Abstract
Introduction
Behavioral couples therapy (BCT) has been found to improve long-term abstinence rates in alcohol- and substance-dependent populations but has not been tested for smoking cessation. This pilot study examined the feasibility and acceptability of BCT for smoking-discordant couples.
Methods
Forty-nine smokers (smoking >10 cigarettes/day) with non-smoking partners were randomized to receive a couples social support (BCT-S) intervention, or an individually-delivered smoking cessation (ST) treatment. The couples were married or cohabiting for at least one year, with partners who had never smoked or had not used tobacco in one year. Both treatments included seven weekly sessions and 8-weeks of nicotine replacement therapy. Participants were followed for six months post-treatment. The Partner Interaction Questionnaire (PIQ) was used to measure perceived smoking-specific partner support.
Results
Participants were 67% male and 88% White. Biochemically-verified cessation rates were 40.9%, 50% and 45% in BCT-S, and 59.1%, 50%, and 55% in ST, at end of treatment, 3-, and 6-months, respectively, and did not differ significantly between treatment conditions at any time point (all p’s > .05). Perceived smoking-specific partner support at post-treatment did not significantly differ between treatment groups (M=2.45, SD .81 in BCT-S; M=2.27, SD .92 in ST; t(38) = .67, p = .51).
Conclusions
Results of this pilot study do not provide support for the efficacy of BCT in smoking discordant couples.
Keywords: smoking cessation, couples therapy, tobacco dependence, behavioral couples therapy
INTRODUCTION
Cigarette smoking is a leading cause of preventable death and smoking-related disability (USDHHS, 2010). For the nearly 25 million non-smokers married to smokers, second-hand smoke exposure is associated with a 35% greater risk of lung cancer for the non-smoking partner (Crispo et al., 2004; Fiore, 2008; USDHHS, 2004). For children, exposure to second-hand smoke has been found to be associated with middle ear infections, respiratory tract infections, and 1 million cases of asthma annually (CDC, 2008). Therefore, effective smoking cessation treatments can have considerable public health impact for smokers, their partners, and their families. Although smoking rates in the U.S. have declined since 2005 to approximately 18.1%, little change has been noted since 2012 indicating a plateau in cessation rates (CDC, 2014). Even among those who quit successfully, relapse often occurs within 5 months following the quit attempt (USDHHS, 2000). Continued improvement in treatments are needed that build upon current best practices and incorporate advances in substance abuse treatment models to increase long-term abstinence rates (Piasecki & Baker, 2001).
The characteristics of a smoker’s social network may enhance efforts to quit smoking leading to an improved likelihood of long-term abstinence. Perceived social support facilitates attempts to quit smoking (Albertsen, Borg, & Oldenburg, 2006; May, West, Hajek, McEwen, & McRobbie, 2007; Vilchinsky, et al., 2011), and partner support has predicted greater readiness to quit smoking (Rayens, Hahn, & Hedgecock, 2008), an increased likelihood of quitting (Coppotelli & Orleans, 1985; Mermelstein, et al., 1986; Pollack, et al., 2006; Rayens, Hahn, & Nicholson, 2011) and a lower likelihood of relapse after quitting (Gulliver et al., 1995; Mermelstein, Lichtenstein, & McIntyre, 1983; Pollak & Mullen, 1997).
Social support from a romantic partner has been found to be particularly influential in smoking cessation attempts. Simply having a partner, as opposed to being single, leads to a higher likelihood of abstinence after a smoking cessation intervention (Brothers & Borrelli, 2011). In a recent longitudinal study of couples in which one or both partners smoked, higher perceived partner responsiveness at baseline predicted a decreased likelihood of smoking and fewer cigarettes smoked per day nine years later (Derrick, Leonard, & Homish, 2013). Smokers who are confident in their ability to work with their partner as a team in a smoking cessation effort are more likely to successfully quit (Sterba, et al., 2011), and there is evidence that partners of smokers are interested in helping their partners quit (Thomas, et al., 2009). Positive partner support for quitting smoking has been related to higher engagement in smoking cessation treatment (Richardson et al., 2013). Interventions that explicitly promote romantic partner support may improve long-term abstinence rates in smokers attempting to quit.
Previous smoking cessation studies that included a component to enhance partner support have had limitations and did not demonstrate evidence of improved quit rates (Park, Tudiver, & Campbell, 2012). Various interventions were utilized, however, results suggested that some of the interventions failed to increase perceived social support (Park, Tudiver, & Campbell, 2012). Past studies often utilized a wide definition of partner that included co-workers and friends, in addition to spouses and live-in partners. In an earlier review, Park (2004) found that studies that included solely married or live-in partners produced higher odds ratios of cessation compared with other trials. Because romantic cohabitating partners have greater proximity to the smoker, they may be better able to provide consistent smoking-specific support behaviors over time than more distal partners (May & West, 2000). Additional limitations of previous studies included a lack of biochemical verification of cessation, non-randomized designs, lack of adequate control groups, and the lack of a theoretical framework to guide the study (May & West, 2000; Park et al., 2012; Westmaas, 2010).
