Abstract
AIM
To analyze the correlation of Goldmann applanation tonometer (GAT), I-Care tonometer and Tono-Pen tonometer results in young healthy persons, and to investigate the influence of central corneal thickness (CCT) on intraocular pressure (IOP) measurements recorded with these tonometers.
METHODS
We conducted a pilot clinical study in 78 eyes of 78 subjects aged 22-28 years old (44 women and 34 men; mean age 23.8±1.19y). IOP was measured using GAT, I-Care and Tono-Pen tonometers, followed by measurements of CCT. Statistical analysis was performed using SPSS 20.0.
RESULTS
The mean IOPs and standard deviation (±SD) for GAT, I-Care and Tono-Pen were 15.62±2.281 mm Hg, 16.29±2.726 mm Hg and 16.32±2.393 mm Hg, respectively. The mean CCT was 555.15±29.648 µm. Clear positive correlations between GAT and I-Care, GAT and Tono-Pen, and I-Care and Tono-Pen tonometers were found (r=0.867, P<0.001; r=0.861, P<0.001; r=0.915, P<0.001, respectively). In comparison between devices, Bland–Altman analysis showed a significant mean difference (MD) in the measurements by GAT and I-Care of −0.679 mm Hg and by GAT and Tono-Pen of −0.705 mm Hg ( P<0.001), but there was no significant difference between I-Care and Tono-Pen ( P>0.05). Both non-gold standard tonometers were affected by CCT; that is, both I-Care and Tono-Pen tonometer values were significantly higher with higher CCT means (>555 µm; MD=−1.282, P<0.001; MD=−0.949, P<0.001, respectively) compared with GAT.
CONCLUSION
Both I-Care and Tono-Pen tonometers overestimated IOP compared with the GAT values. Either the I-Care or Tono-Pen tonometer could be used instead of GAT because there was no significant difference between their results. Higher CCT values (>555 µm) were associated with overestimated IOP values.
Keywords: Goldmann tonometer, I-Care tonometer, Tono-Pen tonometer, corneal thickness, intraocular pressure
INTRODUCTION
Many different intraocular pressure (IOP) measurement devices are commercially available. The recognized gold standard, the Goldmann's applanation tonometer (GAT), was introduced in the mid-20th century[1]. It is considered to be the most accurate modern tonometer[2], although some limitations associated with the instrument have been reported, including the influence of central corneal thickness (CCT) on IOP readings, tear film, refractive surgery, the use of topical anesthetic and fluorescein dye, corneal surface irregularity (which makes an accurate IOP determination difficult, if not impossible), the non-utility for patients who cannot be examined by slit-lamp biomicroscopy, the requirement of a certain amount of experience and risk of secondary infection via exposure to the cornea[1],[3]–[5].
The electronic Tono-Pen XL was introduced in 1988 and was the first commercially-available portable tonometer[6]–[7]. This device uses the same physical principle as GAT but the applanated area is much smaller (approximately 1.0 mm in diameter)[8]. Its advantage is that it is usable in both upright and supine positions and is not dependent on a source of alternating current[1].
In 2005, the new hand-held I-Care rebound tonometer (RBT)—a reproducible method of determining IOP in humans[9]-became available[10]. The main advantages of this device are that no topical anesthetic is required (which is especially helpful in the examination of children) and its portability[3]–[4],[11]–[13].
The aim of this study was to evaluate the utility of the RBT and Tono-Pen XL by comparing it with the GAT in young healthy people, and to investigate a correlation between IOP readings and CCT.
SUBJECTS AND METHODS
From September to December 2013, we used GAT, I-Care and Tono-Pen tonometers to examine 78 eyes in 78 healthy individuals (34 males, 44 females, mean age 23.8±1.19y) who were seen at the Vilnius University Hospital Santariskiu Klinikos. All participants had had no history of contact lens wear, corneal surface disease, or intraocular surgeries. There were no eyes with ocular hypertension or glaucoma. Tests were conducted from 10 a.m. to 12 p.m. in a sitting position. This study was approved by the Vilnius University Faculty of Medicine Human Ethics Committee. All patients gave their informed consent prior to inclusion in the study.
