Abstract
AIM
To compare the agreement of anterior chamber depth (ACD) and central vault measurements obtained by anterior segment optical coherence tomography (AS-OCT) and ultrasound biomicroscopy (UBM) of post surgical high myopic eyes with posterior chamber phakic intraocular lens (Visian ICL; STAAR Surgical) implantation.
METHODS
Fifty-two phakic eyes of 28 high myopic patients who underwent implantable Collamer lens (ICL) surgery for the correction of high myopia were studied. The postoperative ACD, the distance between the corneal endothelium and the anterior surface of ICL (cornea-ICL) and the central vault were measured with the AS-OCT system and the UBM system. Intraclass correlation coefficient (ICC) and the Bland-Altman plot were used to evaluate the repeatability and agreement of two devices.
RESULTS
The mean ACD, cornea-ICL and central vault in the 52 phakic eyes after ICL surgery was 3.19±0.28 mm, 2.47±0.28 mm, 0.50±0.19 mm by AS-OCT and 3.13±0.25 mm, 2.49±0.25 mm, 0.44±0.19 mm by UBM, respectively. Pairwise comparison of ACD and central vault measurements showed significant differences between AS-OCT and UBM (P<0.05). However, no statistically significant difference was found between these imaging techniques in cornea-ICL (P>0.05). The Pearson correlation coefficient (r) between AS-OCT and UBM measurements for ACD, cornea-ICL and vault was 0.88, 0.80 and 0.89, respectively (P<0.001). The ICC was 0.89-0.94 for the measurements of AS-OCT and UBM. Bland-Altman analysis showed the 95% limits of agreement of ACD, cornea-ICL, central vault measurements between these two devices were -0.20 to 0.32 mm, -0.36 to 0.32 mm and -0.12 to 0.24 mm, respectively.
CONCLUSION
Central ACD and vault measurements using AS-OCT demonstrated a slight significantly higher value than using UBM in phakic eyes after ICL surgery. These two devices should not be used interchangeably for measurements of central ACD and vault in patients after phakic intraocular lens implantation.
Keywords: anterior chamber depth, vault, phakic intraocular lens, anterior segment imaging, optical coherence tomography, ultrasound biomicroscopy
INTRODUCTION
Implantable Collamer lens (ICL) surgery has become a predictable and widely accepted technique for the correction of high myopia. Although this technique has been reported to be a relatively safe, effective, alterable, and even reversible surgical approach, patients must consider a variety of possible complications, such as lens opacification, endothelial cell loss, high intraocular pressure (IOP), rotation of ICL, anterior chamber inflammation[1]–[6].
The anterior segment parameters are the crucial indication of suitability of refractive surgery and post-surgical evaluation. Anterior chamber depth (ACD) is one of the most important parameters for evaluating patients' eligibility of ICL surgery and selection proper size of ICL[7]. ACD value less than 2.80 mm is the contraindication for ICL surgery. Central vault, which defined as the distance between the back surface of the ICL and the front surface of the lens, is of crucial value for estimation the safety of surgery postoperatively. Excessive vault is a risk factor of inducing glaucoma, and insufficiency vault is responsible for the formation of anterior subcapsular cataract[4]. Recently, several studies reported that central vault gradually decreases by time after ICL implantation[8]–[10]. Hence, an accurate and objective ACD and central vault assessment are both of great value to ICL surgery.
Ultrasound biomicroscopy (UBM) can produce in vivo high resolution cross-section images of anterior segment and objective quantitative measurements of anterior segment parameters[11]. However, it is a contact apparatus that requiring topical anesthesia and an immersion bath with a coupling medium. Anterior segment optical coherence tomography (AS-OCT), a non-contact tomographic and biomicroscopic device, has recently been introduced as an alternative imaging modality to UBM. It is based on low-coherence interferometry and commonly used for measurement of the anterior segment biometric parameters in glaucoma and refractive surgery.
Previous studies have reported the comparison of UBM and AS-OCT of ACD measurements with phakic eyes, pseudophakic eyes and eyes after iris-fixated phakic intraocular lens implantation and different documented results were obtained. Among those studies, there was none of them comparing these methods of ACD, and the central vault measurements in patients with high myopia after ICL implantation[12]–[14]. The purpose of this investigation was to evaluate the repeatability of anterior section parameters measurements using AS-OCT and UBM and determine the agreement between the measurement methods for phakic eyes after ICL surgery.
