Abstract
Antimicrobial resistance (AMR) is one of the most serious global public health threats in this century. The first World Health Organization (WHO) Global report on surveillance of AMR, published in April 2014, collected for the first time data from national and international surveillance networks, showing the extent of this phenomenon in many parts of the world and also the presence of large gaps in the existing surveillance. In this review, we focus on antibacterial resistance (ABR), which represents at the moment the major problem, both for the high rates of resistance observed in bacteria that cause common infections and for the complexity of the consequences of ABR. We describe the health and economic impact of ABR, the principal risk factors for its emergence and, in particular, we illustrate the highlights of four antibiotic-resistant pathogens of global concern – Staphylococcus aureus, Klebsiella pneumoniae, non-typhoidal Salmonella and Mycobacterium tuberculosis – for whom we report resistance data worldwide. Measures to control the emergence and the spread of ABR are presented.
Keywords: Antimicrobial resistance, Global surveillance, Antibiotic use, Veterinary medicine, MRSA, Klebsiella pneumoniae, Non-typhoidal Salmonella, Mycobaterium tuberculosis
Introduction
Antimicrobial resistance (AMR) has emerged as one of the principal public health problems of the 21st century that threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi no longer susceptible to the common medicines used to treat them. The problem of AMR is especially urgent regarding antibiotic resistance in bacteria. Over several decades, to varying degrees, bacteria causing common or severe infections have developed resistance to each new antibiotic coming to market. Faced with this reality, the need for action to avert a developing global crisis in health care is imperative.
The World Health Organization (WHO) has long recognised the need for an improved and coordinated global effort to contain AMR. In 2001, the WHO Global Strategy for Containment of Antimicrobial Resistance has provided a framework of interventions to slow the emergence and reduce the spread of antimicrobial-resistant microorganisms;1 In 2012, WHO published The Evolving Threat of Antimicrobial Resistance – Options for Action2 proposing a combination of interventions that include strengthening health systems and surveillance; improving use of antimicrobials in hospitals and in community; infection prevention and control; encouraging the development of appropriate new drugs and vaccines; and political commitment.
Following the indication of a primary role for surveillance, in April 2014, WHO published the first global report on surveillance of AMR collecting experiences from national and international surveillance networks.3 This report shows that surveillance data, where available, can be very useful for orienting treatment choices, understanding AMR trends, identifying priority areas for interventions, and monitoring the impact of interventions to contain resistance. The lack of adequate surveillance in many parts of the world leaves large gaps in existing knowledge of the distribution and extent of this phenomenon.
Our review examines the main factors contributing to the development of antibiotic resistance and the consequences for human health focussing on the impact of resistance in species commonly associated with infection (i.e. Staphylococcus aureus, Klebsiella pneumoniae, non-typhoidal Salmonella) in different settings and in the treatment of tuberculosis.
Impact of Antibiotic Resistance
The impact of antibiotic resistance in terms of mortality and of the public health cost is quite difficult to estimate, and there are few studies addressing this issue. The US Center for Disease Control and Prevention (CDC) conservatively estimated that, in the US, more than two million people every year are affected with antibiotic-resistant infections, with at least 23 000 dying as a result of the infection.4
In Europe each year, the number of infections and deaths due to the most frequent multidrug-resistant bacteria (S. aureus, Escherichia coli, Enterococcus faecium, Streptococcus pneumoniae, Klebsiella pneumoniae and Pseudomonas aeruginosa) was estimated at ∼400 000 and 25 000, respectively, in 2007.5
Several fields of modern medicine depend on the availability of effective antibiotic drugs; chemotherapy for cancer treatment, organ transplantation, hip replacement surgery, intensive care for pre-term newborns and many other activities could not be performed without effective antibiotics. In fact, infections caused by multidrug-resistant bacterial strains are among the main factors influencing morbidity and mortality in patients undergoing these procedures. A report from the University of Texas, published in 2014, showed high antibiotic resistance rates in infections in cancer patients with chemotherapy-related neutropenia.6 A recent study from the Medical University of Warsaw, on infections after orthotopic liver transplantation, showed a high proportion of isolates of antibiotic-resistant bacteria.7
Common infections in neonatal intensive care are increasingly becoming extremely difficult, and sometimes impossible, to treat.8Staphylococcal species, most notably S. epidermidis and S. aureus, cause ∼60%–70% of infections, and numerous outbreaks of methicillin-resistant S. aureus (MRSA) have been reported in these units.9
Also the economic impact of antibiotic resistance is difficult to quantify, as several types of consequences must be taken into account. Increased resistance leads to elevated costs associated with more expensive antibiotics (when infections become resistant to first-line antimicrobials, treatment has to be switched to second- or third-line drugs, which are nearly always more expensive), specialised equipment, longer hospital stay and isolation procedures for the patients. Societal costs include death and loss of productivity. In Europe, the overall crude economic burden of antibiotic resistance was estimated to be at least 1.5 billion euros with more than 900 million euros corresponding to hospital costs. Productivity loss due to absence from work or death from infection accounted for 40% of the total estimated cost.5 However, the estimate was based on antibiotic resistance surveillance data collected in 2007 and may underestimate the present burden of antibiotic resistance, which is a constantly evolving phenomenon.
In the US, the CDC estimated the cost of AMR as $55 billion per year overall: $20 billion in excess for direct healthcare costs, with additional society costs for lost productivity as high as $35 billion a year.4
Factors contributing to the emergence of antibiotic resistance
Antibiotic resistance is a natural phenomenon that occurs when microorganisms are exposed to antibiotic drugs. Under the selective pressure of antibiotics, susceptible bacteria are killed or inhibited, while bacteria that are naturally (or intrinsically) resistant or that have acquired antibiotic-resistant traits have a greater chance to survive and multiply. Not only the overuse of antibiotics but also the inappropriate use (inappropriate choices, inadequate dosing, poor adherence to treatment guidelines) contribute to the increase of antibiotic resistance.
