Abstract
Objectives:
(1) To find out the prevalence of dementia in the study population and its social determinants. (2) To explore the family caregivers’ perceptions and their support needs.
Materials and Methods - Study Setting:
This study was undertaken in the field practice area of 55 villages of three Primary Health Centres in Villupuram District of Tamil Nadu.
Study Design:
An exploratory mixed-methods study design, where a qualitative method (key informant interview) was followed by a quantitative method (survey).
Sample Size:
A representative sample of 1300 respondents was selected by two-stage sampling.
Analysis:
Manual content analysis was done for qualitative data. Multiple logistic regression was performed on quantitative data.
Results:
The prevalence of dementia among study sample was found to be 3.1%. The determinants for dementia were age, sex, socioeconomic status, and previous involvement in family decision making and cardiovascular risk factors. The family caregivers strongly felt that caregiving interferes with their personal and professional life; they also felt that caregiving is an integral part of Indian culture, and the elderly prefer home-based care. Caregivers preferred government owned public health facility for medical care. All the responding caregivers strongly felt that they are not adequately trained in caregiving.
Conclusions and Recommendations:
Routine screening of elderly for early identification of dementia and its medical and social risk factors should be initiated in primary health care facility. Care of caregivers should be seen as an integral part of dementia care program.
Keywords: Caregivers, Dementia, India, Old age, Rural
INTRODUCTION
India is amidst a demographic transition with a growing trend toward an ageing population. The aging population (aged ≥ 60 years) has been estimated to double-up from 8% in the year 2010 to 19% in the year 2050.[1] Correspondingly, we are experiencing an increase in the incidence of noncommunicable diseases, including dementia. Dementia is a syndrome due to disease of the brain – usually of a chronic or progressive nature – in which there is disturbance of multiple higher cortical functions, including memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgment. Consequently, the person loses his ability to perform even everyday activities and develops various behavioral problems. It cripples not only the people who have it, but also overwhelms their caregivers and families. Dementia is one of the major causes of disability and dependency among older people worldwide, and it even increases the risk of death by 2–2.5 times. Thus, it is emerging as an important public health issue; but has not yet received enough attention in developing countries like India.[2] The most common subtype of dementia is Alzheimer's disease which accounts for two-third of the cases in those over 65 years of age. Previous studies have reported prevalence figures ranging from 0.84% to 3.5% in rural India.[3] Knowledge of the prevalence and social determinants help in developing the context-specific community-based programs.
The role of family level caregivers is crucial in the management of dementia. In the West, it has been noted that the caregivers are at risk of developing stress, depression, cardiovascular problems, and other health complications as a result of prolonged caregiving.[4] There is a growing emphasis over the care of caregivers as part of dementia management. In India, not much is known about the challenges faced by family level caregivers of dementia patients. Hence, this study was carried out with the following objectives.
To find out the prevalence of dementia in the study population and its social determinants
To explore the family level caregivers’ perceptions and their support needs.
MATERIALS AND METHODS
Study area and setting
This study was undertaken in the field practice area of the Rural Health Training Centre at Thiruvennainallur under the Department of Community Medicine, Sri Manakula Vinayagar Medical College and Hospital (SMVMCH), Puducherry. It consisted of 55 villages in three Primary Health Centres (Thiruvennainallur, Iruvelpattu, and Sirumadurai) in Villupuram District of Tamil Nadu. The study area had a total population of 137,599 in 27,177 households. In Villupuram district, overall literacy is 72%, and one-fourth of the population lives below poverty line. The main occupation of the residents has been cultivation of agricultural land and daily wage laborers. There is sufficient land irrigation done through channels/canals, wells, tanks, and other sources.[5]
Study design
It was an exploratory mixed-methods study design [Figure 1] where a qualitative method (key informant interview [KII]) was followed by a quantitative method (survey).[6]
Figure 1.
