Abstract
Although some studies have shown negative associations between birth weight and risk of depression, others have not. Studies also differ in their age- and gender-specificity of reported associations. We report a study of 5830 women aged 20-34 years from the general population in Southampton UK that found no relationship between birth weight and current depressive symptoms or past treatment for depression. Prevalence ratios for current symptoms and for past treatment, in relation to reported or recorded birth weights were all remarkably close to 1.0, with narrow 95 percent confidence intervals. For example, the prevalence ratio from the fully adjusted model for current depressive symptoms in relation to a standard deviation increase in reported birth weight was 1.01 (95 percent confidence interval: 0.98, 1.05). Generally, the associations reported elsewhere are not strong. We found a weak inverse association in exploratory analyses of duration of gestation at birth in relation to depressive symptoms, but this requires replication. As birth weight and duration of gestation are relatively poor markers of fetal development, other markers of fetal and early development should be explored. However, our data do not support a major developmental contribution to the etiology of depression in women.
Keywords: Birth weight, depression, depressive symptoms, gestational age, women
Data on the relationship between birth weight and depressive symptoms are inconsistent. Recently Alati et al (1) reported a study of adults aged 21 years and found a negative association in women but not in men and the interaction with sex was strongly significant. Gale and Martyn (2) reported similarly discordant findings between the sexes at age 26 years, with a stronger negative association with birth weight in women than in men. In contrast, Thompson et al (3) in a study of older adults aged 68 years found a negative association in men but not women. Neither of these two studies reported a formal test of the interaction with sex. In a study of over 10,000 men followed prospectively, no association between birth weight and admission to psychiatric ward for depression was found (4). Mixed findings have been reported elsewhere but without information on sex differences; a study in twins aged 8-17 years reported a small association (5), and borderline significant associations were found in adults aged around 50 years old (6). Other studies have reported negative associations between birth weight and more general psychological symptoms (7) or mood disorder (8), and between infant growth and suicide (9). In all but three of these studies (3, 4, 9) the birth weights were adjusted for gestational age, but none of them reported on the relationship between depressive symptoms and length of gestation. Recently, however, an association between depressive symptoms and duration of gestation, but not birth weight, has been reported in a Finnish cohort (10).
Consistent evidence of a relationship between birth weight and depression has not been found, nor whether there are differences between the sexes. Rates of depression differ between men and women and so the etiology may also differ between the two genders. As the highest rates of depression are seen in women of child bearing years (11) we examined the associations of birth weight and gestation at birth with past treatment for depression and current depressive symptoms in young women in the peak child-bearing years of 20-34 years in Southampton, UK.
MATERIALS AND METHODS
The Southampton Women’s Survey (SWS) was established in 1998 to study young women in Southampton of child-bearing age and follow them through their subsequent pregnancy. We aimed to assess the influence of maternal factors operating before and during pregnancy on the subsequent growth and development of the offspring. Between 1998 and 2002 all general practitioners in Southampton were asked to help recruit their female patients aged 20–34 years. Full details of the Survey have been described elsewhere (12). The recruited women were representative of the population of Southampton, which is similar to that of England and Wales except that ethnic minority groups are under-represented; approximately 94 percent of women in the study are white (12).
The information collected at baseline included socio-demographic factors and the women’s own birth weights. Where women were uncertain of their birth weight they were asked to contact their parents for the information. They were also asked if they were born early, late or at term, and, if not at term, how many days early or late. From this, an estimate of gestational age at birth was derived. In addition to reported birth weight, birth weights and gestational ages recorded at the time of the birth were obtained from local hospital obstetric records for all those women who had been born in Southampton.
From March 2000, all SWS women were asked at initial interview to complete the 12-item version of the general health questionnaire (GHQ-12) to assess current depressive symptoms (13). The women were also asked whether they had ever received treatment for depression, anxiety, or other mental health problem in the past. For each of the GHQ-12 questions, there are four options in response. The two items indicating a lower likelihood of depressive symptoms were scored as 0 and the other two as 1 (0-0-1-1 scoring method). The scores were summed across the 12 questions and women with a score of 3 or more were categorized as being potentially depressed at baseline.
The study received approval from the Southampton and South West Hampshire Local Research Ethics Committee.