Behavioral couples’ therapy (BCT), an empirically developed intervention, is recognized as an efficacious method for the treatment of alcohol and other substance use disorders (SUD; Epstein, E.E., & McCrady, B.S. (2002); Epstein, E.E., McCrady, B.S., Morgan, T.J., Cook, S.M., Kugler, G., & Ziedonis, D., 2007a; Powers, Vedel & Emmelkamp, 2008). BCT has well-specified treatment components involving partners who do not have substance abuse or dependence issues, and may be ideal for smoking cessation. BCT offers a partner-involved approach designed to focus not only on the addictive behavior, but also on the partner’s role in supporting abstinence and on the relational support factors conducive to long-term abstinence (O’Farrell & Schein, 2011). Across studies of SUD, BCT has demonstrated significantly greater abstinence up to two years post-treatment compared to individual-focused approaches (O’Farrell & Clements, 2012). BCT has also demonstrated efficacy in improving relationship functioning, increasing session attendance, and promoting greater treatment retention compared to individual-only modalities (O’Farrell, Murphy, Alter & Fals-Stewart, 2010; Stanton & Shadish, 1997; Powers et al, 2008). To date, no known studies have adapted and applied BCT to cohabitating couples in which one partner smokes. The purpose of this pilot randomized clinical trial was to examine the feasibility and acceptability of BCT for smoking cessation in smoking-discordant cohabitating couples. We also wanted to compare smoking cessation outcomes among smokers who were randomized to receive either BCT or an individual cessation treatment (ST), with a non-smoking significant other. Based on previous research with BCT for alcohol and other SUD (Meis et al., 2013), we hypothesized that smokers who participated in a BCT intervention would demonstrate higher point-prevalence abstinence at end of treatment, 3-month, and 6-month follow-ups.
METHODS
Participants
Participants were 49 current smokers who wanted help quitting smoking and their non-smoking partners. To be included, participants had to be: a) at least 18 years of age, b) smoking at least 10 cigarettes per day for at least one year; c) in a heterosexual marriage or cohabiting romantic relationship for more than one year; and, d) willing to use and have no contraindications for transdermal nicotine patch (TNP). Partners of eligible smokers had to be at least 18 years of age, nonsmokers (or not used tobacco in the previous one year), willing to participate in the study, and have an expired carbon monoxide (CO) level at baseline < 10 parts per million. Potential participants were excluded at baseline if they were: a) currently pregnant or nursing; b) using smokeless or other forms of tobacco; c) in a severely distressed romantic relationship or marriage (defined as 1.5 SD below Dyadic Adjustment Scale score [DAS] mean or DAS < 60; Spanier, 1976), or have a history of physical domestic violence by their partner (by self or partner report) in the prior year; d) currently using other pharmacotherapies for smoking cessation, or e) diagnosed with a psychiatric disorder, taking prescribed psychotropic medication, or receiving psychotherapy. Two items from the Alcohol Use Disorders Identification Test (AUDIT) were used to screen out those participants who were drinking alcohol at problematic levels of use (Saunders, et al., 1993). Potential participants were asked: How often do you have a drink containing alcohol? (never; less than monthly; monthly; weekly; daily or almost daily); How many drinks containing alcohol do you have on a typical day when you are drinking? (1–2; 3–4; 5–6; 7–9; 10 or more). We excluded only persons who engaged in binge drinking or heavy drinking on a regular basis. The National Jewish Health Institutional Review Board approved the study and all participants provided written informed consent to participate.
Procedure
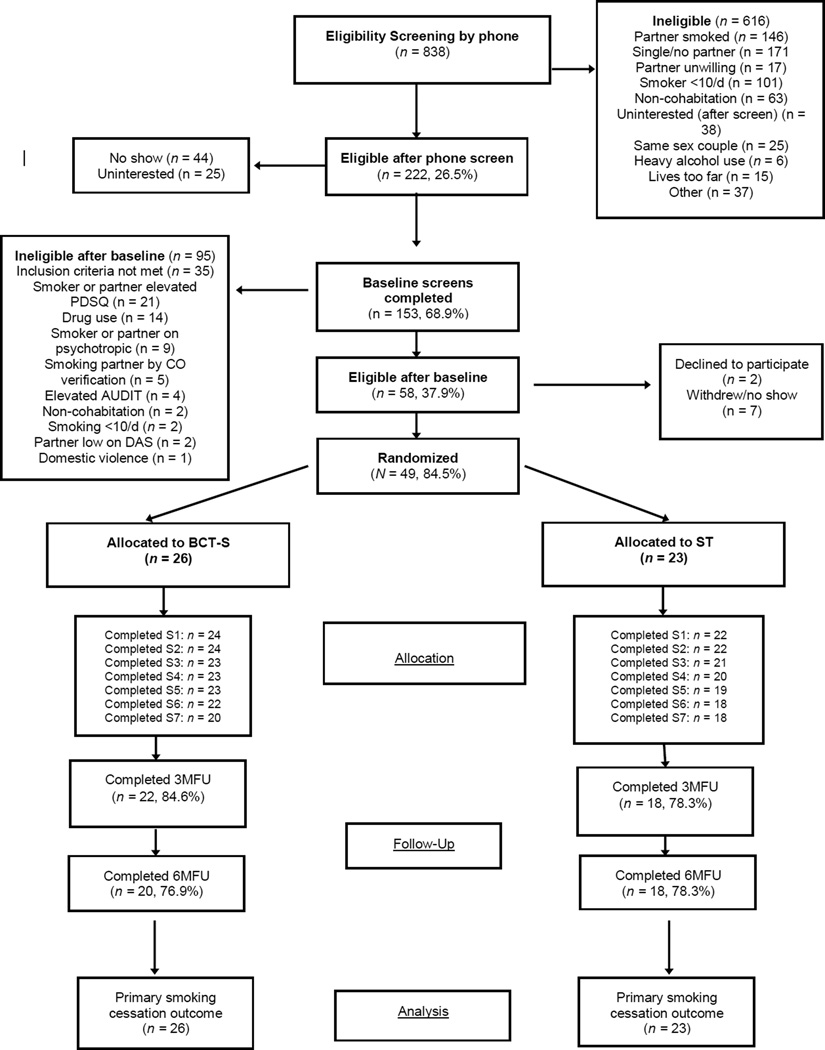
