Abstract
AIM
To review indications and corneal tissue use for penetrating and lamellar surgery between 2002 and 2011.
METHODS
The surgical reports of corneal grafts performed during 2002-2011, using tissues supplied by the Eye Bank of Piedmont (Italy), were reviewed retrospectively. Patient demographic data, date of intervention, indication for surgery, and surgical technique used were recorded. Surgical techniques included penetrating keratoplasty (PK), deep anterior lamellar keratoplasty (DALK) and endothelial keratoplasty (EK). The χ2 test was used to compare the distribution of indications and types of surgical technique used, for corneal grafts done during 2002-2006 versus those done during 2007-2011.
RESULTS
The number of corneal grafts increased by 30.7% from 2002-2006 to 2007-2011 (from 1567 to 2048). Comparing the two periods, both main indications and surgical techniques changed significantly. In 2007-2011, the proportion of interventions for aphakic/pseudophakic bullous keratopathy (from 16.8% to 21.3%), graft failure (from 16.4% to 19.1%) and Fuchs endothelial dystrophy (from 12.8% to 16.7%) all increased significantly (P<0.05), while those for keratoconus decreased significantly (from 35.6% to 27.3%; P<0.001). In 2007-2011, the proportion of PK decreased significantly (from 92.4% to 57.2%; P<0.001) while that of EK and DALK went from 0.4% to 30.2% (P<0.001) and from 7.2% to 12.6% (P<0.001) respectively.
CONCLUSION
During 2002-2011 the number of interventions increased significantly for corneal endothelial diseases and graft failure. The growing demand for interventions for these diseases corresponded to the widespread adoption of EK techniques. The use of DALK also increased, but more moderately than EK procedures.
Keywords: indications for corneal graft, lamellar keratoplasty, penetrating keratoplasty
INTRODUCTION
In recent years, indications for corneal grafts and the surgical techniques employed have been changing. It has been reported that surgery for aphakic and pseudophakic bullous keratopathy (ABK/PBK) is now less frequent[1]–[3]. For treating keratoconus, which is the leading indication for corneal graft in young patients, advances in contact lens technology may have increased the threshold for surgery. Moreover, new therapeutic options, such as intracorneal ring segment implantation and riboflavin/ultraviolet-A-induced collagen cross-linking, have emerged[4]–[5].
For many years penetrating keratoplasty (PK) was the preferred surgical approach for corneal grafts[6]. However new lamellar keratoplasty techniques have recently been developed[7]–[13]. These have clinically-significant advantages over PK[6],[14], and have led to this type of approach's being increasingly preferred over PK[15]–[20].
A precise knowledge of the changes in indications, surgical techniques, and demand for corneal grafts is crucial both to assess patients' needs and to plan eye banks' activity. Moreover, it also provides the possibility of making a comparison of the preferences and decisions of surgeons who operate in different countries. In the light of the evolving situation, this study aimed to review indications and corneal tissue use for penetrating and lamellar surgery between 2002 and 2011.
SUBJECTS AND METHODS
The surgical reports of patients who had undergone corneal grafting between January 1st 2002 and December 31st 2011, using tissues supplied by the Eye Bank of Piedmont (Italy), were reviewed retrospectively. The study was performed with the approval of the Institutional Review Board of Turin Eye Hospital and conducted in accordance with the tenets of the Declaration of Helsinki.
All surgical reports relating to the study period had been received by the Eye Bank of Piedmont from 8 surgical centers. During the study period, these centers had performed more than 90% of the corneal grafts in northwestern Italy. The surgical reports had been compiled by surgeons at the end of the intervention and provided the following data: recipient's demographic information (name, gender, date of birth), eye bank case number, date of surgery, eye laterality, indication for surgery, surgical procedure, and any surgical complications or adverse reactions. Only surgical records that had been properly completed were included in the data set for analysis.
The indications for surgery were grouped using a modification of the diagnostic classification proposed by Lindquist et al[21]. The classification included 10 categories: keratoconus, ABK/PBK, graft failure, Fuchs endothelial dystrophy, microbial keratitis, herpetic keratitis, non-infectious keratitis, trauma, stromal dystrophies, and other corneal disorders. Surgical procedures were grouped into three main categories: PK, deep anterior lamellar keratoplasty (DALK), and endothelial keratoplasty (EK). Traditional lamellar grafts (superficial, patch grafts) were not included in the study. Deep anterior keratoplasties were defined as those in which the anterior cornea was replaced down to Descemet membrane, regardless of the surgical technique used. EKs were stratified by the surgical technique into deep lamellar EK, Descemet stripping automated EK, and Descemet membrane EK.