The IOP of both eyes was measured; however, only right eyes were included in the study. CCT was measured with the ultrasound contact pachymeter (Pocket Pachymeter, Quantel Medical, CP, Cournon-D'Auvergne, France) and repeated five times. The pachymeter automatically calculated the mean CCT. To avoid possible reduction in IOP induced by contact applanation tonometry, IOP measurements were made sequentially in the following order: I-Care (I-Care Finland Oy, Finland), Tono-Pen XL (TPA; Reichter Inc., Depew, New York, USA) and GAT (Haag-Streit AG, Bern, Switzerland). The median of three readings per instrument was used for comparison among tonometers. Three consecutive measurements per patient were made with I-Care. When the patient blinked or an error sign (“-”) was displayed, the data were discarded and measurements were repeated until such error signs were not displayed. We used a calibrated GAT connected to a slit-lamp microscope. Three sequential IOP readings were also measured. The average of the IOPs was used for analysis.
The survey was carried out following the principles laid down in Helsinki Declaration. Statistical analysis was made using SPSS version 20.00. Correlation between the groups was defined using the Pearson correlation coefficient. The compatibility of the methods was analyzed using the Bland–Altman diagram.
RESULTS
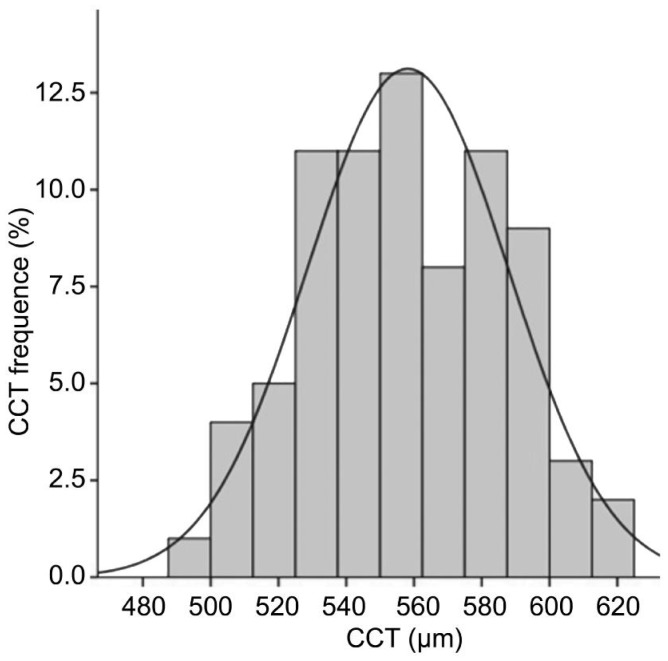
In total, 78 participants [44 (56.41%) women and 34 (43.59%) men] were examined. Patients were 22-28 years old (mean 23.8 ±1.19y). The identified CCT in the tested group of people ranged from 499 to 623 µm. The mean CCT was 555.15 ±29.648. As indicated in Figure 1, the CCT distribution corresponded to the normal distribution under the Gauss Law.
Figure 1. CCT distribution corresponded to the normal distribution under the Gauss Law.
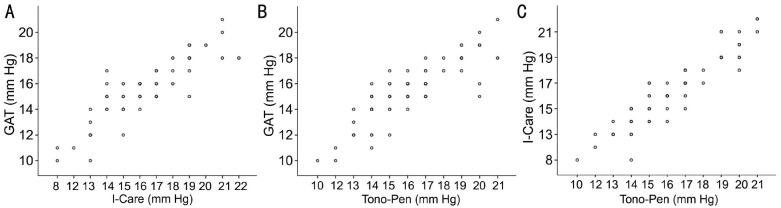
The lowest IOP values measured with the Tono-Pen tonometer, I-Care and GAT were 10, 8 and 10 mm Hg, respectively. The highest IOP values measured were 21, 22, and 21 mm Hg (Table 1), respectively. The mean IOP values measured with the Tono-Pen tonometer, I-Care and GAT were 16.32±2.393, 16.29±2.726, and 15.62±2.281 mm Hg, respectively. Clear positive correlations between GAT and I-Care, GAT and Tono-Pen and I-Care and Tono-Pen tonometers were found (r=0.867, P<0.001; r=0.861, P<0.001; r=0.915, P<0.001, respectively). The correlations between measurements were very strong (Figure 2).
Table 1. IOP measurements with Tono-Pen, I-Care and GAT.
| Tonometer | Mean | Minimal value | Maximal value |
| I-Care | 16.29±2.726 | 8 | 22 |
| Tono-Pen | 16.32±2.393 | 10 | 21 |
| GAT | 15.62±2.281 | 10 | 21 |
n=78 (mm Hg)
Figure 2. Correlation between values measured by various tonometers.
