Abstract
Coping behavior is of critical importance in diabetes because of its impact upon self-care and hence eventual medical outcome. We examined how coping behavior and its relationship to personality, diabetes health threat communication (DHTC) and illness representations changes after diagnosis of diabetes. Newly diagnosed diabetic patients were assessed after diagnosis and at 6, 12 and 24 months using the DHTC, Illness Perceptions and Coping inventory questionnaires. Personality traits were assessed at baseline. Active coping, planning, positive reinterpretation and growth (PRG), seeking emotional and instrumental (social) support decreased over the 2 years from diagnosis while passive acceptance increased. Openness/intellect and conscientiousness traits were associated with active coping and seeking instrumental support. Openness/intellect also associated with planning and PRG. These relationships did not vary over time. Perceived threat and serious consequences were associated with active coping but the effect diminished over time. Illness coherence (understanding of diabetes), personal and treatment control were associated with active coping, planning and seeking instrumental support and did not change over time. The coping strategies most commonly employed by diabetic patients are adaptive. Coping behavior changes over the 2 years from diagnosis. Promoting better understanding of diabetes, perceptions of personal control and treatment effectiveness are more likely than perception of health threat to sustain adaptive problem focused coping behavior.
Key words: diabetes, illness cognitions, patient education, psychosocial
Introduction
Diabetes often has few symptoms yet most patients have some, if limited, awareness of the potential for serious complications in the long term. Thus, despite the lack of overt effect on physical health diabetes often has substantial psychological impact to which individuals must adjust.1 The term coping behaviors refers to responses the individual makes to their diagnosis. Leventhal’s Self Regulatory Model or Common Sense Model (CSM) postulates coping behaviors are determined by the individual’s illness representations (IRs, Personal Models) meaning their beliefs about their diabetes, which in turn are determined by a variety of fixed traits (personality) and external influences (social, educational).2 Coping behavior will change with reappraisal.3 The consequent coping strategies may be classified broadly as active versus passive or problem focused versus emotion focused (meaning dealing with the emotion rather than the objective medical condition). The effectiveness of one strategy over another depends on the stressor. For better self-management of diabetes active problem focused coping, where the issue is directly addressed such as by seeking professional help, is more likely to be successful than emotion focused by the expression of anger, use of alcohol, illicit drugs or denial. Control of emotional symptoms may be important but active problem focused coping is associated with less psychological distress as well as better medical outcome.4
Studies of patients with chronic pain, spinal cord injury and irritable bowel syndrome suggest that coping behaviors change little over periods of six months to two years,5-8 but little is known about the coping strategies of newly diagnosed diabetes patients and how initial coping alters over time. IRs have been shown to change after the diagnosis of diabetes with increasing illness coherence and reducing emotional response.9,10 Thus, it is important to understand what changes in coping behavior occur following this and the relationship to factors which influence IRs (demographic factors, personality and perceived health threat). Personality and social and environmental factors may not change but their relationship to coping behavior may alter over time. Also, very differing emotional responses occur.11 These can dominate behavior adversely as shown in qualitative work.12 Emotional responses are associated principally with perception of health threat.13 We therefore developed the DHTC to measure this parameter.14 The period immediately after diagnosis is likely to be the time of maximum psychological impact. Perceived threat (measured by DHTC questionnaire) at diagnosis remains a major influence on emotional responses measured 2 years afterwards.10 The CSM predicts that this effect on IRs would translate into altered coping behavior. This is also the time when patients generally receive formal diabetes education. The manner in which this is provided will influence the development of health beliefs (IRs) and hence coping behaviors in the initial years and is therefore potentially critical.
Specific aims
The specific aims are: i) to characterize changes in coping behavior over two years from the diagnosis of diabetes; ii) to assess the relationship of social and environmental factors, personality, perceived health threat and illness representations to the changes in coping over this period.
This analysis may suggest interventions to achieve more adaptive coping behavior.
