Abstract
Background
There is considerable interest in determining whether mass drug administration (MDA) with ivermectin for onchocerciasis control will eliminate coendemic lymphatic filariasis (LF). The objective of this study was to determine the prevalence of LF microfilaremia in onchocerciasis endemic districts that had received 7 years of MDA with ivermectin.
Method
Three villages with a 2010 LF circulating antigenaemia prevalence (determined in a mapping exercise using immunochromatography tests) ranging from 23 to 56% were surveyed for the presence of Wuchereria bancrofti microfilaria (mf) in 2012. These villages had been treated with ivermectin MDA for onchocerciasis with reported total population coverage of ≥65%. A total of 774 residents aged 2 years and above, of both genders, provided 60 μl nocturnal blood samples between 10 pm and 2 am. Standard thick smears were prepared and examined microscopically after Giemsa staining for the presence of W. bancrofti mf.
Results
The mean mf prevalence was 4.7% (village range 1.1–11.0%). The mean mf density was 9.8 mf/60 μl (village range 9–13.1) among the positive individuals. Children in the 2–4-year-old and 5–9-year-old age groups were infected suggesting transmission occurred during the MDA period. A village level review of MDA treatment coverage records showed an average total population coverage of 66.4% over a 7-year period, but with a considerable range of annual coverage (43.0–89.9%). In addition, village level treatment coverage data were missing from the village with the highest mf prevalence (11%) for 2 of the 7 years.
Conclusion
7 years of annual mass treatment with ivermectin monotherapy for onchocerciasis did not interrupt LF transmission. In expanding the onchocerciasis ivermectin MDA programme to include LF, albendazole should be added and treatment coverage improved.
Keywords: Lymphatic filariasis, Onchocerciasis, Annual MDA, Ivermectin, Elimination
Introduction
Lymphatic filariasis (LF) and onchocerciasis are two of five preventive chemotherapy-neglected tropical diseases.1 LF is caused by three species of nematode parasites (Wuchereria bancrofti, Brugia malayi and Brugia timori) and transmitted by several mosquito vectors, including certain species of Anopheles, Culex and Aedes. Globally, it is estimated that 40 million people are disfigured or incapacitated by LF-related hydrocele, lymphoedema and elephantiasis.2,3 About 1.2 billion people worldwide are at risk for LF, and 35 African countries are affected. The main cause of LF infection in Africa is W. bancrofti, usually transmitted on the continent by Anopheles. The approach to LF elimination in most of Africa is based on mass drug administration (MDA) using a combination of ivermectin (Mectizan®, donated by Merck & Co.), and albendazole (donated by GlaxoSmithKline).2,3 The threshold for launching MDA for LF ≥ 1% of prevalence (either nocturnal microfilaremia or antigenaemia) in an implementation unit.1–3 Between 2000 and 2013, a cumulative total of 4.9 billion doses of medicines have been delivered to 1 billion people at risk for LF infection. During the year 2013, the LF programme in Africa targeted 167 million people for MDA and treated 127 million for a reported coverage of 76.1%.2 It is estimated that with good annual treatment coverage (≥65% of total population) of combined ivermectin albendazole MDA, interruption of LF transmission in African can be attained in 4–6 years.3
It is estimated that 102 million people in Africa are at risk of onchocerciasis infections (river blindness).4,5 Ivermectin MDA, one or twice per year, is the strategy used to control disease, or eliminate transmission, of onchocerciasis. In sub-Saharan Africa, coendemicity of LF and onchocerciasis is geographically widespread,5,6 and most onchocerciasis-endemic areas that have been mapped for LF have been found to be coendemic for both conditions.6 The LF and onchocerciasis MDA programmes have been criticized for not working together more closely.5,6
LF and onchocerciasis are both endemic in Ethiopia.2,4,7−9 Considering the importance of LF–onchocerciasis coendemicity, Shifereaw et al. undertook a large mapping exercise from 2008 to 2010 in order to determine LF endemicity in and around onchocerciasis-endemic zones where ivermectin MDA was being delivered.10 Activities generated by the results of the Shifereaw study form the basis for the current report, which seeks to answer the important question of whether ivermectin monotherapy MDA for onchocerciasis control has inadvertently eliminated LF transmission. If this were the case, the LF programme would be freed, in vast areas, of the need to treat LF in onchocerciasis coendemic zones in Ethiopia. Studies by Kyelem et al. in Burkina Faso showed that an annual MDA with ivermectin for onchocerciasis reduced the prevalence of coendemic LF after 6 years, but did not eliminate its transmission.11 In another report by Kyelem suggested that biannual ivermectin MDA for onchocerciasis may have eliminated LF.12 Epidemiological and entomological studies carried out by Richards et al. in Nigeria showed that 7 years of annual MDA with ivermectin did not interrupt transmission of LF.13,14
The objective of the present study was to determine if an annual MDA with ivermectin over a period of 7 years might have reduced W. bancrofti microfilaremia to below the critical <1% mf prevalence threshold, signalling likely LF transmission interruption.