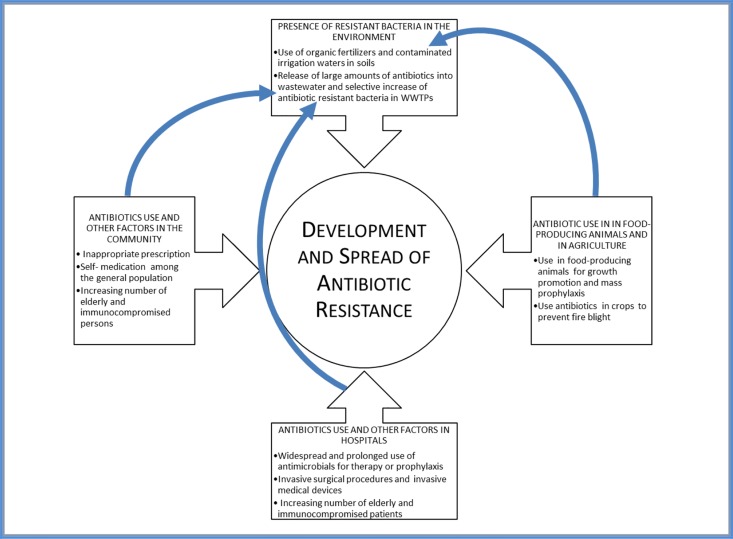
Figure 1 shows a schematic representation of factors involved in the emergence and spread of antibiotic resistance. We identified four main sectors involved in the development of antibiotic resistance: human medicine in community and in hospital, animal production and agriculture, and the environmental compartment.
Figure 1.
Factors involved in the spread of antibiotic resistance, in the sectors: human medicine in the community and in the hospital, animal production and agriculture, and the environment. These sectors are also connected among them: misuse of antibiotics in human beings, animals and agriculture is the main responsible for the presence of resistant bacteria in the environment.
Antibiotic resistance in human medicine
In the community of affluent countries, the excessive prescription by general practitioners, even in the absence of appropriate indications, plays an important role in the inappropriate use of antibiotics. Diagnostic uncertainty often fosters over-prescription especially when the clinical picture of viral or bacterial aetiology is similar. Self-medication (see below) also plays an important part.
In many developing countries, excessive use is due to the easy availability of antimicrobial drugs that can be purchased without prescription of a physician or other qualified health professional. In both situations, there is the perception that antibiotics are the “wonder drugs” that can rapidly cure any kind of ailments.
In the hospital setting, the intensive and prolonged use of antimicrobial drugs is probably the main contributor to the emergence and spread of highly antibiotic-resistant nosocomial infections; but other factors can play an important role: presence of highly susceptible immunosuppressed patients (e.g. AIDS patients, cancer patients, or transplant recipients) and fragile elderly patients, invasive surgical procedures and intensity of clinical therapy, lengthy of stay in hospital,10 failure to control infections spread from patient to patient.
• Antibiotic consumption in the community and in hospital settings
The annual report of the European Surveillance of Antimicrobial Consumption Network (ESAC-Net) reported that in Europe during 2012 the consumption in the community of antibacterials for systemic use [Anatomical Therapeutic Chemical (ATC) group J01], ranged from 11.3 (the Netherlands) to 31.9 (Greece) defined daily doses (DDD) per 1000 inhabitants per day. In all ESAC-Net reports, a geographic gradient in the amount of antibiotics used can be noted, with higher DDD in the South of Europe. In 2012, the beta-lactams/penicillins group (ATC J01C) accounted for 50% of the consumption of antibacterials for systemic use and amoxicillin, alone or in combination with clavulanic acid, was the antibacterial agent most often used in almost all countries, with the exception of Norway and Sweden where the most used agent was phenoxymethylpenicillin.
In the hospital sector ESAC-Net estimated that in 2012, the population-weighted EU/EEA mean consumption for systemic use of antibacterials was 2.0 DDD per 1000 inhabitants, ranging from 1.0 DDD per 1000 inhabitants per day in the Netherlands, to 2.8 in Finland. Also in the hospital setting, the beta-lactams/penicillins group was most often used, accounting for 29.3% of all the consumption of antibacterials for systemic use.11
According to a recent point prevalence survey on healthcare associated infections in Europe, 35.0% of the hospitalised patients in 2011 were receiving antibiotics.12
In the US, healthcare providers prescribed 258.0 million courses of antibiotics (833 prescriptions per 1000 persons) in 2010. Penicillins (23%) and macrolides (22%) were the most common categories prescribed. The most frequently prescribed antibiotic agents were azithromycin and amoxicillin.13
Large-scale assessments of antimicrobial use in hospitals in the USA are derived from studies conducted in groups of acute care hospitals.14,15 According to one of these studies, a mean of 59.3% of all patients received at least one dose of an antimicrobial agent during their hospital stay.14
• Incorrect knowledge about antibiotics in the population and self-medication
Many studies indicate lack of knowledge about antibiotics in the general population, specifically incorrect knowledge about the activity of antibiotics on bacteria and viruses, insufficient awareness about antibiotic resistance and about the adverse effects of antibiotics.