SUBJECTS AND METHODS
Subjects
All the study procedures were conducted in accordance with the tenets of the World Medical Association's Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of Zhongshan Ophthalmic Center and all participants were informed about the study procedure and gave their consent.
A total of 52 eyes of 28 participants (15 males, 13 females) who had undergone ICL implantation at Zhongshan Ophthalmic Center between February 2009 and March 2011 were enrolled in the study. Patients with any of the following findings were excluded for surgery: anterior chamber depth less than 2.80 mm; endothelial cell count less than 2000 cells/mm2; IOP greater than 21 mm Hg; a history of ocular surgery or uveitis, cataract, glaucoma, diabetes mellitus, other ocular or systemic autoimmune disease; younger than 18 years old.
Methods
Surgical procedure of implantable Collamer lens surgery
The size of the ICL was determined with a STAAR sizing calculation formula that based on the measurement of horizontal corneal diameter (white-to-white, WTW) and ACD with Orbscan II Topographer (version 3.12, Bausch&Lomb). The high myopic patients had standard implantation of ICL (STAAR Surgical) by the same surgeon (Yu KM, corresponding author). Briefly, two peripheral iridectomies were created at the 10:30 and 1:30 clock-hour position using neodymium:YAG laser to prevent postoperative pupillary block. Patients were given cycloplegic agents 3 times at 10-minute intervals before surgery. After topical anesthesia, an injector cartridge (STAAR Surgical) was used to insert ICL through a 3.0 mm corneal incision after placement of a hyaluronic acid material (Singclean, Hangzhou, Zhejiang Province, China) in the anterior chamber. A specially designed intraocular spatula was used to place 4 footplates of ICL on the ciliary sulcus. The remaining viscoelastic material was entirely washed out with balanced salt solution. Postoperatively, tobramycin 0.3%-dexamethasone 0.1% eyedrops (Tobradex) was administered locally 4 times daily for 2wk.
Anterior segment parameters measurement
AS-OCT (Carl Zeiss, Germany) is a computerized instrument that acquires and analyzes cross-sectional tomographic of the anterior eye segment. The high-resolution images of the eye were obtained by a low-coherence interferometry optical technique without contacting the eye. The light source is a 1310 nm super-luminescent light emitting diode (SLD), which the wavelength has a limited penetration depth into the eye. In our study, the anterior segment single-scan mode, on the horizontal meridian was performed in a dark room. The eye of the seated subjects was instructed to focus on the optical target in the system with their chin on the chinrest and forehead against the forehead rest. Then, the image was captured when a vertical white line along the center of the cornea happened. The anterior chamber parameters were measured by drawing calipers.
UBM (SW-3200L, SUOER, Tianjin, China) was performed by an experienced technician. The principle of image formation for UBM is analogous to an ultrasound B-scan. It acquires high resolution (50 µm) ocular anterior segment information with high-frequency ultrasound (50-100 MHz) energy and transforms to two-dimensional images by digital technology. The examination was performed in a dark room with ambient illumination below 5 lx. The eyes were topical anesthesia of proparacaine 0.5% with the patients in a supine position. An appropriate size eyecup filled with methylcellulose 2% as a coupling agent was applied. During the examination, the contralateral eye should fix on the target to minimize the variation. UBM images of the horizontal anterior segment were recorded without pressure to the globe and touching of the cornea. The anterior chamber parameters were performed using the integrated standard UBM software system.
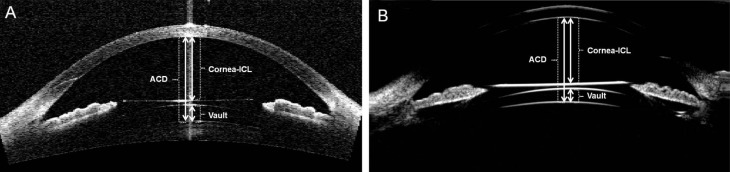
All subjects were examined using AS-OCT, UBM in the same order on the same day under controlled dark conditions by the same experienced operators. The ACD was measured from the center of the corneal endothelial to the anterior surface of the crystalline len. The distance between the corneal endothelium and anterior surface of ICL was defined as the cornea-ICL. The vault was defined as the distance from the back surface of the ICL to the front surface of the crystalline len (Figure 1).