Materials and Methods
Patients and questionnaires
Ethical approval was obtained. Precepts of the Declaration of Helsinki were followed. Patients newly diagnosed with diabetes were recruited over 15 months from hospital clinics (26% of those completing the study) at 3 centers and by practice nurses in primary care (74%). All subjects had their baseline interview within 3 months of diagnosis of diabetes. Follow up visits were at 6, 12 and 24 months from baseline, all conducted by the same researcher (VL). Inclusion criteria were type 1 or type 2 diabetes, age 18-65 years with no comorbid conditions or major diabetic complications that might influence patients’ health beliefs. Of 197 contacted, 158 were interviewed at baseline and 138 (mean age 49y, range 19-65) completed the study: 84 male and 54 female, 29 with type 1 diabetes and 109 type 2. Treatment of diabetes was with diet alone (49%), oral medication (27%) or insulin ± oral agents (25%). Data from these 138 is presented here. Those who did not complete the study were younger (mean age 43y, range 19-60, P<0.01) but there were no other differences in demographic or medical factors compared with those who did complete. Education was recorded as educational level achieved: pre GCSE, GCSE, A-level, degree. 79% were living with a partner. Personality was assessed using the shorter questionnaire known as Mini-markers to quantify Goldberg’s Big Five personality domains:15,16 openness/intellect (reliability in the present study: Cronbach α=0.81), conscientiousness (α=0.79), extroversion (α=0.82), agreeableness (α=0.76) and emotional stability (α=0.75). Health Threat Communication was measured using the DHTC questionnaire.14 This comprises two factors: reassurance (α=0.85-0.87 at the 4 time points) and threat (α=0.66-0.73). We assessed illness perceptions using the revised Illness Perception Questionnaire (IPQ-R).17 The IR domains are: symptoms (α=0.78-0.82), internal cause (α=0.82-0.86) referring to the patient’s own behavior being responsible, consequences (α=0.54-0.58) for the patient’s life in general, personal control (α=0.76-0.87) over the illness, treatment control (α=0.65-0.76) by therapy, professionals and the NHS, time-line (α=0.78-0.81) assessing variability and predictability of the condition, illness coherence (α=0.84-0.89) meaning the patient’s perception of understanding of the condition and emotions (α=0.80-0.88) : anxiety, depression, anger and fear. Coping behaviors were assessed using the situational version of the COPE inventory.18 The following coping behaviors were studied over 2 years: active coping (α=0.71-0.76) meaning taking action to remove or circumvent the stressor, planning (α=0.83-0.86) how to confront the problem, seeking instrumental support (α=0.74-0.79): assistance or advice from any relevant source, seeking emotional support (α=0.72-0.81), positive reinterpretation and growth (PRG, α=0.74-0.80) meaning making the best of a situation by reviewing it more favorably and acceptance (α=0.78-0.83) meaning accepting the condition is real but without necessarily taking action.
Given the stability of personality traits over time the Mini-markers were administered at baseline only.19 The DHTC questionnaire, IPQ-R and COPE were administered at baseline, 6, 12 and 24 months after the diagnosis of diabetes. All questions are scored on a numerical scale and a mean score obtained for the factor for each subject.
Statistical methods
To examine changes in coping over time and determine the association of the static baseline factors (type of diabetes, age, gender, presence of partner, educational level) with the coping response variables, General Linear Mixed Models using Restricted Maximum Likelihood (REML) were used (Genstat, VSN International, Hemel Hempstead, UK). Since observations are irregularly spaced in time (0, 6, 12 & 24 months) conventional repeated measures analysis would be less appropriate. Profile plots were used to illustrate the influence of significant categorical demographic variables on coping measures. These highlight how different levels of the demographic factors associated with differences in behavior. The relationship of each of the 5 personality factors with coping was modeled similarly using REML analysis. To assess the influence of reassurance/threat and of the illness representations on coping behavior, separate models were constructed using data from all four time points. This yields regression covariates that change over time and so are not constant throughout the study. These are often described as time-varying covariates. This is in contrast to the static baseline variables mentioned earlier. All covariates were estimated as fixed effects in the model and have the following interpretation. For the main effects and a coping score treated as a continuous outcome, the coefficients reflect the mean change in the baseline level of the outcome variable (coping behavior) with one unit change in the independent variable. For categorical variables (e.g. educational level) we can investigate how the baseline level of the outcome compares to a reference category (the lowest of the 4 educational categories). Where there was significant interaction with time the coefficients give monthly changes in the response with one unit change in the independent variable. The fixed coefficient for a time-varying covariate represents a combination of two types of co-variation: i) main effect (overall different level of response) and ii) time interaction (a changing response over time). A power model with the property that the correlation depends on the distance between the time points was used to capture the correlation structure of the repeated measurements and thereby take account of the irregularly spaced nature of the data. The variance of the observations increased over time. This was directly modeled by specifying heterogeneity to be introduced into the power model. Changes in the deviance indicated that the heterogeneous power model provided a better fit to the variance structure. For these analyses Genstat imputes any missing value of a continuous score with the mean. We assume missing observations are missing at random. It is known that the linear mixed model is fairly robust towards misspecification of certain parts of the model, though residual diagnostic plots revealed the models to be a reasonable approximation to the data.