A survey, carried out in 2009, on the use and on the knowledge of antibiotics among European citizens, revealed that 20% of the people interviewed admitted they had taken antibiotics to treat flu-like symptoms, although they knew that antibiotics do not act against viruses. In addition, 14% also said that they had taken antibiotics to treat a common cold.16
A survey among adults in the United Kingdom showed that 38% of respondents did not know that antibiotics do not work against most coughs or colds.17 On the contrary, in Sweden, the knowledge about antibiotics as well as the risk of antibiotic resistance is fairly good and homogeneous. Only one-fifth of respondents was convinced that antibiotics cure common colds more quickly.18
The inappropriate use of antibiotics is also associated with other common behaviour patterns, such as failure to complete the recommended treatment or self-medication. Self-medication with antimicrobials almost always involves unnecessary, inadequate, and ill-timed dosing, creating an ideal environment for microbes to adapt rather than be eliminated. Self-medication with antimicrobials is common in many areas of world, particularly in developing countries with loose regulatory systems where antibiotics are sold over the counter drugs, but also in some affluent countries. A higher prevalence of self-medication with antibiotics was reported in South Europe (19%) in comparison with northern Europe (3%) and central Europe (6%). In some countries of Africa, 100% of antimicrobial use is without prescription and in Asia it reaches 58%.19
Use of antibiotics in food-producing animals and in agriculture
A substantial proportion of total antibiotic use occurs outside the field of human medicine. Antimicrobial use in food-producing animals and in aquaculture for growth promotion and for disease treatment or prevention is probably a major contributor to the overall problem of resistance.20 While the use of antibiotics as growth promoters has been completely banned in Europe since 2006, this is still common practice in several countries, including the USA.21
The fourth report of European Surveillance of Veterinary Antimicrobial Consumption (ESVAC) that includes data from 26 EU countries showed that sales of antibiotics for use (therapy or prophylaxis) in food-producing animals during 2012, amounted to 8000 tonnes of active ingredients, with tetracyclines, penicillins and sulphonamides being the most sold antimicrobial classes.22 In the US, in 2012, sales of antimicrobials approved for use in food-producing animals was ∼14 800 tonnes and tetracyclines represented the most sold antimicrobial class, accounting for 41% of the total.23
The use of antibiotics in agriculture is a controversial practice. The main use of antibiotics, specifically streptomycin, is to prevent a disease of apple and pear trees named fire blight that is caused by a bacterium named Erwinia amylovora. The concern that antibiotic use in agriculture might increase the frequency of antibiotic resistance genes in bacteria living on plant surfaces and that genes conferring resistance might then be transferred into clinically important bacteria has resulted in tighter restrictions on the use of antibiotics in plant agriculture in Europe and in USA.24
The environment and the spread of resistance
During the last years, the importance of the environment in the spread of antibiotic resistance has been widely recognised.
The soil is regarded as a reservoir of antibiotic resistance genes, since most antibiotics are derived from soil microorganisms that are intrinsically resistant to the antibiotics produced. In addition, water potentially contaminated with faecal microorganisms and organic fertilisers used on food crops may disseminate drug-resistant bacteria in the soil.
Water is a major way of dissemination of bacteria between different environmental compartments. Large amounts of antibiotics are released into municipal wastewater due to incomplete metabolism in human beings or due to disposal of unused antibiotics. Some available data show that antibiotic-resistant bacteria and antibiotic-resistant genes can be detected in wastewater samples and that the conditions in wastewater treatment plants (WWTPs) are favourable for the proliferation of resistant bacteria. In the last decade, several studies have reported high concentrations of tetracycline and sulphonamide-resistant bacteria and sulphonamide-resistant genes in WWTPs.25,26
The emergence of resistance in some bacterial species commonly cause of human infections
An increasing number of pathogenic organisms are resistant to one or more antimicrobial drugs. As a consequence, some common infections have become extremely difficult and in some cases nearly impossible to treat. Pneumonia, which was readily treatable after the introduction of penicillin, now more often requires second- and third-line antibiotics. Cystitis, one of the most common bacterial infections in women, which was easily treatable using oral medication, now needs quite always more complex antibiotic treatments that impose additional costs on the patients and the health system.27,28
We describe below three bacterial species, which exemplify antibiotic-resistant pathogens causing infections in different settings: S. aureus, common in hospital and in the community; non-typhoidal Salmonella (NTS), a major cause of foodborne diseases; and K. pneumoniae, causing healthcare-associated infections. In addition, a paragraph will be devoted to drug-resistant tuberculosis.
Table 1 shows the extent of resistance in S. aureus, NTS and K. pneumoniae to antibiotics commonly used to treat infections caused by these pathogens, summarised by WHO region.3 We have considered only national data (based on at least 30 tested isolates) and not single studies, to limit the heterogeneity of the information. Unfortunately, in few countries only, national official sources are available and therefore the table provides insight into the existing surveillance gaps in ABR surveillance.
Table 1.
Resistance to key antibiotics of S. aureus, K. pneumoniae and NTS in the six World Health Organization (WHO) world regions. The data are derived from WHO3
| WHO regions | S. aureus resistance to methicillin (MRSA) | NTS resistance to fluoroquinolones | K. pneumoniae resistance to third-generation cephalosporins | K. pneumoniae resistance to carbapenems | |
|---|---|---|---|---|---|
| Africa region (47 countries) | Countries with national data | 9 (19.1%) | 9 (19.1%) | 13 (27.6%) | 4 (8.5%) |
| Range (%) | 0–100 | 0–35 | 8–77 | 0–4 | |
| Country with lowest/highest proportion | Lesotho/Guinea-Bissau | Central African Republic/Mauritania | Namibia/South Africa | Central African Republic/South Africa | |
| Region of the Americas (47 countries) | Countries with national data | 15 (31.9%) | 13 (27.6%) | 17 (36%) | 17 (36.2%) |
| Range (%) | 21–90 | 0–96 | 4–71 | 0–11 | |
| Country with lowest/highest proportion | Canada/Chile | Several countriesa/Peru | Canada/Peru | Canada-Dominican Republic/United States of America | |
| Eastern Mediterranean region (23 countries) | Countries with national data | 4 (17.4%) | 4 (17.4%) | 4 (17.4%) | 4 (17.4%) |
| Range (%) | 10–53 | 2–49 | 22–50 | 0–54 | |
| Country with lowest/highest proportion | Bahrain/Iran | Oman/Jordan | Oman/Bahrain | Oman/Iran | |
| European region (53 countries) | Countries with national data | 36 (67.9%) | 29 (50.9%) | 33 (62.3%) | 31 (58.5%) |
| Range (%) | 0.3–55 | 0–21 | 2–82 | 0–68 | |
| Country with lowest/highest proportion | Norway/Portugal | Several countriesa/Finland | Sweden/Georgia | Several countriesa/Greece | |
| South-east Asia region (11 countries) | Countries with national data | 3 (27.3%) | 2 (18.1%) | 4 (36.4%) | 4 (36.4%) |
| Range (%) | 10–26 | 0.2–4 | 34–81 | 0–8 | |
| Country with lowest/highest proportion | Bhutan/Myanmar | Thailand/Nepal | Bhutan/Sri Lanka | Bhutan/Myanmar | |
| Western Pacific region (37 countries) | Countries with national data | 16 (43.2%) | 9 (24.3%) | 12 (32.4%) | 9 (24.3%) |
| Range (%) | 4–70 | 0–14 | 1–71 | 0–8 | |
| Country with lowest/highest proportion | Micronesia/Republic of Korea | Brunei Darussalam/Philippines | Kiribati/Micronesia | New Zeland/China |
We reported “several countries” when more than two countries have the same rate of resistance.