Figure 1. Anterior segment measured by AS-OCT (A) and UBM (B) in phakic eyes after ICL implantation.
ACD: Anterior chamber depth; Cornea-ICL: Distance between the corneal endothelium and anterior surface of ICL; Vault: Distance between the back surface of the ICL and the front surface of the lens.
Statistical Analysis
The data was presented as the mean±standard deviation (SD) and the 95% limits of agreement (LoA) was defined as the mean±1.96 SD. All anatomical parameters were accord with normal distribution which was confirmed by the Kolmogorov-Smirnov test (all P>0.05). Paired t-tests were applied to compare measurements between AS-OCT and UBM with patients after ICL surgery using IBM SPSS Statistics 19. The Pearson coefficient was calculated to assess the correlation between anatomical parameters measured with each imaging technique. In addition, intraclass correlation coefficient (ICC) was analyzed to determine the reliability between the measurements of two devices. Bland-Altman analysis for the agreement between the two methods was studied. All tests were two tailed, and P values less than 0.05 were considered statistically significant.
RESULTS
The measurements were performed in the 52 eyes of 28 participants (15 males, 13 females) after ICL implantation. The mean age was 30.2±7.8y (range, 21 to 49y). The mean preoperative spherical equivalent (SE) was -13.09±3.96D (range, -8 to -22 D). The mean preoperative refractive cylinder was -1.34±0.98 D (range, 0 to -5D). The mean implanted ICL power was -18.19±3.16 D (range, -13 to -23 D). No complications occurred during the surgical procedures and follow up time. The AS-OCT and UBM measurements were performed at the last follow up time. The mean follow up time was 19.00±8.11mo (range, 13 to 39mo).
Comparison of Measurements
Table 1 compares the AS-OCT and UBM measurements for anterior section parameters of the 52 phakic eyes postoperatively. Both ACD and vault measured with AS-OCT was significantly higher than that obtained with the UBM system (all P<0.05). However, the cornea-ICL measured with these two devices was not statistically significant (P=0.413).
Table 1. Comparison of anterior section parameters measurements using AS-OCT and UBM.
| Parameters | AS-OCT | UBM | Mean difference | T | P |
| ACD | 3.19±0.28 | 3.13±0.25 | 0.06±0.13 | 3.171 | 0.003 |
| Cornea-ICL | 2.47±0.28 | 2.49±0.25 | -0.02±0.17 | -0.825 | 0.413 |
| Vault | 0.50±0.19 | 0.44±0.19 | 0.06±0.09 | 4.817 | 0.000 |
AS-OCT: Anterior segment optical coherence tomography; UBM: Ultrasound biomicroscopy; ACD: Anterior chamber depth; Cornea-ICL: Distance between the corneal endothelium and anterior surface of ICL; Vault: Distance between the back surface of the ICL and the front surface of the lens. Paired t-tests were used to compare measurements between AS-OCT and UBM. P values less than 0.05 were considered statistically significant.
mm
Interchangeability and Agreement
The ICC values in Table 2 shows the high reliability of AS-OCT and UBM for anterior section parameters measurements (all P<0.001). Table 2 shows the Pearson correlation coefficient for ACD, cornea-ICL, central vault measurements. A statistically significant good correlation was found between these two devices in all parameters [Pearson (r) all P<0.001].
Table 2. Results of ICC and Pearson correlation coefficient (r) between AS-OCT and UBM measurements for each parameter.
| Parameters | ICC | P (ICC) | Pearson (r) | P (r) |
| ACD | 0.94 | 0.00 | 0.88 | 0.00 |
| Cornea-ICL | 0.89 | 0.00 | 0.80 | 0.00 |
| Vault | 0.94 | 0.00 | 0.89 | 0.00 |
AS-OCT: Anterior segment optical coherence tomography; UBM: Ultrasound biomicroscopy; ICC: Intraclass correlation coefficient; Pearson (r): Pearson correlation coefficient; ACD: Anterior chamber depth; Cornea-ICL: Distance between the corneal endothelium and anterior surface of ICL; Vault: Distance between the back surface of the ICL and the front surface of the lens. P values less than 0.05 were considered statistically significant.