Participants were recruited from the community via newspaper and television advertisements for cigarette smokers who wanted to quit and were living with a non-smoking partner who was interested in assisting with the cessation effort. Individuals who responded to advertisements completed a brief telephone screen to determine initial eligibility prior to scheduling a baseline session. Potential participants were asked their age, relationship status, current smoking level and other tobacco use, estimate of partner’s smoking and/or tobacco use, current medications prescribed, any diagnosed medical conditions, and recent hospitalizations. If deemed potentially eligible, participants (smokers) and their partners were invited to a baseline assessment interview to confirm study eligibility. At that time, the Psychiatric Diagnostic Screening Questionnaire (PDSQ) was administered to smokers and their partners to exclude individuals that met criteria for current mood, anxiety, substance dependence, psychotic or somatoform disorders (Zimmerman & Mattia, 2001). The baseline consent and assessment session lasted approximately 40–50 minutes. See Figure 1 for a diagram of participant flow.
Figure 1.
Participant flow diagram
CONSORT flowchart of eligibility, randomization, treatment, follow-up, and inclusion in analyses. BCT-S = behavioral couples treatment. ST = standard, individual smoking cessation treatment. MFU = month follow-up.
Randomization
At baseline, participants were randomly assigned to receive either a couples’ social support smoking cessation intervention (BCT-S), or an individually-delivered behavioral therapy smoking cessation treatment (ST). An urn randomization procedure (Stout, Wirtz, Carbonari, & DelBoca, 1994; Wei, & Lachin, 1978) was used to probabilistically balance the experimental and control groups on three potential prognostic factors: 1) gender of the smoker; 2) nicotine dependence severity assessed by time to first cigarette of the day [<30 minutes after waking, versus >30 minutes]; and 3) relationship happiness on the Dyadic Adjustment Scale (using a 7-point Likert item: >3.5 (“happy or better”) by both members of the couple versus <3.5 (“less than happy”) by one or both partners. Twenty-six participants were randomized to BCT-S and 23 were randomized to ST.
Assessments
Following consent and randomization, participants were informed of their treatment assignment. All couples attended the baseline assessment together; however, they completed baseline assessments, such as the DAS, separately. In the treatment sessions that followed, participants attended as couples in BCT-S only. Participants completed assessments at each treatment session and at 3- and 6-months post-treatment. Both treatment conditions included seven weekly, 60-minute sessions and 8-weeks of transdermal nicotine replacement therapy.
Treatments
Across both BCT-S and ST, treatments were conducted according to specific manuals, and were administered by five therapists (a licensed psychologist, a master’s level clinician, an intern, and two bachelor’s level therapists) trained in BCT-S and ST protocols. All therapists delivered both BCT-S and ST treatments. The session number, duration, and therapist contact time were matched across conditions. Participants in both conditions received behavioral strategies to assist with smoking cessation based on the most current clinical guidelines during the time that the intervention was completed (USDHHS, 2000). The initial treatment manual for BCT-S was written using an adaption of the empirically supported techniques and the clinical approach specified by BCT (O’Farrell & Fals-Stewart, 2006). The preliminary manual was piloted with five smoking-discordant couples prior to initiation of this study. An iterative treatment development process was conducted in which participants completed brief questionnaires in which they rated session utility, helpfulness, participant motivation, and compliance. Open-ended questions also assessed treatment utility and acceptability of treatment sessions and exercises. Sessions were audiotaped and reviewed by the investigative team to assess the utility, feasibility, and acceptability of the BCT-S treatment components and procedures. Session content for each treatment condition is detailed in Table 1.
Table 1.
