
The authors declare they have no competing or potential conflicts of interest to report.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Angelosante AG, Pincus DB, Whitton SW, Cheron D, Pian J. Implementation of an intensive treatment protocol for adolescents with panic disorder and agoraphobia. Cognitive and Behavioral Practice. 2009;16(3):345–358. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York, NY: Guilford Press; 2002. [Google Scholar]
- Barlow DH, Comer JS. What are the optimal treatment courses for geriatric psychiatry, and how do we find out? American Journal of Psychiatry. 2013;170(7):707–711. doi: 10.1176/appi.ajp.2013.13040513. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Craske MG. Mastery of your Anxiety and Panic. Boulder, CO: Graywind; 2000. [Google Scholar]
- Barlow DH, Craske MG, Cerny JA, Klosko JS. Behavioral treatment of panic disorder. Behavior Therapy. 1989;20(2):261–282. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitran S, Morissette SB, Spiegel DA, Barlow DH. A pilot study of sensation-focused intensive treatment for panic disorder with moderate to severe agoraphobia: Preliminary outcome and benchmarking data. Behavior Modification. 2008;32(2):196–214. doi: 10.1177/0145445507309019. [DOI] [PubMed] [Google Scholar]
- Chase RM, Whitton SW, Pincus DB. Treatment of adolescent panic disorder: A nonrandomized comparison of intensive versus weekly CBT. Child and Family Behavior Therapy. 2012;34(4):305–323. [Google Scholar]
- Comer JS, Barlow DH. The occasional case against broad dissemination and implementation: Retaining a role for specialty care in the delivery of psychological treatments. American Psychologist. 2014;69(1):1–18. doi: 10.1037/a0033582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Blanco C, Hasin DS, Liu S, Grant BF, Turner J, Olfson M. Health-related quality of life across the anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2011;72(1):43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Kendall PC. Methodology, design, and evaluation in psychotherapy research. In: Lambert MJ, editor. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change. 6. Hoboken, NJ: Wiley; 2013. [Google Scholar]
- Craske MG, Barlow DH. Mastery of your anxiety and panic: Therapist Guide. 4. New York, NY: Oxford University Press; 2006. [Google Scholar]
- Diler RS, Birmaher B, Brent DA, Axelson DA, Firinciogullari S, Chiapetta L, Bridge J. Phenomenology of panic disorder in youth. Depression and Anxiety. 2004;20(1):39–43. doi: 10.1002/da.20018. [DOI] [PubMed] [Google Scholar]
- Ehrenreich JT, Santucci LC. Special series: Intensive cognitive-behavioral treatments for child and adolescent anxiety disorders. Cognitive and Behavioral Practice. 2009;16:290–293. doi: 10.1016/j.cbpra.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins RM, Comer JS, Pincus DP. A psychometric evaluation of the Panic Disorder Severity Scale for Children and Adolescents (PDSS-C) Psychological Assessment. 2014;26(2):609–618. doi: 10.1037/a0035283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo KP, Chan PT, Buzzella BA, Whitton SW, Pincus DB. The impact of an 8-day intensive treatment for adolescent panic disorder and agoraphobia on comorbid diagnoses. Behavior Therapy. 2012;43(1):153–159. doi: 10.1016/j.beth.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo KP, Cooper-Vince CE, Hardway C, Pincus DB, Comer JS. Trajectories of change across outcomes in intensive treatment for adolescent panic disorder and agoraphobia. Journal of Clinical Child and Adolescent Psychology. 2014;43:742–750. doi: 10.1080/15374416.2013.794701. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Goldstein RB, Smith S, Huang B, Saha TD. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67(3):363–374. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- Grills AE, Ollendick TH. Multiple informant agreement and the anxiety disorders interview schedule for parents and children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(1):30–40. doi: 10.1097/00004583-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Hoffman EC, Mattis SG. A developmental adaptation of panic control treatment for panic disorder in adolescence. Cognitive and Behavioral Practice. 2000;7(3):253–261. [Google Scholar]
- Kazdin A. The state of child and adolescent psychology research. Child and Adolescent Mental Health. 2002;7(2):53–59. doi: 10.1111/1475-3588.00011. [DOI] [PubMed] [Google Scholar]
- Kearney CA, Albano AM, Eisen AR, Allan WD, Barlow DH. The phenomenology of panic disorder in youngsters: An empirical study of a clinical sample. Journal of Anxiety Disorders. 1997;11(1):49–62. doi: 10.1016/s0887-6185(96)00034-5. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Comer JS. Research methods in clinical psychology. In: Barlow DH, editor. The Oxford Handbook of Clinical Psychology. NY: Oxford University Press; 2010. [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Merikangas KR. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012;69(4):372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King NJ, Bernstein GA. School refusal in children and adolescents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(2):197–205. doi: 10.1097/00004583-200102000-00014. [DOI] [PubMed] [Google Scholar]
- Masi G, Favilla L, Mucci M, Millepiedi S. Panic disorder in clinically referred children and adolescents. Child Psychiatry and Human Development. 2000;31(2):139–151. doi: 10.1023/a:1001948610318. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Ames M, Cui L, Stang PE, Ustun T, Von Korff M, Kessler RC. The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Archives of General Psychiatry. 2007;64(10):1180–1188. doi: 10.1001/archpsyc.64.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH. Brief, high intensity interventions with children and adolescents with anxiety disorders: Introductory comments. Psychopathology Review. 2014;1:169–174. [Google Scholar]
- Olfson M, He J-P, Merikangas KR. Psychotropic medication treatment of adolescents: Results from the National Comorbidity Survey–Adolescent Supplement. Journal of The American Academy Of Child & Adolescent Psychiatry. 2013;52(4):378–388. doi: 10.1016/j.jaac.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus DB, Ehrenreich JT, Mattis SG, Barlow DH. Mastery of anxiety and panic for adolescents: Riding the wave, therapist guide. New York, NY: Oxford University Press; 2008. [Google Scholar]
- Pincus DB, May JE, Whitton SW, Mattis SG, Barlow DH. Cognitive-behavioral treatment of panic disorder in adolescence. Journal of Clinical Child and Adolescent Psychology. 2010;39(5):638–649. doi: 10.1080/15374416.2010.501288. [DOI] [PubMed] [Google Scholar]
- Pincus DB, Whitton SW, Gallo KP, Weiner CL, Chow C, Hardway C, Barlow D. Intensive treatment of adolescent panic disorder: Results of a randomized controlled trial with short-term maintenance. 2015 Manuscript in preparation. [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55(1):56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Sandler I, Ostrom A, Bitner MJ, Ayers TS, Wolchik S, Daniels DS. Developing effective prevention services for the real world: A prevention service development model. American Journal of Community Psychology. 2005;35:127–142. doi: 10.1007/s10464-005-3389-z. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and parent versions. San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-Retest Reliability of Anxiety Symptoms and Diagnoses With the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Storch EA, Bagner DM, Geffken GR, Adkins JW, Murphy TK, Goodman WK. Sequential cognitive-behavioral therapy for children with obsessive-compulsive disorder with inadequate medication response: A case series of five patients. Depression and Anxiety. 2007;24(6):375–381. doi: 10.1002/da.20260. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman R, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of Clinical Child And Adolescent Psychology. 2002;31(3):335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]