Abstract
Workplace stress can influence healthcare professionals’ physical and emotional well-being by curbing their efficiency and having a negative impact on their overall quality of life. The aim of the present study was to investigate the impact that work environment in a local public general hospital can have on the health workers’ mental-emotional health and find strategies in order to cope with negative consequences. The study took place from July 2010 to October 2010. Our sample consisted of 200 healthcare professionals aged 21-58 years working in a 240-bed general hospital and the response rate was 91.36%). Our research protocol was first approved by the hospital’s review board. A standardized questionnaire that investigates strategies for coping with stressful conditions was used. A standardized questionnaire was used in the present study Coping Strategies for Stressful Events, evaluating the strategies that persons employ in order to overcome a stressful situation or event. The questionnaire was first tested for validity and reliability which were found satisfactory (Cronbach’s α=0.862). Strict anonymity of the participants was guaranteed. The SPSS 16.0 software was used for the statistical analysis. Regression analysis showed that health professionals’ emotional health can be influenced by strategies for dealing with stressful events, since positive re-assessment, quitting and seeking social support are predisposing factors regarding the three first quality of life factors of the World Health Organization Quality of Life - BREF. More specifically, for the physical health factor, positive re-assessment (t=3.370, P=0.001) and quitting (t=−2.564, P=0.011) are predisposing factors. For the ‘mental health and spirituality’ regression model, positive re-assessment (t=5.528, P=0.000) and seeking social support (t=−1.991, P=0.048) are also predisposing factors, while regarding social relationships positive re-assessment (t=4.289, P=0.000) is a predisposing factor. According to our findings, there was a notable lack of workplace stress management strategies, which the participants usually perceive as a lack of interest on behalf of the management regarding their emotional state. Some significant factors for lowering workplace stress were found to be the need to encourage and morally reward the staff and also to provide them with opportunities for further or continuous education.
Key words: Coping strategies, stressful conditions, healthcare professionals, doctors and nurses, work environment
Introduction
In an era of intense industrialization, rapid technological advent and globalization, employees are expected to work more intensely and successfully deliver more. Being exposed to stress for too long, may lower a person’s efficiency and could trigger negative consequences on one’s health or family and social life. Nevertheless, not every manifestation of stress is always workplace stress. Workplace stress may be caused by various factors. Some professions are inherently more stressful than others. Professions that involve human contact and rapid decision-making skills, while those decisions can have a serious (financial, social or other) impact, are among the most stressful ones.1
Healthcare professions are among the first six most stressful ones.1 Not all health professionals develop the same level of stress, and not all of them develop signs of professional burn-out either. According to several studies, Intensive Care Unit medical/nursing staff report that dealing with death is their first source of stress, compared to nurses who work in Internal Medicine or Surgical Departments. For those professionals, workload and adequate manning is their most important stress source.2 According to other studies, surgical nurses assess the emotional aspect as less important compared to their colleagues in oncology and hematology departments.3 In general, healthcare professionals are more prone to stress and professional burn-out, because they are responsible for human lives and their actions – or lack of action – can have a serious impact on their patients.4
Nevertheless, since stress is a complicated phenomenon, we can never be too confident and decisive regarding stress sources; on the contrary we should take into account what each person individually perceives as a stressful factor. Some factors that may play a role regarding workplace-related emotional disorders and could have a negative impact on the health professionals’ emotional health are the following: i) the stressful nature of the profession. Work-related stress in combination with psychological quests, ethical dilemmas and the patients’ demands can be a burden on the professional’s emotional state.5,6 ii) Workplace anxiety and tensions could lead to lower quality of care, which in its turn could lower professional satisfaction and consequently their quality of life.7 iii) Continuous interaction with the patients and their families/friends can foster emotions of anger, embarrassment, fear, and desperation, especially when there are no solutions to the patients’ problems, thus leading health professionals to a more complicated, frustrating situation.6,7 iv) Lack of support from colleagues and higher rank staff, conflicts among members of the therapeutic team, vague roles, different hierarchy ranks, lack of an organizational structure and administration-related factors have their share regarding psychiatric morbidity.7,8 v) Some causal factors for psychiatric morbidity include individual characteristics, such as personality, personal experiences, emotional maturity, personal style, as well as demographics such as age, sex, socio-economical status, years of employment and family status. 8,9