Staphylococcus aureus
S. aureus is a Gram-positive bacterium that is part of the normal flora of the anterior nares, but is one of the most commons causes of nosocomial and community-acquired bloodstream infections, skin and soft tissue infections (SSTIs) and pneumonia in almost all geographic areas.
Strains of S. aureus resistant to antistaphylococcal penicillins are termed MRSA. The first strains of MRSA emerged during the 1960s and spread in the subsequent years3 in association with the increase in the number of elderly and immunocompromised patients. In the healthcare setting, MRSA can cause severe infections such as bloodstream infections, sepsis, pneumonia, and surgical site infections. Hospital-acquired MRSA (HA-MRSA) infections are associated with insertion of medical devices such as central vein catheters, with haemodialysis, or with surgical procedures such as joint replacement.29,30 Recently, MRSA has become a common cause of infections also in the community (CA-MRSA) affecting children and young persons without underlying diseases. Community acquired-MRSA can especially infect persons in activities that cause skin damage and close contacts or crowding (athletes, military personnel, inmates, etc.). While most of the CA-MRSA infections involve the skin, some presentation (necrotising pneumonia, fasciitis) can be very serious.31,32 Methicillin-resistant S. aureus infections require second-line antibacterials, such as vancomycin, that are less effective, more expensive, and need careful monitoring to avoid adverse side effects. New treatment options for MRSA, such as linezolid and daptomycin, are also expensive and not devoid of side effects.
In the United States, in 2011, MRSA were estimated to account for more than 80 000 invasive infections; of these only 14 000 occurred in the hospital.33,34
During the past decade in Europe, several countries implemented national action plans targetted at reducing the spread of MRSA in healthcare facilities. According to the data reported by European Antimicrobial Resistance Surveillance Network (EARS-Net), in the last years (2010–2013), six European countries (Belgium, France, Germany, Ireland, Spain and the United Kingdom), reported a significant decrease in the percentage of MRSA from invasive infections; however, the percentage of MRSA remained above 25% in seven out of 30 reporting countries, mainly in southern and eastern Europe.35
Globally, MRSA proportions exceed 20% in all WHO regions, and in some countries exceed 80%3 (Table 1).
Non-typhoidal Salmonella (NTS)
Salmonellosis is one of the most common and widely distributed foodborne diseases and is caused by bacteria of the genus Salmonella. NTS are infections caused by all serotypes of Salmonella enterica except for serovars Typhi and Paratyphi, which are more invasive and are associated with enteric fever.
There are over 1500 NTS serotypes, the most common being S. Enteritidis, S. Typhimurium and S. Heidelberg, that can be found worldwide in domestic and wild animals (including birds and amphibians). In recent years, the incidence of NTS infection has increased considerably; A study on the global burden of NTS estimated that there are 94 million cases of NTS gastroenteritis, resulting in 155 000 deaths globally each year.36 The majority of the disease burden is in the South-east Asian region.
As for all zoonotic pathogens, also for NTS, the widespread use of antimicrobial agents in food animal production for growth promotion, prophylaxis or treatment purposes has contributed to the spread of antibiotic resistance.37–39 Multidrug resistance to different commonly used antimicrobial agents (ampicillin, chloramphenicol, sulphonamides and tetracycline) is frequent in NTS. Multidrug resistance has been associated with a higher risk of invasive infection, higher frequency and duration of hospitalisation and increased risk of death as compared to infections caused by susceptible strains.40,41 In addition, from 2000, several studies have shown a decreased susceptibility to fluoroquinolones, drugs of choice for treatment of invasive gastrointestinal infections, in many parts of the world.42–44
According to data reported by WHO, fluoroquinolone resistance in NTS is lower in the European region, while it is much higher in some countries of Africa (30%–35%), of Eastern Mediterranean region (46%–49%) and in Peru (96%). In the South-east Asian and Western Pacific regions, where disease burden is very high, there are many information gaps3 (Table 1).
Klebsiella pneumoniae
K. pneumoniae causes infections (bloodstream infections, urinary and respiratory tract infections) that are particularly common in hospitals among vulnerable individuals such as pre-term infants, elderly and patients with impaired immune systems.45,46 In intensive care units and neonatal care facilities, K. pneumoniae can spread readily among patients, leading to nosocomial outbreaks. In recent years, the number of multidrug-resistant K. pneumoniae has risen rapidly.47 Resistance mediated by extended-spectrum beta-lactamases (ESBLs) includes all penicillins, cephalosporins (including third-generation cephalosporins) and aztreonam. Recent studies showed a prevalence of ESBL-producing K. pneumoniae of 38.9% in Europe, 8.8% in the USA and 21.5% in the Asia-Pacific region.48 WHO reported that third-generation cephalosporins resistance in K. pneumoniae was higher than 30% worldwide and higher than 60% in some countries3 (Table 1). This high proportion of cephalosporin resistance means that treatment for severe K. pneumoniae infections have to rely on carbapenems.