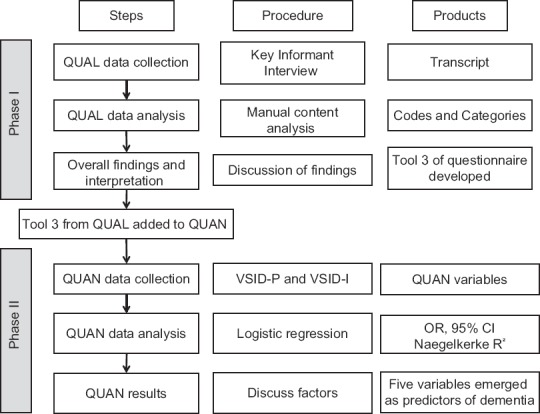
Visual diagram of the study design
Phase I: Qualitative data collection
Six, KII were undertaken with the experts in the field of community-based geriatric care in the study area, assuming that they know the dynamics of caregiving at the household level. A trained interviewer interviewed the key informants using semi-structured guidelines at the prefixed date, time, and venue. The interviews were audio-recorded. The guidelines consisted of broad, open-ended questions on the challenges faced by caregivers and the solutions to it. The transcripts were prepared verbatim. Manual content analysis of the transcripts was done. Inductive and deductive codes were derived from the transcripts. Later, similar codes were merged together to form the categories.[7] Any disagreements were resolved by discussion. The findings were used in developing a context-specific questionnaire for the caregivers interview in this study (Tool 3).
Phase II: Quantitative data collection
Sample size
Considering the percentage of the geriatric population suffering from dementia to be 3.5%,[3] design effect-2, absolute precision of 1.5% and 10% nonresponse, the sample size of 1300 was considered adequate [Calculated by Epi_Info (6.04d), which is a public domain statistical software developed by Centre for Disease Control, Atlanta, USA and World Health Organization, Geneva, Switzerland].
Study participants
All elderly people ≥65 years and the primary caregiver of that person at the household level.
Study duration
The data was collected between July 2013 and April 2014.
Sampling and respondents
A list of all the villages in the study area and their population was obtained from the local Block Development Office of Thiruvennainallur. The desired sample was chosen by a two-stage sampling technique. In the first stage, the number of elderly participants to be interviewed in each village was decided by the “probability proportional to size” method. In the second stage, systematic random sampling was done to select the households in each village. In the selected house, a respondent (≥65 years) and one primary caregiver were selected. If there was more than one elderly person in the house, then one respondent was chosen by a lottery method. If there was no elderly person in the selected house, then the next adjacent house was selected.
Tools used for data collection
Vellore Screening Instrument for Dementia-Patient version (VSID-P - Tool 1) and Vellore Screening Instrument for Dementia-Informant version (VSID-I - Tool 2); both comprising of 10 items were used. This tool was constructed at a place which has a culture very similar to that of the study population and was validated for use in a community setting. A combination of both patient and informant version was reported to have a sensitivity of 80% and specificity of 92%.[8] As mentioned above, the information given by key informants was used to develop a context-specific questionnaire for the caregivers (Tool 3). It was a five point “Likert type scale” to measure the range and level of the intensity of the various problems faced by the primary caregivers.[9] The predesigned questionnaires were pilot tested on 30 volunteers, who were respondents (≥65 years) and their caregivers in a village other than the study area to check the wording and the appropriateness of the questions in the questionnaire.
Later, the trained investigator paid house-to-house visit. After getting informed consent, the information on sociodemographic details such as age, gender, socioeconomic status, occupation, education, health insurance, living arrangements, religion, and membership in self-help groups, utilization of pension scheme and addictions was obtained. Socioeconomic status was assessed by type of ration card, which is being distributed by the Government of Tamil Nadu under the Public Distribution System. The detailed information about each respondent was obtained by using Tool 1 and Tool 2. Further, a primary caregiver was interviewed using Tool 3 when a responding old person was suspected to have dementia.
Ascertaining the diagnosis of dementia
All those patients with a VSID-P score ≤3 and VSID-I score ≤8 were considered as “potential cases” of dementia by the investigator.[8] In psychiatry, since the diagnosis primarily rely on the history of patient and the information given by their caregivers, a qualified psychiatrist carefully reviewed the information provided in the scanned copies of Tool 1 and Tool 2 and in addition also obtained an additional short case summary on onset, duration, progression of symptoms, and functional deterioration to ascertain the final diagnosis. The information collected was considered to be reasonably adequate for the psychiatrist to make a final diagnosis in all potential cases, except in couple of cases, where the interviewer was asked to go back in the community to obtain some clarifications. Diagnostic and Statistical Manual of Mental Disorders-IV criteria were used while ascertaining the final diagnosis.[10]
The clearance was obtained from the Research Committee and the Institutional Ethics Committee of SMVMCH, Puducherry. Those study subjects who were diagnosed to have dementia were referred to seek specialist care and management.