Session Content for Treatment Conditions
| Behavioral Couples Therapy- Smoking (BCT-S) |
Individual Standard Treatment (ST) |
|---|---|
| Session 1–7 Content | Session 1–7 Content |
| Review Commitment to Quitting | Review Commitment to Quitting |
| Discussion of motivation to quit. | Discussion of motivation to quit. |
| Couples complete I Quit Contract. | |
| Discussion of Quitting | Discussion of Quitting |
| Review past/current quit strategies with couples. |
Review past/current quit strategies. |
| Effective Use of The Patch | Effective Use of The Patch |
| Review instructions and provide patch. | Review instructions and provide patch. |
|
Couples learn and practice I Quit Discussion. |
Anticipate High Risk Situations |
| Anticipate High Risk Situations | |
| Review withdrawal, cravings, urges. | Review withdrawal, cravings, urges. |
|
Develop coping plan with smoker and partner. |
Develop coping plan. |
| Prepare for Quitting (Session 1) | Prepare for Quitting (Session 1) |
|
Couple exercise: Prepare a Non- Smoking Home. |
Encourage smoker to clean home. |
| Social Support | Social Support |
|
Couple exercise: Social Support Strategies. |
Encourage smoker to obtain support. |
|
Training: Catch Your Partner Doing Something Nice. |
|
| Relaxation Training | Relaxation Training |
|
Couples given brief overview on progressive muscle relaxation. |
Individuals taught extended progressive muscle relaxation technique and a therapist-guided practice. |
| Celebration day (Sessions 3–7) | Reward day (Sessions 3–7) |
|
Couples identify a weekly Celebration Day activity. |
Individuals are encouraged to celebrate their successful quitting. |
| Relapse prevention Skill review. | Relapse prevention Skill review. |
| Handouts Clearing the Air. | Handouts Clearing the Air. |
Two treatment sessions were held prior to the assigned quit date (during the first week of study participation) and the quit date occurred at session 3 for both treatment conditions. We “front-loaded” the treatment schedule during the first few days after the quit attempt - sessions four and five occurred 3 days and 7 days after the quit date, respectively. Session 6 occurred one week later (at 14 days post-quit) and the final session (session 7) occurred 28 days post-quit. Participants were then followed for 6 months post-treatment.
Behavioral Couples Therapy - Smoking (BCT-S)
Participants were provided a BCT-S Couples Workbook that provided an overview of the treatment approach, session format, and all handouts. Motivation for smoking cessation for both the smoker and partner was discussed. The couples completed an I Quit Contract in which the smoker and the partner signed a written agreement detailing their commitment to quitting. Daily I Quit Discussion exercises designed to support the quit attempt were introduced. The couple was asked to role-play during the session, to specify a time each day to perform the I Quit Discussion, and to record the exercise on their study calendar. The smokers were asked to identify strategies that contributed to past successes and relapses and partners were asked about their experiences of either quitting (if a former smoker) or expectations of quitting (if never smoked).
Each couple completed a High Risk Situations Worksheet in which the smoker identified situations that could jeopardize abstinence. The smoker was asked to problem-solve ways to avoid, alter, or use substitutes for cigarettes to cope with the situation and partners were encouraged to offer solutions and helpful support behaviors. The couple agreed on a specific time within 24-hours prior to the assigned quit day to complete the Prepare A Non-Smoking Home exercise. This included discarding all tobacco products and cleaning smoking areas to minimize triggers and smoking cues. Couples were asked to complete a Catch Your Partner Doing Something Nice exercise, which involved surprising one another with praise and/or acknowledgment and they were encouraged to continue this exercise through the week. At subsequent sessions, the therapist congratulated smokers on their success and the couples for their ability to work as a team to achieve the abstinence goal.
The couple was instructed in common withdrawal symptoms and the importance of effective coping via the Support Strategies handout. The couple was asked to: consider behaviors that provided positive support (encouragement) and/or negative support (reminding, questioning); create a menu of support behaviors tailored to reinforce the smoker’s efforts to quit; and consider how they used support behaviors over the prior weeks. Both positive and negative support behaviors were identified and respective utility was discussed. The therapist taught the couples basic communication skills (i.e., active listening) and conflict resolution behaviors to minimize any potential conflict that may have occurred. Participants were provided a brief overview on progressive muscle relaxation and were asked to briefly practice this technique in the session.
Couples were asked to identify a weekly Celebration Day activity to acknowledge successful non-smoking. The couple was also asked to develop shared rewarding activities to complete regularly and plans were developed for the upcoming week. In the final sessions, a relapse Prevention Plan was developed.
Standard Smoking Cessation Treatment (ST)
In the standard condition (ST), smoking cessation treatment was individually delivered and followed guidelines for smoking cessation (USDHHS, 2000). Sessions focused on learning behaviors and skills associated with quitting. Participants received self-help materials that included instructions on how to enlist social support (Orleans et al., 1991) consistent with standard practices used in community smoking cessation programs.