Statistical Analysis
The 10-year study period was subdivided for analytical purposes into two five-year periods: from 1st January 2002 to 31st December 2006; and from 1st January 2007 to 31st December 2011. This subdivision was chosen because the majority of new surgical procedures were introduced in the early years of 2000. The χ2 test was used to compare the distribution of indications and surgical technique used for corneal grafts, in the two time intervals. The type I error was set at 0.05. Data analysis was performed using the SPSS for Windows software (version 10.1, SPSS, Inc.).
RESULTS
The Eye Bank of Piedmont supplied 3615 tissues for corneal grafting during the 10-year study period: 1567 during 2002-2006, and 2048 during 2007-2011. The surgical report was sufficiently complete to meet the inclusion criteria in 3426 (94.8%) of cases.
The recipients were 1146 females (58.1%) and 826 males; mean age at the time of intervention was 67.2±17.5y. The corneal graft was performed in 1704 (49.7%) right eyes and in 1722 (50.3%) left eyes.
Indications for Corneal Graft
During the 10-year study period, indications for corneal graft were, in order of decreasing frequency, keratoconus (1055 cases; 30.8%), ABK/PBK (667 cases; 19.5%), graft failure (615 cases; 18.0%), Fuchs endothelial dystrophy (516 cases; 15.1%), herpetic keratitis (148, 4.3%), microbial keratitis (142 cases; 4.1%), trauma (71 cases; 2.1%), stromal dystrophies (60 cases; 1.8%), non-infectious keratitis (35 cases; 1%) and other corneal disorders (117 cases; 3.4%).
In both five-year periods, keratoconus, ABK/PBK, graft failure and Fuchs endothelial dystrophy were the four most common indications (Table 1). However, their individual proportions changed significantly. In 2007-2011, the proportion of corneal grafts for ABK/PBK, graft failure and Fuchs endothelial dystrophy were significantly higher (P<0.05), and that for keratoconus significantly lower (P<0.05) than they were in 2002-2006. Herpetic and microbial keratitis were the fifth and sixth common indications during the first period. Their order was inverted in the second period, although their proportion did not change significantly. Stromal dystrophies, trauma and non-infectious keratitis were less common indications (<2.5%); the proportion of interventions for these diseases did not change from 2002-2006 to 2007-2011.
Table 1. Distribution of indications for corneal grafts performed in the periods 2002-2006 and 2007-2011.
| Indication | No. of interventions |
Comparison 2002-2006 vs 2007-2011 |
|
| 2002-2006 n=1440 | 2007-2011 n=1986 | P | |
| Keratoconus | 513 (35.6) | 542 (27.3) | <0.001 |
| ABK/PBK | 242 (16.8) | 425 (21.3) | <0.001 |
| Graft failure | 236 (16.4) | 379 (19.1) | 0.04 |
| Fuchs endothelial dystrophy | 184 (12.8) | 332 (16.7) | 0.001 |
| Herpetic keratitis | 59 (4.1) | 89 (4.5) | 0.58 |
| Microbial keratitis | 65 (4.5) | 77 (3.9) | 0.36 |
| Trauma | 32 (2.2) | 39 (2.0) | 0.60 |
| Stromal dystrophies | 31 (2.2) | 29 (1.4) | 0.13 |
| Non-infectious keratitis | 18 (1.2) | 17 (0.9) | 0.25 |
| Others | 60 (4.2) | 57 (2.9) | 0.04 |
ABK/PBK: Aphakic/pseudophakic bullous keratopathy.