Quantitative data analysis
The data were entered and analyzed using Epi_info (version 3.5.1) software package and SPSS 12.0.1 software (SPSS Inc., Chicago, Illinois, USA) package. Chi-square (χ2) test was applied to proportions to test the level of significance. The level of significance was fixed at 0.05.
Multivariate analysis
Multiple regression analysis was used to identify the combinations of variables that best predict the risk of the development of dementia. Eleven sociodemographic and one health predictors were loaded using the “Enter” selection method. Social security variable was created by clubbing the variables such as old age pension, membership in self-help groups, and free ration by the government. The multiple coefficients of determination (R2) were used as the goodness-of-fit statistic for the model: It represents the proportion of variance in the outcome variable that can be accounted for by the predictors in the model. Statistical significance was set at 5% (P < 0.05).
RESULTS
Findings from qualitative interviews
Five categories emerged from the interview data of key informants. They are (1) the role of caregivers, (2) risks faced by caregivers, (3) supportive factors and obstacles (4) role of the family, and (5) suggestions for improvement in caregiving. These are described below as:
Role of caregivers
According to key informants, the role of caregivers should be supportive; like helping them with their daily activities, and giving additional support when required. They need to be adaptable and should have a service attitude.
“The caregivers need to wake them up. They have to help them in brushing, cleaning themselves, washing clothes, cleaning their surroundings, eating food, and other things.”
As mentioned by the respondents, the caregivers themselves are at risk of (1) medical, (2) emotional, (3) social, and (4) financial problems. The medical problems could be risk of getting any infection and developing noncommunicable diseases like hypertension due to stress. The caregivers might develop mental health problems such as depression, anxiety, anger, stress, boredom, and poor adjustment. Some caregivers might face social isolation, marital discord as well as loss of job/payments leading to financial problems.
“The caregivers may develop tension, hypertension, and emotional problems.” “Some financial remuneration has to be arranged for them.”
Supportive factors and obstacles
The supportive factors were related to sharing of caregiving responsibilities with other family members, recognition, training, previous experience, awareness, and having a source of decent income and appreciation by other family members. The obstacles were criticism, lack of cooperation, lack of trust, financial problems, boredom, and longing to take a break.
“The caregivers will or should be appreciated socially when they take care of the elderly in a proper way.”
Role of family
Family members need to be aware of old age and its related problems. Hence, they should be oriented to emotional, psychological, social, and financial needs of an elderly person.
“The work of caregivers has to be shared by other family members joint family is the best caregiving unit in our country.”
Suggestions for the improvement in care provided to patients of dementia
The key informants offered the following suggestions – (1) training and support system for the caregivers, (2) retention of Indian tradition of respecting and caring elders at their home, (3) financial support to caregivers, (4) medical care and periodic screening for the elderly, and (5) awareness in the society.
Findings from quantitative survey
Out of 1304 respondents, 42 (3.2%) were “suspected” to have dementia and 41 (3.1%) were confirmed to have dementia (27 male and 14 female).
Out of 1304 respondents, 719 (55.1%) were male and remaining 585 (44.9%) were female. The mean age of the respondents was 71.21 (±6.2 standard deviation [SD]) years, where the mean age of the male 71.78 (±6. 2 SD) was significantly higher than that of female respondents 70.51 (±6.09 SD) (P < 0.05). About 256 (19.6%) respondents were “below the poverty line” and majority 1020 (78.2%) belonged to “Other” category and 28 (2.1%) did not have the ration card. There was no difference between male and female with respect to socioeconomic status. Regarding education, 845 (64.8%) were illiterate, 266 (20.4%) had primary education, 94 (7.2%) had a middle school education, 84 (6.4%) had a high school education, and 15 (1.1%) had a higher secondary education and above. Illiteracy was significantly higher among females (84.4%) as compared to males (48.8%) (P < 0.001). As compared to females, significantly more proportion of males had primary school education, middle school education and high school education (P < 0.001). About 835 (64%) responding old persons had a “not working” status with a significant preponderance for male gender while 20% were involved in the household level work with preponderance for the female gender. Noteworthy, 899 (68.9%) respondents had a health insurance in the Chief Minister's comprehensive health insurance scheme which was significantly higher among male (74.7%) than female (61.9%) (P < 0.05) [Table 1].
