Abstract
Despite common wisdom that reducing alcohol intake will facilitate weight loss, little research has examined whether participants in behavioral weight loss treatments actually decrease their alcohol intake, or whether reduced alcohol intake relates to weight loss outcomes in this context. This study examined the relationship of alcohol use to energy intake excluding alcohol and to weight in 283 overweight and obese adults participating in a 26-session behavioral weight loss treatment. The majority of participants consumed low to moderate levels of alcohol at baseline. Participants who consumed alcohol at baseline meaningfully reduced their alcohol intake by end-of-treatment. Alcohol use did not relate to weight at baseline or end-of-treatment when controlling for relevant demographic variables, and change in alcohol use was unrelated to weight change in the overall sample during treatment. However, end-of-treatment alcohol intake did relate to end-of-treatment energy intake excluding alcohol. In addition, behavioral impulsivity and change in alcohol intake interacted to predict weight loss, such that decreases in alcohol intake were associated with greater percent weight loss at end-of-treatment for participants with higher levels of impulsivity. Alcohol consumption may lead to overeating episodes, and highly impulsive individuals may be at risk for increased energy intake during or after episodes of drinking. Therefore, the recommendation to reduce alcohol intake in the context of behavioral weight loss treatment seems warranted, particularly for individuals with high levels of impulsivity.
Keywords: Alcohol consumption, behavioral weight loss treatment, impulsivity, obesity
Introduction
Reducing alcohol intake is a common recommendation for participants in weight loss programs, with the expectation that making such reductions will improve weight loss outcomes. For instance, government agencies (United States Department of Agriculture, 2015), health organizations (American Heart Association, 2014), and popular weight loss programs (Mayo Clinic, 2014) explicitly recommend reducing alcohol intake during weight loss attempts. Such prescriptions seem logical given that alcohol is energy-dense and that alcohol consumption can trigger impulsive behavior (Marczinski, Abroms, Van Selst, & Fillmore, 2005), with the potential to increase risk for disinhibited eating (e.g. Polivy & Herman, 1976). While there is mixed support for the hypothesis that dietary restraint (the use of cognitive strategies rather than satiety to limit energy intake; Herman & Polivy, 1980) enhances the effects of alcohol on disinhibited eating, consistent findings indicate that alcohol use is associated with increases in short-term energy intake (Caton, Nolan, & Hetherington, 2015).
Currently, available cross-sectional and longitudinal evidence regarding the general relationship between alcohol use and weight management is inconsistent (Gruchow, Sobocinski, Barboriak, & Scheller, 1985; Liu, Serdula, Williamson, Mokdad, & Byers, 1994; Sayon-Orea, Martinez-Gonzalez, & Bes-Rastrollo, 2011), though some recent literature suggests that only heavy or frequent alcohol consumption, rather than light-to-moderate consumption, contributes to elevated weight (Traversy & Chaput, 2015). Furthermore, the amount of alcohol consumed by individuals seeking behavioral weight loss treatment is unclear.
The degree to which individuals adopt the recommendation to reduce alcohol intake during weight loss treatment is also unknown. One study (Egger, Bolton, O’Neill, Freeman, 1996) found that men participating in a group-based behavioral weight loss intervention were successful in losing weight, and that they had reduced their alcohol intake at the end of the treatment. On the other hand, another study (Collins, Morgan, Warren, Lubans, & Callister, 2011) found that men in an internet-based weight loss intervention were successful in losing weight, but that they had not reduced their alcohol intake at the end of the treatment. Neither study examined whether change in alcohol use was directly related to weight loss. In addition, there are no studies investigating whether women participating in behavioral weight loss treatments reduce their alcohol intake.
In addition to the lack of evidence regarding changes in alcohol use in the context of behavioral weight loss, there is no existing research evaluating whether reductions in alcohol intake relate to weight management outcomes. While research has not directly investigated relationships between change in alcohol intake and weight control over time, several experimental studies suggest that alcohol use may make weight control more challenging. For example, alcohol consumption has been shown to stimulate appetite (Yeomans & Phillips, 2002) and lead to increased food intake when consumed prior to or with a meal (Yeomans, 2010). Consumption of alcohol has also been linked to increased desire for and intake of high fat, savory foods (Schrieks et al., 2015). The recommendation to reduce alcohol intake in the context of weight-loss interventions intends to address these risks, but there is insufficient knowledge about how alcohol intake relates to weight, weight loss, or energy intake prior to or after a weight loss attempt.
It is also possible that changes in alcohol intake may differentially relate to weight outcomes across individuals. Certain individual characteristics may influence the importance of reductions in alcohol as a treatment target, and knowledge of these factors can assist in tailoring interventions. For instance, impulsivity, defined as a personality trait involving a lack of reflectiveness and planning, rapid decision making, and carelessness (Schalling, 1978), may be a relevant factor to consider in the relationship between alcohol use and weight outcomes. It is widely understood that self-report measures assess impulsivity as a stable trait, while behavioral measures assess impulsivity as a variable state; however, both types of measures tend to be positively correlated (Meule, 2013). Self-reported impulsivity (and particularly the subdomain of attentional impulsivity) is strongly related to overeating and obesity (Mobbs, Crépin, Thiéry, Golay, & Van der Linden, 2010; Murphy, Stojek, & MacKillop, 2014), as well as to alcohol abuse (Dick et al., 2010). Research also suggests that that both obese individuals (Nederkoorn, Smulders, Havermans, Roefs, & Jansen, 2006) and individuals who abuse alcohol (Verdejo-Garcia, Lawrence, & Clark, 2008) display higher levels of behavioral impulsivity. Furthermore, behavioral impulsivity is related to relapse following both obesity and alcohol treatment (Cox, Hogan, Kristian, & Race, 2002; Elfhag & Rössner, 2005). In the general population, both self-reported and behavioral impulsivity relate to unhealthy eating behaviors such as eating in response to external cues and negative emotional states and making food choices based on taste rather than health, all of which are associated with increased BMI (Jasinska et al., 2012). In this study, we choose to focus on behaviorally-measured impulsivity, as there are no studies examining alcohol use and behavioral impulsivity in the context of weight loss treatment to date.