Results
Changes in coping strategies over time
Table 1 shows mean scores for the COPE domains at baseline, 6, 12 and 24 months. Only the first six coping behaviors listed are included in the following analyses owing to infrequent use of the remainder. In each of the subsequent saturated models all these six coping strategies changed significantly over the two years from diagnosis: acceptance increased (P<0.02) but planning (P<0.001), active coping (P<0.035), seeking instrumental support (P<0.02), seeking emotional support (P<0.02) and trying to see diabetes in a positive way (PRG, P=0.002) decreased.
Table 1.
Mean scores for coping behaviors over time.
| Time from diagnosis (months) |
0 Mean (SD) |
6 Mean (SD) |
12 Mean (SD) |
24 Mean (SD) |
|---|---|---|---|---|
| Acceptance | 3.35 (0.68) | 3.49 (0.55) | 3.48 (0.57) | 3.56 (0.52) |
| Planning | 2.88 (0.82) | 2.63 (0.81) | 2.58 (0.83) | 2.58 (0.84) |
| Active | 2.77 (0.72) | 2.60 (0.75) | 2.63 (0.72) | 2.65 (0.67) |
| Instrumental support | 2.73 (0.74) | 2.60 (0.73) | 2.55 (0.74) | 2.65 (0.70) |
| Emotional support | 2.34 (0.85) | 2.05 (0.76) | 1.89 (0.71) | 1.94 (0.80) |
| PRG | 2.42 (0.88) | 2.23 (0.84) | 2.26 (0.84) | 2.33 (0.81) |
| SCA | 1.51 (0.55) | 1.45 (0.55) | 1.54 (0.55) | 1.43 (0.49) |
| Religion | 1.33 (0.67) | 1.29 (0.63) | 1.27 (0.61) | 1.20 (0.50) |
| Venting emotions | 1.43 (0.66) | 1.34 (0.48) | 1.29 (0.45) | 1.29 (0.44) |
| Denial | 1.21 (0.48) | 1.16 (0.41) | 1.15 (0.39) | 1.14 (0.33) |
| Mental disengagement | 1.13 (0.34) | 1.11 (0.23) | 1.06 (0.22) | 1.07 (0.18) |
| Behavioral disengagement | 1.01 (0.06) | 1.08 (0.29) | 1.08 (0.25) | 1.07 (0.19) |
| Alcohol/drugs | 1.05 (0.28) | 1.05 (0.26) | 1.04 (0.19) | 1.04 (0.20) |
| Humor | 1.78 (0.87) | 1.79 (0.85) | 1.67 (0.85) | 1.69 (0.84) |
PRG, positive reinterpretation and growth, SCA, suppressing competing activities.
Mean scores (n=138, unadjusted data) for coping behaviors measured using the COPE inventory at baseline, 6, 12 and 24 months from diagnosis of diabetes. The minimum score of 1 means do not do this at all; the maximum score of 4 means do this a lot.
A saturated model was fitted to assess the relationship of age, gender, type of diabetes, living with partner and educational level to each of the six coping scores. Type of diabetes bore no relationship to any coping behavior. Age was associated with seeking less emotional support (β=-0.026, P=0.003), less instrumental support (β=-0.008, P=0.049) and less PRG (β=-0.016, P=0.009). Higher educational level was associated with more planning (P=0.005) and more PRG (P=0.002). Age (P<0.001), gender (P=0.037) and presence of partner (P=0.011) were associated with changes in acceptance over time (interactions significant). The age by time interaction was significant because of a positive association with age at 6 months but less acceptance with age at 1 and 2 years. For categorical demographic factors we generated profile plots where there were significant differences between the categories in use of acceptance as a coping strategy. These show large differences at baseline for gender and partner/no partner with opposite trajectories over time (Figure 1). Educational background influenced the level of Planning and PRG scores, but the shape of the profiles over time is similar across the four groups (Figure 2) consistent with the finding of no significant educational level versus time interaction.