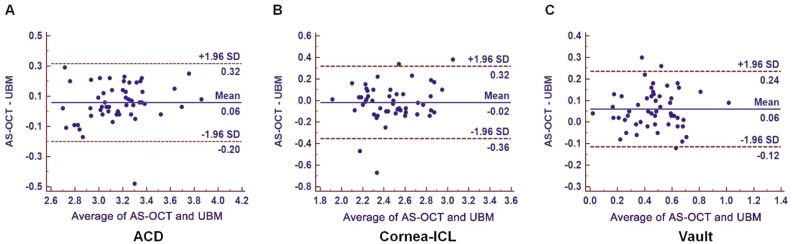
Figure 2 shows Bland-Altman analysis of the agreement for AS-OCT and UBM measurements. The 95% LoA of ACD, cornea-ICL, central vault measurements between these two devices were -0.20 to 0.32 mm, -0.36 to 0.32 mm and -0.12 to 0.24 mm, respectively.
Figure 2. Bland-Altman plots of the differences between AS-OCT and UBM of ACD (A), Cornea-ICL (B), Vault(C) measurements in the 52 high myopic eyes.
The vertical axis represents the difference between these measurements and the horizontal axis shows their mean. The 95% LoA are shown with dashed lines, and the middle bold line represents the mean difference between these measurements. All scales in mm. ACD: Anterior chamber depth; Cornea-ICL: Distance between the corneal endothelium and anterior surface of ICL; Vault: Distance between the back surface of the ICL and the front surface of the lens.
DISCUSSION
In this study, we evaluated the agreement and interchangeability of central ACD, cornea-ICL and central vault measurements between AS-OCT and UBM in high myopia eyes after implantation of ICL. Several previous studies have compared ACD measurements with AS-OCT and UBM in phakic eyes and pseudophakic eyes. Piñero et al[15] found that AS-OCT measurements slightly overestimated ACD in phakic eyes by a mean of 0.09 mm compared with UBM but without statistically significant differences (P>0.05), and the measurements were well correlated. The range of agreement between two devices in ACD mearsurements was 0.20 mm and not clinically relevant. Dada et al[16] who found a mean ACD of 2.85 mm using AS-OCT and 2.78 mm using UBM (P>0.05) and the two methods showed good correlation (r=0.97). Zhang et al[13] found that the mean ACD was 3.91 mm by AS-OCT and 3.76 mm by UBM in pseudophakic eyes (P<0.05) and 2.97 mm by AS-OCT and 2.90 mm by UBM in phakic eyes (P>0.05). The 95% LoA of ACD measurements with the AS-OCT and UBM was -0.11 to 0.25 in phakic eyes and -0.32 to 0.62 mm in pseudophakic eyes, and the authors concluded that AS-OCT and UBM measurements can be used interchangeably in phakic eyes but not advisable to use in pseudophakic eyes. Our results showed that ACD measurements were higher with AS-OCT by a mean of 0.058 mm compared with UBM and with statistically significant differences (P<0.05). Our findings were agreed with previously studies that the ACD measurements with AS-OCT and UBM were well correlated (r=0.88, P<0.05). The 95% LoA between the two instruments was -0.20 to 0.32 mm which was not clinical acceptable. Our results indicated that these two devices in high myopia eyes after ICL surgery cannot be used interchangeably for ACD measurement.
According to all we know so far, there has been no study reported in previous literature that comparison of cornea-ICL and central vault measurements with AS-OCT and UBM. In our study, we found AS-OCT gave a significantly higher reading than UBM for central vault measurement in eyes after ICL implantation (P<0.05). However, AS-OCT and UBM in high myopia eyes after ICL surgery yield comparable results of cornea-ICL measurements, with no statistically significant differences between them (P>0.05). A statistically significant good correlation was found between the devices for cornea-ICL and vault measurement (r=0.80, 0.89, respectively, P<0.001). Bland-Altman plots show the 95% LoA of cornea-ICL, vault measurements between these two devices were -0.36 to 0.32 mm and -0.12 to 0.24 mm, respectively. Some previous studies defined an excellent vault as 0.25 to 0.75 mm[17]. The range of agreement between the imaging systems was not clinically acceptable for high myopia patient who evaluating the safety of ICL implantation postoperatively. This indicates that AS-OCT and UBM cannot be used interchangeability for the measurement of cornea ICL and vault.