In addition to research suggesting that impulsivity relates to risk for substance use, alcohol intake acutely increases behavioral impulsivity (Dougherty, Marsh-Richard, Hatzis, Nouvion, Mathais, 2008). High levels of impulsivity may therefore compound the risk for alcohol-related energy intake; highly impulsive individuals may be more likely to consume alcohol, which may result in a higher risk for further impulsive behavior, such as unplanned eating. For this reason, reducing alcohol intake might be a particularly important target for highly impulsive individuals undergoing weight loss treatment to prevent these overeating events. To date, no research has evaluated the role of impulsivity in eating behaviors during periods of alcohol consumption.
The current study sought to examine how changes in alcohol use over time in behavioral weight loss treatment relate to weight loss outcomes after one year of treatment. We anticipated overall reductions in alcohol intake at end-of-treatment, consistent with program recommendations. Further, we hypothesized that alcohol intake would positively relate to energy intake excluding alcohol and to weight at both baseline and end-of-treatment time points. In addition, we expected that change in alcohol intake during treatment would be associated with change in energy intake excluding alcohol as well as change in weight, as reductions in alcohol intake should facilitate reductions in overall calorie intake. Finally, we hypothesized that there would be an interaction between baseline levels of behavioral impulsivity and change in alcohol intake in predicting weight change, such that individuals with higher levels of impulsivity who decreased their alcohol intake would see the most weight loss benefit.
Method
Participants
Participants were 283 overweight and obese adults (21.1% male, Mage = 53.2 years ± 9.7; MBMI = 35.2 kg/m2 ± 5.0) enrolled in a one-year behavioral weight loss program. All participants received the same recommendation to reduce alcohol use as a method of decreasing overall caloric intake, though reducing alcohol consumption was not a particular focus of the program. Most participants identified as White (65.7%) or Black or African American (29.3%), with a minority of participants identifying as American Indian or Alaskan native (0.4%), Asian (0.4%), Native Hawaiian or other Pacific Islander (0.4%), or multiracial (3.5%). Approximately eight percent (8.1 %) of participants identified as Hispanic or Latino.
Eligibility required a BMI between 27.0 and 45.0 kg/m2 and age between 18–70 years. Participants were excluded from the parent study if they were: a) lactating, pregnant, or planning to become pregnant during the course of the trial; b) reported taking a medication or having a medical or psychiatric problem known to cause weight loss or weight gain; c) reported a medical or psychiatric condition that could limit their ability to comply with the program’s behavioral recommendations; d) reported having undergone weight loss surgery; e) were insulin-dependent; or f) had a current or lifetime history of an eating disorder. Participants who met criteria for current substance abuse at baseline were excluded from the parent study.
Procedure
Participants completed self-report measures, including reports of average alcohol intake, at baseline. At baseline and end-of-treatment, individuals also completed three 24-hour food and beverage recalls and had their weight measured by research staff. Two cohorts (n=68) of the parent study were enrolled in a substudy, which included the completion of a computerized Go/No-Go task at baseline. The Go/No-Go task was added to this study to test an exploratory aim and, as such, was only administered to these cohorts in order to reduce participant burden. This sub-sample did not differ from the full sample on measures of gender, racial/ethnic group, age, baseline BMI, or baseline alcohol intake (all p > .05).
Measures
24-hour food and beverage recalls
Participants completed three 24-hour food and beverage recalls via telephone during the baseline and end-of-treatment assessment periods. Recalls were completed for two weekdays and one weekend day. Analyses indicated that there were no significant differences between days of the week in terms of mean alcohol consumed. Registered dieticians conducted the recalls in a multiple pass format and calculated kilocalories per day and grams of nutrients, including alcohol, per day for each participant. Several studies have supported the accuracy of multiple pass 24-hour recalls for the measurement of dietary intake (Conway, Ingwersen, & Moshfegh, 2004; DeMaio, Ciochetto, & Davis, 1993; Jonnalagadda et al., 2000), including for the measurement of alcohol intake (Johannson et al., 2002; Munger, Folsom, Kushi, Kaye, & Sellers, 1992).
Additional self-report of alcohol intake
At baseline, participants reported on the Weight and Lifestyle Inventory (WALI; Wadden & Foster, 2006) how many servings each of wine, beer, and mixed drinks or liquor they typically consumed per week. They also reported any history of problems with alcohol consumption and treatment they received. These WALI items have been shown to have excellent test-retest reliability (Wadden et al., 2012). This measure was used to confirm the validity of the 24-hour recall, and the correlation between daily alcohol consumption as measured by 24-hour recalls and by these WALI items was strong, r(266)= .70, p < .01. Go/No-Go-Task. One cohort of participants completed a computerized Go/No-Go task at baseline as a measure of behavioral impulsivity. During the task, participants were instructed to press a button when pictures appeared on a certain area of the computer screen (“go” stimulus), but not on another (“no-go” stimulus). Pictures of office supplies were chosen for the task so that they were neutral (i.e., not food- or alcohol-related) stimuli for all participants. The outcome measure of interest for the current investigation was the number of times a participant inappropriately pressed the button in response to no-go stimuli, also known as errors of commission. Such a design is commonly used to measure behavioral impulsivity (Jasinska et al., 2012).
Weight
Weights were measured by trained research staff in duplicate using a digital scale (Tanita® model WB-3000) at the baseline and end-of-treatment assessments.
Analytic Plan
Preliminary analyses included examining baseline differences between participants who reported some alcohol consumption versus those who did not using independent-samples t-tests and chi-square tests. In addition, Pearson bivariate correlations between all relevant variables were computed. Primary outcomes included several evaluations. First, change in alcohol during treatment was examined via a paired-samples t-test. Next, the effect of change in alcohol consumption on change in energy intake excluding alcohol was calculated through linear regression. Finally, a model was estimated to examine the interaction between impulsivity and alcohol use in predicting weight change using Hayes’ (2013) SPSS Process Macro. Variables were mean-centered prior to analyses and corrected for heteroscedasticity as recommended (Hayes, 2013). Prior to analyses, the normality of the all variables were examined; grams of alcohol at baseline and end-of-treatment, change in grams of alcohol, energy intake excluding alcohol at baseline and end-of-treatment, and Go/No-Go scores revealed significant skew and were transformed using Tabachnick & Fidell’s (2007) guidelines. Subsequent analyses were completed using these transformed variables.