To match on time and attention, the ST condition contained an extended module on relaxation training. In a recent meta-analysis, relaxation training was not shown to be an active treatment component in smoking cessation and did not significantly improve treatment outcomes (Fiore, 2008). The relaxation module included a rationale for relaxation to manage stress while quitting and a therapist-guided progressive muscle relaxation practice during the session. In sessions 2–7, a shortened progressive muscle relaxation protocol was used. The therapist inquired briefly as to the participants’ use of the techniques outside of the session but practice was not assigned.
Follow-up post-treatment
At the last treatment session, participants in both conditions were scheduled for follow-up interviews at 3- and 6-months post treatment, which were conducted with smokers at the study center and via phone for partners. All participants were contacted for follow-up assessment, regardless of degree of session attendance. Smokers and their partners were compensated for all treatment sessions and follow-ups.
Therapist Training
Therapists were required to read literature on BCT (O’Farrell & Fals Stewart, 2006) and to read the Smoking Cessation Clinical Guidelines (USDHHS, 2000). Using BCT-S and ST therapist training manuals, therapists participated in weekly one-hour training sessions for two months prior to randomization. Training included an overview of BCT-S and ST treatment rationale and protocols, review of manuals and handouts, review of taped examples of sessions conducted by the PI for each session, and role-play exercises. In group training, therapists were required to role play each session protocol before participants were assigned to them. The PI and fellow therapists completed Adherence Checklists while each therapist role-played sessions.
Treatment Integrity
Manualized protocols for rating treatment integrity were used for both BCT-S and ST, adapted from the Raters Manual for Project Match Tape Rating Scale and the Yale Adherence and Competence Scale Guidelines (Carroll et al, 2000). In addition to live supervision (role-plays), all sessions were audiotaped (with participant informed consent) and rated by the PI (LaChance) and the research coordinator. Therapists were rated weekly and provided feedback on adherence to manual-specific active components, level of skill across treatments, appropriate structure and focus, and empathy and facilitation of the therapeutic alliance. To monitor treatment implementation, therapists were provided ratings of their adherence and competence. Therapists followed the Adherence Checklist, which outlined each of the critical content topics, during their session administration. The checklists were then reviewed by the research coordinator to ensure the total protocol content was covered in sessions. Therapist audiotapes were reviewed and rated by the PI and research coordinator on the frequency and extensiveness of therapist behaviors and the quality of treatment delivery (i.e., competence).
Measures
At the baseline interview, smokers and their partners each provided demographic and other background information including age, gender, marital status, race/ethnicity, education level, employment status, and income level. Smoking history included number of cigarettes smoked per day, number of years smoked, age of onset of regular smoking, and number of previous lifetime quit attempts. Nicotine dependence (in the smoker) was assessed with the 6-item Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991) with higher scores indicating greater nicotine dependence.
Smoking status
The primary outcome analyses were based on biochemically verified 7-day point-prevalence abstinence (defined as self-reported no smoking for the 7-days prior to the interview date) immediately post-treatment, and at 3- and 6-month follow ups (Hughes, et al., 2004). Self-reported abstinence was verified by expired air breath samples for carbon monoxide (CO), assessed with a Bedfont Scientific Smokelyzer® breath CO monitor, at baseline (both smoker and partner), at each treatment session (smoker only), and at each follow-up interview (smoker only). Detected values above the stated cutoff (> 8 ppm) were considered indicative of smoking (SRNT, Subcommittee on Biochemical Verification, 2002). At 3- and 6-month follow ups (after completion of TNP), point-prevalence was verified by urinary cotinine analysis using the NicAlert Cotinine Test Strips (>3 indicated active smoking; Cooke et al., 2008) for stated abstinence of 7 days. Continuous abstinence was a secondary smoking outcome and was operationalized as the combination of both self-reported abstinence and repeated biochemically-confirmed abstinence at every intermediate time point; from quit day to each subsequent treatment session, to post treatment, and follow ups. In cases where abstinence could not be biochemically verified, participants were characterized as smoking. This occurred in two cases at both post-treatment (PT) and 6 months (M6); at PT, both cases were in the BCT-S condition, at 6M, one case was noted in each condition.
Partner support
The Partner Interaction Questionnaire (PIQ) was used to measure each smoker’s perceived smoking-specific support from his or her partner (Cohen et al., 1990; Mermelstein et al., 1983). This 20-item scale inquires about the support for quitting provided by a spouse or cohabitating partner and includes 10 positive and 10 negative behaviors a partner might perform. The ratio of positive to negative behaviors has been shown to be a better predictor of abstinence than positive or negative behaviors alone and higher ratios have been associated with abstinence (Cohen et al., 1990). Examining the PIQ ratio allowed us to compare partner support across treatment conditions.
The Dyadic Adjustment Scale is a 32-item scale to measure relationship adjustment (DAS; Spanier, 1976) and general relationship functioning with a range of scores from 0 to 151; a higher score indicates greater functioning. We used the DAS to examine whether interpersonal functioning was significantly related to abstinence at 6-months post-treatment.