All of the above factors, as well as a professional’s ability to be actively involved in work-related decisions, may influence the intensity of the symptoms and the consequences psychiatric morbidity may have on a person’s life.7 Stress sources act accumulatively on a person leading to physical, psychological and behavioral reactions, or even to psychosomatic disease.10 A study that took place in the United Kingdom, Sweden, Germany, Japan, Singapore, USA, Nigeria, South Africa, Brazil and Egypt showed that time pressure, deadlines, poor working conditions, excessive workload, prolonged working hours, conflict between different beliefs, interpersonal relationships and maladministration, are among the top workplace stress factors.10 Stress has consequences on both persons and their workplace. Regarding the individuals concerned, stress may lead to poor mental health as well as alcohol abuse, heavier smoking habits and pharmaceutical substance abuse.11
The effects of stress on the staff fall within the following categories. i) Subjective experiences (stress, depression, anxiety, emotional withdrawal, gradual loss of empathy towards the patients).8,9,12 ii) Physical consequences (the whole range of psychosomatic conditions, short-duration migraines, skin rashes, irritable bowel syndrome, cardiovascular diseases and strokes).9,12,13 iii) Behavioral changes (irritability, alcoholism, addictive behaviors).11,14 Stress can compromise a professional’s ability to provide high quality care to his/her patients, since it can promote professional burn-out and recurring depressive episodes. Finally, work-related stress can have an impact on the professional’s family by decreasing their overall quality of life.15
Psychological risk factors differ from other kinds of risk factors in that, under different circumstances, they may even have positive effects, and are not easily evaluated, since individuals differ significantly regarding how sensitive they may be to different stressors, how they perceive them and how they react to them.16 Cognitive evaluation plays an important role between the stressful event and a person’s reaction to it.17 And this happens because a person’s thoughts about what a given situation demands from him/her and if s/he is able to cope with those demands, play also an important role.18-20
The perception of stress depends on a cognitive evaluation process, which makes a person evaluates the significance of the events and also his/her potential to deal with them.20,21 The evaluation process for a potentially stressful stimulus includes two phases.18
During the primary evaluation phase, a person determines if the event is important to him/her, and if it can have threatening consequences. In the secondary evaluation phase, the individual determines if his/her capabilities and psychological reserves are enough for him/her to deal with the stressful event.18,20 According to Lazarus & Folkman, there are eight kinds of coping strategies that people use in order to manage stress.18 Those strategies tend to be problem-centered or emotion-centered. Proper stress management is related to good quality of life and good health, while poor management leads to poor quality of life and disease.
According to a Greek study about coping strategies and professional satisfaction of doctors, it was found that they prefer coping strategies oriented towards direct problem management, through a positive approach, reassessment and ultimately solution. More specifically, female doctors prefer emotion-centered coping strategies (wishful thinking/reverie, seeking help from God), while male doctors usually prefer solving the problem. Older doctors use more often positive approaches.22 According to studies that involved nurses working in hospitals in Australia and New Zealand, nurses use problem-centered coping strategies that tend to be linked to better mental health regarding stress management at work.23-26 This has to do with the Western cultures, because some studies that took place in hospitals from Japan, Thailand and Korea, found that nurses used emotion-centered strategies, also linked to good mental health.27-29
The aim of the present study was to investigate how the working environment of a general hospital can affect health professionals’ emotional health and coping strategies.
Materials and Methods
Study sample
In order to include all relevant specialties and professional groups, stratified random sampling was used for the selection of the participants. Our sample consisted of 200 professionals working in a 240-bed local hospital, aged 21-58 years; 29% of them were males and 71% females. 220 questionnaires were handed out and 200 were returned (response rate: 91.36%).