Results
Description of alcohol intake
During baseline 24-hour recalls, participants reported consuming an average of 6.2 grams (SD = 11.2 grams) of alcohol per day, equivalent to 0.44 alcoholic beverages per day. Approximately 44% of participants (n = 125) consumed at least one gram of alcohol over the three-day recall period. Among these participants, the average daily alcohol intake according to 24-hour recalls was 14.1 grams (SD = 13.2 grams), or about 1.0 alcoholic beverage per day. Twenty-three participants (8.1% of the full sample) met National Institute for Alcohol Abuse and Alcoholism (2014) criteria for “heavy drinking” (more than three alcoholic beverages on any given day for women and more than four for men). On the Weight and Lifestyle Inventory, participants who consumed some alcohol reported an average intake of 0.71 alcoholic beverages per day at baseline; per week, these participants reported consuming an average of 2.6 servings of wine, 1.5 servings of beer, and 0.99 servings of mixed drinks or liquor. For the participants who consumed some alcohol, the correlation between daily alcohol consumption as measured by 24-hour recalls and by self-report was strong, r(117)= .70, p < .01. With regards to individual differences in alcohol consumption, men were more likely to consume alcohol at baseline than women, χ2 (1, N = 285) = 8.04, p < .01. Racial/ethnic group was also predictor of alcohol intake at baseline, χ2 (5, N = 283) = 18.3, p < .01; specifically, White participants were more likely to consume some alcohol at baseline as compared to participants of other racial/ethnic categories, χ2 (1, N = 283) = 14.9, p < .01. The likelihood of consuming alcohol also differed by household income, χ2 (8, N = 275) = 16.3, p < .05. Participants who earned less than $50,000 were less likely to consume alcohol than other participants, χ2(1, N = 275) = 8.2, p < .01. Finally, education level was a significant predictor of alcohol intake at baseline, χ2 (4, N = 282) = 11.3, p < .05. Participants whose highest level of education was a high school diploma or GED were less likely to consume alcohol than other participants, χ2 (1, N = 282) = 5.1, p < .05. Baseline alcohol intake was not significantly correlated with age r(280)= .03.
Change in alcohol intake
According to 24-hour recalls, 45.1% of participants did not consume alcohol at either baseline or end-of-treatment, 15.5% only consumed alcohol at baseline, 11.4% only consumed alcohol at end-of-treatment, and 28.0% consumed alcohol at both assessment points. Participants who did consume alcohol at baseline significantly decreased their mean daily grams of alcohol intake between baseline (M=14.1, SD=13.2) and end-of-treatment (M=11.5, SD=16.2), t(83)= 5.03, p < .01. Of participants who consumed at least one alcoholic beverage per day at baseline (n= 49), 50.0% reduced their alcohol consumption by at least half a beverage (7 grams of alcohol) per day at end-of-treatment.
Relationship of alcohol intake to weight and energy intake
Correlations among alcohol intake and weight-related variables are presented in Table 1. Alcohol intake, as measured by 24-hour recalls, was significantly correlated with BMI at baseline; however, this effect was not significant when controlling for racial/ethnic group. Alcohol intake was not correlated with BMI at end-of-treatment, and change in alcohol intake was not associated with percent weight loss at end-of-treatment. Alcohol intake was also uncorrelated with kilocalories from non-alcohol foods and beverages at baseline. However, among those participants who did consume alcohol at end-of-treatment, alcohol intake was correlated with kilocalories excluding alcohol at this time point, r(74) = .30, p < .01. This correlation remained significant when controlling for percent weight loss at end-of-treatment, r(74) = .26, p < .05, indicating this effect was not simply a result of participants adhering to all treatment recommendations, as well as when controlling for demographic variables. In contrast, change in alcohol intake from baseline to end-of-treatment did not predict change in energy intake excluding alcohol over the same period.
Table 1.
Pearson bivariate correlations among variables of interest
| Mean (SD) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. Baseline BMI (n = 283) | 35.27 (5.21) |
.08 | −.14* | −.02 | .06 | −.002 | −.03 | |
| 2. Weight change (%; n = 204) | −11.11 (7.74) |
−.04 | .11 | −.07 | .19** | .04 | ||
| 3. Baseline alcohol intake (g/day; n = 283) |
6.21 (11.15) |
−.10 | .08 | .09 | .11 | |||
| 4. Change in alcohol intake (g/day; n = 192) |
0.18 (9.06) |
−.05 | .12 | .02 | ||||
| 5. Baseline kilocalories (excluding alcohol; n = 283) |
1812.11 (524.70) |
.02 | −.02 | |||||
| 6. Change in kilocalories (excluding alcohol; n = 192) |
−325.75 (512.52) |
.10 | ||||||
| 7. Go/no-go score (n = 102) | 24.56 (4.97) |
Note.
p < .05,
p < .01.
Relationship of behavioral impulsivity to change in alcohol intake and weight
Next, the interaction between behavioral impulsivity and change in alcohol intake in predicting change in weight was examined. These analyses were performed for the two cohorts of participants who completed the behavioral impulsivity task (n = 68; 20.6% male, Mage = 54.7 years ± 8.7; MBMI = 35.5 kg/m2 ± 5.9). Participants in this cohort did not differ significantly from the rest of the sample in terms of gender, racial/ethnic group, age, baseline BMI, or baseline alcohol intake. For this model, analyses conducted with the transformed variables revealed similar results to analyses conducted with data in their original metric. Therefore, the model reported here includes original variables for ease of interpretation. All variables were measured continuously during analyses. Results of this analysis are reported in Table 2.
Table 2.