The accuracy and repeatability of anterior segment parameter measurements for the Visante OCT system and UBM system has reported in previous studies and indicated a high level of agreement between the devices in this parameter[18]. Visante OCT had a slight tendency to give larger values than UBM. There are several reasons that might be causing the difference between AS-OCT and UBM: firstly, AS-OCT uses an infrared light of a 1310 nm wavelength to obtain the structures of the anterior segment, however, UBM uses ultrasound energy and must be performed through an immersion bath with a coupling medium. There is an internal fixation for the examined eye by AS-OCT, however, the contralateral eye should fix the external target to minimize the variation during UBM examination. Secondly, AS-OCT is performed with the patient seated, and UBM is performed with the patient supine with a coupling medium. Ishikawa[19] analysed that the water filled with eyecup may put pressure on the eyeball and may influence the results. Thirdly, light conditions and accommodation status were not the same during the measurement of two devices, as reported by Piñero et al[15]. Finally, with both instruments, you must draw the tangential lines with a digital calibrated caliper and this process can vary from one measurement to another depending on where you locate the tangential point. These factors may cause the underestimation of ACD and central vault using the UBM method. AS-OCT and UBM can provide an objective way of measuring of ACD, cornea-ICL and central vault. However, we could not determine whether OCT or UBM was more precise for measuring ACD and central vault because of lacking a gold standard method for anterior segment. UBM can obtain clear images through opaque media and provide the visualization of the ciliary body. However, there is a risk for infection or corneal injury by this contact examination. As a noncontact imaging device, the measuring procedure of AS-OCT is fast and easy for the examiner and patient, especially better than UBM for examining patients in early postoperative period. However, this device has an important limitation that it cannot measure any object behind any opaque structure.
In conclusion, both AS-OCT and UBM own their advantages and disadvantages for anterior section parameters measurements for evaluating the safety of ICL surgery. AS-OCT demonstrated a slight significantly higher value than using UBM in phakic eyes after ICL surgery. Therefore, these two devices were not advisable to use interchangeably for measurements of central ACD and vault in patients after phakic ICL implantation.
Acknowledgments
Conflicts of Interest: Zhang J, None; Luo HH, None; Zhuang J, None; Yu KM, None.
REFERENCES
- 1.Igarashi A, Shimizu K, Kamiya K. Eight-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am J Ophthalmol. 2014;157(3):532–539.e1. doi: 10.1016/j.ajo.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Ju Y, Gao XW, Ren B. Posterior chamber phakic intraocular lens implantation for high myopia. Int J Ophthalmol. 2013;6(6):831–835. doi: 10.3980/j.issn.2222-3959.2013.06.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gomez-Bastar A, Jaimes M, Graue-Hernandez EO, Ramirez-Luquin T, Ramirez-Miranda A, Navas A. Long-term refractive outcomes of posterior chamber phakic (spheric and toric implantable collamer lens) intraocular lens implantation. Int Ophthalmol. 2014;34(3):583–590. doi: 10.1007/s10792-013-9860-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernandes P, González-Méijome JM, Madrid-Costa D, Ferrer-Blasco T, Jorge J, Montés-Micó R. Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J Refract Surg. 2011;27(10):765–776. doi: 10.3928/1081597X-20110617-01. [DOI] [PubMed] [Google Scholar]