Methods
The original purpose of this field work was to collect baseline nocturnal microfilarial prevalence in potential LF sentinel villages in districts where LF antigen prevalence was ≥1% in the Shifereaw et al. study. This was in accord with WHO guidelines for districts eligible for LF MDA, as sentinel village ‘baseline’ LF microfilaria prevalence is needed to monitor progress towards LF elimination.15,16 The sentinel village nocturnal blood follow-up surveys gave us an opportunity to observe the impact of onchocerciasis MDA on LF microfilaremia as compared to very high baseline mapping LF antigen prevalence.
Study site selection
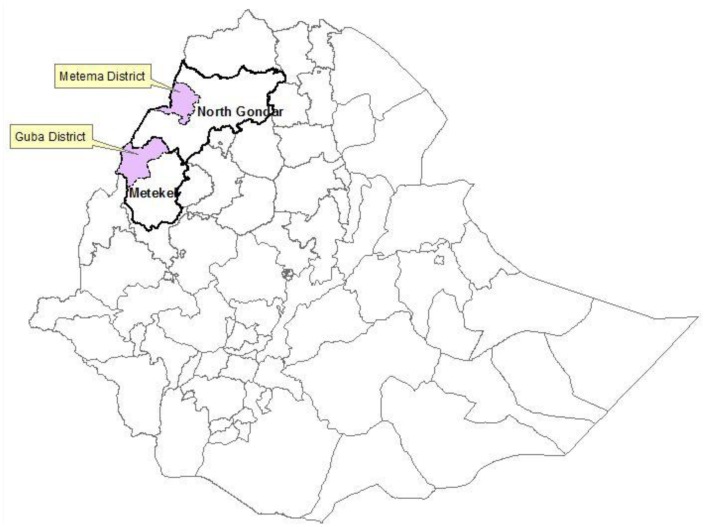
The survey sites were in Metema district (woreda) in North Gondar zone of the Amhara Region, and in Guba district in the Metekel zone of Benishangul-Gumuz Region (Fig. 1). Both districts had received ivermectin MDA for onchocerciasis for a period of 7 years prior to the follow-up survey. Two villages in Guba district (Fanguso and Omedilla) and one in Metema district (Tumet) were selected as potentail sentinel villages for LF due to their high circulating filarial antigen levels as determined on finger-stick blood using ICT (Binax NOW® Binax Inc. Scarborough, Maine, USA) with methods described by Shifereaw et al.9,17 Two villages in Guba District were tested based on somewhat modified sampling procedures from the WHO Operational Guidelines for Mapping of Bancroftian Filariasis in Africa.18 In each district (woreda), the mapping study aimed to test 100 individuals for W. bancrofti antigenaemia. Approximately, 30 households per village with 160–200 people were randomly selected and their occupants were invited to participate. If the number of occupants in the households selected was too small to provide a sample of 100 (as was the case with Omedilla village), an additional village in the same district was selected (in this case Fanguso village in Guba district) and the exercise was repeated there to complete the 100 person sample.
Figure 1.
Map of Ethiopia showing the study areas of Guba and Metema districts.
The mean antigen rate for the three villages was 39% (range 23–56%, Table 1). The two villages in Guba district (Fanguso and Omedilla) had about twice the rates (mean antigen 55%) of Tumet village in Metema (23%) (χ2(Corrected) = 0.1976, p < 0.01). The Ethiopian programme made the decision that it would be preferable to visit both these villages to evaluate each as potential LF sentinels due to these high baseline antigen levels, even though one of these (Omedilla) had a population smaller than the WHO recommended 500. This was because the programme sought a sentinel village for the district where the baseline nocturnal microfilaria (mf) prevalence would be well above the 1% needed to monitor impact of the programme, regardless of population size.
Table 1.