n (%)
Type of Surgical Procedure
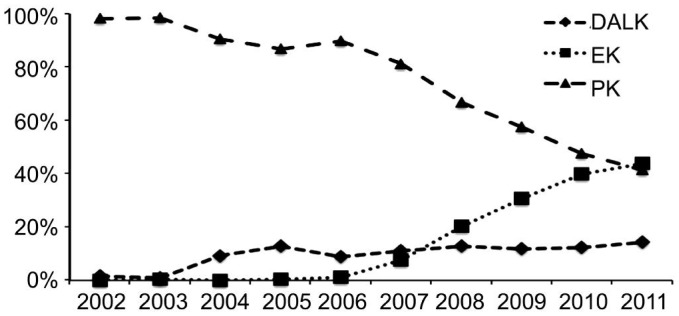
During the 10-year study period, the preferred surgical approach was PK (2466 procedures), followed by EK (606 procedures), and DALK (354 procedures) (Table 2). EK procedures included 580 interventions of Descemet stripping automated EK, 12 of deep lamellar EK, and 14 of Descemet membrane EK. The proportion of PK, EK and DALK performed each year is shown in Figure 1. Comparing the 2 five-year periods, the proportion of PK significantly (P<0.001) decreased and that of DALK and EK significantly (P<0.001) increased in 2007-2011 (Table 2).
Table 2. Type of surgical procedure performed in the periods 2002-2006 and 2007-2011.
| Type of surgical procedure | No. of interventions |
Comparison 2002-2006 vs 2007-2011 |
|
| 2002-2006 n=1440 | 2007-2011 n=1986 | P | |
| Penetrating keratoplasty | 1330 (92.4) | 1136 (57.2) | <0.001 |
| Endothelial keratoplasty | 6 (0.4) | 600 (30.2) | <0.001 |
| DALK | 104 (7.2) | 250 (12.6) | <0.001 |
DALK: Deep anterior lamellar keratoplasty.
n (%)
Figure 1. Proportion of PK, EK and DALK procedures out of total surgeries performed each year from 2002 to 2011.
The surgical approach used for each indication is listed in Table 3. During 2007-2011, the proportion of DALK increased significantly (P<0.001) for the treatment of keratoconus, microbial and herpetic keratitis; the proportion of EK also increased significantly (P<0.001) for the treatment of ABK/PBK, graft failure and Fuchs endothelial dystrophy.
Table 3. Proportion of lamellar keratoplasties performed for different indications in the periods 2002-2006 and 2007-2011.
| Indication | Proportion of lamellar keratoplasties |
Comparison 2002-2006 vs 2007-2011 |
|
| 2002-2006 n=1440 | 2007-2011 n=1986 | P | |
| Keratoconus1 | 77/513 (15.0) | 162/542 (29.8) | <0.001 |
| ABK/PBK2 | 2/242 (0.8) | 263/425(61.9) | <0.001 |
| Graft failure2 | 0/236 (0.0) | 113/379 (29.8) | <0.001 |
| Fuchs endothelial dystrophy2 | 4/184 (2.2) | 224/332 (67.5) | <0.001 |
| Herpetic keratitis1 | 5/59 (8.5) | 28/89 (31.5) | 0.001 |
| Microbial keratitis1 | 8/65 (12.3) | 38/77 (49.3) | <0.001 |
| Trauma | 0/32 (0.0) | 1/39 (2.6) | 0.36 |
| Stromal dystrophies1 | 13/31 (42.0) | 19/29 (65.5) | 0.06 |
| Non-infectious keratitis | 0/18 (0.0) | 1/17 (5.9) | 0.29 |
| Others | 1/60 (1.7) | 1/57 (1.8) | 0.97 |
ABK/PBK: Aphakic/pseudophakic bullous keratopathy. 1Diseases treated using DALK; 2Diseases treated using EK procedures.
n (%)
DISCUSSION
The study showed that the number of corneal grafts increased by 30.7% from 2002-2006 to 2007-2011. This demand was met by the Eye Bank of Piedmont, thanks to the increasing number of donors and additional available tissues. Corneal tissues unsuitable for PK, being in a sub-optimal endothelial condition, were supplied for anterior lamellar graft. Moreover, with modern eye-banking procedures a single donor cornea can provide sufficient tissue for EK plus DALK in two patients.