Figure 1.
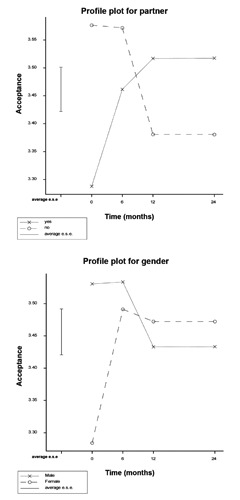
Profile plots demonstrating changes in Acceptance over time according to gender and presence of partner. Error bar shows average estimated SE.
Figure 2.
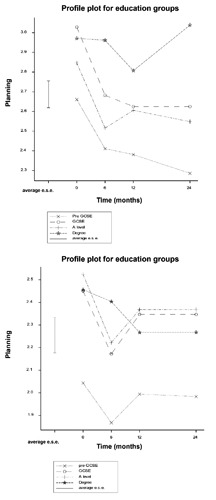
Profile plots demonstrating changes in Planning and PRG over time according to educational level. Error bar shows average estimated SE.
Table 2 shows the relationship of personality and perceptions of reassurance and threat with coping over 2 years. Neuroticism did not relate significantly to any of the six coping strategies. Table 3 shows the relationship between IRs and the 6 coping behaviors. Risk/causation and timeline are not shown because they showed no significant relationships with coping. Table 4 shows effect sizes for changes in coping over time: initial value and absolute changes at 6, 12 and 24 months using the saturated model containing the demographic and medical factors. The regression coefficients indicate change from baseline. For acceptance, the significant increase occurred at 12 months. For seeking emotional support the significant reduction occurred at 24 months. Planning, PRG and seeking instrumental support all showed significant reduction at 6 months.
Table 2.
Significant relationships of personality traits, reassurance and threat with coping behaviors.
| Response | Acceptance | Active | Emotional support | Planning | PRG | Instrumental support | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed term | DF | β | F prob | β | F prob | β | F prob | β | F prob | β | F prob | β | F prob |
| Openness/intellect | 1 | 0.085 | <0.001 | 0.11 | <0.001 | 0.079 | <0.001 | 0.087 | 0.005 | ||||
| Conscientiousness | 1 | 0.051 | 0.050 | 0.015 | 0.027 | ||||||||
| Extroversion | 1 | 0.095 | 0.028 | ||||||||||
| Agreeableness | 1 | -0.031 | 0.023 | 0.14 | <0.001 | 0.18 | 0.023 | 0.25 | <0.001 | 0.33 | <0.001 | 0.11 | 0.010 |
| Reassurance | 1 | 0.06 | 0.002 | 0.05 | 0.013 | 0.023 | |||||||
| Threat | 1 | 0.17 | <0.001 | 0.11 | <0.001 | 0.14 | <0.001 | 0.15 | <0.001 | 0.14 | <0.001 | ||
| Threat x time | 3 | 0 -0.12 -0.02 -0.12 |
0.037 | ||||||||||
Relationship of personality traits, reassurance and threat to coping behaviors over time. Significant results only are shown. None of the personality factors or reassurance showed significant interaction with time. Significant interaction between threat and time generates a standardized coefficient for each time point in relation to the baseline (at diagnosis) measurement.
Table 3.
Significant relationships between illness representations and coping behaviors.