Villages selected for detection of W. bancrofti microfilariae based on 2010 ICT results
| Zone | District | Village | ICT Tested 2008 | ICT pos (%) |
|---|---|---|---|---|
| Metekel | Guba | Fanguso | 50 | 28 (56%) |
| Omedilla | 50 | 27 (54%) | ||
| Guba total | 100 | 55 (55%) | ||
| North Gondar | Metema | Tumet | 100 | 23 (23%) |
| Overall total | 200 | 78 (39%) |
Onchocerciasis treatment
MDA had been carried out using the community-directed treatment with ivermectin (CDTI) approach19 in Guba and Metema districts from 2005 to 2011. Treatment data for the three surveyed villages were obtained from programme records kept at the village and district level. Coverage (shown in Table 2) was calculated for both the eligible population, which excludes children <5 years of age, and for the total population, living the village.20 The records kept at village level were compiled yearly from community household treatment registers. The population to be treated, however, varied considerably between years due to agricultural migratory events. Therefore, we were unable to distinguish the ‘resident’ coverage from the ‘visitor’ coverage. Records kept at district level often only documented that MDA took place (e.g. did not always have individual village treatment coverage figures). Of particular concern was missing 2005 and 2008 treatment information for Omedilla at the village level, although district level records indicated that treatment had occurred, but without information on treatment coverage figures.
Table 2.
Reported MDA treatment coverage with Ivermectin in three villages in Guba and Metema districts (2005–2011)
| District | Village | Year | Treated Population | Total Population | % Total Population | Eligible Population | % Eligible Population |
|---|---|---|---|---|---|---|---|
| Guba | Fanguso | 2005 | 623 | 1164 | 53.5% | 978 | 63.7% |
| 2006 | 623 | 1161 | 53.7% | 977 | 60.0% | ||
| 2007 | 621 | 962 | 64.6% | 808 | 80.0% | ||
| 2008 | 895 | 1223 | 73.2% | 1027 | 87.0% | ||
| 2009 | 852 | 1269 | 67.1% | 1066 | 80.0% | ||
| 2010 | 387 | 648 | 59.7% | 544 | 70.0% | ||
| 2011 | 796 | 1062 | 75.0% | 892 | 90.0% | ||
| Average Interval | 63.8% | 75.8% | |||||
| Omedilla | 2005 | NA | NA | NA | NA | NA | |
| 2006 | 90 | 158 | 57.0% | 133 | 67.8% | ||
| 2007 | 68 | 158 | 43.0% | 133 | 50.0% | ||
| 2008 | NA | NA | NA | NA | NA | ||
| 2009 | 149 | 166 | 89.8% | 140 | 100.0% | ||
| 2010 | 174 | 267 | 65.2% | 224 | 70.0% | ||
| 2011 | 278 | 326 | 85.3% | 274 | 100.0% | ||
| Average Interval | 68.0% | 77.6% | |||||
| Metema | Tumet | 2005 | 2284 | 3524 | 64.8% | 2960 | 77.2% |
| 2006 | 3016 | 4346 | 69.4% | 3651 | 82.6% | ||
| 2007 | 2536 | 3674 | 69.0% | 3086 | 82.2% | ||
| 2008 | 2433 | 4867 | 50.0% | 4088 | 59.5% | ||
| 2009 | 3875 | 5157 | 75.1% | 4332 | 89.5% | ||
| 2010 | 4090 | 5867 | 69.7% | 4928 | 83.0% | ||
| 2011 | 3411 | 4572 | 74.6% | 3840 | 88.8% | ||
| Average Interval | 67.5% | 80.4% | |||||
| Overall Treatment Coverage | 66.5% | 77.9% |
We considered acceptable treatment coverage to be ≥65% of the total population per year. We summarized the MDA treatment coverage by calculating a 7-year average ‘interval coverage’ (the sum of the mean reported treatment coverage for each year divided by 7 multiplied by 100). Because we were unable to document at district level that treatments had taken place for all 7 years in Omedilla, we used the sum of the reported treatment coverage for each year divided by 5 multiplied by 100 as an estimate for the 7-year average interval coverage. The assumption was that the 5-year mean would be representative of the MDA coverage in 2005 and 2008.
Nocturnal microfilaremia survey
The blood survey was conducted in 2012 using the convenience sample methodology (e.g. not randomized) in residents ≥2 years of age. We revisited three villages discovered by Shifereaw et al. to have high LF antigenaemia in an onchocerciasis coendemic area of Ethiopia. Residents were defined as children under 5 who had spent their entire lives in the community, and older persons who had lived in the communities for at least 5 years. The survey was conducted 11 months after the last ivermectin MDA treatment round so as to allow for maximum likely mf prevalence (e.g. the nadir of the MDA effect). The survey did not include seasonal migratory workers or visitors since their infection status might not provide information about recent transmission in the surveyed population.