The sample included physicians, nurses of higher and university education level, assistant nurses, other health professionals and also medical/nursing students who have everyday contacts with the patients. All hospital departments and units were included (internal medicine and surgical departments, dialysis unit, intensive care unit). Employees who were on sick leave during the study were excluded. Our research protocol was granted approval by the hospital’s Review Board. Department chief doctors and nurses were then informed about the study and the questionnaires were distributed. All participants were given written instructions and everyone signed a written informed consent form. The present study was under the supervision of the Medical School of the University of Athens for the completion of a Master’s degree thesis, it took place from July 2010 to (and including) October 2010, and is best described as a descriptive correlational study.
Study instrument
A standardized questionnaire was used in the present study. This instrument Coping Strategies for Stressful Events (CSSE), evaluates the strategies that persons employ in order to overcome a stressful situation or event. It also focuses on a person’s (cognitive and behavioral) attempts to manage (lower, minimize, overcome or simply endure) the internal and external demands imposed by their interaction with their environment, and especially those demands that could compromise or be too much for a person’s abilities. The instrument also investigates a person’s interaction with their environment aiming at physical and mental health. The purpose of the questionnaire is to examine coping strategies employed by individuals when dealing with stressful events. It is the Greek standardized version of Lazarus & Folkman’s Ways of Coping, after the Authors’ permission.30
Factor analysis for the Greek population unveiled five reliable major factors with separate dimension within factors 1, 3 and 4. Basically, CSSEs are divided in two major groups. Problem-centered strategies (solving the problem, seeking social support, active hands-on approaches towards the problem) and emotion-centered ones (positive reassessment, wishful thinking/reverie with its 2 dimensions, avoidance/escaping with its 2 dimensions). Positive approach with 2 dimensions includes positive reassessment and problem solving, which also includes a person’s attempt to reassess stressful events in a positive way and at the same time plan specific techniques to solve the problem.
Seeking social support includes a person’s attempts to find proper support from his/her social environment in order to deal with his/her problems.
Wishful thinking/reverie with its 2 dimensions, also includes wishful thinking and seeking help from God. This particular factor focuses on a person’s tendency to wish for a miracle to happen, or thinking how things would had gone if something negative had not happen.
Avoidance/escaping with its 2 dimensions includes quitting and denying. This factor evaluates an individual’s tendency to re-assess a situation by devaluating it or by ignoring its true significance. Finally, the hands-on problem solving, is a factor that evaluates a person’s attempt to reach a solution by dealing actively and directly with the situation or the person behind the situation. As far as data analysis was concerned, a factor analysis in oblique rotation was used for each factor separately (factors within a factor).23 For the needs of this study, another questionnaire for the participants’ demographics was created. It included sex, age, family status, educational level, place of residence, specialty and years of employment in the hospital.
Validity and reliability of the instrument
Internal cohesion validity was tested by Cronbach’s α and Standardized Item α. Internal cohesion validity for all the scale items was α=0.862, and Standardized Item α=0.866. Internal cohesion coefficients were satisfactory for almost all of the questionnaire variables. Most coefficient values range from 0.60 to 877, which demonstrates a satisfactory internal cohesion validity, except from the scale of denial (α=0.458) and hands-on problem solving (αα=0.429) that have a moderate internal cohesion validity.
Study limitations
The present study was focused on the effects that workplace may have on the emotional health of the medical-nursing staff of a local hospital and coping strategies employed for stressful situations. Health workers that during the course of the study were absent, or on sick leave or on vacation, were excluded. The study has the following limitations.
The sample consisted from healthcare professionals working in one local hospital, thus the sample is small and cannot be thought to be representative for the whole country. Also, it cannot be certain if the participants answered in full honesty all the questionnaire items, although clear instructions had been provided to the participants before and during the questionnaire completion. Also the participants completed themselves the questionnaires, in order to feel more free and honest.
Statistical analysis
After the data were coded, a preliminary test took place in order to see if the data could be used for parametric statistical analysis. Explore and Frequencies processes showed equal variations among compare groups and that normal distribution applied. Since it was established that the sample was indeed random and continuous depended variables were defined, parametric tests took place in order for the mean values. T-Test Groups was used to test hypotheses on two different groups and also One-Way Anova. Null hypotheses were tested by linear regression with quality of life as the dependent variable, while psychiatric morbidity was the explanatory variable, and also demographics that had been tested with Pearson’s r and had been shown to be significantly correlated to quality of life. The SPSS v.16 software was used fordata analysis.