The first K. pneumoniae producing an enzyme (carbapenemase) capable of hydrolysing all beta-lactams, including the carbapenems, was identified in the USA in 1996. Since then, carbapenem-resistant K. pneumoniae rapidly emerged as a cause of multidrug-resistant infections worldwide. The WHO showed alarming rates of carbapenem resistance in K. pneumoniae, exceeding 50% in some countries of Eastern Mediterranean and Europe.3 In 2013, EARS-Net reported that the most affected countries in Europe were Greece and Italy with a percentage of carbapenem resistance of 59.4% and 34.3%, respectively.35 Very few therapeutic options remain to treat infections due to carbapenemase-resistant K. pneumoniae, one being an old and rather toxic antibiotic, colistin. However, a recent Italian study showed that among 178K. pneumoniae carbapenemase-producing K. pneumoniae isolates from different hospitals, 43% were also resistant to colistin.49 Infection control and interventions targetted to prevent the dissemination of these almost untreatable pathogens are highly needed.
Development of drug resistance in tuberculosis
The emergence and spread of multidrug-resistant strains of Mycobacterium tuberculosis (MDR-TB) represent one of the most daunting challenges to disease control worldwide. Incorrect treatment, consisting in prescription errors, low patient compliance, or poor quality of drugs, is the main cause for the development of resistant TB.50 The development of resistance to anti-TB drugs began shortly after the initial introduction of drugs to treat TB; MDR-TB is defined as TB caused by a multidrug-resistant strain, that is strain resistant to rifampicin and isoniazid. In MDR-TB, the number of drugs necessary for treatment is higher than in non-MDR-TB, the treatment outcome is less favourable and mortality is higher.51
In 2012, the estimated global burden of MDR-TB was of 450 000 cases, of whom 300 000 were incident cases. Globally, almost 4% of all new TB cases and more than 20% of those with previous history of TB treatment are estimated to be MDR-TB.50
Table 2 shows the number of TB and MDR-TB cases notified in the years 2011–2013 in the six WHO regions.52,53 Europe, South-east Asian and Africa are the regions with the highest number of MDR-TB cases since over 50% of the global MDR-TB cases in 2012 occurred in the Russian Federation, India and South Africa,3 respectively.
Table 2.
Number of notified TB and multidrug-resistant strains of M. tuberculosis (MDR-TB) cases and ratio between MDR-TB and TB cases in the six World Health Organization (WHO) world regions. The data are derived from WHO52
| 2011 | 2012 | 2013 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WHO regions | Populationa | No. of TB cases | No. of MDR-TB cases | MDR-TB/TB cases (%) | No. of TB cases | No. of MDR-TB cases | MDR-TB/TB cases (%) | No. of TB cases | No. of MDR-TB cases | MDR-TB/TB cases (%) |
| Africa region | 755 424 976 | 1 468 455 | 12 390 | 0.8 | 1 422 655 | 18 156 | 1.3 | 1 387 929 | 13 531 | 1.0 |
| Region of the Americas | 884 408 678 | 234 488 | 3475 | 1.5 | 233 985 | 2967 | 1.3 | 233 083 | 2961 | 1.3 |
| Eastern Mediterranean region | 529 821 657 | 418 238 | 835 | 0.2 | 421 865 | 2246 | 0.5 | 448 633 | 2923 | 0.7 |
| European region | 885 342 838 | 383 577 | 34 184 | 8.9 | 365 282 | 36 877 | 10.1 | 360 783 | 39 540 | 11.1 |
| South-East Asia region | 1 696 547 103 | 2 358 127 | 6615 | 0.3 | 2 331 455 | 19 202 | 0.8 | 2 297 033 | 28 618 | 1.2 |
| Western Pacific region | 1 750 811 276 | 1 387 741 | 4394 | 0.3 | 1 410 835 | 5749 | 0.4 | 1 375 213 | 5908 | 0.4 |
Population data refer to the year 2005.53
Extensively drug-resistant TB (XDR-TB) is defined as TB caused by an MDR strain that is also resistant to any fluoroquinolone and to any of the second-line injectable drugs (capreomycin, kanamycin, or amikacin). The first XDR-TB cases were described in 2006; in 2012, XDR-TB cases were reported from 92 countries. It is estimated that 9.6% of MDR-TB cases are indeed XDR-TB.
The only measure to reduce the burden of patients with XDR-TB is appropriate treatment of patients with MDR-TB.54 Therefore, the identification of new and effective drugs to fight resistant strains of M. tuberculosis is of the outmost importance. The introduction of bedaquiline for treatment of MDR-TB is a first step towards this end.51
Concluding remarks
Antimicrobial resistance is now recognized by the scientific community, the society at large and most policy-makers as an important problem to confront.
The WHO global report on surveillance of AMR, providing for the first time a global picture of the magnitude of AMR, also reveals the lack of adequate surveillance in many parts of the world and large gaps in information on microbes of major public health importance that preclude an accurate analysis of the real situation and of trends over time.
It is critical to strengthen and harmonise the AMR surveillance through the development of agreed epidemiological and microbiological methods, the adoption of common definitions to enhance the ability to share and compare resistance information, and to attain a better coordination of the surveillance networks.