After explaining the purpose of the survey, between 10:00 pm and 2:00 am, participants of both genders were registered and oral consent obtained from adults and assent from parents of minors. Using sterile lancets, 60 μl of blood by finger prick was obtained in non-heparinaized capillary tubes. Seven hundred and seventy-four persons participated in the nocturnal blood surveys. The blood was placed on a microscope slide in a standard thick blood smear preparation and allowed to air dry. At The Carter Center’s laboratory in Addis Ababa, the dried smears were dehaemoglobinized, dried, fixed in methanol and stained in 3% Giemsa for 45 min. The stained slides were examined by trained laboratory technicians using light microscopy for the presence of W. bancrofti mf and all mf on positive slides were counted. For quality control, all positive slides and 10% of negative slides were confirmed by a second microscopist.
Ethical approval
Ethical approval for the survey was provided by the Ethiopian National Ethical Review Committee of the Ministry of Ethiopian Science and Technology. The Institutional Ethics Review Boards of the Faculty of Medicine and Addis Ababa University also reviewed the protocol, as well as the Emory Institutional Review Board, which classified the assessment activities as programme performance assessment (‘non-research’). On several occasions prior to the surveys, community-wide meetings that included community leaders were held to explain the purpose of the survey. The meetings, which included health education messages, were conducted by the study team together with the zonal, district and community health staff. In these meetings, it was made clear that participation was voluntary and anyone was free to opt out of the study without fear of repercussions.
Data analysis
Data were analyzed in Microsoft Excel® and SPSS version 15.0 (SPSS. Chicago IL, USA). The average MDA interval coverage was calculated as described above. The mf prevalence was calculated as the number of W. bancrofti mf slide positives divided by the number of persons examined multiplied times 100, and results were expressed both by age group and gender. The overall prevalence was not age gender adjusted. Mean microfilaria density per 60 μl among infected persons was expressed as the sum of all mf counted on all positive slides divided by the number of positive individuals. To compare prevalence data between age groups, the Pearson chi-square – χ2 test was used with P values < 0.05 considered significant. The binomial exact confidence interval (CI) calculation was used to determine 95% CI.
Results
MDA Coverage
Over the 7-year treatment interval, the average interval coverage of the total population was 66.5%, and the average interval coverage of the eligible population was 70.5% (Table 2). The highest average coverage for total population was in Omedilla (68.0%), while the highest average eligible population coverage was in Tumet (80.4%). In Fanguso, the average treatment coverage over the 7-year period was 63.8% (range 53.5–75%) for the total population and 75.8% (ranged 60–90%) for the eligible. For Tumet, the total population average coverage was 67.5% (range 64.8–75.1%) and eligible 80.4% (range 59.5–89.5%). In Omedilla, the average for 5 years (excluding 2005 and 2008 when treatment was given but coverage was unknown) was 68.0% (range 43.0–85.3%) for the total population and 77.6% (range 67.8–100%) for the eligible population.
Microfilaremia (mf) prevalence and Mf density
The overall mean mf prevalence (Table 3) was 4.7% among the 774 persons (range 1.1–11.0%, 95% CI, 3.27–6.37%). Tumet (with a baseline 2010 LF antigen of 23%) had the lowest 2012 mf prevalence of 1.1% (95% CI, 0.29–2.74%). Fanguso (baseline LF antigen 56%) had an mf prevalence of 6.8% (95% CI, 4.19–10.28%), significantly higher than Tumet (p < 0.05). Omedilla village, with a baseline LF antigen similar to Fanguso (54%), and the highest total population average treatment coverage (68.0%) had the highest mf prevalence 11.0% (95% CI, 5.82–18.44%). Omedilla’s mf prevalence was higher than Tumet (p < 0.05%), but not statistically significantly different from Fanguso.
Table 3.
Blood microfilaria (mf) prevalence and microfilaria density in surveyed villages
| District | Village | Number of persons tested for mf | No. (%) positive for microfilaria | 95% Confidence Interval (CI) | microfilaria density/60 μl among positives cases |
|---|---|---|---|---|---|
| Metema | Tumet | 370 | 4 (1.1%) | 0.29–2.74 % | 9 |
| Guba | Fanguso | 295 | 20 (6.8%) | 4.19–10.28 % | 13.8 |
| Omedilla | 109 | 12 (11.0%) | 5.82–18.44 % | 6.6 | |
| Total | 774 | 36 (4.7%) | 3.27–6.37 % | 9.8 |
The overall mean mf density among infected persons was 9.8 mf/60 μl blood (Table 3). Fanguso (13.8 mf/60 μl) had the highest mf density, followed by Tumet (9 mf/60 μl) and Omedilla (6.6 mf/60 μl).