The increasing number of corneal graft was mainly due to the high demand for interventions for corneal endothelial diseases (ABK/PBK, Fuchs endothelial dystrophy) and graft failure. Both the number and the proportion of interventions for corneal endothelial diseases increased, respectively from 426 to 757, and from 29.6% to 38%. Different factors probably underlay these changes: aging population, large number of cataract operations and, especially, the introduction of EK procedures. ABK/PBK and Fuchs endothelial dystrophy affect older persons, and as the Italian population has aged, the proportion of corneal grafts for these diseases has increased in recent years. The growing demand for interventions for corneal endothelial diseases paralleled the widespread adoption of EK procedures, which offer faster visual recovery, more predictable refractive results, and easier postoperative management than PK. These advantages have probably increased patients' and surgeons' propensity for surgery. Surgeons may also consider surgery earlier, since EK procedures must be performed before corneal scarring occurs. These findings are in agreement with observations by Shtein et al[22]. These authors reported that in the United States of America, where EK procedures have been widely adopted, the odds of undergoing corneal graft have increased for patients with corneal endothelial diseases. Analyzing a large cohort of patients, they found a 47% increase in 2007-2009 versus 2001-2006.
Comparing the two periods, the proportion of interventions for graft failure also significantly increased (from 16.4% to 19.1%). Graft failure is one of the main indications in tertiary centers and those with specialized in corneal grafting: failure of prior corneal grafts leads to repeat grafting. Another factor that may have contributed to the increased graft failure rate is the recent adoption of new lamellar procedures. The survival of lamellar grafts was worse than the survival of penetrating grafts in the study of Coster et al[18]. Croasdale et al[16] reported that the graft replacement rate was very high when surgeons started adopting EK procedures. In northwestern Italy, the corneal surgeons started using the lamellar techniques during the study period, and the learning curve might have contributed to increasing the failure rate.
The increasing demand for interventions for corneal endothelial diseases and graft failure reduced the proportion of intervention for keratoconus in 2007-2011; however, the number of interventions was similar in the two periods: 513 in 2002-2006, and 542 in 2007-2011. The prevalence of keratoconus[23]–[26], is high in the Mediterranean area, and it remains the leading indication for corneal graft. In recent years, new techniques, such as intracorneal ring segment implantation and riboflavin/ultraviolet-A-induced collagen cross-linking[4]–[5], have emerged to treat keratoconus. These techniques have been widely adopted also in our country. Nowadays they have not reduced the number of corneal grafts. Intracorneal ring segments cannot actually be considered an alternative to corneal grafting: in most cases they are implanted in eyes with mild or intermediate keratoconus, in which corneal grafts are not required. The efficacy of riboflavin/ultraviolet-A-induced collagen cross-linking in halting the progression of keratoconus has been widely reported[27]. However this technique was introduced in 2003[5]. Thus more time will be required to assess whether it will reduce the need for corneal grafts for this disease.
The surgical approach to corneal grafting changed significantly during the study period. The vast majority of interventions in 2001-2006 were PK (92.4%). The proportion of lamellar procedures increased markedly in 2007-2011, almost reaching that of PK (42.8% versus 57.2%). EK procedures were chiefly responsible for this advance in lamellar surgery: they rose from 1.2% in 2006 to 44% in 2011. The Descemet stripping automated EK technique was used in more than 95% of EK procedures, becoming the preferred technique for surgical treatment of corneal endothelial diseases. Early posterior lamellar techniques, such as deep lamellar EK, were technically very difficult[9]–[10], requiring donor and recipient corneas to be dissected manually. Using the Descemet stripping automated EK technique, the posterior lamella is easily dissected with a microkeratome. The optical quality of the donor-recipient interface is good, as is postoperative visual recovery. The high proportion of corneal tissues assigned for EK procedures is comparable to reports from North America[15]–[17]. The proportion of corneal tissues supplied by the Eye Bank Association of America for EK procedures was 44.9% in 2010 and 46.6% in 2011. In other European countries, EK procedures have been less widely adopted[19],[20]. In Western Scotland they were used for 9.1% of corneal grafts in 2006-2010[19]. This difference may be partially due to the lower proportion of interventions for endothelial diseases in those countries.
The proportion of DALK procedures also increased significantly in the later period. This technique has several advantages over PK[14]. It is a non-penetrating intervention, reduces post-operative endothelial cell loss, eliminates the risk of endothelial rejection, and requires shorter topical steroid treatment. However, it was adopted in a moderate proportion of cases: 12.6% of interventions in 2007-2011. This rate is comparable to that reported from other registries[17]–[18],[20]. It appears probable that corneal surgeons have been more cautious in adopting this technique, which is technically more demanding and takes longer than PK. If the posterior stroma is not completely removed, visual recovery can be delayed[28]. Moreover, some studies reported that the proportion of eyes with 10/10 postoperative Snellen best corrected distance visual acuity was lower than with PK[29]–[30]. However, most comparative studies have shown that DALK provides postoperative visual and refractive results comparable to those of PK[14]. The use of this technique may therefore be expected to increase in the coming years.