Table 1.
Background characteristics of the respondents
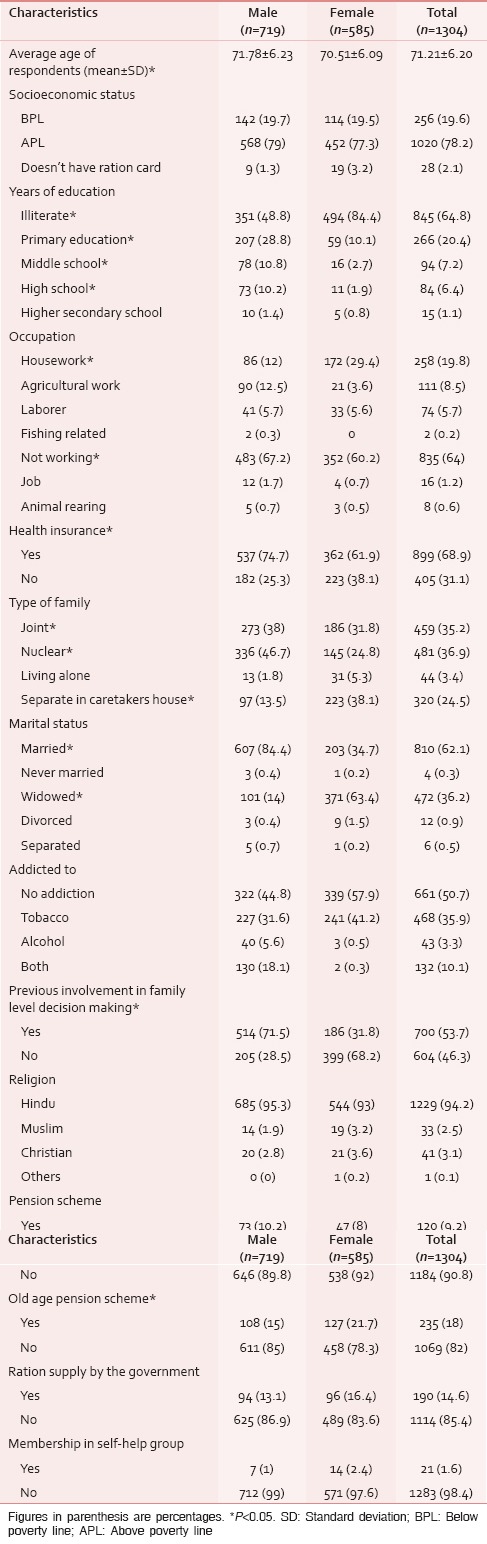
As seen in Table 1, among the total respondents, 481 (36.9%) lived in nuclear families, 459 (35.2%) lived in joint families, 320 (24.5%) lived separately in the caretaker's house, and 44 (3.4%) lived alone. Significantly, more males lived in joint (38%) and nuclear families (46.7%), whereas more females (38.1%) lived separately in caretaker's house. About 810 (62.1%) respondents were married, 472 (36.2%) were widowed, 12 (0.9%) were divorced, 6 (0.5%) were separated, and 4 (0.3%) never married. The proportion of married males (84.4%) was significantly more than that of married females (34.7%) while the proportion of widowed females (63.4%) was significantly more than that of widower males (14%) (P < 0.001). There were no sex differences seen in other categories.
About 700 (53.7%) respondents were previously involved in family level decision making, male (71.5%) were significantly more than female (31.8%) (P < 0.001). About 120 (9.2%) elderly were receiving a pension at the time of the survey. About 235 (18%) respondents reported receiving old age pension, in which females were significantly more (21.7%) than males (15%) (P < 0.05). Nearly 190 (14.6%) respondents reported to receive rice supply by the Government and 21 (1.6%) respondents had membership in self-help groups [Table 1].