The moderating effect of impulsivity on the relationship between change in alcohol intake and percent weight lost
| b | SE | t | p | |
|---|---|---|---|---|
| b1 Change in alcohol intake → percent weight lost | 1.72 | 0.71 | 2.42 | 0.02 |
| b2 Impulsivity → percent weight lost | −0.19 | 0.20 | −0.96 | 0.41 |
| b3 Change in alcohol intake × impulsivity → percent weight lost |
−0.74 | 0.36 | −2.07 | 0.04 |
Note. n = 68. b values for b1 and b2 reflect unstandardized conditional coefficients when the value of the alternate predictor variable is equal to the mean (e.g., b1 equals 1.72 at the average level of impulsivity). b3 reflects an unstandardized interaction coefficient indicating that as impulsivity increases by one unit, the difference in percent weight loss between two cases that differ by one unit in alcohol intake changes by b3 units. SE = standard error; NS = not significant.
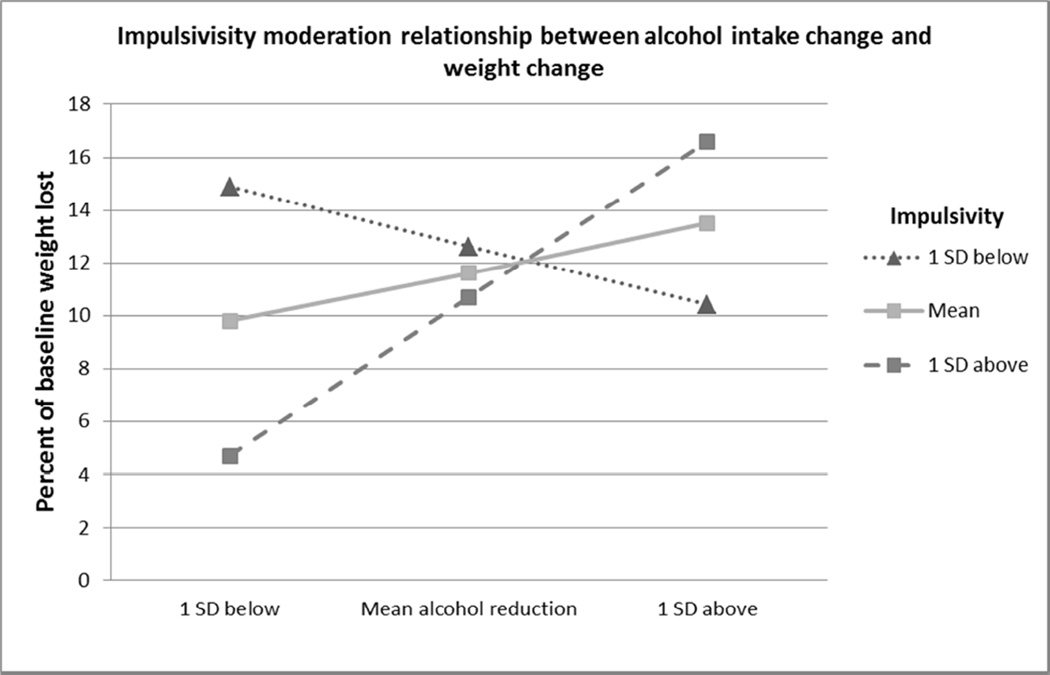
There were no significant correlations between change in alcohol intake, percent weight loss, and impulsivity as measured by the Go/No-Go task. Results revealed a significant conditional effect of change in alcohol intake on percent weight change at the mean value of impulsivity, meaning that the reductions in alcohol intake did predict weight loss at the average level of impulsivity in this sample. There was no conditional effect of impulsivity on weight change at the mean value of change in alcohol intake. Impulsivity interacted with change in alcohol intake to predict weight change. At higher levels of impulsivity, there was a significant association between change in alcohol intake and weight change, such that decreased alcohol consumption from baseline to post-treatment was associated with greater weight loss from baseline to post-treatment. As impulsivity decreased, however, the relationship between change in alcohol intake and weight change diminished. The slope of the relationship between change in alcohol intake and weight change was computed for GNG scores corresponding to one standard deviation above and below the mean level of impulsivity to examine the effect of change in alcohol use on percent weight change at varying levels of impulsivity. This analysis (Figure 1) revealed that change in alcohol intake was negatively associated with weight change (such that a larger decrease in alcohol intake was associated with greater percent weight loss) at higher levels of impulsivity; however, as impulsivity decreased, the relationship between change in alcohol intake and weight change weakened. Additional analysis utilizing the Johnson-Neyman technique (Hayes, 2013; Johnson & Faye, 1950) revealed that a larger change in alcohol intake was associated with a greater percent weight loss at post-treatment until a participant’s impulsivity exceeded a raw score of 25.2, meaning that it fell below approximately the 60th percentile of impulsivity.
Figure 1. The relationship between change in alcohol intake and percent of baseline weight lost at increasing levels of impulsivity.
Note. Closed squares represent impulsivity percentiles at which the relationship between change in alcohol intake and percent weight loss is statistically significant. Closed triangles represent impulsivity percentiles at which the relationship between change in alcohol intake and percent weight loss is not statistically significant.
Discussion
The current study offered novel information regarding prevalence of alcohol use among individuals seeking behavioral weight loss treatment and changes in alcohol use during the course of treatment. According to 24-hour recalls, most participants consumed low to moderate levels of alcohol at baseline, although a small subset met NIAAA (2014) criteria for heavy drinking. In line with past research (Moore et al., 2005), White participants and men were more likely than other participants to consume some alcohol at baseline, while participants whose highest level of education was a high school diploma and those who earned less than $50,000 were less likely to consume alcohol. In addition, participants tended to decrease their alcohol consumption during the course of the study, in line with program recommendations. Half of participants who consumed at least one alcoholic beverage per day at baseline had decreased their alcohol intake by at least half a beverage per day at end-of-treatment.
No previous study has examined the relationship between baseline alcohol intake or change in alcohol intake and weight change in the context of behavioral weight loss treatment, and epidemiological evidence regarding this relationship is equivocal (Gruchow, Sobocinski, Barboriak, & Scheller, 1985; Liu, Serdula, Williamson, Mokdad, & Byers, 1994; Sayon-Orea, Martinez-Gonzalez, & Bes-Rastrollo, 2011; Wannamethee & Shaper, 2003). The current study directly examined this relationship and found that alcohol intake was not significantly related to weight at either time point in the overall sample, and that change in alcohol intake during the course of treatment was also unrelated to weight loss across participants. Given that Black individuals tend to have higher BMIs than individuals of other racial or ethnic groups (Jackson et al., 2013) and that White individuals tend to consume more alcohol (Moore et al., 2005), this relationship was examined when controlling for racial/ethnic group.