A: IOP measurement correlation between values measured by GAT and I-Care tonometers (r=0.867, P<0.001); B: IOP measurement correlation between values measured by GAT and Tono-Pen tonometers (r=0.861, P<0.001); C: IOP measurement correlation between values measured by I-Care and Tomo-Pen tonometers (r=0.915, P<0.001).
The mean differences between GAT and I-Care, GAT and Tono-Pen, and I-Care and Tono-Pen were −0.979±1.363, −0.750±1.239, and −0.026±1.104 mm Hg, respectively.
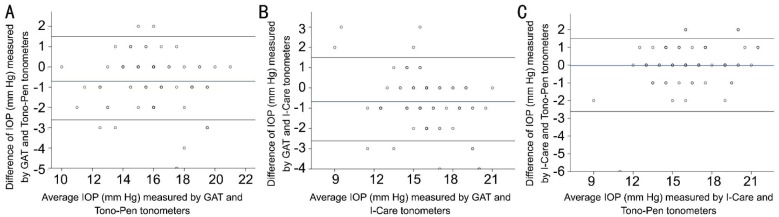
To better compare the two measurements, we performed an agreement analysis suggested by Bland and Altman.
The Bland–Altman plots for all readings are presented in Figure 3. The limits of agreement for GAT and I-Care, GAT and Tono-Pen, and I-Care and Tono-Pen (±1.96 SD) were +1.99 and −3.35 mm Hg, +1.75 and −3.13 mm Hg, and +2.13 and −2.19 mm Hg, respectively. We found that 94.87% of the differences were within the agreement limits of GAT and Tono-Pen and GAT and I-Care, and 98.71% were within the agreement limits of I-Caree and Tono-Pen. In comparison between devices, Bland–Altman analysis showed a significant mean difference (MD) in the measurements by GAT and I-Care of −0.679 mmHg and by GAT and Tono-Pen of −0.705 ( P<0.001), but there was no significant difference between I-Care and Tono-Pen ( P>0.05).
Figure 3. Bland-Altman plot displaying the difference in IOP measurements plotted against mean IOP measuring.
A: Agreement on IOP taken with GAT against Tonopen; B: Agreement on IOP taken with GAT against I-Care; C: Agreement on IOP teaken with I-Care against Tonopen (bottom left). Blue line: mean difference (bias); black lines: 95% of limits of agreement.
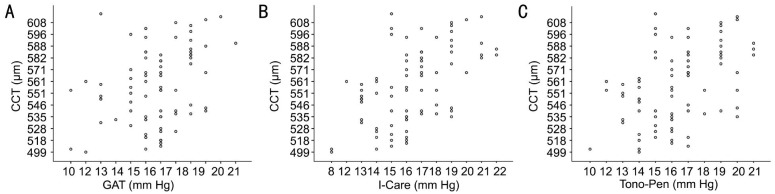
The associations between CCT and IOP measured with GAT (r=0.341, P=0.002), I-Care (r=0.564, P=0.000), and Tono-Pen XL (r=0.462, P=0.000) were all significant (Figure 4). Linear regression analyses also disclosed that both I-Care and Tono-Pen tonometer values were significantly higher with higher CCT means (>555 µm; MD=−1.282, P<0.001; MD=−0.949, P<0.001, respectively; Figure 4) than those for GAT.
Figure 4. Correlation of CCT and IOP measured by various tonometers scatterplots.
A: Scatterplot showing the correlation between CCT and IOP value measured by GAT (r=0.341, P=0.002); B: Scatterplot showing the correlation between CCT and IOP value measured by I-Care tonometer (r=0.564, P=0.000); C: Scatterplot showing the correlation between CCT and IOP value measured by Tono-Pen tonometer (r=0.462, P=0.000).
DISCUSSION
In our study, young healthy people were examined. Measurements performed with the I-Care and the Tono-Pen XL were in good agreement with that of the GAT[14]. In most previous studies, higher I-Care rebound tonometer measured values relative to GAT were detected[3],[5]. In the present study, both non-gold standard tonometers also showed a slight IOP overestimation compared with GAT[3]. Muttuvelu et al[5] found a greater overestimation (central IOP-GAT) than in most previous studies and argued that because the I-Care measurements in those studies were performed with a handheld device, the researchers may have angled or measured a little more to the periphery, which would have tended to reduce the overestimation. Although Smedowski et al[15] and Avitabile et al[16] found no significant difference between GAT and rebound tonometer (RT) IOP values -15.6±3.75 and 15.6±3.5 mm Hg, respectively—our measurements were 15.62±2.281 and 16.29±2.726 mm Hg with the GAT and the RT, and 16.32±2.393 mm Hg with the Tono-Pen XL. The intraocular measurements performed by Ceska et al[17] produced almost identical mean values with the GAT and Tono-Pen XL (16.55±2.95 and 16.13±3.4 mm Hg, respectively).