Gender-based mf prevalence
Table 4 shows the mf prevalence by gender and by seven age groups. Males (n = 365) did not have a significantly higher mf prevalence compared with females (n = 389) (4.15% compared to 5.14%, χ2 (corrected) = 0.2307, p = 0.631). When compared at village level (Table 4), the higher prevalence of female infections in Omedilla (16% vs. the 4% in males) almost reached statistical significance (Mantel-Haenzel χ2 3.8, p = 0.051).
Table 4.
Population examined and W. bancrofti microfilaria positive cases, by gender and age group
| 2-4yrs | 5-9yrs | 10-14yrs | 15-19yrs | 20-29yrs | 30-49yrs | 50+yrs | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Village | Gender | Examination | Positive | Examination | Positive | Examination | Positive | Examination | Positive | Examination | Positive | Examination | Positive | Examination | Positive | Examination | Positive |
| Tumet (n=371) | Male | 11 | 0 | 24 | 0 | 25 | 0 | 30 | 0 | 39 | 1 | 51 | 0 | 13 | 0 | 193 | 1 (0.5%) |
| Female | 10 | 0 | 36 | 1 | 26 | 0 | 8 | 0 | 57 | 1 | 29 | 1 | 11 | 0 | 177 | 3 (1.7%) | |
| Total | 21 | 0 (0%) | 60 | 1 (1.7%) | 51 | 0 (0%) | 38 | 0 (0%) | 96 | 2 (2.0%) | 80 | 1 (1.2%) | 24 | 0 (0%) | 370 | 4 (1.1%) | |
| Fanguso (n=295) | Male | 15 | 1 | 25 | 1 | 31 | 2 | 16 | 0 | 14 | 1 | 20 | 4 | 24 | 4 | 145 | 13 (9.0%) |
| Female | 12 | 0 | 31 | 2 | 23 | 0 | 12 | 0 | 24 | 0 | 35 | 2 | 13 | 3 | 150 | 7 (4.7%) | |
| Total | 27 | 1 (3.7%) | 56 | 3 (5.4%) | 54 | 2 (3.7%) | 28 | 0 (0%) | 38 | 1 (2.6%) | 55 | 6 (10.9%) | 37 | 7 (18.9%) | 295 | 20 (6.8%) | |
| Omedilla (n=109) | Male | 6 | 0 | 10 | 0 | 7 | 0 | 1 | 0 | 4 | 0 | 10 | 0 | 9 | 2 | 47 | 2 (4.3%) |
| Female | 5 | 0 | 17 | 4 | 8 | 3 | 2 | 0 | 13 | 1 | 6 | 1 | 11 | 1 | 62 | 10 (16.1%) | |
| 11 | 0 (0%) | 27 | 4 (1.5%) | 15 | 3 (20%) | 3 | 0 (0%) | 17 | 1 (5.9%) | 16 | 1 (6.3%) | 20 | 3 (15%) | 109 | 12 (11.0%) | ||
| Overall | Male | 32 | 1 | 59 | 1 | 63 | 2 | 47 | 0 | 57 | 2 | 81 | 4 | 46 | 6 | 385 | 16 (4.2%) |
| Female | 27 | 0 | 84 | 7 | 57 | 3 | 22 | 0 | 94 | 2 | 70 | 4 | 35 | 4 | 391 | 20 (5.1%) | |
| Overall | 59 | 1 (1.7%) | 143 | 8 (5.6%) | 120 | 5 (4.2%) | 69 | 0 (0.0%) | 151 | 4 (2.7%) | 151 | 8 (5.3%) | 81 | 10 (12.4%) | 774 | 36 (4.7%) |
Age group mf prevalence
Prevalence was greatest in the >50-year-old age group (12.4%) and lowest (0%) in the 15–19-year age group (Table 4). Infected children were detected in the 2–4-year-old age group (one child, 1.7%) and among 5–9-year olds (5.6%). The infected child in the 2–4-year age group was a 3-year-old boy in Fanguso, the village which had the best average treatment coverage of the eligible population (80.4%, range 59–88%). All three villages had children with microfilaremia in the 5–9-year age group, a likely indicator of recent LF transmission.