Results
Our sample consisted of 200 persons (58 males, 142 females), and 59.7% were nurses of three different levels, 30.3% were doctors, 9.5% had had other health professions, and 0.5% were students (P=0.001). Regarding education level, 36.8% were higher education graduates, 24.4% had post-high school vocational training, 24.4% were university graduates, 10% had a Master’s degree (P=0.001).
The mean values were the following: positive approach (mean=32.6±5.7), seeking social support (mean=18.1±2.9), wishful thinking/reverie (mean=22.9±4.5), avoidance/escape (mean=26.2±3.8), hands-on problem solving (mean=10.9±2.1).
Female participants scored higher in the following scales: wishful thinking/reverie (P=0.000), wishful thinking (P=0.003) and seeking help from God (P=0.002), scoring higher than male participants with a significant variation (Table 1). It seems that females have a tendency to employ strategies pertaining to wishful thinking and seeking God’s help more than males. Mean values of the wishful thinking/reverie scale in females compared to males (M=23.6 SD=4.4 vs M=21.2 SD=4.3), showed a statistically significant variation (t=-3.649, df=198, P<0.05). The mean values of the subscale wishful thinking compared to male participants (=14.9, DS=3.1 vs M=13.5, DS=2.9), also showed a significant variation (t=-3.033 df=198 P=0.003). Finally regarding seeking God’s help the values among the two genders (M=8.7 SD=2.1 vs M=7.6 SD=2.1), also showed a significant variation (t=-3.210 df=198 P=0.002).
Table 1.
T-test for men and women according to the Greek edition of the Coping Strategies for Stressful Events questionnaire.
| Variables | Men (n=58) | Women (n=142) | Difference | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | Test | P | |
| Positive approach | 31.9 | 6.5 | 32.9 | 5.4 | -0.976 | 0.332 |
| Positive reassessment | 20.6 | 4.1 | 21.5 | 3.5 | -1,577 | 0.116 |
| Problem solving | 11.3 | 2.7 | 11.4 | 2.4 | -0.126 | 0.900 |
| Quest for social support | 17.9 | 2.8 | 18.2 | 2.9 | -0.690 | 0.491 |
| Wishful thinking-reverie | 21.2 | 4.3 | 23.6 | 4.4 | -3.649 | 0.000 |
| Wishful thinking | 13.5 | 2.9 | 14.9 | 3.1 | -3.033 | 0.003 |
| Search divine help | 7.6 | 2.1 | 8.7 | 2.1 | -3.210 | 0.002 |
| Avoidance/escape | 26.4 | 3.7 | 26.1 | 3.9 | 0.383 | 0.702 |
| Resignation | 15.1 | 2.7 | 14.8 | 2.6 | 0.838 | 0.403 |
| Refusal | 11.2 | 2.1 | 11.4 | 2.1 | -0.365 | 0.715 |
| Assertiveness problem solving | 11.2 | 1.7 | 10.8 | 2.2 | 1.294 | 0.197 |
M, mean; SD, standard deviation; test=on parametric Mann Whitney. P, P-value (bilateral). Italics the statistically significant results.
The existence of a health problem also seems to play a role. It was found that the participants had a tendency to report that they had had no health problems, which is related to a positive approach to life, and both relevant subscales had high scores =-3.746 P=0.001), as well as denial (t=-2.525, P=0.12) (Table 2). It was also found that health professionals who use strategies related to problem solving (t=-3.793 P=0.000) and positive re-assessment (t=-3.313 P=0.001), do not report any health problems and their emotional state seems to be better than those who employ other coping strategies. Family status seems to influence positive approach and its sub-factors. Single and married people use a positive approach more often than divorced individuals and widowed ones (P=0.003), (P=0.036), (P=0.039) (Table 3). This finding confirms that divorced and widowed individuals, because of their family status, tend not to use the above-mentioned strategies. Also years of employment seem to account for significant variations. Individuals who worked for 20-30 years scored higher than workers with less years of employment in Wishful thinking/reverie (P=0.013), and wishful thinking (P<0.025). Those who had been working for 10-20 years scored higher than their newer colleagues in the hands-on problem solving scale (P<0.01) (Table 4). It seems that newer workers do not usually try to solve problems actively, perhaps because of short-term contracts, or their professional roles (resident doctor, novice nurse, etc). Regarding health status, it was found that if the professionals enjoyed good health status, they also tended to use positive approach strategies (positive re-assessment and problem solving) (P=0.0001) (Figure 1).