Statistical analysis
We derived standard deviation (SD) scores for birth weight as our main independent risk variable and assessed the relationship between birth weight and (a) whether the woman reported ever having received treatment for depression and (b) whether she was classified as suffering from depressive symptoms or not according to the GHQ-12. Poisson regression with robust variance (14) was used to estimate prevalence ratios and 95 percent confidence intervals (CIs) for our measures of depressive symptoms in relation to the factors of interest. An analysis using categories of birth weight was also conducted to assess whether there was any evidence for a threshold effect.
Adjustment for gestational age at birth was conducted in two ways. Firstly, we derived birth weight SD scores using the British 1990 growth reference data (15) and, secondly, using polynomial regression.
Other factors known to influence depression or that might confound the relationship with birth weight were assessed in adjusted models. The factors considered were age, education, social class, perceived financial strain, and low income as defined by whether the woman was on social security benefits or not.
All analyses were repeated for those women for whom birth weight as recorded at birth were available from the hospital records. Exploratory analyses were undertaken relating our measures of depressive symptoms to reported and recorded gestation at birth.
RESULTS
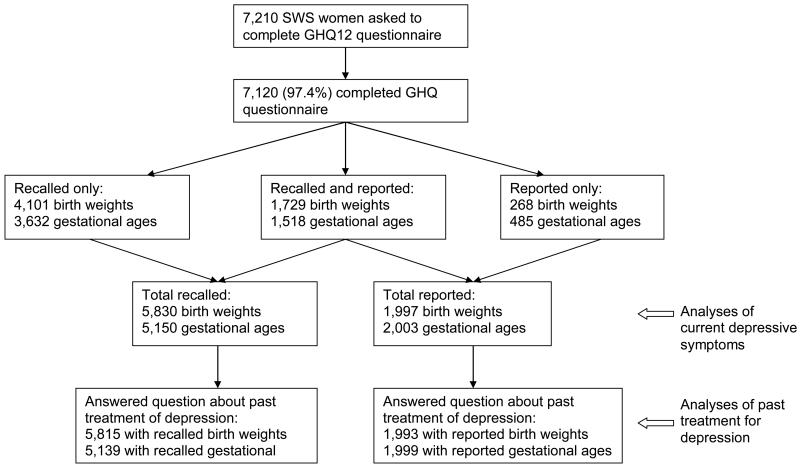
Some 75 percent of those who were contacted about participation in the SWS were interviewed. From March 2nd 2000, 7210 women participated in the SWS and of these 7020 (97.4 percent) completed a GHQ12 questionnaire. Figure 1 gives details of numbers of women with recalled and reported birth weight and gestational ages and the numbers who reported on whether they had received past treatment for depression.
Figure 1.
Flow chart explaining numbers of participants in each stage of the study of depressive symptoms among women in the Southampton Women’s Survey interviewed between March 2000 and November 2002.
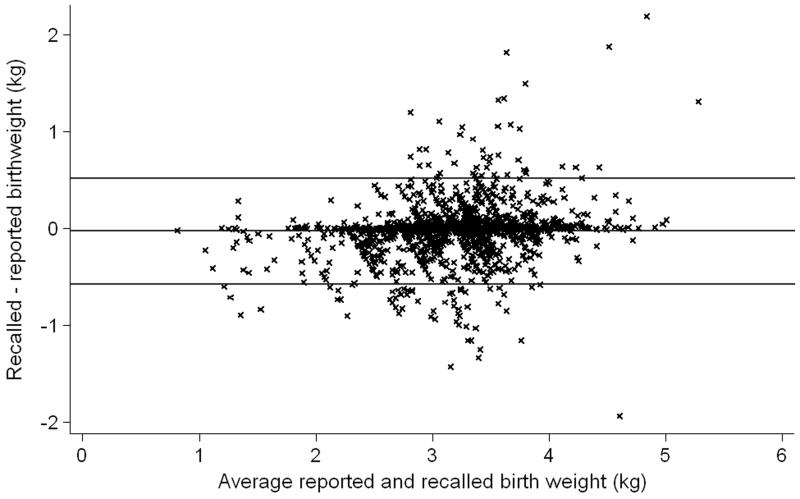
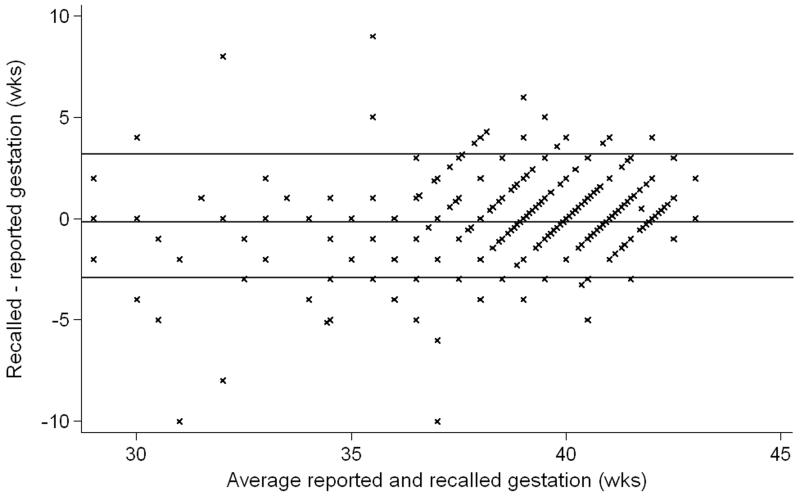
The mean recalled birth weight was identical to the mean reported birth weight at 3.2kg. The proportions of low birth weights (<2.5kg) were 10.1% for the recalled values and 7.3% for those that were reported. Among the 1729 women with both reported and recorded birth weights, Spearman’s rank correlation coefficient for the two assessments was 0.87, and for gestational ages among the 1518 women with reported and recorded assessments the correlation coefficient was 0.62. Bland Altman plots of the relationships between reported and recorded values are given in Figures 2 and 3 and both indicate reasonable agreement.
Figure 2.
Bland-Altman plot to show agreement between reported and recorded birth weights in 1729 participants in the Southampton Women’s Survey interviewed between March 2000 and November 2002.
Figure 3.