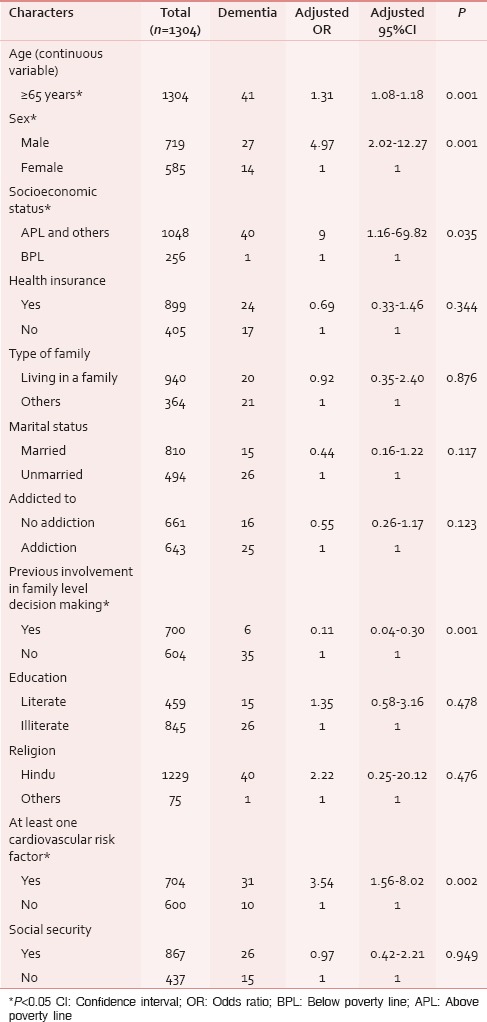
In multivariate analysis, five variables emerged as significant predictors for the risk of developing dementia. The risk of developing dementia among respondents increases about 1.31 times (CI: 1.08–1.18) for a unit increase in age (P < 0.001). Male respondents were at 4.97 times (CI: 2.02–12.27) higher risk of developing dementia as compared to female (P < 0.001). The respondents above poverty line were at 9 times (CI: 1.16–69.82) higher risk of developing dementia as compared to those below poverty line (P < 0.05). The odds of developing dementia in those previously involved in family level decision making were 0.11 times (CI: 0.04–0.30) as that of those not involved previously in it. Those with at least one cardiovascular risk factor were at 3.54 times (CI: 1.56–8.02) higher risk of developing dementia as compared to those without it (P < 0.05). The Nagelkerke pseudo - R2 value for the final model was 33.7% [Table 2].
Table 2.
Multivariate logistic regression analysis for the determinants of dementia
Out of 41 caregivers of dementia patients, 2 (4.8%) were male, and 39 (95.1%) were female. The mean age of the caregivers was 48.07 (±13.54 SD) years, where the mean age of the female was 48.28 (±13.84 SD) which was higher than that of male 44 (±4.2 SD). Among the caregivers, 18 (43.9%) were daughters in law, spouse 10 (24.4%), and daughters were 8 (19.5%). Of the remaining two were the son (4.9%), one sister, a grand-daughter, and grandson each (2.4%). Among those, 23 (59%) were involved in housework, 8 (19.5%) were working as laborers, 4 (9.8%) had a job, 3 (7.3%) were not working, 2 (4.8%) were doing agricultural work, and 1 (2.4%) was involved in animal rearing.
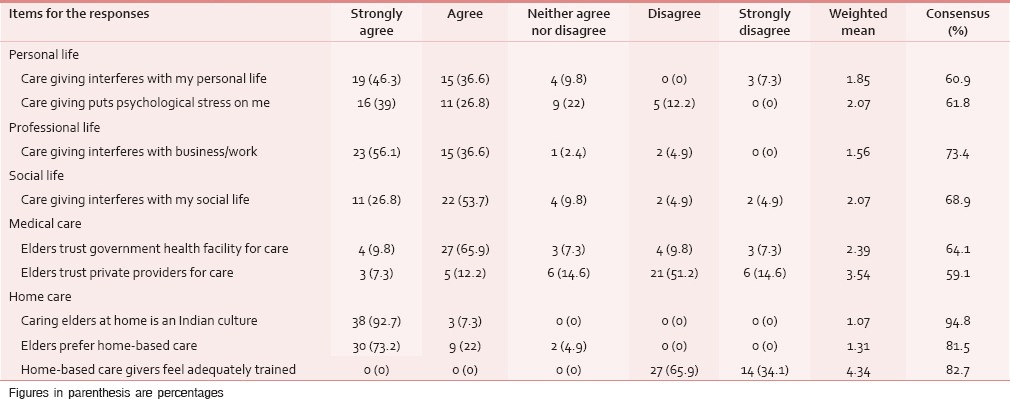
The caregivers strongly felt that caregiving interfered in their personal life (weighted mean: 1.85; consensus: 60.9%) and professional (work) life (weighted mean: 1.56; consensus: 73.4%). Noteworthy, most of them also strongly agreed that it is part of our Indian culture (weighted mean: 1.07; consensus: 94.8%) to care for old people at home. Also, caregivers had a strong opinion that old people prefer home-based care (weighted mean: 1.31; consensus: 81.5%).