Table 2.
T-test regarding health related problems according to the questionnaire of the Coping Strategies for Stressful Events.
| Variables | Existing health problem (n=65) | No health problems (n=136) | Difference | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | Test | P | |
| Positive approach | 30.2 | 6.8 | 33.7 | 4.8 | -3.7463# | 0.000 |
| Positive reassessment | 19.9 | 4.3 | 21.9 | 3.1 | -3.313# | 0.001 |
| Problem solving | 10.4 | 2.98 | 11.9 | 2.2 | -3.793# | 0.000 |
| Quest for social support | 17.9 | 2.9 | 18.2 | 2.9 | -0.779 | 437 |
| Wishful thinking-reverie | 22.8 | 4.6 | 22.9 | 4.5 | -0.319 | 0.750 |
| Wishful thinking | 14.2 | 3.2 | 14.7 | 3.1 | -1.060 | 0.291 |
| Search divine help | 8.6 | 2.2 | 8.3 | 2.1 | 0.854 | 403 |
| Avoidance/escape | 26.1 | 3.9 | 26.2 | 3.8 | -0.195 | 0.846 |
| Resignation | 15.3 | 2.7 | 14.7 | 2.6 | 1.669 | 0.097 |
| Refusal | 10.8 | 1.9 | 11.6 | 2.1 | -2.525 | 012 |
| Assertiveness problem solving | 10.6 | 2.2 | 11.0 | 1.9 | -1.269 | 0.206 |
M, mean; SD, standard deviation; test, non parametric Mann Whitney if indicated by #, otherwise t-test. P, P-value (bilateral).
Table 3.
Bonferroni criterion for statistically significant differences regarding family status and questionnaire scales.
| Variables | Single | Separated | Widowed | Married | Divorced | Average difference (single-married) | P |
|---|---|---|---|---|---|---|---|
| Positive approach | 34.1±4.9a | 32.4±8.01a,b | 27.8±4.9 | 32.9±5.7b | 29.5±5.9 | a=4.603* b= 3.394* |
0.003 0.036 |
| Positive reassessment | 22.01±3.2a | 20.8±5.5a,b | 18±2.9 | 21.4±3.6b | 19.5±3.9# | b=2.48391* -2.48391* |
0.023 0.023 |
| Problem solving | 12.1±2.2a | 11.6±3.5a,b,c | 9.8±2.5c | 11.5±2.6b | 9.9±2.2 | a=2.11954* b=1.48526* c=3.95000* |
0.001 0.035 0.039 |
*The mean difference is significant at the 0.05 level.
#The mean difference is significant at the 0.05 level.
a,b,cMarkers for couples reviling significant differences.
Table 4.
Bonferroni criterion for the years of working for the Coping Strategies for Stressful Events questionnaire.
| Dependent variable | Years of service (I) | Years of service (J) | Average difference (I-J) | P |
|---|---|---|---|---|
| Wishful thinking-reverie | 1 | 3 | -2.55826* | 0.009 |
| Wishful thinking | 1 | 3 | -1.60270* | 0.022 |
| Assertiveness problem solving | 1 | 2 | -0.95521* | 0.008 |
*The mean difference is significant at the 0.05 level. 1=1-10 years, 2=10-20 years, 3=20-30 years.
Figure 1.
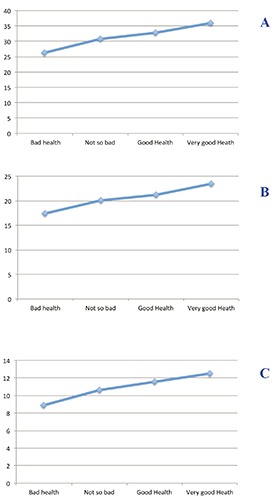
Self-reported health status regarding signs of positive approach (A); positive reassessment (B); and problem solving (C).