Bland-Altman plot to show agreement between reported and recorded lengths of gestation in 1518 participants in the Southampton Women’s Survey interviewed between March 2000 and November 2002.
No relationship was found between birth weight and depressive symptoms. Table 1 presents the prevalence rates and prevalence ratios for current depressive symptoms and past treatment for depression in relation to birth weight SD scores. Adjustment for gestational age and potential confounding variables made minimal difference to the findings, indicating that they were not exerting a confounding effect on the birth weight and depressive symptoms association. Only the analyses using gestational age adjusted against the 1990 British growth standard are presented in Table 1 but the alternative form of adjustment for gestational age gave rise to very similar findings. Using categories of birth weight led to similar conclusions with no evidence of any threshold effect below a particular weight.
TABLE 1. Prevalence rates and prevalence ratios for depressive symptoms in relation to birth weight in the Southampton Women’s Survey.
| Measure of depressive symptoms | Reported or recorded birth weight | Number in analysis | Number depressed (prevalence %) | Prevalence ratio* (95%CI) [unadjusted] | Prevalence ratio* (95%CI) [adjusted for gestational age]† | Prevalence ratio* (95%CI) [fully adjusted]‡ |
|---|---|---|---|---|---|---|
| Ever treated for depression | Reported | 5815 | 1910 (33%) | 0.97 (0.94,1.01) | 1.00 (0.97,1.03) | 1.01 (0.98,1.04) |
| Recorded | 1993 | 668 (34%) | 0.96 (0.91,1.02) | 1.03 (0.97,1.09) | 1.02 (0.96,1.08) | |
| Current depressive symptoms (GHQ-12 assessment) | Reported | 5830 | 1866 (32%) | 0.99 (0.95,1.03) | 1.01 (0.98,1.04) | 1.01 (0.98,1.05) |
| Recorded | 1997 | 631 (32%) | 0.97 (0.91,1.04) | 1.01 (0.95,1.08) | 1.00 (0.94,1.07) |
The prevalence ratios indicate the increase/decrease in risk of depression associated with one standard deviation increase in birth weight.
Birth weight adjusted for gestational age using the 1990 Child Growth reference charts
Adjusted for gestational age as above, but also for age, educational qualifications, social class, perceived financial strain and whether in receipt of social security benefits.
We found weak relations between longer reported duration of gestation and lower prevalence ratios for current depressive symptoms and having ever been treated for depression (P=0.040 and P=0.028, respectively; prevalence ratios (95 percent CIs) for both associations 0.98 (0.96, 1.00), n=5150). Recorded duration of gestation was available for fewer women; prevalence ratios for current depressive symptoms and past treatmentfor depression were 0.97 (0.94, 1.00), (P=0.08, n=2003) and 0.96 (0.93, 0.99) (P=0.006, n=1999), respectively. Adjustment for potential confounding variables made little difference to the associations with reported duration of gestation, but had some effect on associations with recorded duration of gestation (adjusted P-values 0.05 and 0.08 for current depressive symptoms and having ever been treated for depression, respectively).