Discussion
There has been considerable interest in the LF community in determining if years of ivermectin MDA to control onchocerciasis could interrupt transmission of LF where these two conditions are coendemic.5,6,11–14 The results from this study in Ethiopia show that, despite 7 years of annual MDA with ivermectin for onchocerciasis, all three LF onchocerciasis coendemic communities had W. bancrofti microfilaremia exceeding the critical ≥1% prevalence threshold. This implies that LF transmission was not interrupted,21 and that these two districts should implement an LF MDA programme by adding albendazole to ivermectin for more effective combined therapy,15 and forgoing any consideration of undertaking LF transmission assessment surveys.21,22 However, it is difficult to draw conclusions about the effectiveness of onchocerciasis MDA against LF from this study because no village achieved more than three consecutive ‘effective’ MDA rounds where coverage was ≥65% (Table 2).
The finding of one resident child (a 3-year-old male) with mf in the 2–4-year-old age group in Fanguso village strongly suggests that transmission occurred within the 7-year ivermectin MDA period. While it could be argued that Fanguso only had four effective (≥65%) MDA rounds,22 three of these occurred during the 4-year period 2008–2011, which encompassed the lifespan of this child. In the 5–9-year age group, there were 8 (5.6%) infections among 143 children, with infections in this age group occurring in all three communities, including Tumet, which had 5 effective rounds (not including an additional ‘ineffective’ round of 64.8%). The child with the highest higher infection density (9 mf/60 μl) was in Tumet.
Some of the age- and sex-specific infection rates were surprising. First, there were no positive cases in the 15–19-year age group. This could have been due to a small number of persons in this age group participating in the survey compared to other adult age groups. The number tested (69) in the 15–19 age group was the second smallest, after the 2–4-year olds (59 tested), where one infection was found. Perhaps most important explanation for the low infection rate in the 15–19-year-old age group is that the village with the highest infection rate (Omedilla, with 11% overall prevalence) had only three persons (3% of that village’s sample) in that age group tested. This could have reduced the likelihood of finding microfiladermia in age category. Second was the higher prevalence of female infections in Omedilla (16% vs. 4% in males), a difference that almost reached statistical significance (p = 0.051). Reasons for this finding are unclear and warrant further investigation.
Omedilla, the village with the highest microfilaremia prevalence (11.0%), also had the highest average treatment coverage (68% of total population coverage), but only three MDA annual rounds were documented as being ≥65%, and there was no village-level documentation for MDA for 2005 and 2008. Because we found evidence at the district level that MDA had been delivered during those years, we decided to assume that the average coverage for 5 years was representative of the 7-year-treatment interval. It is important to note that if we had not made this assumption, and assumed instead that no MDA was delivered in 2005 and 2008, then Omedilla would have had the lowest interval treatment coverage (55.4% eligible and 48.6% total population). The ‘Omedilla uncertainty’ is a major limitation of this study. The need for better treatment records is a major recommendation from this experience. We also recommend periodic coverage surveys in order to validate reported coverage.23 Our results would have been strengthened if at least one coverage survey in Guba and Metema districts had been carried out during the MDA period.
Another limitation of the study was that it was not randomized, the subjects for nocturnal survey were self-selected and as such these ‘convenience sample’ results are subject to selection bias. People who voluntarily presented for night testing could possibly be those more likely to accept ivermectin during MDAs, which would result in underestimating the actual mf prevalence and density in the communities. The last limitation to mention is that the study was restricted to only permanent residents and so avoided inclusion of the seasonal migratory individuals, many of whom may or may not have been infected depending upon whether their origin was an LF or non-LF endemic areas. Future studies should consider randomization procedures, as well as determination of the extent to which the migratory labour force contributes to local LF transmission dynamics. It would be important to continue to include non-residents and visitors in the onchocerciasis/LF MDA programmes, as appears to be happening now given the fluctuations in treatment populations observed from year to year.
Interestingly, the vector for LF in Ethiopia is Anopheles gambiae, which have cibarial armature (‘teeth’) that destroy many ingested mf during a blood meal.24,25 As more mf are ingested by the mosquito, the cibarial armature’s effect decreases as mf debris accumulates on the teeth, and by masking them to allow other mf to enter the vector unharmed. Once inside the vector, they may develop into infective larvae.26 The presence of higher density mf carriers therefore favours LF transmission in Anopheles transmission zones. Therefore, our finding of individuals with relatively high mf counts is another piece of evidence that supports active local LF transmission in these villages. On the other hand, these vector infection dynamics also suggest that ivermectin treatment, which is primarily microfilaricidal,15 ought to have an impact on LF transmission simply by lowering mf counts. Of note is that in addition to ivermectin MDA from the onchocerciasis programme, the national scale up of long-lasting insecticidal bednets by the Ethiopian malaria programme may have worked in favour of reducing LF transmission in this area.27,28 Therefore, it was disappointing to find evidence of ongoing transmission in these three villages in Ethiopia.