Data Analysis
Descriptive statistics including means, proportions and standard deviations were calculated for all demographic and clinical characteristics. We used chi-square analyses and t-test statistics to examine between-groups differences in smokers’ and partners’ baseline characteristics. Chi-square tests were used to examine group differences in biochemically confirmed 7-day point prevalence abstinence rates at each time point. Independent t-tests were used to examine differences in continuous abstinence and differences in perceived partner support by treatment condition. Logistic regression was used to determine whether abstinence at six months was associated significantly with DAS score, treatment condition, or perceived smoking-specific partner support. Two-tailed tests and 95% significance levels were used to test for statistical significance. All statistical analyses were performed using Statistical Package for the Social Sciences version 21 (SPSS).
RESULTS
Enrolled smokers were 67% (n =33) male, 87.8% White (n = 43), 4.1% Black (n=2), 2% American Indian/Alaska native (n=1), and 6.1% self-identified as multiracial (n=3). The mean age of the smokers was 42.8 (SD = 11.2) and 26.5% (n = 13) were college graduates. At baseline, participants smoked an average of 18.1 (SD = 5.2) cigarettes per day, had been smoking for an average of 25.8 (SD = 11.9) years, and had a mean FTND score of 4.9 (SD = 1.6). Demographic and clinical characteristics of the 49 smokers (total sample and by treatment condition) are presented in Table 2. At baseline, there were no significant differences in the baseline and demographic characteristics of the smokers between treatment conditions. The partners of enrolled smokers had a mean age of 42.9 (SD = 11.6), were 79.6% White/Caucasian, 46.9% were employed full time, and 31 (63.3%) identified as never smoked.
Table 2.
Baseline demographics (smokers) and comparison across treatment conditions.
| Smokers (N = 49) |
BCT-SC (N = 26) |
IND (N = 23) |
P | |
|---|---|---|---|---|
| Age, years (mean ± SD) | 42.8 ± 11.2 | 42.4 ± 10.6 | 43.2 ± 11.9 | .78 |
| Male gender (N, %) | 33 (67.3%) | 18 (54.5%) | 15 (45.5%) | .76 |
| Married (N,%) | 38 (77.6%) | 20 (52.6%) | 18 (47.4%) | .91 |
| Race, White/Caucasian (n, %) | 43 (87.8%) | 24 (48.9) | 19 (38.8) | |
| Education (n, %) | ||||
| Some high school HS graduate | 2 (4.1) | 6 (12.2) | 9 (18.4) | .85 |
| HS graduate | 6 (12.2) | 20 (40.8) | 14 (28.5) | |
| GED/Some college | 23 (47.0) | |||
| Tech/bus school | 5 (10.2) | |||
| College graduate | 11 (22.4) | |||
| Some graduate school | 2 (4.1) | |||
| Employment (n, %) | 29 (59.2%) | 19 (38.8%) | 15 (30.6) | .68 |
| Full time | ||||
| Household Income (n, %) | 3 (6.1) | .58 | ||
| Less than $29,000 | 5 (10.2%) | 2 (4.0) | 20 (40.8) | |
| $30,000 - $59,000 | 20 (40.8%) | 10 (20.4) | 14 (28.5) | |
| $60,000 – 89,000 | 14 (28.5%) | 7 (14.2) | 10 (20.4) | |
| More than $90,00 | 10 (20.4) | 7 (14.2) | ||
|
Smoking history variables (mean ±SD) |
||||
| Cigs per day | 18.1 ± 5.2 | 17.9 (5.5) | 18.4 (4.8) | .72 |
| Number of years smoked | 25.8 ± 11.9 | 25.2 (10.9) | 26.5 (13.2) | .72 |
| Age started daily cig smoking | 17.2 ± 3.9 | 13.8 (5.3) | 15.2 (4.3) | .30 |
| Nicotine dependence (FTND) | 4.9 ± 1.6 | 5.9 (1.3) | 5.7 (1.6) | .52 |
Biochemically-verified cessation rates were 40.9%, 50% and 45% in the BCT-S arm and 59.1%, 50%, and 55% in the ST arm, at end of treatment, 3-months, and 6-months, respectively. Biochemically confirmed 7-day point prevalence abstinence rates did not differ significantly between treatment arms at any time point (all p > .05; Table 3). Outcomes also did not differ significantly by treatment provider. Smokers in BCT had longer continuous abstinence (M = 60.7 days, SD 66.8) versus in ST (M = 50.3 days, SD 70.8) from quit date through the month six follow up, although the difference was not statistically significant, t(45.5) =.528, p= .60.
Table 3.
Outcomes at follow-up Biochemically-verified 7-day point prevalence abstinence (N, %)
| Intervention (BCT) |
Standard treatment (IND) |
p value | |
|---|---|---|---|
| Post-treatment (N = 49) | 9 (40.9%) | 13 (59.1%) | .12 |
| 3 months (N = 49) | 10 (50%) | 10 (50%) | .72 |
| 6 months (N = 49) | 9 (45%) | 11 (55%) | .35 |
With regard to social support, smokers in the BCT-S condition had a similar PIQ ratio of perceived positive/negative partner support at immediate post-treatment (M = 2.5, SD .81) compared with smokers in the ST condition (M=2.3, SD .92), and this did not differ significantly (t(38) = .67, p= .51). Using regression analyses, verified abstinence at six months was not significantly associated with post-treatment DAS scores (B = -.003, 95% CI [.89, 1.1], p = .96), post-treatment perceived partner support (B = .178, 95% CI [.50, 2.82], p = .69), or treatment condition (B = -.85, 95% CI [.12, 1.54], p = .19).