With this aim, the WHO regional office for Europe (EURO) supports a new project (CAESAR-Central Asian and Eastern European Surveillance of Antimicrobial Resistance) to develop a network of national surveillance systems in the countries of the region that are not part of the EU and do not participate to EARS-Net, facilitating comparison of data throughout the entire European region.55
Different but coordinated strategies against AMR should be implemented, considering the type of pathogen (human or zoonotic), the setting in which it spreads (hospital or the community) and possible other specific factors contributing to the emergence of resistance. A special case is represented by the strategy against the development of MDR-TB, for which the only prevention is the improvement of treatment compliance in patients with susceptible TB.
In the hospital setting, infection control measures and antimicrobial stewardship programmes – administered by multidisciplinary teams of experts such as infectious diseases physicians, clinical pharmacists, clinical microbiologists, etc. – are very important to prevent emergence and transmission of antimicrobial-resistant microorganisms and ensuring the efficacy of available antimicrobials.56–58
Antimicrobial stewardship needs to be extended also to family doctors in the community, where there is a great consumption of antibiotics. The actions needed to reduce antibiotic misuse and inappropriate antibiotic prescriptions should consider: information campaigns for the consumers, information and training for the healthcare professionals, improved diagnostics for treatment decisions, treatment guidelines, and prescription audits.59
In veterinary medicine, the urgent need to take action for monitoring the antimicrobials use in food animals was stressed during the 2011 World Health Day. The interventions required consist in enforcing regulations governing the use of antimicrobials in food-producing animals, strengthening surveillance and monitoring, and reducing the need for antimicrobials through better animal husbandry.2
In January 2015, European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA) and European Medicines Agency (EMA) published for the first time a joint report on the integrated analysis of the consumption of antimicrobials and AMR in bacteria from human beings and food-producing animals. This is a very important signal for a coordinated surveillance, although several limitations in carrying out this type of analysis have been identified.60
In addition, innovative approaches are needed for the development of new antibiotics and other products to limit AMR. There is a shortage of new antibiotics in the pipeline and few incentives for industry to invest in research and development in this field. Only two novel classes of antibiotics have been marketed over the past 30 years (oxazolidinones and cyclic lipopeptides)2 but both these molecules target Gram-positive pathogens. There are very few effective drugs to treat multidrug-resistant infections due to Gram-negative bacteria that represent the main threat at present. The introduction of new vaccines may reduce the prevalence of infectious diseases and thereby reduce the need for antibiotics. For example, the introduction of the pneumococcal conjugate vaccines has led to the reduction in resistant Streptococcus pneumoniae not only in the vaccinated population but also in the population as a whole.61,62 The development of rapid point-of-care diagnostic tools may be of use to reduce clinical uncertainty, to save unnecessary antibiotic treatments, and to select effective antibiotics where resistance has rendered first-line treatment ineffective.63 The recent discovery of a new antibiotic called teixobactin, with excellent activity against Gram-positive pathogens, including drug-resistant strains, represents a hope for the future and an example for new researches.64
Disclaimer Statements
Contributors All named authors contributed to this article.
Funding None.
Conflicts of interest The authors declare they have no competing interest.
Ethics approval Ethical approval not required.
References
- 1.World Health Organization WHO global strategy for containment of antimicrobial resistance. Geneva: WHO; 2001. [Google Scholar]
- 2.World Health Organization The evolving threat of antimicrobial resistance. Options for action. Geneva: WHO Library Cataloguing-in-Publication Data; 2012. [Google Scholar]
- 3.World Health Organization Antimicrobial resistance: global report on surveillance 2014. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 4.Centres for Disease Control and Prevention, US Department of Health and Human Services. Antibiotic resistance threats in the United States. Atlanta: CDC; 2013. Available from: http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf [Google Scholar]
- 5.ECDC/EMEA The bacterial challenge: time to react. Stockholm: European Center for Disease Prevention and Control; 2009. [Google Scholar]
- 6.Nesher L, Rolston KV. The current spectrum of infection in cancer patients with chemotherapy related neutropenia. Infection. 2014;42(1):5–13. [DOI] [PubMed] [Google Scholar]
- 7.Kawecki D, Pacholczyk M, Lagiewska B, Sawicka-Grzelak A, Durlik M, Mlynarczyk G, et al. Bacterial and fungal infections in the early post-transplantation period after liver transplantation: etiologic agents and their susceptibility. Transplant Proc. 2014;46(8):2777–81. [DOI] [PubMed] [Google Scholar]
- 8.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel SJ, Saiman L. Antibiotic resistance in neonatal intensive care unit pathogens: mechanisms, clinical impact, and prevention including antibiotic stewardship. Clin Perinatol. 2010;37(3):547–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vincent J. Nosocomial infections in adult intensive-care units. Lancet. 2003;361(9374):2068–77. [DOI] [PubMed] [Google Scholar]