- 5.Kamiya K, Shimizu K, Kobashi H, Igarashi A, Komatsu M. Three-year follow-up of posterior chamber toric phakic intraocular lens implantation for moderate to high myopic astigmatism. PLoS One. 2013;8(2):e56453. doi: 10.1371/journal.pone.0056453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sari ES, Pinero DP, Kubaloglu A, Evcili PS, Koytak A, Kutluturk I, Ozerturk Y. Toric implantable collamer lens for moderate to high myopic astigmatism: 3-year follow-up. Graefes Arch Clin Exp Ophthalmol. 2013;251(5):1413–1422. doi: 10.1007/s00417-012-2172-8. [DOI] [PubMed] [Google Scholar]
- 7.Lim DH, Lee MG, Chung ES, Chung TY. Clinical results of posterior chamber phakic intraocular lens implantation in eyes with low anterior chamber depth. Am J Ophthalmol. 2014;158(3):447–454. doi: 10.1016/j.ajo.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Schmidinger G, Lackner B, Pieh S, Skorpik C. Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology. 2010;117(8):1506–1511. doi: 10.1016/j.ophtha.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 9.Cao X, Tong J, Wang Y, Zhou T, Ye B, Li X, Shen Y. Long-term ultrasound biomicroscopy observation of position changes of a copolymer posterior chamber phakic intraocular lens. J Cataract Refract Surg. 2014;40(9):1454–1461. doi: 10.1016/j.jcrs.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 10.Alfonso JF, Fernández-Vega L, Lisa C, Fernandes P, González-Meijome J, Montés-Micó R. Long-term evaluation of the central vault after phakic Collamer® lens (ICL) implantation using OCT. Graefes Arch Clin Exp Ophthalmol. 2012;250(12):1807–1812. doi: 10.1007/s00417-012-1957-0. [DOI] [PubMed] [Google Scholar]
- 11.Kojima T, Yokoyama S, Ito M, Horai R, Hara S, Nakamura T, Ichikawa K. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153(4):632–637.e1. doi: 10.1016/j.ajo.2011.06.031. [DOI] [PubMed] [Google Scholar]
- 12.Nakakura S, Mori E, Nagatomi N, Tabuchi H, Kiuchi Y. Comparison of anterior chamber depth measurements by 3-dimensional optical coherence tomography, partial coherence interferometry biometry, Scheimpflug rotating camera imaging, and ultrasound biomicroscopy. J Cataract Refract Surg. 2012;38(7):1207–1213. doi: 10.1016/j.jcrs.2012.02.036. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Q, Jin W, Wang Q. Repeatability, reproducibility, and agreement of central anterior chamber depth measurements in pseudophakic and phakic eyes: optical coherence tomography versus ultrasound biomicroscopy. J Cataract Refract Surg. 2010;36(6):941–946. doi: 10.1016/j.jcrs.2009.12.038. [DOI] [PubMed] [Google Scholar]
- 14.Nolan W. Anterior segment imaging: ultrasound biomicroscopy and anterior segment optical coherence tomography. Curr Opin Ophthalmol. 2008;19(2):115–121. doi: 10.1097/ICU.0b013e3282f40bba. [DOI] [PubMed] [Google Scholar]
- 15.Piñero DP, Plaza AB, Alio JL. Anterior segment biometry with 2 imaging technologies: very-high-frequency ultrasound scanning versus optical coherence tomography. J Cataract Refract Surg. 2008;34(1):95–102. doi: 10.1016/j.jcrs.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 16.Dada T, Sihota R, Gadia R, Aggarwal A, Mandal S, Gupta V. Comparison of anterior segment optical coherence tomography and ultrasound biomicroscopy for assessment of the anterior segment. J Cataract Refract Surg. 2007;33(5):837–840. doi: 10.1016/j.jcrs.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Kamiya K, Shimizu K, Komatsu M. Factors affecting vaulting after implantable collamer lens implantation. J Refract Surg. 2009;25(3):259–264. doi: 10.3928/1081597X-20090301-04. [DOI] [PubMed] [Google Scholar]
- 18.Zhou SY, Wang CX, Cai XY, Huang D, Liu YZ. Optical coherence tomography and ultrasound biomicroscopy imaging of opaque corneas. Cornea. 2013;32(4):e25–e30. doi: 10.1097/ICO.0b013e318261eb2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ishikawa H. Anterior segment imaging for glaucoma: OCT or UBM? Br J Ophthalmol. 2007;91(11):1420–1421. doi: 10.1136/bjo.2007.121038. [DOI] [PMC free article] [PubMed] [Google Scholar]