Discussion
The present study attempted to assess the effects of wok environment on the health workers’ emotional state in a local general hospital. The CSSE questionnaire was used in order to examine coping strategies employed by those healthcare professionals. Our participants’ scores were found to be similar to those of the general, normal, population.30
The participants’ response was quite satisfactory since 91.36% completed and returned the questionnaires. This response rate is similar to those from other Greek and international studies which typically range from 72 to 80%.31,32 This high participation rate reflects health workers’ interest in expressing themselves about issues of concern. Regarding demographics, gender seems to influence the wishful thinking scale, since female participants scored higher. Females also scored higher in the seeking God’s help subscale. Also, females scored higher in the physical health scale, independence levels and quality of life compared to males (t=-2.155 P<0.05). This finding is in agreement with a previous Greek study,22 which included doctors working in a public hospital. In this study it was found that female doctors employ emotion-centered CSSEs, such as wishful thinking, seeking help from God, while male doctors employ more often problem solving and positive approach. On the other hand, relevant studies that included nurses working in hospitals in Australia and New Zealand regarding stress and coping with it, showed that female nurses used problem-centered coping strategies for dealing with stress in the workplace.23-26
The existence of a health problem also seemed to play a role. Participants who did not report health issues scored higher in positive approach and its subscales, but also in denial too. This finding is in agreement with a Finnish study which showed that healthcare professionals prefer self-treatment (80-84% of male participants, 72-74% of females) for both physical and mental conditions.33 Education, kind of employment and professional category (nursing, medical, other) did not have an effect on the questionnaire subscales.
On the other hand, family status (single, married, widowed, divorced, separated) seemed to have an effect on positive approach and its sub-factors, positive re-assessment and problem solving. Single and married individuals use more often strategies pertaining to problem solving, positive approach and reassessment, compared to divorced and widowed individuals. This finding is in agreement with a study by Cooper et al.,10 where it was found that physical and mental well-being is not affected by work environment alone, but also by individual attitudes and family problems Years of employment also seemed to affect the participants’ answers, since they had significant differences regarding the factors wishful thinking/reverie, wishful thinking and hands-on problem solving. More specifically, those who had been employed for 20-30 years reported using the above mentioned strategies more often than newer professionals who had been working for 1-10 years, who used more often the positive approach strategy. Also, those who had been working for 10-20 years resort more often to hands-on problem solving than newer health workers with 1-10 years of employment. Regarding quality of life, newer healthy workers scored higher in all sub-scales compared to those who had been working for 10-30 years. Newer health workers develop healthier social relationships and enjoy better mental and physical health compared to those who had been working for more than 10 years.
The way participants perceive their health status through a single question, seemed to have an effect on the mean values of positive approach, positive re-assessment and problem solving scales of the questionnaire. More specifically, when health workers deal their health status by using the above mentioned strategies, they have less stress symptoms and better quality of life.
Correlation tests (Pearson’s r) showed that when positive approach, re-assessment, problem solving and seeking for social support are being used more often, symptoms of stress, depression or physical illness diminish; on the contrary, when quitting is employed more often, these symptoms usually increase. And when denial is the strategy more often chosen, the symptoms decrease again. Similar findings were found in a study by Lazarus & Folkman, who concluded that when individuals employ inefficient CSSEs and fail to address the source of the problem, even more stress emerges, which results in a state of inability that includes chronic stress and depressive symptoms and fatigue.34
Finally, a major finding of the present study was that stressful situations are the most significant risk factor for healthcare professionals’ mental/emotional health, something that is in agreement with other studies that have concluded that working conditions of health workers should be improved and have highlighted that a stressful and often hazardous work environment plays a critical role in their decision to stay at their job or leave it.35,36 A Greek study by Datsis et al., has also reached a similar conclusion.37 That study investigated health workers perceptions about their job and work environment and found that a high proportion of the participants would consider leaving their job due to excessive stress.