Conclusion
Seven years of annual mass treatment with ivermectin alone, given for onchocerciasis control, did not interrupt LF transmission in three Ethiopian villages. This MDA failure may have been due to the inability of ivermectin monotherapy to break transmission, and/or to too few effective MDA rounds having been delivered. In coendemic areas for LF and onchocerciasis, albendazole should be given in combination with ivermectin as recommended for LF elimination by WHO. It is also imperative that these medicines be provided to the targeted populations at optimal coverage in every round of treatment. Good records and treatment coverage surveys are needed to document that such effective treatment coverage was attained.
Funding
Financial support for the LF nocturnal mf surveys was provided by The Carter Center. Partial financial support to onchocerciasis MDA was provided by Lions Clubs International Foundation and the African Programme for Onchocerciasis Control (APOC).
References
- 1.WHO Report Sustaining the drive to overcome the global impact of neglected tropical diseases. 2013; World Health Organization 20, Avenue Appia CH-1211 Geneva 27.
- 2.World Health Organization Global programme to eliminate lymphatic filariasis: progress report on mass drug administration in 2013. Wkly Epidemiol Rec. 2014;89:409–420.25243263 [Google Scholar]
- 3.WHO Report World Health Organization. Global program to eliminate Lymphatic filariasis. Progress report 2000-2009 and Strategic plan 2010-2020 “halfway towards eliminating LF…” WHO/HTM/NTD/PCT/2010.6.
- 4.World Health Organization African programme for onchocerciasis control—report of the national task forces, September 2012. Wkly Epidemiol Rec. 2012;87:493–508.23311004 [Google Scholar]
- 5.World Health Organization Meeting of the international task force for disease eradication January 2014 (Elimination of onchocerciasis and lymphatic filariasis in Africa). Wkly Epidemiol Rec. 2014;89:153–155.24754045 [Google Scholar]
- 6.Evans D, Unnasch T, Richards F. Onchocerciasis and lymphatic filariasis elimination in Africa: it’s about time. The Lancet. 2015;385:2151–2152. 10.1016/S0140-6736(15)61022-4 [DOI] [PubMed] [Google Scholar]
- 7.McConnell E, Schmidt LM. Bancrotian filariasis in Gambella, Illuababor Province, Ethiopia. Trop Geogr Med. 1973;25:300–303. [PubMed] [Google Scholar]
- 8.McConnell E, Asfaha W, Dennis W (1976). A survey of Wuchereria bancrofti in Ethiopia. Ethiop Med J. 1976;14:31–36. [PubMed] [Google Scholar]
- 9.Jemaneh L, Kebede D. Clinico-epidemiological study of lymphatic filariasis southwestern Ethiopia. Ethiop Med J. 1995;33:143–153. [PubMed] [Google Scholar]
- 10.Shiferaw W, Kebede T, Graves PM, Golasa L, Gebre T, Mosher Aryc W., et al. Lymphatic filariasis in western Ethiopia with special emphasis on prevalence of Wuchereria bancrofti antigenaemia in and around onchocerciasis endemic areas. Trans Roy Soc Trop Med Hyg. 2012;106:117–127. 10.1016/j.trstmh.2011.10.006 [DOI] [PubMed] [Google Scholar]
- 11.Kyelem D, Sanou S, Boatin B, Medlock J, Coulibaly S, Molyneux DH. Impact of long-term ivermectin (Mectizan®) on Wuchereria bancrofti and Mansonella perstans infections in Burkina Faso: strategic and policy implications. Ann Trop Med Parasitol. 2003;97:827–838. 10.1179/000349803225002462 [DOI] [PubMed] [Google Scholar]
- 12.Kyelem D, Medlock J, Sanou S, Bonkoungou M, Boatin B, Molyneux DH. Short communication: Impact of long-term (14 years) bi-annual ivermectin treatment on Wuchereria bancrofti microfilaraemia. Trop Med Int Health. 2005;10:1002–1004. 10.1111/tmi.2005.10.issue-10 [DOI] [PubMed] [Google Scholar]
- 13.Richards F, Eigege A, Pam D, Kal A, Lenhart A, Oneyka J et al. Mass ivermectin treatment for onchocerciasis does not interrupt LF transmission (Wuchereria bancrofti) where the parasites are co-endemic in central Nigeria. Filaria J. 2005;4:6–10. 10.1186/1475-2883-4-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richards FO Jr, Eigege A, Pam D, Kal A, Lenhart A, Oneyka JO, et al. Mass ivermectin treatment for onchocerciasis: lack of evidence for collateral impact on transmission of Wuchereria bancrofti in areas of co-endemicity. Filaria J. 2005;4:6. doi: 10.1186/1475-2883-4-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gyapong JO, Kumaraswami V, Biswas G, Ottesen EA. Treatment strategies underpinning the global programme to eliminate lymphatic filariasis. Expert Opin Pharmacother. 2005;6:179–200. 10.1517/eop.2005.6.issue-2 [DOI] [PubMed] [Google Scholar]