Some authors[16] have claimed that the Tono-Pen is less affected by corneal biomechanical properties than the GAT because it applanates a smaller area of the cornea. As the Bland–Altman analysis in our study showed, the mean difference in measurements was slightly greater between the GAT and Tono-Pen (−0.705) than between the GAT and I-Care (−0.679).
We found very strong positive correlations between GAT and I-Care and GAT and Tono-Pen (r=0.867, P<0.001; r=0.861, P<0.001, respectively) compared with other studies. For example, Schreiber et al[7] and Baily et al[18] reported the following results: r=0.633 (P<0.001) and r=0.592 (P<0.001), respectively. We also found a very strong positive correlation between the I-Care and Tono-Pen (r=0.915, P<0.001).
The I-CareONE RT was developed for self-measuring IOP and according to Sakamoto et al[19], IOP measurements with this tonometer showed excellent agreement with GAT measurements.
The I-CarePRO was introduced to measure supine patients. One recent study found that the IOP was significantly elevated when the eyeball was against the pillow in the lateral decubitus position (LDP)[20]. The I-CarePRO tonometer, in comparison with its predecessor I-CARE® TA01 evaluated in the past, shows a much smaller average difference in collected values compared with GAT[21].
Yilmaz et al[9] included non-contact airpuff tonometer in their study. The results showed, that non-contact airpuff tonometer and Tono-Pen XL provide IOP measurements comparable to those of the gold standard GAT in normotensive eyes.
Some studies found that higher IOP values showed a more obvious difference between RBT and GAT[13],[22]–[23]. In this study, we did not observe a wide range of IOP values, so this could be a possible reason why the mean IOP differences between the tonometers were small.
The second purpose of our study was to evaluate the influence of CCT on the IOP measurements obtained with the new I-Care tonometer and to calculate how these measurements could be corrected in accordance to CCT.
CCT measurement is a classic and convenient method for measuring corneal properties. However, it is known that the IOP values could be somewhat overestimated in eyes with a thicker cornea and underestimated in eyes with a thinner cornea[5],[13],[24]–[28]. Our results confirmed this and showed that GAT measurements were significantly higher than those of I-Care and Tono-Pen tonometers, with higher CCT means (>555 µm; MD=-1.282, P<0.001; MD=-0.949, P<0.001). Baily et al[18] stated that the difference in IOP was independent of CCT and a diagnosis of glaucoma.
Both I-Care and Tono-Pen tonometers overestimated the GAT values. Both I-Care and Tono-Pen are reliable and can be used equally in place of a GAT because they showed no significant differences in their measurements. Higher CCT values (>555 µm) were correlated with overestimated IOP values.
In our study only young adults were examined. Sakata and Numaga[4] compared IOP readings using the I-CarePro tonometer versus the GAT in late elderly (aged 75y or older) subjects with or without glaucoma and evaluated the influence of CCT on IOP readings. The results showed, that IOP readings measured using the RBT and GAT were within the allowable range in the late elderly subjects with or without glaucoma and the eyes with glaucoma were correlated closely with CCT using each instrument.
Also, in the study we didn't search for possible different measurement abilities for high IOP. In Hohmann et al[29] study, divided all the measurements into three groups (group I <16 mm Hg, group II 16-23 mm Hg and group III >23 mm Hg) and did found that the standard deviation in group III (4.04 mm Hg) was greater than in groups I (1.98 mm Hg) and II (1.79 mm Hg).
Acknowledgments
Conflicts of Interest: Galgauskas S, None; Strupaite R, None; Strelkauskaite E, None; Asoklis R, None.