Notably, while alcohol intake did not relate to energy intake at baseline, alcohol intake was positively associated with energy intake excluding alcohol at end-of-treatment. There are several possible explanations for this finding. First, participants’ weight loss suggests that they were restricting their energy intake to a greater degree at end-of-treatment. The cognitive restraint required to effectively restrict intake during weight loss interventions (Phelan et al., 2009) may place individuals at greater risk for disinhibited eating episodes (Heatherton, Polivy, & Herman, 1990). In addition, individuals may believe that their goal of restraint has been violated after consuming alcohol (Herman & Polivy, 1980), and, as a result, may be more vulnerable to eating episodes that are not consistent with this goal of dietary restraint during concurrent alcohol consumption. Research suggests that restrained individuals, for instance, may eat more following alcohol administration (Polivy & Herman, 1976), though this effect has failed to replicate in paradigms that differ from the original experiment (e.g. Källmen & Gustafson, 1998; Poppitt, et al., 1996). Alternatively, it is possible that overeating in response to alcohol consumption is moderated by factors like impulsivity, a hypothesis that has not yet been empirically examined. Similarly, alcohol-related expectancies, or the belief that alcohol will enhance appetite and promote excessive energy intake, may also influence the degree to which individuals are susceptible to overeating following alcohol consumption (Caton, Nolan, & Hetherington, 2015), and individuals high in impulsivity may be predisposed to developing such expectancies. Further, alcohol ingestion may heighten the hedonic value of foods, increasing likelihood of consumption in the absence of an increase in physiological hunger (Hofmann, Forster & Stroebe, 2011). In relation to the current sample, susceptibility to hedonic cues may be heightened during a weight loss effort (Rosenbaum, Sy, Pavlovich, Leibel, & Hirsch, 2008; Papies, Stroebe, & Aarts, 2007).
An alternative explanation for the finding that alcohol intake was more strongly related to energy intake excluding alcohol at end-of-treatment is that individuals were, overall, consuming less energy at end-of-treatment. The effects of alcohol consumption on energy intake may be heightened when individuals are consuming less energy overall, as an increase of the same number of kilocalories consumed would represent a greater proportion of overall consumption.
Despite findings that, on average, change in alcohol did not relate to weight loss, the study identified that reducing alcohol intake was relevant to successful weight loss for certain individuals. Namely, decreasing alcohol intake provided additional weight loss benefits as behavioral impulsivity increased; thus, individuals with higher levels of behavioral impulsivity experienced larger weight loss benefits from reducing their alcohol consumption during treatment. Existing literature suggests that negative urgency, a subtype of impulsivity that has been associated with difficulty in inhibiting prepotent responses on a measure of behavioral impulsivity (Gay, Rochat, Billieux, Acremont, & Van der Linden, 2008; Billieux, Gay, Rochat, & Van der Linden, 2010), relates to problem-level involvement in maladaptive behaviors (e.g. problem drinking, binge eating, problem gambling), but not to the frequency of engaging in gambling or drinking (Smith et al., 2007). Furthermore, trait urgency has been found to strengthen the relationship between feelings of anxiety and episodes of alcohol intoxication (Simons, Dvorak, Batien, & Wray, 2010). Considered in the context of the current findings, even when frequency of drinking is similar, highly impulsive individuals may be more likely to experience alcohol-related problems, including overeating, that arise from a disposition towards rash action. These actions, such as unplanned eating events or eating highly caloric foods, may derail their weight loss attempts. It is important to note that these unplanned eating episodes may not have been driven by physiological hunger cues, but rather a hedonic desire for good tasting food and unwillingness to restrain from consumption. For instance, studies suggest that physical appetite increases occur after ingesting 24g of alcohol (Hetherington, Cameron, Wallis, & Pirie, 2001; Caton, Ball, Ahern, & Hetherington, 2004; Caton, Marks, & Hetherington, 2005; Caton, Bate, & Hetherington, 2007), which is a greater amount of alcohol than the majority of our participants reported drinking. It is unlikely, then, that increases in food consumption for highly impulsive individuals who drank were due solely to physical appetite stimulation resulting from alcohol intake. Overall, targeting reductions in alcohol intake may be of importance for impulsive individuals, who are already more prone than their non-impulsive counterparts to unhealthy eating behaviors (Jasinska et al., 2012). Limiting alcohol intake directly reduces energy consumption and may also prevent overeating surrounding drinking episodes, which in turn reduces overall energy intake.
Limitations and Future Directions
This study had several strengths, including the novel investigation of relationships among impulsivity, alcohol use, and weight loss during behavioral weight loss treatment. In addition to the noted strengths, some limitations of the current findings should be considered. First, three 24-hour food and beverage recalls were the primary tool used to measure alcohol intake. This measure may not have captured some drinking behaviors (e.g. if a participant tends to drink heavily on multiple days per week, but these days were not part of the three day record), or been representative of typical intake (e.g. if a participant had an unusual night of heavy drinking that was captured in their food recall). However, the literature does support the validity of this tool for measuring alcohol intake (Johannson et al., 2002; Munger et al., 1992), and a strong relationship existed between alcohol intake measured through the 24-hour recalls and self-reported alcohol intake on the Weight and Lifestyle Inventory. Additionally, although there was no significant relationship between alcohol intake and weight or weight loss in the current study, it is possible that this relationship exists, but that we were not able to detect it in the current sample.
Notably, individuals in this study reported a lower level of alcohol intake than the general population (LaVallee & Yi, 2011; Substance Abuse and Mental Health Services Administration, 2012). The relatively low levels of alcohol consumption were likely the result of the high average age and restricted age range in this sample (Moore, et al., 2005) and the exclusion of individuals who abuse alcohol. The comparatively low levels of alcohol use and the small subset of heavy drinkers are a limitation of this study. However, many participants did consume some alcohol at baseline and, despite the relatively low use, the results demonstrate participants did make meaningful changes in their alcohol intake.