Treatment satisfaction in both conditions was high (range 1 – 4), however there were no significant differences noted between smokers in the BCT-S (M= 3.55, SD .74) and ST (M=3.78, SD .55) treatment conditions, t(38) = −1.11, p = .27. The mean number of sessions attended out of seven was 6.12 (SD = 2.0) in BCT-S and 6.09 (SD = 1.9) in ST and did not differ significantly between treatment conditions (p = .96).
DISCUSSION
In this study, we developed and conducted a pilot randomized clinical trial of a BCT-based intervention for smoking, which was specifically designed to address limitations of previous studies and test the feasibility of BCT for smoking cessation. Although we were able to implement the intervention, we did not see significant differences in abstinence rates between the intervention and control groups. However, the biochemically-verified cessation rates were high in both treatment conditions, remaining at 45–55% through six months post-treatment. This is noteworthy because although frequent attempts to quit are made, often only a small percentage of smokers (approximately 6%) continue to abstain through 1 year (CDC, 2014). Studies that have combined transdermal nicotine therapy with a behavioral component often report low abstinence rates (18–26%) at follow-up (Fiore et al., 2008).
Our results do suggest that a BCT intervention for smoking cessation is both feasible and acceptable in smoking discordant couples. Notable features of our study results are excellent treatment session attendance and retention, high rates of treatment satisfaction, and overall high rates of confirmed smoking abstinence.
Smokers in the BCT-S condition did not perceive significantly higher positive support from their partners at immediate post-treatment compared with smokers in the ST condition. In a review by Park and colleagues (2012), they reported that only two studies of the eight reviewed demonstrated that partner support was increased after the partner support intervention, and four studies reported no difference in partner support between the intervention and control groups. Additionally, our results did not indicate that perceived partner support was significantly related with 6-month smoking abstinence. When BCT is used with patients with alcohol use disorders (AUD), it has been shown to be clearly more effective than individual treatment at increasing abstinence, and improving relationship functioning (O’Farrell & Schein, 2011; O’Farrell et al., 2010). Perhaps persons with AUD have substantially more relationship dysfunction and partner support issues related to their alcohol use compared with cigarette smokers, therefore substantiating the differences seen in BCT effectiveness with this population.
This study has several strengths. It is the first trial to incorporate and test BCT, an empirically-supported efficacious treatment for substance use disorders, for smoking cessation. It used a rigorous experimental design with a time-matched active control condition. Follow-up rates were high and did not differ by treatment condition. The study provided support for the feasibility and acceptability of BCT-S. Smokers in both groups had remarkable quit rates at immediate post-treatment, which were largely maintained through 6-months post-treatment.
The study had some limitations. This was a pilot trial and therefore was not powered to demonstrate a statistically significant difference between treatment conditions. Kraemer et al. (2006) have suggested that perhaps significance may not be demonstrated in a pilot study, not because the results are clinically non-significant but potentially because the sample sizes are often too small to see statistically significant effects. However, pilot studies remain important in the research process to test the feasibility of new or innovative treatment protocols, to demonstrate the availability of participants for a treatment study, and to train research personnel in new study procedures (Kraemer et al, 2006). In our study, BCT was compared to an intensive active control condition (which included seven treatment sessions and 8 weeks of nicotine replace therapy). This raises the question as to whether involvement in the trial (or assessment alone) increased ST partners’ support for the smokers’ success. This may have contributed to the difficulty in detecting a significant effect related to the treatment condition. If BCT-S had been compared to “usual care”, the effect may have been more robust. Another factor to consider is that smokers in smoking-discordant relationships may in general have higher success rates with cessation attempts (Chandola et al., 2004). Traditionally, research on BCT for substance abuse disorders has excluded dual substance-using couples in order to utilize the non-substance-using partner’s support in modeling and reinforcing abstinence in the using partner (O’Farrell & Schein, 2011). For this reason, we included only smoking-discordant couples in our study. Given that a recent study of BCT reported similar success rates when one or both partners had an AUD (Schumm, O’Farrell, & Andreas, 2012), that tobacco use is highly correlated within couples (Sutton, 1993), and that partner smoking is related to relapse (Kahn, Certain, & Whitaker, 2002), a BCT intervention for couples in which both partners smoke may be warranted. Future research should examine this question. Finally, this pilot study had a fairly homogeneous sample; our inclusion/exclusion criteria were specifically designed to achieve homogeneity and maximize power for treatment development testing (Rounsaville et al., 2001). This may have contributed to our high cessation rates across both treatment conditions. We don’t know how BCT-S would perform in a more heterogeneous sample and subsequent larger scale trials should include more diverse samples.