REFERENCES
- 1.Kirstein EM, Elsheikh A, Gunvant P. Gunvant P, editor. Tonometry-past, present and future. Glaucoma-Current Clinical and Research Aspects. 2011:88–89. [Google Scholar]
- 2.Stamper RL. A history of intraocular pressure and its measurement. Optom Vis Sci. 2011;88(1):E16–28. doi: 10.1097/OPX.0b013e318205a4e7. [DOI] [PubMed] [Google Scholar]
- 3.Kyoung NK, Jeoung JW, Park KH, Yang MK, Kim DM. Comparison of the new rebound tonometer with Goldmann applanation tonometer in a clinical setting. Acta Ophthalmol. 2013;91(5):e392–e396. doi: 10.1111/aos.12109. [DOI] [PubMed] [Google Scholar]
- 4.Sakata R, Numaga J. The utility of rebound tonometer in late elderly subjects. Clin Interv Aging. 2014;9:227–232. doi: 10.2147/CIA.S57644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muttuvelu DV, Baggesen K, Ehlers N. Precision and accuracy of the I-Care tonometer-Peripheral and central IOP measurements by rebound tonometry. Acta ophthalmol. 2012;90(4):322–326. doi: 10.1111/j.1755-3768.2010.01987.x. [DOI] [PubMed] [Google Scholar]
- 6.Handley N. From Blue to blink - a history of glaucoma diagnosis and testing. Glaucoma Forum, Autumn 2002 [Google Scholar]
- 7.Schreiber W, Vorwerk CK, Langenbucher A, Behrens-Baumann W, Viestenz A. A comparison of rebound tonometry (ICare) with TonoPenXL and Goldmann applanation tonometry. Ophthalmologe. 2007;104(4):299–304. doi: 10.1007/s00347-007-1487-z. [DOI] [PubMed] [Google Scholar]
- 8.Schweier C, Hanson JV, Funk J, Töteberg-Harms M. Repeatability of intraocular pressure measurements with I-Care PRO rebound, Tono-Pen AVIA, and Goldmann tonometers in sitting and reclining positions. BMC Ophthalmol. 2013;13:44. doi: 10.1186/1471-2415-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yilmaz I, Altan C, Aygit ED, Alagoz C, Baz O, Ahmet S, Urvasizoglu S, Yasa D, Demirok A. Comparison of three methods of tonometry in normal subjects: Goldmann applanation tonometer, non-contact airpuff tonometer, and Tono-Pen XL. Clin Ophthalmol. 2014;8:1069–1074. doi: 10.2147/OPTH.S6391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahlmann-Noor AH, Puertas R, Tabasa-Lim S, El-Karmouty A, Kadhim M, Wride NK, Lewis A, Grosvenor D, Rai P, Papadopoulos M, Brookes J, Bunce C, Khaw PT. Comparison of handheld rebound tonometry with Goldmann applanation tonometry in children with glaucoma: a cohort study. BMJ Open. 2013;3(4):pii: e001788. doi: 10.1136/bmjopen-2012-001788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pakrou N, Gray T, Mills R, Landers J, Craig J. Clinical comparison of the I-Care tonometer and Goldmann applanation tonometry. J Glaucoma. 2008;17(1):43–47. doi: 10.1097/IJG.0b013e318133fb32. [DOI] [PubMed] [Google Scholar]
- 12.Grigorian F, Grigorian AP, Olitsky SE. The use of the I-Care tonometer reduced the need for anesthesia to measure intraocular pressure in children. J AAPOS. 2012;16(6):508–510. doi: 10.1016/j.jaapos.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Martinez-de-la-Casa JM, Garcia-Feijoo J, Vico E, Fernandez-Vidal A, Benitez del Castillo JM, Wasfi M, Garcia-Sanchez J. Effect of corneal thickness on dynamic contour, rebound, and goldmann tonometry. Ophthalmology. 2006;113(12):2156–2162. doi: 10.1016/j.ophtha.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 14.van der Jagt LH, Jansonius NM. Three portable tonometers, the TGDc-01, the I-CARE and the Tonopen XL, compared with each other and with Goldmann applanation tonometry. Ophthalmic Physiol Opt. 2005;25(5):429–435. doi: 10.1111/j.1475-1313.2005.00318.x. [DOI] [PubMed] [Google Scholar]
- 15.Smedowski A, Weglarz B, Tarnawska D, Kaarniranta K, Wylegala E. Comparison of three intraocular pressure measurement methods including biomechanicl properties of the cornea. Invest Ophthalmol Vis Sci. 2014;55(2):666–673. doi: 10.1167/iovs.13-13172. [DOI] [PubMed] [Google Scholar]