Caregivers also stated that caregiving put psychological stress on them (weighted mean: 2.07; consensus: 61.8%) and it interfered with their social life (weighted mean: 2.07; consensus: 68.9%). Caregivers also stated that the elders preferred a government health facility for medical care (weighted mean: 2.39; consensus: 64.1%). All the responding caregivers strongly felt that they were not adequately trained in caregiving (weighted mean: 4.34; consensus: 82.7%) [Table 3].
Table 3.
Caregivers perspectives and their challenges
DISCUSSION
The prevalence of dementia was found to be 3.1%. Factors such as rising age, male sex, better socioeconomic status, and lack of previous involvement in family decision making were the social determinants of dementia. The presence of at least one cardiovascular risk factor emerged as a health determinant for dementia. The caregivers strongly felt that caregiving interferes with their personal life and professional (work) life. All of them strongly agreed that caring for elders is an integral part of Indian culture. Caregivers strongly mentioned that old people prefer home-based care and preferred government health facility for care. All the responding caregivers strongly felt that they are not adequately trained in caring for an old person with dementia.
In this study, the prevalence of dementia was found to be 3.1%, which is consistent with the other studies done in rural parts of Southern India.[3,11,12]
Factors such as rising age, male sex, better socioeconomic status, and lack of previous involvement of the old person in the family decision were the social determinants of dementia. Tripathi et al. in North India found that the sociocultural factors like cognitively stimulating activities, active socialization, and living in joint families were protective against dementia.[13] The knowledge of these social determinants is important for developing targeted interventions in a community-based dementia care program. It is also useful to inform family level caregivers the importance of the practice of involving old people in family level decision making process or other cognitively stimulating activities as they are likely to delay the development of dementia.
In this study, the presence of at least one cardiovascular risk factor was found to be a health determinant for dementia. A study in urban Kerala found that increasing age, family history, and hypertension were significant risk factors for dementia.[11] Hence, there is a need to emphasize the reduction of cardiovascular risk factors and promotion of a healthy lifestyle among elderly and middle-aged people. Notably, this has been emphasized in the World Alzheimer's Disease Report 2014.[14]
The family caregivers strongly felt that caregiving interfered in their personal life and professional life. All of them also strongly felt that, it is part of our Indian culture. Family level caregivers strongly opined that old people prefer home-based care. Government health facility was preferred by more caregivers as compared to a private health facility. All the responding caregivers strongly felt that they are not adequately trained in caregiving This implies that there is an unmet need of caregivers for guidance on how to efficiently perform their role of caregiving without allowing it to disturb their own quality of life. Another study done in Kerala also found that the caregivers (n = 29) face a lot of stress and psychiatric morbidity.[15] It is to be noted that the care of patients with dementia seems highly interprofessional in nature, where one of the important stakeholder is family caregivers, who also need medical, psychological, financial, and social care.
The findings of the present study are based on a representative sample drawn systematically in a wider geographical area of three primary health centres in a rural setting. The data was collected using a valid questionnaire for screening in a community setting, and the final diagnosis was confirmed by qualified Psychiatrist. However, the limitation of the present study should be kept in mind. A degree of inaccuracy in ascertaining the final diagnosis might be present as the final diagnosis was based upon scanned copies of the field interviews and a case summary made by the investigator; without a direct examination by the psychiatrist.