Furthermore, while the current study examined the interaction between impulsivity and alcohol use to predict weight loss, there was no direct evidence of the mechanism. We hypothesize that alcohol consumption puts highly impulsive individuals at a greater risk for disinhibited eating episodes that counteracted weight loss efforts. The lack of evidence for this mechanism leaves the results open to alternative interpretations. Alcohol-related expectancies, rather than disinhibition, could explain the pattern of our results. There is support for the theory that norms regarding intoxicated behavior may be adequately powerful to cause said behaviors (Caton , Nolan, & Hetherington, 2015). In other words, overeating after alcohol consumption could be driven by the belief that alcohol leads to overeating. Another alternative is that highly impulsive drinkers were simply less skilled at planning their alcohol use and subsequently adapting their energy intake excluding alcohol to stay within their calorie goals compared to less impulsive drinkers. The design of the current study means that we were unable to definitively identify a mechanism, although understanding the mechanism will be important for informing treatment recommendations. The current study also did not include repeated measures during the course of treatment, meaning that we were not able to examine the effect of changes in alcohol intake on acute weight loss early in treatment.
The aforementioned limitations demonstrate the need for further research on this topic, with alcohol use during behavioral weight loss treatment as a primary outcome measure. Such investigations should replicate the findings in a larger and more heterogeneous sample. Specifically, the current findings should be explored in the context of a younger treatment-seeking sample, as it has been shown that young adulthood is a particularly vulnerable period for weight gain (Truesdale et al., 2006) and that young adults consume more alcohol than older adults (Moore et al., 2006). While age and alcohol intake were unrelated in the current sample, the small percentage of young individuals (e.g., only 2.4% of participants were under the age of 30) did not allow for a full evaluation of this relationship. Future studies should also consider using a more comprehensive assessment of alcohol intake. For example, using timeline follow-back or ecological momentary assessments (EMA), two common approaches in alcohol-related research (Carney, Tennen, Affleck, Del Boca, & Kranzler, 1998; Shiffman, 2009), would provide more detailed information about alcohol use during weight loss treatment. Most importantly, research should aim to identify the mechanism behind the current findings in order to inform treatment recommendations.
Conclusions
Overall, findings from the current investigation provide valuable information regarding the relationship between alcohol use and treatment outcome in behavioral weight loss treatment. While initial levels of alcohol consumption did not relate to non-alcohol consumption, this relationship was important as individuals progressed in treatment. Further, reductions in alcohol use during treatment appeared to be particularly relevant for the success of individuals who displayed high levels of impulsivity. Altogether, current guidelines to reduce alcohol intake during weight loss treatment appear warranted, with such recommendations being differentially important across individuals.
Most adult participants of a behavioral weight loss treatment consumed low to moderate levels of alcohol at baseline.
Those participants who did consume alcohol at baseline had meaningfully reduced their alcohol intake by the end-of-treatment.
End-of-treatment alcohol intake was correlated with end-of-treatment intake of non-alcohol energy.
Behavioral impulsivity and change in alcohol intake interacted to predict weight loss.
Acknowledgments
Funding Source: R01 DK 092374
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Heart Association. Alcohol and heart health. 2014 Retrieved from http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/Alcohol-and-Heart-Health_UCM_305173_Article.jsp.
- Billieux J, Gay P, Rochat L, Van der Linden M. The role of urgency and its underlying psychological mechanisms in problematic behaviours. Behaviour Research and Therapy. 2010;48(11):1085–1096. doi: 10.1016/j.brat.2010.07.008. [DOI] [PubMed] [Google Scholar]
- Butryn ML, Coletta M, Clark VL. Behavioral treatment for obesity. In: Akabas SR, Lederman SA, Moore BJ, editors. Understanding Obesity: Biological, Psychological and Cultural Influences. New York, NY, USA: Wiley; 2012. pp. 253–272. [Google Scholar]
- Carney MA, Tennen H, Affleck G, del Boca FK, Kranzler HR. Levels and patterns of alcohol consumption using timeline follow-back, daily diaries and realtime. Journal of Studies on Alcohol and Drugs. 1998;59(4):447. doi: 10.15288/jsa.1998.59.447. [DOI] [PubMed] [Google Scholar]
- Caton SJ, Ball M, Ahern A, Hetherington MM. Dose-dependent effects of alcohol on appetite and food intake. Physiology & Behavior. 2004;81(1):51–58. doi: 10.1016/j.physbeh.2003.12.017. [DOI] [PubMed] [Google Scholar]
- Caton SJ, Bate L, Hetherington MM. Acute effects of an alcoholic drink on food intake: aperitif versus co-ingestion. Physiology & Behavior. 2007;90(2):368–375. doi: 10.1016/j.physbeh.2006.09.028. [DOI] [PubMed] [Google Scholar]
- Caton SJ, Marks JE, Hetherington MM. Pleasure and alcohol: manipulating pleasantness and the acute effects of alcohol on food intake. Physiology & Behavior. 2005;84(3):371–377. doi: 10.1016/j.physbeh.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Caton SJ, Nolan LJ, Hetherington MM. Alcohol, Appetite and Loss of Restraint. Current Obesity Reports. 2015;4(1):99–105. doi: 10.1007/s13679-014-0130-y. [DOI] [PubMed] [Google Scholar]
- Christian JG, Tsai AG, Bessesen DH. Interpreting weight losses from lifestyle modification trials: using categorical data. International Journal of Obesity. 2010;34(1):207–209. doi: 10.1038/ijo.2009.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins CE, Morgan PJ, Warren JM, Lubans DR, Callister R. Men participating in a weight-loss intervention are able to implement key dietary messages, but not those relating to vegetables or alcohol: The self-help, exercise and diet using internet technology (SHED-IT) study. Public Health Nutrition. 2011;14(1):168–175. doi: 10.1017/S1368980010001916. [DOI] [PubMed] [Google Scholar]