Several limitations need to be acknowledged. It cannot be excluded that errors in disease diagnosis might have occurred. Although surgeons provided indications for surgery, disease diagnosis was not confirmed by histopathological examination. The surgical reports do not include preoperative visual acuity, which would have been very useful to assess whether the introduction of lamellar surgical techniques has changed the threshold of surgery; further studies are required to clarify this point.
In conclusion, the trend in indications and surgical techniques adopted for corneal grafts changed during the study period. The number of corneal grafts for Fuchs endothelial dystrophy, ABK/PBK and graft failure increased significantly. The increasing demand for interventions for these paralleled the widespread adoption of EK procedures. The use of DALK techniques also increased, but more moderately than that observed for posterior lamellar procedures.
Acknowledgments
Conflicts of Interest: de Sanctis U, None; Alovisi C, None; Bauchiero L, None; Caramello G, None; Girotto G, None; Panico C, None; Vinai L, None; Genzano F, None; Amoroso A, None; Grignolo F, None.
REFERENCES
- 1.Dobbins KR, Price FW, Whitson WE. Trends in the indications for penetrating keratoplasty in the midwestern United States. Cornea. 2000;19(6):813–816. doi: 10.1097/00003226-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Kang PC, Klintworth GK, Kim T, Carlson AN, Adelman R, Stinnett S, Afshari NA. Trends in the indications for penetrating keratoplasty, 1980-2001. Cornea. 2005;24(7):801–803. doi: 10.1097/01.ico.0000157407.43699.22. [DOI] [PubMed] [Google Scholar]
- 3.Darlington JK, Adrean SD, Schwab IR. Trends of penetrating keratoplasty in the United States from 1980 to 2004. Ophthalmology. 2006;113(12):2171–2175. doi: 10.1016/j.ophtha.2006.06.034. [DOI] [PubMed] [Google Scholar]
- 4.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26(8):1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 5.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 6.Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012;379(9827):1749–1761. doi: 10.1016/S0140-6736(12)60437-1. [DOI] [PubMed] [Google Scholar]
- 7.Melles GR, Remeijer L, Geerards AJ, Beekhuis WH. A quick surgical technique for deep, anterior lamellar keratoplasty using visco-dissection. Cornea. 2000;19(4):427–432. doi: 10.1097/00003226-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Anwar M, Teichmann KD. Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea. 2002;21(4):374–383. doi: 10.1097/00003226-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Melles GR, Eggink FA, Lander F, Pels E, Rietveld FJ, Beekhuis WH, Binder PS. A surgical technique for posterior lamellar keratoplasty. Cornea. 1998;17(6):618–626. doi: 10.1097/00003226-199811000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty in the first United States patients: early clinical results. Cornea. 2001;20(3):239–243. doi: 10.1097/00003226-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Melles GR, Wijdh RH, Nieuwendaal CP. A technique to excise the descemets membrane from a recipient cornea (descemetorhexis) Cornea. 2004;23(3):286–288. doi: 10.1097/00003226-200404000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Gorovoy MS. Descemet stripping automated endothelial keratoplasty. Cornea. 2006;25(8):886–889. doi: 10.1097/01.ico.0000214224.90743.01. [DOI] [PubMed] [Google Scholar]
- 13.Melles GR, Ong TS, Ververs B, van der Wees J. Descemet membrane endothelial keratoplasty (DMEK) Cornea. 2006;25(8):987–990. doi: 10.1097/01.ico.0000248385.16896.34. [DOI] [PubMed] [Google Scholar]
- 14.Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(1):209–218. doi: 10.1016/j.ophtha.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Boimer C, Lee K, Sharpen L, Mashour RS, Slomovic AR. Evolving surgical techniques of and indications for corneal transplantation in Ontario from 2000 to 2009. Can J Ophthalmol. 2011;46(4):360–366. doi: 10.1016/j.jcjo.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 16.Croasdale CR, Barney E, Warner EJ. Eye bank tissue utilization between endothelial keratoplasty and penetrating keratoplasty. Cornea. 2013;32(3):280–284. doi: 10.1097/ICO.0b013e3182561305. [DOI] [PubMed] [Google Scholar]
- 17.Eye Bank Association of America Statistical report 2011. Available at http://www.restoresight.org/about-us/ebaa-materials-publications. Accessed June 6, 2013.