| Response | Acceptance | Active | Emotional support | Planning | PRG | Instrumental support | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed term | DF | β | Chi prob | β | Chi prob | β | Chi prob | β | Chi prob | β | Chi prob | β | Chi prob |
| Consequences | 1 | 0.23 | 0.041 | 0.22 | 0.025 | 0.14 | 0.036 | ||||||
| Emotion | 1 | -0.19 | <0.001 | -0.19 | 0.030 | ||||||||
| Ill. coherence | 1 | 0.15 | <0.001 | 0.15 | <0.001 | 0.06 | 0.004 | 0.06 | <0.001 | 0.06 | <0.001 | 0.23 | <0.001 |
| Personal control | 1 | 0.23 | 0.003 | 0.23 | <0.001 | 0.28 | 0.005 | 0.19 | <0.001 | -0.18 | <0.001 | 0.34 | 0.003 |
| Symptoms | 1 | -0.04 | 0.008 | -0.004 | 0.028 | 0.018 | 0.008 | 0.01 | 0.045 | 0.04 | <0.001 | ||
| Treatm’t control | 1 | 0.07 | 0.012 | 0.50 | <0.001 | 0.60 | 0.031 | 0.09 | 0.005 | ||||
| Consequences x time | 3 | 0 -0.19 -0.27 -0.24 |
0.002 | ||||||||||
| Emotion x time | 3 | 0 -0.01 -0.34 -0.30 |
0.013 | ||||||||||
| Symptoms x time | 3 | 0 -0.004 0.028 0.027 |
0.004 | ||||||||||
The relationships between illness representations and coping over time. Significant results only are shown. Significant interactions generate a standardized coefficient for each time point in relation to the baseline (at diagnosis) measurement.
Table 4.
Coping behavior score at baseline and effect sizes over time.
| COPE score Time (months) |
Mean 0 |
Change from baseline (SE) | ||
|---|---|---|---|---|
| 6 | 12 | 24 | ||
| Acceptance | 3.36 (0.18) | 0.18 (0.14) | 0.65 (0.21)* | 0.47 (0.24) |
| Active | 2.71 (0.17) | -0.31 (0.21) | -0.068 (0.30) | -0.043 (0.28) |
| Emotional support | 2.41 (0.19) | -0.29 (0.19) | -0.46 (0.28) | -0.80 (0.30)** |
| Planning | 2.68 (0.19) | -0.46 (0.22)** | -0.24 (0.33) | -0.32 (0.32) |
| PRG | 2.54 (0.21) | -0.39 (0.19)** | -0.002 (0.30) | -0.011 (0.30) |
| Instrumental support | 2.81 (0.17) | -0.43 (0.19)** | -0.24 (0.29) | -0.23 (0.28) |
Coping behaviors: summary of baseline value (the minimum score of 1 means do not do this at all; the maximum score of 4 means do this a lot) and effect sizes (change in score from baseline) over time using the saturated model containing the demographic and medical factors.
*P<0.01
**P<0.05.
Discussion
Use of coping behaviors
After diagnosis of diabetes passive acceptance was used more than other coping strategies and this was evident up to two years post diagnosis. Acceptance is important with an incurable long-term condition where the stressor must be accommodated. Acceptance alone is less helpful when the stressor is amenable to change. Consistent with previous work our subjects used problem-focused coping eg planning, active coping and gaining instrumental support to a greater extent than passive/emotional and avoidance coping (as listed in Table 1).1,20 Problem-focused coping and acceptance is associated with better functioning but individuals with long-term conditions often use both problem-focused and emotion-focused coping.20,21 Our patients frequently sought emotional support. Carver, Scheier & Weintraub have described seeking emotional support as a double-edged sword.18 The reassurance gained from receiving emotional support may encourage a return to problem-focused coping. But if used only as an outlet for expressing negative emotions it may be less adaptive. Redefining the problem in a positive way (PRG), may be used to manage distressing emotions and can lead to active problem-focused coping responses. In the current study many patients highlighted positive consequences associated with a diagnosis of diabetes including improved diet and lifestyle. Since PRG and seeking emotional support were used in conjunction with problem-focused coping, we have interpreted these two coping strategies as being effective (adaptive) strategies potentially contributing to diabetes management.
Changes in coping over two years following diagnosis of diabetes
Acceptance increased over the 2-years following diagnosis of diabetes with the largest change at 1 year. Seeking emotional support progressively reduced. Our research has shown that emotional representations of this patient group decrease and understanding of diabetes (illness coherence) increases over time.10 The reduction in planning, PRG and seeking instrumental support at 6 months suggests behaviour patterns may be established by this stage.