- 11.European Centre for Disease Prevention and Control Surveillance of antimicrobial consumption in Europe 2012. Stockholm: ECDC; 2014. Available from: http://ecdc.europa.eu/en/publications/Publications/antimicrobial-consumption-europe-esac-net-2012.pdf. [Google Scholar]
- 12.Suetens C, Hopkins S, Kolman J, Diaz Högberg L. Point prevalence survey of healthcare associated infections and antimicrobial use in European acute care hospitals. Stockholm, Sweden: European Centre for Disease Prevention and Control; 2013. [Google Scholar]
- 13.Hicks LA, Taylor TH Jr, Hunkler RJ. US outpatient antibiotic prescribing, 2010. N Engl J Med. 2013;368(15):1461–2. [DOI] [PubMed] [Google Scholar]
- 14.Polk RE. Variability in rates of Use of antibacterials among 130 US hospitals and risk-adjustment models for interhospital comparison. Infect Control Hosp Epidemiol. 2008;29(3):203–11. [DOI] [PubMed] [Google Scholar]
- 15.Ibrahim OM, Polk RE. Benchmarking antimicrobial drug use in hospitals. Expert Rev Anti Infect Ther. 2012;10(4):445–57. [DOI] [PubMed] [Google Scholar]
- 16.Special Eurobarometer 338 Antimicrobial resistance, November-December 2009. Brussels: TNS Opinion & Social; 2010. [Google Scholar]
- 17.McNulty CA, Boyle P, Nichols T, Clappison P, Davey P. Don't wear me out - the public's knowledge of and attitudes to antibiotic use. J Antimicrob Chemother. 2007;59(4):727–38. [DOI] [PubMed] [Google Scholar]
- 18.Andre M, Vernby A, Berg J, Lundborg CS. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother. 2010;65(6):1292–6. [DOI] [PubMed] [Google Scholar]
- 19.Morgan DJ, Okeke IN, Laxminarayan R, Perencevich EN, Weisenberg S. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. 2011;11(9):692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marshall BM, Levy SB. Food animals and antimicrobials: impacts on human health. Clin Microbiol Rev. 2011;24(4):718–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Safety Ef, editor. Regulation European. Ban on antibiotics as growth promoters in animal feed enters into effect (1831/2003/EC). Brussels: Europa; 2005. [Google Scholar]
- 22.European Medicines Agency (EMA) Sales of veterinary antimicrobial agents in 26 EU/EEA countries in 2012 Fourth ESVAC report. 2014. (EMA/333921/2014). Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2014/10/WC500175671.pdf. [Google Scholar]
- 23.Food and Drug Administration (FDA) Department of Health and Human Services Summary report on antimicrobials sold or distributed for use in food-producing animals. Silver Spring, MD: FDA; 2014. [Google Scholar]
- 24.Stockwell VO, Duffy B. Use of antibiotics in plant agriculture. Rev Sci Tech. 2012;31(1):199–210. [DOI] [PubMed] [Google Scholar]
- 25.Bouki C, Venieri D, Diamadopoulos E. Detection and fate of antibiotic resistant bacteria in wastewater treatment plants: a review. Ecotoxicol Environ Saf. 2013;91:1–9. [DOI] [PubMed] [Google Scholar]
- 26.Novo A, Andre S, Viana P, Nunes OC, Manaia CM. Antibiotic resistance, antimicrobial residues and bacterial community composition in urban wastewater. Water Res. 2013;47(5):1875–87. [DOI] [PubMed] [Google Scholar]
- 27.Kaye KS, Engemann JJ, Fraimow HS, Abrutyn E. Pathogens resistant to antimicrobial agents: epidemiology, molecular mechanisms, and clinical management. Infect Dis Clin North Am. 2004;18(3):467–511,viii. [DOI] [PubMed] [Google Scholar]
- 28.Chen LF, Chopra T, Kaye KS. Pathogens resistant to antibacterial agents. Infect Dis Clin North Am. 2009;23(4):817–45. [DOI] [PubMed] [Google Scholar]
- 29.Kalra L, Camacho F, Whitener CJ, Du P, Miller M, Zalonis C, et al. Risk of methicillin-resistant Staphylococcus aureus surgical site infection in patients with nasal MRSA colonization. Am J Infect Control. 2013;41(12):1253–7. [DOI] [PubMed] [Google Scholar]
- 30.Lombardi S, Scutell M, Felice V, Di Campli E, Di Giulio M, Cellini L. Central vascular catheter infections in a Hospital of Central Italy. New Microbiol. 2014;37(1):41–50. [PubMed] [Google Scholar]
- 31.Chambers HF, Deleo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009;7(9):629–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laupland KB, Church DL. Population-based epidemiology and microbiology of community-onset bloodstream infections. Clin Microbiol Rev. 2014;27(4):647–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Methicillin-Resistant Staphylococcus aureus, 2011. Available from: http://www.cdc.gov/abcs/reports-findings/survreports/mrsa11.pdf2011. [Google Scholar]
- 34.Dantes R, Mu Y, Belflower R, Aragon D, Dumyati G, Harrison LH, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med. 2013;173(21):1970–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.European Centre for Disease Prevention and Control (ECDC) Antimicrobial resistance surveillance in Europe 2013. Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Stockholm: ECDC; 2014. Available from: http://ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-surveillance-europe-2013.pdf. [Google Scholar]
- 36.Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O'Brien SJ, et al. The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis. 2010;50(6):882–89. [DOI] [PubMed] [Google Scholar]
- 37.Malathi V, Revathi K, Devaraj SN. Antimicrobial resistance an interface between animal and human diseases. Indian J Vet Anim Sci Res. 2020;43(2):113–4. [Google Scholar]
- 38.Oliver SP, Murinda SE, Jayarao BM. Impact of antibiotic use in adult dairy cows on antimicrobial resistance of veterinary and human pathogens: a comprehensive review. Foodborne Pathog Dis. 2011;8(3):337–55. [DOI] [PubMed] [Google Scholar]
- 39.Al-Dawodi R, Farraj MA, Essawi T. Antimicrobial resistance in non-typhi Salmonella enterica isolated from humans and poultry in Palestine. J Infect Dev Ctries. 2012;6(2):132–6. [DOI] [PubMed] [Google Scholar]