- 18.Coster DJ, Lowe MT, Keane MC, Williams KA, Australian Corneal Graft Registry Contributors A comparison of lamellar and penetrating keratoplasty outcomes: a registry study. Ophthalmology. 2014;121(5):979–987. doi: 10.1016/j.ophtha.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 19.Ting DS, Sau CY, Srinivasan S, Ramaesh K, Mantry S, Roberts F. Changing trends in keratoplasty in the West of Scotland: a 10-year review. Br J Ophthalmology. 2012;96(3):405–408. doi: 10.1136/bjophthalmol-2011-300244. [DOI] [PubMed] [Google Scholar]
- 20.Keenan TD, Carley F, Yeates D, Jones MN, Rushton S, Goldacre MJ, NHSBT Ocular Tissue Advisory Group and contributing ophthalmologists (OTAG Audit Study 8) Trends in corneal graft surgery in the UK. Br J Ophthalmol. 2011;95(4):468–472. doi: 10.1136/bjo.2010.182329. [DOI] [PubMed] [Google Scholar]
- 21.Lindquist TD, McNeill JI, Wilhelmus KR. Indications for keratoplasty. Cornea. 1994;13(2):105–107. doi: 10.1097/00003226-199403000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Shtein RM, Raoof-Daneshvar D, Lin HC, Sugar A, Mian SI, Nan B, Stein JD. Keratoplasty for corneal endothelial disease, 2001-2009. Ophthalmology. 2012;119(7):1303–1310. doi: 10.1016/j.ophtha.2012.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Legeais JM, Parc C, d'Hermies F, Pouliquen Y, Renard G. Nineteen years of penetrating keratoplasty in the Hotel-Dieu Hospital in Paris. Cornea. 2001;20(6):603–606. doi: 10.1097/00003226-200108000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Pahor D, Gracner B, Falez M, Gracner T. Changing indications for penetrating keratoplasty over a 20-year period, 1985-2004. Klin Monbl Augenheilkd. 2007;224(2):110–114. doi: 10.1055/s-2007-962962. [DOI] [PubMed] [Google Scholar]
- 25.Muraine M, Toubeau D, Gueudry J, Brasseur G. Impact of new lamellar techniques of keratoplasty on eye bank activity. Graefes Arch Clin Exp Ophthalmol. 2007;245(1):32–38. doi: 10.1007/s00417-006-0390-7. [DOI] [PubMed] [Google Scholar]
- 26.Siganos CS, Tsiklis NS, Miltsakakis DG, Georgiadis NS, Georgiadou IN, Kymionis GD, Pallikaris IG. Changing indications for penetrating keratoplasty in Greece, 1982-2006: a multicenter study. Cornea. 2010;29(4):372–374. doi: 10.1097/ICO.0b013e3181bd44a1. [DOI] [PubMed] [Google Scholar]
- 27.Suri K, Hammersmith KM, Nagra PK. Corneal collagen cross-linking: ectasia and beyond. Curr Opin Ophthalmol. 2012;23(4):280–287. doi: 10.1097/ICU.0b013e328354865e. [DOI] [PubMed] [Google Scholar]
- 28.Fontana L, Parente G, Tassinari G. Clinical outcomes after deep anterior lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2007;143(1):117–124. doi: 10.1016/j.ajo.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 29.Funnell CL, Ball J, Noble BA. Comparative cohort study of the outcomes of deep lamellar keratoplasty and penetrating keratoplasty for keratoconus. Eye (Lond) 2006;20(5):527–532. doi: 10.1038/sj.eye.6701903. [DOI] [PubMed] [Google Scholar]
- 30.Jones MN, Armitage WJ, Ayliffe W, Larkin DF, Kaye SB, NHSBT Ocular Tissue Advisory Group and Contributing Ophthalmologists (OTAG Audit Study 5) Penetrating and deep anterior lamellar keratoplasty for keratoconus: a comparison of graft outcomes in the United Kingdom. Invest Ophthalmol Vis Sci. 2009;50(12):5625–5629. doi: 10.1167/iovs.09-3994. [DOI] [PubMed] [Google Scholar]