Conclusions
The participants’ mental-emotional health is affected by their work environment, as well as the coping strategies they employ, since positive re-assessment, quitting and seeking social support are factors that could affect their physical, mental and social well-being. Gender can also be a significant factor, since females seemed to enjoy better physical health compared to males. Coping Strategies for Stressful Events play a central role in the interaction between individuals and their environment. Consequently, their effect on physical and psychosocial health is significant. Based on our findings, the following measures are proposed: mental health promotion interventions, focused on medical-nursing staff who work in clinical, high-intensity settings. Health workers could be trained to employ relaxation techniques and stress management strategies. Creation and development of psychological support and counseling programs. Active support of the medical and – mainly – nursing staff on behalf of the Hospital’s managers. Wider participation of (new) doctors and nurses in the creation of health policies and the decision-making processes.
References
- 1.Cooper CL, Cooper RD, Eaker LH. Living with stress. Harmonsworth: Pengium; 1988. [Google Scholar]
- 2.Foxall M, Zimmerman L, Standley R, Bene C. A comparison of frequency and sources of nursing job stress perceived by intensive care, hospice and medical-surgical nurses. J Adv Nurs 1990;15:577-84. [DOI] [PubMed] [Google Scholar]
- 3.Tyler PA, Ellison RN. Sources of stress and psychological well-being in high-dependency nursing. J Adv Nurs 1994;19:469-76. [DOI] [PubMed] [Google Scholar]
- 4.Sapountzi D, Lemonidou C. Nursing in Greece. Developments and prospects. Athens: Academy of Health Professions; 1994. [Google Scholar]
- 5.Bakker AB, Killmer CH, Siegriest J, Schaufeli Effort-reward imbalance and burnout among nurses. J Adv Nurs 2000;31:884-91. [DOI] [PubMed] [Google Scholar]
- 6.Arnold J, Cooper C, Robertson IT. Work psychology: understanding human behavior in the work place. 2nd ed. London: Pitman; 1995. [Google Scholar]
- 7.Boumans N, Landeweerd J. A Dutch study of effects of primary nursing on job characteristics and organizational processes. J Adv Nurs 1996;24:16-23. [DOI] [PubMed] [Google Scholar]
- 8.de Boer J, Lok A, Van't Verlaat E, et al. Work-related critical incidents in hospital-based health care providers and the risk of post-traumatic stress symptoms, anxiety, and depression: a meta-analysis. Soc Sci Med 2011;73:2:316-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mészáros V, Cserháti Z, Oláh A, et al. Coping with work-related stress in health care professionals: strategies for the prevention of burnout and depression. Orv Hetil 2013;24;154:449-54. [DOI] [PubMed] [Google Scholar]
- 10.Cooper C, Cooper R, Eaker L. Living with stress. Athens: Scientific Publication Parisianou SA; 2002. [Google Scholar]
- 11.Fagin L, Bartlett H. The Claybury CPN stress survey: background and methodology. Carson J, Fagin L, Ritter S, eds. Stress and coping mental health nursing. London: Chapman and Hall; 1995. [Google Scholar]
- 12.McGarry S, Girdler S, McDonald A, et al. Paediatric health-care professionals: relationships between psychological distress, resilience and coping skills. J Paediatr Child Health 2013;49:725-32. [DOI] [PubMed] [Google Scholar]
- 13.Hillert A. How is burnout treated? Treatment approaches between wellness, job-related prevention of stress, psychotherapy, and social criticism. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2012;55:190-6. [DOI] [PubMed] [Google Scholar]
- 14.Coffey M. Stress and burn out in forensic community mental health nurses: an investigations of its causes and effects. J Psychiatr Mental Health Nurs 1999;6:433-43. [DOI] [PubMed] [Google Scholar]