Differences in coping according to demographic factors
There were significant differences within the group in terms of the use of acceptance as a coping strategy. The use of acceptance as a coping strategy followed a different trajectory for those with and without partners at baseline. People living with a partner were less likely to accept their diabetes immediately after diagnosis but acceptance increased over time. In contrast, acceptance decreased over the first year in patients without a partner. With no supportive partner to encourage and reinforce recommended lifestyle changes, especially in the absence of symptoms, patients may be more likely to ignore their diabetes. Males were more likely than females to accept their diabetes initially. Females have been shown to react with more emotion focused coping and avoidance than men.22 However, by 6 months scores had leveled out. Acceptance scores for all groups were relatively high. Older patients were less likely to seek instrumental support, use PRG and seek emotional support over time. The elderly may minimize health risk.23 Others suggest older people with a long-term condition and those with lower educational level use more avoidant and/or emotion-focused coping.1 Profile plots for the 4 educational groups showed that people with a degree were more likely to use planning to cope with diabetes. Those who had not achieved GCSE level (or equivalent) were less likely than the other groups to plan or attempt to view their diabetes in a positive way.
The profile plots (Growth curve modeling) showed no differences in coping over time between those with type 1 and those with type 2 diabetes. Previous studies have shown type 1 diabetes was associated with more symptoms and type 2 diabetes with more internal cause (self-blame) but otherwise no difference in illness perceptions between type 1 and type 2 diabetes.10 There were no differences in perceptions of personal control, treatment effectiveness or consequences between patients with type 1 and type 2 diabetes. Consequently it is unsurprising that there was no difference in coping behavior with type of diabetes. The initial symptoms of type 1 diabetes do not seem to influence perceptions of diabetes or behavior. Conclusions with respect to type of diabetes should be treated with caution owing to the relatively small number of type 1 diabetic patients.
Changes in coping according to personality
Openness/intellect was associated with use of adaptive coping strategies. This trait is felt to reflect a more flexible, imaginative and intellectually curious outlook which could contribute to the coping behaviors seen here.24 Perhaps surprisingly, conscientiousness showed weaker association with active coping and seeking (instrumental) support e.g. from friends, family or professionals. One would expect these traits to be associated with adaptive coping and hence better control of diabetes, however, Lane et al. were unable to show a relationship with glycemic control but conscientiousness has been shown to be associated with slower decline in renal function in diabetes, presumably due to better self-care.25,26
Those scoring high for agreeableness might be expected to show acceptance, more positive reinterpretation and to undertake the active measures advised and they did so. However, this trait was also associated with seeking emotional support which might not have been anticipated. Agreeableness showed the strongest association with adaptive coping. Booth-Kewley & Vickers found conscientiousness and agreeableness to be important determinants of health behavior.27
In our analysis neuroticism showed no association with coping behaviors. In general, neuroticism has been consistently associated with passive and ineffectual coping behaviors. Surprisingly, Lane et al. found more neuroticism associated with better glycemic control.25 However, in a comparison of models in young adults with type 1 diabetes, Skinner et al found emotional stability positively influenced self-care through the IR of perceived threat and that conscientiousness influences self-care through its influence on the perception of treatment effectiveness.28
Personality traits were an important influence on coping behavior but these relationships did not vary over time. We were unable to assess relationships to maladaptive coping strategies (denial, venting emotions, mental/behavioral disengagement, use of alcohol, drugs or humor) due to low use of these coping behaviors.
Changes in coping according to health threat communication
Perceived threat showed strong association with active coping, seeking emotional and instrumental support, planning and PRG. We interpret this constellation of coping behaviors as an adaptive approach to the medical condition. However, active coping in response to perceived threat significantly declined from baseline when assessed at 6, 12 and 24 months. This change over time is mirrored by the active coping response to perceived consequences which also declined suggesting that the health threat is perceived less severe and becomes less motivating over time. It seems likely that the DHTC threat domain and the IPQ-R consequences domain measure similar constructs. However, health threat as measured by the DHTC is more focused on diabetes and its complications whereas IPQ-R includes financial consequences and effects on family.14,17 Woodcock & Kinmonth showed that professionals underestimate patients’ fear of the consequences of diabetes in the first year after diagnosis.29 We found that patients coping response to both perceived threat and consequences progressively declines.
Changes in coping according to illness representations (patient’s health beliefs)
The CSM suggests a close relationship between IRs and coping. In the present analysis we show that illness coherence (understanding of diabetes), symptoms, personal and treatment control relate closely to the six coping behaviors most commonly used by diabetic patients. Illness coherence, personal and treatment control especially are associated positively with adaptive coping. Interestingly, more symptoms associated with less active coping but seeking more emotional support suggesting symptoms may result in a less adaptive approach.