DISCUSSION
We found no apparent relationship between our measures of depression and birth weight, whether the latter was reported by the woman or recorded in the hospital records at the time of her birth. This is one of the larger studies of the relationship between birth weight and depressive symptoms reported to date in women, so our statistical power is high and the 95 percent confidence intervals around our prevalence ratios are narrow. We have used two different assessments of depressive symptoms, unlike other studies, and found no relationship with birth weight. Although we do not have recorded birth weights and gestational ages on all the women in the study, reported birth weights were improved by information provided by parents and there was reasonable agreement between the reported birth weights and those recorded in hospital records among women for whom both were available. Nonetheless, there is error in reported birth weights and gestational ages as the Bland-Altman plots in Figures 2 and 3 show, and this might have contributed to obscuring a relationship with depressive symptoms. Strikingly though, no evidence of a relationship was seen in the group with more accurate birth weights.
Depressive symptoms were assessed in two ways, but both methods have their weaknesses; studies using standardized clinical interviews would be needed to address this limitation, though none have been reported to date. For our first measure, we considered those who reported ever having being treated for depression, anxiety or other mental health problem. This measure is broader than depression per se, although most of the treatments will have been for depression, or mixed anxiety and depression (16). It provides a summary of the lifetime experience of depression of a severity that led the woman to ask for help. While it is possible that women might under-report past treatment for depression, the question was asked in questionnaire that was self-completed by the woman at the end of an interview with a research nurse when considerable rapport had developed.
Our second measure, the GHQ-12, assesses current symptoms of depression and anxiety, including depression that might be undiagnosed. However, this measure is also not specific for depression as it includes anxiety and other symptoms. As a screening instrument, the GHQ-12 has a low threshold of severity for the identification of possible ‘cases’ compared to a standardized clinical interview. It is also sensitive to recent changes in psychological well-being and will include ‘false positives’ with mild transient psychological disturbance. The prevalence of cases in this study (32 percent) is similar to rates of 27 and 30 percent found among women in the annual British Household Panel Surveys (17, 18), but is lower than the rate of 22 percent found in a British community survey using a standardized clinical interview (16). It is possible that we failed to find an association with birth weight because our measures of depressive symptoms also included other symptoms , such as anxiety, which are not related to birth weight. However, this seems unlikely to be the whole explanation, as previous research using questions from the GHQ-12 did find an association with birth weight (6).
Our results contribute to the studies that have examined the relationship between birth weight and depressive symptoms. While a number of studies have reported significant associations, this is not universal and no association was found in a particularly large study of men (4). Additionally, some studies have pointed to associations in women but not in men or vice versa. Notably, our age group of 20-34 years is not dissimilar to the two studies that found associations in women but not men in their twenties (1, 2). However, our study, which focused solely on women, cannot address the question of whether relationships between birth weight and depression differ in men and women.
These various studies are providing a confusing picture of whether a relationship between birth weight and depressive symptoms exists and point to a need for a systematic review of the literature in this area. It is possible that positive publication bias has led studies reporting an association to be over-represented in the literature and if so, then the relationship might be weaker than the published studies indicate. Conversely, however, birth weight is a poor proxy summary of development in utero and there may be detrimental aspects of fetal development that are only weakly summarized by birth weight but that contribute to the development of depression in adulthood. In exploratory analyses we found some evidence for a weak association between a shorter duration of gestation at birth and later depressive symptoms, though the relationship is not as strong as reported in an older Finnish cohort (11). Limitations in our gestational age data (either reported or abstracted from the clinician’s assessment in the labor ward records) precludes detailed exploration of this association in our study, but we would encourage its examination elsewhere. The issue of whether maternal depression in pregnancy or post-natally affects risk of depression in the offspring, or alters the relationship between birth weight and depression, has been addressed but no association was found (1). It appears that greater understanding of fetal development and early maternal and other influences on the fetus and child is needed. Studies recording information on such developmental influences are required before assessment of the early origins of depression can be developed to a greater extent.
ACKNOWLEDGEMENTS
We are grateful to the General Practitioners in Southampton who made this study possible, to Southampton Women’s Survey staff, and particularly to the women of Southampton for taking part. The Southampton Women’s Survey is grateful for financial support from the UK Medical Research Council, the University of Southampton, and the Dunhill Medical Trust.