- Conway JM, Ingwersen LA, Moshfegh AJ. Accuracy of dietary recall using the USDA five-step multiple-pass method in men: an observational validation study. Journal of the American Dietetic Association. 2004;104(4):595–603. doi: 10.1016/j.jada.2004.01.007. [DOI] [PubMed] [Google Scholar]
- Cox WM, Hogan LM, Kristian MR, Race JH. Alcohol attentional bias as a predictor of alcohol abusers’ treatment outcome. Drug and Alcohol Dependence. 2002;68(3):237–243. doi: 10.1016/s0376-8716(02)00219-3. [DOI] [PubMed] [Google Scholar]
- Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neuroscience & Biobehavioral Reviews. 2004;28(3):343–351. doi: 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- DeMaio TJ, Ciochetto S, Davis WL. Research on the continuing survey of food intakes by individuals. 1993 Proceedings of the Section on Survey Research Methods, American Statistical Association. 1993:1021–1026. [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, Sher K. Review: understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15(2):217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Marsh-Richard DM, Hatzis ES, Nouvion SO, Mathias CW. A test of alcohol dose effects on multiple behavioral measures of impulsivity. Drug and Alcohol Dependence. 2008;96(1):111–120. doi: 10.1016/j.drugalcdep.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger G, Bolton A, O’Neill M, Freeman D. Effectiveness of an abdominal obesity reduction programme in men: The GutBuster “waist loss” programme. InternationalJ journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 1996;20(3):227–231. [PubMed] [Google Scholar]
- Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews. 2005;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Gay P, Rochat L, Billieux J, d’Acremont M, Van der Linden M. Heterogeneous inhibition processes involved in different facets of self-reported impulsivity: Evidence from a community sample. Acta Psychologica. 2008;129(3):332–339. doi: 10.1016/j.actpsy.2008.08.010. [DOI] [PubMed] [Google Scholar]
- Gruchow HW, Sobocinski KA, Barboriak JJ, Scheller JG. Alcohol consumption, nutrient intake and relative body weight among US adults. The American Journal of Clinical Nutrition. 1985;42(2):289–295. doi: 10.1093/ajcn/42.2.289. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY, USA: Guilford Press; 2013. [Google Scholar]
- Heatherton TF, Polivy J, Herman CP. Dietary restraint: Some current findings and speculations. Psychology of Addictive Behaviors. 1990;4(2):100. [Google Scholar]
- Herman C, Polivy J. Restrained eating. In: Stunkard AJ, editor. Obesity. Philadelphia, PA, USA: WB Saunders; 1980. pp. 208–225. [Google Scholar]
- Hetherington MM, Cameron F, Wallis DJ, Pirie LM. Stimulation of appetite by alcohol. Physiology & Behavior. 2001;74(3):283–289. doi: 10.1016/s0031-9384(01)00598-4. [DOI] [PubMed] [Google Scholar]
- Hofmann W, Förster G, Stroebe W, Wiers RW. Handbook of Behavior, Food and Nutrition. Springer New York: 2011. The great disinhibitor: alcohol, food cues, and eating behavior; pp. 2977–2991. [Google Scholar]
- Jackson CL, Szklo M, Yeh HC, Wang NY, Dray-Spira R, Thorpe R, Brancati FL. Black-white disparities in overweight and obesity trends by educational attainment in the United States, 1997–2008. Journal of Obesity. 2013 doi: 10.1155/2013/140743. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasinska AJ, Yasuda M, Burant CF, Gregor N, Khatri S, Sweet M, Falk EB. Impulsivity and inhibitory control deficits are associated with unhealthy eating in young adults. Appetite. 2012;59(3):738–747. doi: 10.1016/j.appet.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson I, Hallmans G, Wikman Å, Biessy C, Riboli E, Kaaks R. Validation and calibration of food-frequency questionnaire measurements in the Northern Sweden Health and Disease cohort. Public Health Nutrition. 2002;5(03):487–496. doi: 10.1079/phn2001315. [DOI] [PubMed] [Google Scholar]
- Johnson PO, Fay LC. The Johnson-Neyman technique, its theory and application. Psychometrika. 1950;15(4):349–367. doi: 10.1007/BF02288864. [DOI] [PubMed] [Google Scholar]
- Jonnalagadda SS, Mitchell DC, Smiciklas-Wright H, Meaker KB, Van Heel N, Karmally W, Kris-Etherton PM. Accuracy of energy intake data estimated by a multiplepass, 24-hour dietary recall technique. Journal of the American Dietetic Association. 2000;100(3):303–311. doi: 10.1016/s0002-8223(00)00095-x. [DOI] [PubMed] [Google Scholar]
- Källmén H, Gustafson R. Alcohol and disinhibition. European Addiction Research. 1998;4(4):150–162. doi: 10.1159/000018948. [DOI] [PubMed] [Google Scholar]
- Kleiner KD, Gold MS, Frostpineda K, Lenzbrunsman B, Perri MG, Jacobs WS. Body mass index and alcohol use. Journal of Addictive Diseases. 2004;23(3):105–118. doi: 10.1300/J069v23n03_08. [DOI] [PubMed] [Google Scholar]
- Lahti-Koski M, Pietinen P, Heliövaara M, Vartiainen E. Associations of body mass index and obesity with physical activity, food choices, alcohol intake, and smoking in the 1982–1997 FINRISK Studies. The American Journal of Clinical Nutrition. 2002;75(5):809–817. doi: 10.1093/ajcn/75.5.809. [DOI] [PubMed] [Google Scholar]
- LaVallee RA, Yi H. Apparent per capita alcohol consumption: National, state, and regional trends, 1997–2009 (No. 92) US Department of Health and Human Services, Public Health Service, National Institutes of Health; 2011. [Google Scholar]
- Liu S, Serdula MK, Williamson DF, Mokdad AH, Byers T. A prospective study of alcohol intake and change in body weight among US adults. American Journal of Epidemiology. 1994;140(10):912–920. doi: 10.1093/oxfordjournals.aje.a117179. [DOI] [PubMed] [Google Scholar]
- Marczinski CA, Abroms BD, Van Selst M, Fillmore MT. Alcohol-induced impairment of behavioral control: differential effects on engaging vs. disengaging responses. Psychopharmacology. 2005;182(3):452–459. doi: 10.1007/s00213-005-0116-2. [DOI] [PubMed] [Google Scholar]
- Mayo Clinic. Alcohol use: If you drink, keep it moderate. 2014 Retrieved from http://www.mayoclinic.org/healthy-living/nutrition-and-healthy-eating/in-depth/alcohol/art-20044551.