- 16.Avitabile T, Longo A, Rocca D, Amato R, Gagliano C, Castaing M. The influence of refractive errors on IOP measurement by rebound tonometry (I-Care) and Goldmann applanation tonometry. Graefes Arch Clin Exp Ophthalmol. 2010;248(4):585–591. doi: 10.1007/s00417-009-1176-5. [DOI] [PubMed] [Google Scholar]
- 17.Ceska BM, Ferrova K, Filous A, Oskorypová K, Lezatková P, Sedlácková P. Comparative study of intraocular pressure measurements by Goldmann applanation tonometer, noncontact tonometer and TonoPen. Cesk Slov Oftalmol. 2012;68(1):43–46. [PubMed] [Google Scholar]
- 18.Baily C, Dooley I, Collins N, Hickey-Dwyer M. The difference in intraocular pressure readings between 3 applanation tonometers is independent of central corneal thickness, in glaucomatous and nonglaucomatous eyes. J Glaucoma. 2013;23(9):620–623. doi: 10.1097/IJG.0b013e318287abcd. [DOI] [PubMed] [Google Scholar]
- 19.Sakamoto M, Kanamori A, Fujihara M, Yamada Y, Nakamura M, Negi A. Assessment of I-CareONE rebound tonometer for self-measuring intraocular pressure. Acta Ophthalmol. 2014;92(3):243–248. doi: 10.1111/aos.12108. [DOI] [PubMed] [Google Scholar]
- 20.Kim HS, Park KH, Jeoung JW. Can we measure the intraocular pressure when the eyeball is against the pillow in the lateral decubitus position? Acta Ophthalmol. 2013;91(7):e502–e505. doi: 10.1111/aos.12151. [DOI] [PubMed] [Google Scholar]
- 21.Hladíková E, Pluhácek F, Marešová K. Comparison of measurement of intraocular pressure by I-CARE PRO® tonometer and Goldman applanation tonometer. Cesk Slov Oftalmol. 2014;70(3):90–93. [PubMed] [Google Scholar]
- 22.Suman S, Agrawal A, Pal VK. Rebound tonometer: ideal tonometer for meadurements of accurate intraocular pressure. J Glaucoma. 2013;23(9):633–637. doi: 10.1097/IJG.0b013e318285fefd. [DOI] [PubMed] [Google Scholar]
- 23.Munkwitz S, Elkarmouty A, Hoffmann EM, Pfeiffer N, Thieme H. Comparison of the I-Care rebound tonometer and the Goldmann applanation tonometer over a wide IOP range. Graefes Arch Clin Exp Ophthalmol. 2008;246(6):875–879. doi: 10.1007/s00417-007-0758-3. [DOI] [PubMed] [Google Scholar]
- 24.Rosentreter A, Jablonski KS, Mellein AC, Gaki S, Hueber A, Dietlein TS. A new rebound tonometer for home monitoring of intraocular pressure. Graefes Arch Clin Exp Ophthalmol. 2011;249(11):1713–1719. doi: 10.1007/s00417-011-1785-7. [DOI] [PubMed] [Google Scholar]
- 25.Tonnu PA, Ho T, Newson T, El Sheikh A, Sharma K, White E, Bunce C, Garway-Heath D. The influence of central corneal thickness and age on intraocular pressure measured by pneumotonometry, non-contact tonometry, the Tono-Pen XL, and Goldmann applanation tonometry. Br J Ophthalmol. 2005;89(7):851–854. doi: 10.1136/bjo.2004.056622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinez-de-la-Casa JM, Garcia-Feijoo J, Castillo A, Garcia-Sanchez J. Reproducibility and clinical evaluation of rebound tonometry. Invest Ophthalmol Vis Sci. 2005;46(12):4578–4580. doi: 10.1167/iovs.05-0586. [DOI] [PubMed] [Google Scholar]
- 27.Iliev ME, Goldblum D, Katsoulis K. Comparison of rebound tonometry with Goldmann applanation tonometry and correlation with central corneal thickness. Br J Ophthalmol. 2006;90(7):833–835. doi: 10.1136/bjo.2005.089870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brusini P, Salvetat ML, Zeppieri M, Tosoni C, Parisi L. Comparison of I-Care tonometer with goldmann applanation tonometer in glaucoma patients. J Glaucoma. 2006;15(3):213–217. doi: 10.1097/01.ijg.0000212208.87523.66. [DOI] [PubMed] [Google Scholar]
- 29.Hohmann J, Schulze-Schwering M, Chirambo Nyaka T, Moyo V, Kayange PC, Doycheva D, Batumba NH, Spitzer MS. Comparison of the I-Care tonometer with the Goldmann tonometer in Malawi. Ophthalmologe. 2012;109(11):1098–1102. doi: 10.1007/s00347-012-2599-7. [DOI] [PubMed] [Google Scholar]