- 16.Department of Control of Neglected Tropical Diseases (NTD), World Health Organization Progress report 2000–2009 and strategic plan 2010–2020 of the global programme to eliminate lymphatic filariasis. WHO/HTM/NTD/PCT/2011.4 Geneva, Switzerland [Google Scholar]
- 17.Weil GJ, Lammie PJ, Weiss N. The ICT filariasis test: a rapid-format antigen test for diagnosis of bancroftian filariasis. Parasitology Today. 1997;13: 401–404. 10.1016/S0169-4758(97)01130-7 [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization Operational guidelines for mapping of Bancroftian filariasis in Africa. Geneva: World Health Organization; WHO/CDS/CPE/CEE/2000.9 March, 2000. [Google Scholar]
- 19.Katabarawa MN, Habomugisha P, Eyamba A, Byamukama E, Nwane P, Arinaitwe A, et al. Community-directed interventions are practical and effective in low-resource communities: experience of ivermectin treatment for onchocerciasis control in Cameroon and Uganda, 2004–2010. Int Health. 2015;pii: ihv038. doi: 10.1093/inthealth/ihv038 [DOI] [PubMed] [Google Scholar]
- 20.Richards FO Jr, Miri ES, Katabarwa M, Eyamba A, Sauerbrey M, Zea-Flores G, et al. The Carter Center’s assistance to river blindness control programs: establishing treatment objectives and goals for monitoring ivermectin delivery systems on two continents. Am J Trop Med Hyg. 2001;65:108–114. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization Monitoring and epidemiological assessment of mass drug administration in the global programme to eliminate lymphatic filariasis: a manual for national elimination programmes. Geneva: WHO; 2011. [Google Scholar]
- 22.Chu BK, Deming M, Biritwum N-K, Bougma WR, Dorkenoo AM, El-Setouhy M, et al. Transmission assessment surveys (TAS) to define endpoints for lymphatic filariasis mass drug administration: a multicenter evaluation. PLoS Neglected Trop Dis. 2013;7(12):e2584. doi: 10.1371/journal.pntd.0002584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Worrell C, Mathieu E. Drug coverage surveys for neglected tropical diseases: 10 years of field experience. Am J Trop Med Hyg. 2012;87:216–222. 10.4269/ajtmh.2012.12-0167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Snow LC, Michael E. Transmission dynamics of lymphatic filariasis: density-dependence in the uptake of Wuchereria bancrofti microfilariae by vector mosquitoes. Med Vet Entomol. 2002;16:409–423. 10.1046/j.1365-2915.2002.00396.x [DOI] [PubMed] [Google Scholar]
- 25.Erickson SM, Thomsen EK, Keven JB, Vincent N, Koimbu G, Siba PM, et al. Mosquito-parasite interactions can shape filariasis transmission dynamics and impact elimination programs. PLoS Neglected Trop Dis. 2013;7(9):e2433. 10.1371/journal.pntd.0002433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amuzu H, Wilson MD, Boakye DA. Studies of Anopheles gambiae s.l (Diptera: Culicidae) exhibiting different vectorial capacities in lymphatic filariasis transmission in the Gomoa district, Ghana. Parasites Vectors 2010; 3:85. doi: 10.1186/1756-3305-3-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shargie EB, Ngondi J, Graves PM, Getachew A, et al. Rapid increase in ownership and use of long-lasting insecticidal nets and decrease in prevalence of malaria in three regional states of Ethiopia, 2006-2007. J Trop Med. 2010;2010: IC 750978:12 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eigege A, Kal A, Miri E, Sallau A, et al. Long-lasting insecticidal nets are synergistic with mass drug administration for interruption of lymphatic filariasis transmission in Nigeria. PLoS Neglected Trop Dis. 2013;7:e2508. 10.1371/journal.pntd.0002508 [DOI] [PMC free article] [PubMed] [Google Scholar]