- 15.Dawkins J, Depp F, Seltzer N. Stress and psychiatric nurse. J Psychosoc Nurs 1985;23:11:9-15. [DOI] [PubMed] [Google Scholar]
- 16.Cox T, Griffiths A, Barlowe C, et al. Organizational interventions for work stress: a risk management approach. HSE Contract Research Report 286/2000. Sudbury: HSE Book; 2000. [Google Scholar]
- 17.Asimakopoulos M. The burnout job satisfaction and engagement at work in the public sector. PhD thesis. University of Patras, Department of Business Administration, Patras, 2004. [Google Scholar]
- 18.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- 19.Bandura A. Self-efficacy: the exercise of control, New York: Freeman & Co. 1997. [Google Scholar]
- 20.Lazarus RS. Fifty years of the research and the theory of R.S. Lazarus: an analysis of historical and perennial issues, Mahwah: Eribaum; 1999. [Google Scholar]
- 21.Cohen F, Lazarus R. Coping with stress and illness. In Stone GC, Cohenm F, Adler N, eds. Health psychology: a handbook. San Fransisco: Jossey-Bass; 1979. pp 140-68. [Google Scholar]
- 22.Kaleas M, Platsidou M. Strategies to address stressful situations and job satisfaction of Greek in Public hospitals. Modern Soc Educ Mental Health 2008;1:177-200. [Google Scholar]
- 23.Chang E, Bidewell J, Huntington A, et al. A survey of role stress, coping and health in Australian and New Zealand hospital nurses. Int J Nurs Stud 2007;44:1354-62. [DOI] [PubMed] [Google Scholar]
- 24.Happell B, Reid-Searl K, Dwyer T, et al. How nurses cope with occupational stress outside their workplaces. Collegian 2013;20:3:195-9. [DOI] [PubMed] [Google Scholar]
- 25.Happell B, Dwyer T, Reid-Searl K, et al. Nurses and stress: recognizing causes and seeking solutions. J Nurs Manag 2013;21:4:638-47. [DOI] [PubMed] [Google Scholar]
- 26.Lim J, Bogossian F, Ahern K. Stress and coping in Australian nurses: a systematic review. Int Nurs Rev 2010;57:1:22-31. [DOI] [PubMed] [Google Scholar]
- 27.Lambert V, Lambert C, Ito M. Workplace stressors, ways of coping and demographic characteristics as predictors of physical and mental health of Japanese hospital nurses. Int J Nurs Stud 2004;41:85-97. [DOI] [PubMed] [Google Scholar]
- 28.Lambert V, C Lambert, Itano Jet al. Cross-cultural comparison of workplace stressors, ways of coping and demographic characteristics as predictors of physical and mental health among hospital nurses in Japan, Thailand, South Korea and the USA(Hawaii). Int J Nurs Stud 2004;41:671-84. [DOI] [PubMed] [Google Scholar]
- 29.Lambert V, Lambert C, Petrini M, et al. Workplace and personal factors associated with physical an mental health in hospital nurses in China, Nurs Health Sci 2007;9:120-6. [DOI] [PubMed] [Google Scholar]
- 30.Karadimas EH. Adapting to a Greek scale measuring coping strategies, stressful situations, Psychology 1998;5:3:260-73. [Google Scholar]
- 31.Laskari C, Kotsonis K, Velentzas P, et al. Anxiety, stress, depression, and job satisfaction of workers in the field of health services. Pediatrics 2000;63:225-30. [Google Scholar]
- 32.Coomber S, Todd C, Park G, et al. Stress in UK intensive care doctors. Br J Anaesth 2002;89:873-81. [DOI] [PubMed] [Google Scholar]
- 33.Toyry S, Rasanen K, Kujala S, et al. Self-reported health, illness, and self-care among Finnish physicians. Arch Fam Med 2000;9:1079-85. [DOI] [PubMed] [Google Scholar]
- 34.Lazarus RS, Folkman S. Coping and adaptation. Gentry WD, ed. Handbook of behavioral medicine. New York: The Guilford Press; 1984. pp 282-325. [Google Scholar]
- 35.McGills Hall L. Quality work environments for nurse and patient safety. Toronto: Jones & Batlett Publishers; 2005. [Google Scholar]
- 36.International Council of Nurses. Positive practice environments: quality workplace-quality patient care. Geneva: ICN, 2007. [Google Scholar]
- 37.Datsis A, Tragouda E, et al. The opinion of health professionals for their work and the work environment. Nursing 2007;46:2:268-81. [Google Scholar]