In previous analysis, perceptions of symptoms, consequences, time-line, and control of diabetes remained stable after diagnosis of diabetes.10 Emotional responses to diabetes decreased and illness coherence increased. Although coherence here had a positive association with all 6 coping behaviors over the 2 years only acceptance showed a significant increase. Thus, intervention may be of value to maintain and increase adaptive coping behaviors. Emotional reaction was associated with less active coping, less acceptance and over time less PRG. Perceptions of serious consequences were associated with active coping but this became less so over the 2 year period. Thus, neither emotional response nor perceptions of serious consequences seem particularly helpful over time.
The relationships demonstrated here between individual IRs and specific coping behaviors provide further support for the validity of the CSM. Furthermore, these relationships give some insight into the relative contributions of rational objective versus emotional representations to the coping behaviors adopted.
Conclusions
Practice implications
The significance of these data relates to the implications for intervention to increase adaptive coping behavior over time in patients with diabetes. Demographic factors have some relevance: those with lower educational achievement need more support with planning and, importantly, in taking a positive approach to their condition. The relationship between openness/intellect and adaptive coping reflects this also. Identification of and support for those with significant emotional response might limit its adverse effect on active coping. The reduction in the influence of threat and perceived serious consequences over time indicates that practitioners cannot rely on these factors to support adaptive coping. More sustained success is likely to come from aiding greater understanding of diabetes and improving perceptions of personal and treatment control in our patients since these were positively associated with adaptive coping without change over time. A variety of interventions have been tried in both type 1 and type 2 diabetes but generally without psychometric assessment beforehand and with varying success.30 Demographic factors, personality, perceptions of health threat and consequent illness representations differ between patients such that an individualized approach is needed.
Strengths and limitations
Strengths are the longitudinal design over two years and the low attrition rate such that the dataset is relatively complete. The focus was changes over time in higher order coping behaviors. A limitation is that these are not diabetes specific and can only be related to self-care in diabetes in general terms. The finding that adaptive coping is more prevalent than maladaptive meant that our numbers were insufficient to draw conclusions about maladaptive behavior and neuroticism. We cannot draw firm conclusions about type 1 diabetes independently of type 2 because of small numbers although in other studies we have found little difference in IRs according to type of diabetes. Future work should try to relate coping behavior to the outcome measure of glycemic control.
Acknowledgements
We would like to acknowledge with gratitude grant support from Diabetes UK and the invaluable contribution of staff and patients.
References
- 1.Maes S, Leventhal H, de Ridder D. Coping with chronic diseases. Zeidner M, Endler NS, eds. Handbook of coping: theory, research, applications. New York: John Wiley; 1996. pp 221-51. [Google Scholar]
- 2.Leventhal H, Nerenz D, Steele D. Illness representations and coping with health threats. Baum A, Singer J, eds. A Handbook of psychology and health. Hillsdale: Lawrence Erlbaum Associates; 1984. pp 219-52. [Google Scholar]
- 3.Harvey JN, Lawson VL. The importance of health belief models in determining self-care behaviour in diabetes. Diabet Med 2009;26:5-13. [DOI] [PubMed] [Google Scholar]
- 4.Moss-Morris R, Petrie KJ, Weinman J. Functioning in chronic fatigue syndrome: Do illness perceptions play a regulatory role? Br J Health Psychol 1996;1:15-25. [Google Scholar]
- 5.Endler NS, Corace KM, Summerfeldt LJ, et al. Coping with chronic pain. Pers Indiv Differ 2003;34:323-46. [Google Scholar]
- 6.Kennedy P, Marsh N, Lowe R, et al. A longitudinal analysis of psychological impact and coping strategies following spinal cord injury. Br J Health Psychol 2000;5:157-72. [DOI] [PubMed] [Google Scholar]