- Mobbs O, Crépin C, Thiéry C, Golay A, Van der Linden M. Obesity and the four facets of impulsivity. Patient Education and Counseling. 2010;79(3):372–377. doi: 10.1016/j.pec.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Munger RG, Folsom AR, Kushi LH, Kaye SA, Sellers TA. Dietary assessment of older Iowa women with a food frequency questionnaire: nutrient intake, reproducibility, and comparison with 24-hour dietary recall interviews. American Journal of Epidemiology. 1992;136(2):192–200. doi: 10.1093/oxfordjournals.aje.a116485. [DOI] [PubMed] [Google Scholar]
- Murphy CM, Stojek MK, MacKillop J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite. 2014;73:45–50. doi: 10.1016/j.appet.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. What’s “at-risk or “heavy” http://rethinkingdrinking.niaaa.nih.gov/IsYourDrinkingPatternRisky/WhatsAtRiskOrHeavyDrinking.asp
- Meule A. Impulsivity and overeating: a closer look at the subscales of the Barratt Impulsiveness Scale. Frontiers in Psychology. 2013;4:177. doi: 10.3389/fpsyg.2013.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Gould R, Reuben DB, Greendale GA, Carter MK, Zhou K, Karlamangla A. Longitudinal patterns and predictors of alcohol consumption in the United States. American Journal of Public Health. 2005;95(3):458. doi: 10.2105/AJPH.2003.019471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nederkoorn C, Jansen E, Mulkens S, Jansen A. Impulsivity predicts treatment outcome in obese children. Behaviour Research and Therapy. 2007;45(5):1071–1075. doi: 10.1016/j.brat.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Effects of alcohol on eating behavior: influence of mood and perceived intoxication. Journal of Abnormal Psychology. 1976;85(6):601. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National survey on drug use and health (NSDUH) 2012 Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2012/NSDUH-DetTabs2012/HTML/NSDUH-DetTabsSect2peTabs 43to84-2012.htm#Tab2.46B. [PubMed]
- Papies E, Stroebe W, Aarts H. Pleasure in the mind: Restrained eating and spontaneous hedonic thoughts about food. Journal of Experimental Social Psychology. 2007;43(5):810–817. [Google Scholar]
- Phelan S, Liu T, Gorin A, Lowe M, Hogan J, Fava J, Wing RR. What distinguishes weight-loss maintainers from the treatment-seeking obese? Analysis of environmental, behavioral, and psychosocial variables in diverse populations. Annals of Behavioral Medicine. 2009;38(2):94–104. doi: 10.1007/s12160-009-9135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poppitt SD, Eckhardt JW, McGonagle J, Murgatroyd PR, Prentice AM. Short-term effects of alcohol consumption on appetite and energy intake. Physiology & Behavior. 1996;60(4):1063–1070. doi: 10.1016/0031-9384(96)00159-x. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M, Sy M, Pavlovich K, Leibel RL, Hirsch J. Leptin reverses weight loss-induced changes in regional neural activity responses to visual food stimuli. The Journal of Clinical Investigation. 2008;118(7):2583. doi: 10.1172/JCI35055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutrition Reviews. 2011;69(8):419–431. doi: 10.1111/j.1753-4887.2011.00403.x. [DOI] [PubMed] [Google Scholar]
- Schalling D. Psychopathy-related personality variables and the psychophysiology of socialization. In: Hare RD, Schalling D, editors. Psychopathic Behavior: Approaches to Research. New York, NY, USA: Wiley; 1978. pp. 85–106. [Google Scholar]
- Schrieks IC, Stafleu A, Griffioen-Roose S, de Graaf C, Witkamp RF, Boerrigter-Rijneveld R, Hendriks HF. Moderate alcohol consumption stimulates food I intake and food reward of savoury foods. Appetite. 2015;89:77–83. doi: 10.1016/j.appet.2015.01.021. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21(4):486. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Batien BD, Wray TB. Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive Behaviors. 2010;35(12):1045–1053. doi: 10.1016/j.addbeh.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14(2):155–170. doi: 10.1177/1073191106295527. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Boston, MA, USA: Allyn and Bacon; 2007. [Google Scholar]
- Traversy G, Chaput J. Alcohol consumption and obesity: An update. Current Obesity Reports. 2015;4:122–130. doi: 10.1007/s13679-014-0129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truesdale KP, Stevens J, Lewis CE, Schreiner PJ, Loria CM, Cai J. Changes in risk factors for cardiovascular disease by baseline weight status in young adults who maintain or gain weight over 15 years: the CARDIA study. International Journal of Obesity. 2006;30(9):1397–1407. doi: 10.1038/sj.ijo.0803307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Agriculture. Commonly asked questions (FAQs) 2015 Retrieved From http://www.nutrition.gov/weight-management/commonly-asked-questions-faqs.
- Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neuroscience & Biobehavioral Reviews. 2008;32(4):777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, Sarwer DB, Fabricatore AN, Crerand CE, Lipschutz PE, Williams NN. Comparison of Psychosocial Status in Treatment-Seeking Women with Class III vs. Class I–II Obesity. Obesity. 2006;14(S3):90S–98S. doi: 10.1038/oby.2006.288. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Foster GD. The weight and lifestyle inventory (WALI) Obesity. 2006;14(S2):99S–118S. doi: 10.1038/oby.2006.289. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG. Alcohol, body weight, and weight gain in middle-aged men. The American Journal of Clinical Nutrition. 2003;77(5):1312–1317. doi: 10.1093/ajcn/77.5.1312. [DOI] [PubMed] [Google Scholar]
- Yeomans MR. Alcohol, appetite and energy balance: is alcohol intake a risk factor for obesity? Physiology & Behavior. 2010;100(1):82–89. doi: 10.1016/j.physbeh.2010.01.012. [DOI] [PubMed] [Google Scholar]
- Yeomans MR, Phillips MF. Failure to reduce short-term appetite following alcohol is independent of beliefs about the presence of alcohol. Nutritional Neuroscience. 2002;5(2):131–139. doi: 10.1080/10284150290019008. [DOI] [PubMed] [Google Scholar]