- 40.Mather AE, Reid SW, Maskell DJ, Parkhill J, Fookes MC, Harris SR, et al. Distinguishable epidemics of multidrug-resistant Salmonella Typhimurium DT104 in different hosts. Science. 2013;341(6153):1514–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li Y, Xie X, Xu X, Wang X, Chang H, Wang C, et al. Nontyphoidal salmonella infection in children with acute gastroenteritis: prevalence, serotypes, and antimicrobial resistance in Shanghai, China. Foodborne Pathog Dis. 2014;11(3):200–6. [DOI] [PubMed] [Google Scholar]
- 42.Najafi M, Lemon SM, Knobler SL, Burroughs T. The resistance phenomenon in microbes and infectious disease vectors: implications for human health and strategies for containment – workshop summary. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 43.Tamang MD, Nam HM, Kim TS, Jang GC, Jung SC, Lim SK. Emergence of extended-spectrum beta-lactamase (CTX-M-15 and CTX-M-14)-producing nontyphoid Salmonella with reduced susceptibility to ciprofloxacin among food animals and humans in Korea. J Clin Microbiol. 2011;49(7):2671–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aarestrup FM, Wiuff C, Molbak K, Threlfall EJ. Is it time to change fluoroquinolone breakpoints for Salmonella spp.? Antimicrob Agents Chemother. 2003;47(2):827–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viale P, Giannella M, Lewis R, Trecarichi EM, Petrosillo N, Tumbarello M. Predictors of mortality in multidrug-resistant Klebsiella pneumoniae bloodstream infections. Expert Rev Anti Infect Ther. 2013;11(10):1053–63. [DOI] [PubMed] [Google Scholar]
- 46.Li D, Chen Y, Zhang W, Zheng S, Zhang Q, Bai C, et al. Risk factors for hospital-acquired bloodstream infections caused by extended-spectrum β-lactamase Klebsiella pneumoniae among cancer patients. Ir J Med Sci. 2013;182:1–7. [DOI] [PubMed] [Google Scholar]
- 47.Webster DP, Young BC, Morton R, Collyer D, Batchelor B, Turton JF, et al. Impact of a clonal outbreak of extended-spectrum beta-lactamase-producing Klebsiella pneumoniae in the development and evolution of bloodstream infections by K. pneumoniae and Escherichia coli: an 11 year experience in Oxfordshire, UK. J Antimicrob Chemother. 2011;66(9):2126–35. [DOI] [PubMed] [Google Scholar]
- 48.Delgado-Valverde M, Sojo-Dorado J, Pascual A, Rodriguez-Bano J. Clinical management of infections caused by multidrug-resistant Enterobacteriaceae. Ther Adv Infect Dis. 2013;1(2):49–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Monaco M, Giani T, Raffone M, Arena F, Garcia-Fernandez A, Pollini S, et al. Colistin resistance superimposed to endemic carbapenem-resistant Klebsiella pneumoniae: a rapidly evolving problem in Italy, Novemberto April 2014. Euro Surveill. 2013;19(42):20939. [DOI] [PubMed] [Google Scholar]
- 50.Matteelli A, Roggi A, Carvalho AC. Extensively drug-resistant tuberculosis: epidemiology and management. Clin Epidemiol. 2014;6:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization The use of bedaquiline in the treatment of multidrug-resistant tuberculosis: interim policy guidance. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 52.World Health Organization (WHO) Indicators of diagnosis, notification and treatment of multidrug-resistant TB, by region or country and year. Available from: https://extranet.who.int/sree/Reports?op=vs&path=/WHO_HQ_Reports/G2/PROD/EXT/MDRTB_Indicators_charts (accessed 2 February 2015). [Google Scholar]
- 53.World Health Organization (WHO) Population, death rates, and reproductive rates. Available from: http://www.who.int/choice/demography/pop_death_rates/en/. [Google Scholar]
- 54.Chang K, Yew W. Management of difficult multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis: update 2012. Respirology. 2013;18(1):8–21. [DOI] [PubMed] [Google Scholar]
- 55.WHO Regional Office for Europe Central Asian and Eastern European Surveillance on Antimicrobial Resistance (CAESAR). Available from: http://www.euro.who.int/en/health-topics/disease-prevention/antimicrobial-resistance/antimicrobial-resistance/central-asian-and-eastern-european-surveillance-on-antimicrobial-resistance-caesar (accessed 11 February 2015). [Google Scholar]
- 56.Carlet J, Jarlier V, Harbarth S, Voss A, Goossens H, Pittet D. Ready for a world without antibiotics? The pensières antibiotic resistance call to action. Antimicrob Resist Infect Control. 2012;1(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Flanagan M, Ramanujam R, Sutherland J, Vaughn T, Diekema D, Doebbeling BN. Development and validation of measures to assess prevention and control of AMR in hospitals. Med Care. 2007;45(6):537–44. [DOI] [PubMed] [Google Scholar]
- 58.MacDougall C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18(4):638–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rawlins M, McKenzie D, Mar CD. Antimicrobial stewardship: what's it all about? Aust Presc. 2020;36(4):116–3. [Google Scholar]
- 60.ECDC (European Centre for Disease Prevention and Control), EFSA (European Food Safety Authority) and EMA (European Medicines Agency) ECDC/EFSA/EMA first joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals. EFSA J. 2015;13(1):4006–4114, [Stockholm/Parma/London: ECDC/EFSA/EMA, 2015]. [Google Scholar]
- 61.Talbot TR, Poehling KA, Hartert TV, Arbogast PG, Halasa NB, Mitchel E, et al. Reduction in high rates of antibiotic-nonsusceptible invasive pneumococcal disease in tennessee after introduction of the pneumococcal conjugate vaccine. Clin Infect Dis. 2004;39(5):641–48. [DOI] [PubMed] [Google Scholar]
- 62.Kaplan SL, Mason EO, Wald ER, Schutze GE, Bradley JS, Tan TQ, et al. Decrease of invasive pneumococcal infections in children among 8 children's hospitals in the United States after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatrics. 2004;113(3):443–49. [DOI] [PubMed] [Google Scholar]
- 63.Howard SJ, Catchpole M, Watson J, Davies SC. Antibiotic resistance: global response needed. Lancet Infect Dis. 2013;13(12):1001–03. [DOI] [PubMed] [Google Scholar]
- 64.Ling LL, Schneider T, Peoples AJ, Spoering AL, Engels I, Conlon BP, et al. A new antibiotic kills pathogens without detectable resistance. Nature. 2015;517(7535):455–9. [DOI] [PMC free article] [PubMed] [Google Scholar]