- 7.Pollard C, Kennedy P. A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: a 10-year review. Br J Health Psychol 2007;12:347-62. [DOI] [PubMed] [Google Scholar]
- 8.Rutter CL, Rutter DR. Longitudinal analysis of the illness representation model in patients with irritable bowel syndrome (IBS). J Health Psychol 2007;12:141-8. [DOI] [PubMed] [Google Scholar]
- 9.Lawson VL, Bundy C, Belcher J, Harvey JN. Mediation by illness perceptions of the effect of personality and health threat communication on coping with the diagnosis of diabetes. Br J Health Psychol 2010;15:623-42. [DOI] [PubMed] [Google Scholar]
- 10.Lawson VL, Bundy C, Harvey JN. The development of personal models of diabetes in the first 2 years after diagnosis: a prospective longitudinal study. Diabet Med 2008;25:482-90. [DOI] [PubMed] [Google Scholar]
- 11.Peel E, Parry O, Douglas M, Lawton J. Diagnosis of type 2 diabetes: a qualitative analysis of patients’ emotional reactions and views about information provision. Patient Educ Counseling 2004;53:269-75. [DOI] [PubMed] [Google Scholar]
- 12.Lawson V, Lyne PA, Bundy CE, Harvey JN. Understanding why people with type 1 diabetes do not attend for specialist advice: a qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J Health Psychol 2005;10:409-23. [DOI] [PubMed] [Google Scholar]
- 13.Lawson VL, Bundy CB, Harvey JN. The influence of health threat communication and personality on personal models of diabetes in newly diagnosed diabetic patients. Diabet Med 2007;24:883-91. [DOI] [PubMed] [Google Scholar]
- 14.Lawson VL, Bundy C, Harvey JN. Development of the Diabetes Health Threat Communication Questionnaire (DHTCQ). Patient Educ Counseling 2007;67:117-26 [DOI] [PubMed] [Google Scholar]
- 15.Saucier G. Mini-Markers: A brief version of Goldberg’s unipolar Big Five markers. J Pers Assess 1994;63:506-16. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg LR. The development of markers for the Big Five factor structure. Psychol Assess 1992;4:26-42. [Google Scholar]
- 17.Moss-Morris R, Weinman J, Petrie KJ, et al. The Revised Illness Perception Questionnaire (IPQ-R). Psychol Health 2002;17:1-16. [Google Scholar]
- 18.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 1989;56:267-83. [DOI] [PubMed] [Google Scholar]
- 19.Hampson S. State of the art: personality. Psychologist 1999;12:284-8. [Google Scholar]
- 20.Macrodimitrus SD, Endler NS. Coping, control, and adjustment in type 2 diabetes. Health Psychol 2001;20:208-16. [PubMed] [Google Scholar]
- 21.Kaptein AA, Helder DI, Scharloo M, et al. Illness perceptions and coping explain well-being in patients with Huntingdon’s disease. Psychol Health 2006;21:431-46. [Google Scholar]
- 22.Smari J, Valtysdottir H. Dispositional coping, psychological distress and disease-control in diabetes. Pers Indiv Differ 1997;22:151-6. [Google Scholar]
- 23.Leventhal E, Crouch M. Are there differences in perceptions of illness across the lifespan? Petrie KJ, Weinman JA, eds. Perceptions of health & illness. Amsterdam: Harwood Academic Publishers; 1997. pp 77-102. [Google Scholar]
- 24.Watson D, Hubbard B. Adaptational style and dispositional structure: coping in the context of the five-factor model. J Personal 1996;64:737-74. [Google Scholar]
- 25.Lane JD, Parekh PI, McCaskill CC, et al. Personality correlates of glycaemic control in type 2 diabetes. Diabetes Care 2000;23:1321-5. [DOI] [PubMed] [Google Scholar]
- 26.Brickman AL, Yount SE, Blaney NT, et al. Personality traits and long-term health status. The influence of neuroticism and conscientiousness on renal deterioration in type 1 diabetes. Psychosomatics 1996;37:459-68. [DOI] [PubMed] [Google Scholar]
- 27.Booth-Kewley S, Vickers RR. Associations between major domains of personality and health behaviour. J Pers 1994;62:281-98. [DOI] [PubMed] [Google Scholar]
- 28.Skinner TC, Hampson SE, Fife-Schaw C. Personality, personal model beliefs and self-care in adolescents and young adults with type 1 diabetes. Health Psychol 2002;21:61-70. [PubMed] [Google Scholar]
- 29.Woodcock A, Kinmonth AL. Patient concerns in their first year with type 2 diabetes: Patient and practice nurse views. Patient Educ Counseling 2001;42:257-70. [DOI] [PubMed] [Google Scholar]
- 30.Keen A. Which psychological interventions work? J R Coll Physicians Edinb. 2012;40 Suppl 17:20-4. [Google Scholar]