Dementia is a disease that has no cure and has a debilitating course. Hence, exploring the preventive strategies is important. The findings of this study have implications for the development of a comprehensive community-based preventive program focused on early identification by screening, risk factors reduction. It also offers the direction for the formulation of supportive policies and programs for the caregivers of this chronic degenerative condition. We found cardiovascular risk factors as one of the determinants of dementia; suggesting a hypothesis of possible association between the rising incidence of other noncommunicable diseases, and rising incidence of dementia, which may be tested in the future studies.
CONCLUSION
Routine screening of the elderly for early identification of dementia should be done in OPD settings of the primary health care facility. As preferred by the caregivers, the government health care facility should be prepared to offer care for the dementia patients. Early identification and reduction of cardiovascular risk factors may help in the prevention of dementia in the community setting. A support system for the family caregivers should be seen as an integral part of any program which intends to provide comprehensive care for dementia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Scomegna P. Today's Research on Aging. 2012. [Last cited on 2015 Sep 07]. pp. 1–3. Available from: http://www.prb.org/pdf12/todaysresearchaging25.pdf .
- 2.World Health Organization. Dementia: A Public Health Priority. World Health Organization. 2012. [Last cited on 2014 Aug 15]. Available from: http://www.apps.who.int/iris/bitstream/10665/75263/1/9789241564458_eng.pdf?ua=1 .
- 3.Jotheeswaran AT. Prevalence of Dementia in India – Rethinking the Evidence [M.Sc. Dissertation] Institute of Psychiatry London: King's College. 2007 [Google Scholar]
- 4.Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues Clin Neurosci. 2009;11:217–28. doi: 10.31887/DCNS.2009.11.2/hbrodaty. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.District Profile Format. 2013. [Last cited on 2015 May 29]. Available from: http://www.kvktvm.org/image/Pdf%20reports/DISTRICT%20PROFILE%20FORMAT%20TO%20KVKS.pdf .
- 6.Bergman MM, editor. London: Sage Publications Ltd; 2009. Advances in Mixed Methods Research: Theories and Applications. [Google Scholar]
- 7.Creswell JW, Plano Clark VL. London (United Kingdom): Sage Publications Ltd; 2007. Designing and Conducting Mixed Methods Research; pp. 142–5. [Google Scholar]
- 8.Stanley R, Kuruvilla A, Kumar S, Gayathri K, Mathews P, Abraham V, et al. The Vellore screening instruments and strategies for the diagnosis of dementia in the community. Int Psychogeriatr. 2009;21:539–47. doi: 10.1017/S104161020900903X. [DOI] [PubMed] [Google Scholar]
- 9.5-Point vs. 6-Point Likert Scales. [Last cited on 2009 May 12]. Available from: http://www.infosurv.com/images/Likert_Scale_Debate.pdf .
- 10.4th ed. Washington (DC): American Psychiatric Association; 1994. [Last cited on 2010 Mar 08]. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV; p. 866. Available from: http://www.psychiatryonline.com/DSMPDF/dsm-iv.pdf . [Google Scholar]
- 11.Shaji S, Bose S, Verghese A. Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry. 2005;186:136–40. doi: 10.1192/bjp.186.2.136. [DOI] [PubMed] [Google Scholar]
- 12.Shaji S, Promodu K, Abraham T, Roy KJ, Verghese A. An epidemiological study of dementia in a rural community in Kerala, India. Br J Psychiatry. 1996;168:745–9. doi: 10.1192/bjp.168.6.745. [DOI] [PubMed] [Google Scholar]
- 13.Tripathi M, Vibha D, Gupta P, Bhatia R, Srivastava MV, Vivekanandhan S, et al. Risk factors of dementia in North India: A case-control study. Aging Ment Health. 2012;16:228–35. doi: 10.1080/13607863.2011.583632. [DOI] [PubMed] [Google Scholar]
- 14.Prince M, Albanese E, Guerchet M, Prina M. World Alzheimer Report 2014 Dementia and Risk Reduction: An Analysis of Protective and Modifiable Factors. 2014. [Last cited on 2015 May 18]. Available from: https://www.alz.co.uk/research/WorldAlzheimerReport2014.pdf .
- 15.Shaji KS, George RK, Prince MJ, Jacob KS. Behavioral symptoms and caregiver burden in dementia. Indian J Psychiatry. 2009;51:45–9. doi: 10.4103/0019-5545.44905. [DOI] [PMC free article] [PubMed] [Google Scholar]