References
- 1.Alati R, Lawlor DA, Mamun AA, et al. Is there a fetal origin of depression? Evidence from the Mater University Study of Pregnancy and its outcomes. Am J Epidemiol. 2007;165:575–582. doi: 10.1093/aje/kwk036. [DOI] [PubMed] [Google Scholar]
- 2.Gale CR, Martyn CN. Birth weight and later risk of depression in a national birth cohort. Br J Psychiatry. 2004;184:28–33. doi: 10.1192/bjp.184.1.28. [DOI] [PubMed] [Google Scholar]
- 3.Thompson C, Syddall H, Rodin I, et al. Birth weight and the risk of depressive disorder in late life. Br J Psychiatry. 2001;179:450–455. doi: 10.1192/bjp.179.5.450. [DOI] [PubMed] [Google Scholar]
- 4.Osler M, Nordentoft M, Nybo Andersen A. Birth dimensions and risk of depression in adulthood: cohort study of Danish men born in 1953. Br J Psychiatry. 2005;186:400–3. doi: 10.1192/bjp.186.5.400. [DOI] [PubMed] [Google Scholar]
- 5.Rice F, Harold GT, Thapar A. The effect of birth-weight with genetic susceptibility on depressive symptoms in childhood and adolescence. Eur Child Adolesc Psychiatry. 2006;15:383–91. doi: 10.1007/s00787-006-0545-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiles NJ, Peters TJ, Leon DA, et al. Birth weight and psychological distress at age 45-51 years. Results from the Aberdeen Children of the 1950s cohort study. Br J Psychiatry. 2005;187:21–28. doi: 10.1192/bjp.187.1.21. [DOI] [PubMed] [Google Scholar]
- 7.Cheung YB, Khoo KS, Karlberg J, et al. Association between psychological symptoms in adults and growth in early life: longitudinal follow up study. BMJ. 2002;325:749–52. doi: 10.1136/bmj.325.7367.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berle JO, Mykletun A, Daltveit AK, et al. Outcomes in adulthood for children with foetal growth retardation. A linkage study from the Nord-Trondelag Health Study (HUNT) and the Medical Birth Registry of Norway. Acta Psychiatr Scand. 2006;113:501–9. doi: 10.1111/j.1600-0447.2005.00704.x. [DOI] [PubMed] [Google Scholar]
- 9.Barker DJP, Osmond C, Rodin I, et al. Low weight gain in infancy and suicide in adult life. BMJ. 1995;311:1203–4. doi: 10.1136/bmj.311.7014.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Räikkönen K, Peonen A-K, Kajantie E, et al. Length of gestation and depressive symptoms at age 60 years. Brit J Psychiatry. 2007;190:469–74. doi: 10.1192/bjp.bp.106.022145. [DOI] [PubMed] [Google Scholar]
- 11.Somerset W, Newport DJ, Ragan K, et al. Depressive disorders in women: from menarche to beyond the menopause. In: Keyes CLM, Goodman SH, editors. Women and depression: a handbook of the social, behavioural and biomedical sciences. Cambridge University Press; Cambridge: 2006. [Google Scholar]
- 12.Inskip HM, Godfrey KM, Robinson SM, et al. Cohort profile: The Southampton Women's Survey. Int. J. Epidemiol. 2006;35:42–48. doi: 10.1093/ije/dyi202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldberg D, Williams P. A User’s Guide to the General Health Questionnaire. NFER-Nelson; Windsor: 1988. 1988. [Google Scholar]
- 14.Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole TJ, Freeman JV, Preece MA. British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Statistics in Med. 1998;17:407–29. [PubMed] [Google Scholar]
- 16.Meltzer M, Gill B, Petticrew M. The prevalence of psychiatric morbidity among adults aged 16-64, living in private households, in Great Britain. Office of Population Censuses and Surveys; London: 1995. [Google Scholar]
- 17.Weich S, Sloggett A, Lewis G. Social roles and gender difference in the prevalence of the common mental disorders. Br J Psychiatry. 1998;173:489–493. doi: 10.1192/bjp.173.6.489. [DOI] [PubMed] [Google Scholar]
- 18.Weich S, Sloggett A, Lewis G. Social roles and the gender difference in rates of the common mental disorders in Britain: a 7-year, population-based cohort study. Psychol Med. 2001;31:1055–1064. doi: 10.1017/s0033291701004263. [DOI] [PubMed] [Google Scholar]