In sum, this study does not provide evidence of the efficacy of BCT for smoking-discordant couples. Our restricted inclusion/exclusion criteria may have yielded a sample of smokers with a relatively high probability of smoking cessation success and with particularly supportive partners; that is, the relationships of participants may have been sufficiently healthy to preclude benefit from BCT above what could be obtained with an individually focused approach to smoking cessation. Given that BCT is feasible and acceptable for smoking cessation and that BCT has demonstrated efficacy in the treatment of other SUDs, further research may be warranted to determine whether BCT has efficacy in smokers with poorer cessation prognoses, including dual-smoking couples, those with dysfunctional relationships, and smokers with unsupportive partners.
Acknowledgments
We gratefully acknowledge Suzanne Sales for her assistance with data management and data analyses.
FUNDING: This work was supported by the National Institute on Drug Abuse (NIDA) at the National Institutes of Health (Grant number R01 DA021265 to HL). This work was partially supported by NIDA (Grant number T32 DA016184 to PAC), the National Heart Lung and Blood Institute at the National Institutes of Health (Grant number T32 HL076134-07 to ET), and by the Department of Veterans Affairs (TJO).
Footnotes
CONFLICT OF INTERESTS: The authors have no conflicts of interest to disclose.
REFERENCES
- Albertsen K, Borg V, Oldenburg B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Preventive Medicine. 2006;43:291–305. doi: 10.1016/j.ypmed.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Brothers BM, Borrelli B. Motivating Latino smokers to quit: Does type of social support matter? American Journal of Health Promotion. 2011;25:S96–S102. doi: 10.4278/ajhp.100628-QUAN-220. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug & Alcohol Dependence. 57(3):225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults — United States, 2005–2012. Morbidity and Mortality Weekly Report. 2014;63:29–34. Retrieved from http://www.cdc.gov/mmwr. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008;57:1226–1228. Retrieved from http://www.cdc.gov/mmwr. [PubMed] [Google Scholar]
- Chandola T, Head J, Bartley M. Socio-demographic predictors of quitting smoking: how important are household factors? Addiction. 2004;99:770–777. doi: 10.1111/j.1360-0443.2004.00756.x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Lichtenstein E. Partner behaviors that support quitting smoking. Journal of Consulting and Clinical Psychology. 58(3):304–309. doi: 10.1037//0022-006x.58.3.304. [DOI] [PubMed] [Google Scholar]
- Cooke F, Bullen C, Whittaker R, McRobbie H, Chen M, Walker N. Diagnostic accuracy of NicAlert cotinine test strips in saliva for verifying smoking status. Nicotine and Tobacco Research. 2008;10(4):607–612. doi: 10.1080/14622200801978680. [DOI] [PubMed] [Google Scholar]
- Coppotelli HC, Orleans CT. Partner support and other determinants of smoking cessation maintenance among women. Journal of Consulting and Clinical Psychology. 1985;53:455–460. doi: 10.1037//0022-006x.53.4.455. [DOI] [PubMed] [Google Scholar]
- Crispo A, Brennan P, Jöckel KH, Schaffrath-Rosario A, Wichmann HE, Nyberg F, Darby S. The cumulative risk of lung cancer among current, ex-and never-smokers in European men. British Journal of Cancer. 2004;91:1280–1286. doi: 10.1038/sj.bjc.6602078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrick JL, Leonard KE, Homish GG. Perceived partner responsiveness predicts decreases in smoking during the first nine years of marriage. Nicotine & Tobacco Research. 2013;15:1528–1536. doi: 10.1093/ntr/ntt011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EE, McCrady BS, Morgan TJ, Cook SM, Kugler G, Ziedonis D. Couples Treatment for drug-dependent males. Addictive Disorders & Their Treatment. 2007a;6(1):21–37. [Google Scholar]
- Epstein EE, McCrady BS. Couple therapy in the treatment of alcoholism. In: Gurman AS, Jacobson N, editors. Clinical Handbook of Marital Therapy. 3rd. New York: Guilford Publications; 2002. pp. 597–628. [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. May, [Google Scholar]
- Gulliver SB, Hughes JR, Solomon LJ, Dey AN. An investigation of self-efficacy, partner support and daily stresses as predictors of relapse to smoking in self-quitters. Addiction. 1995;90:767–772. doi: 10.1046/j.1360-0443.1995.9067673.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Kahn RS, Certain L, Whitaker RC. A reexamination of smoking before, during, and after pregnancy. American Journal of Public Health. 2002;92:1801–1808. doi: 10.2105/ajph.92.11.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–494. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- May S, West R. Do social support interventions (“buddy systems”) aid smoking cessation? A review. Tobacco Control. 2000;9:415–422. doi: 10.1136/tc.9.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May S, West R, Hajek P, McEwen A, McRobbie H. Social support and success at stopping smoking. Journal of Smoking Cessation. 2007;2:47–53. [Google Scholar]
- Meis LA, Griffin JM, Greer N, Jensen AC, MacDonald R, Carlyle M, Wilt TJ. Couple and family involvement in adult mental health treatment: A systematic review. Clinical Psychology Review. 2013;33:275–286. doi: 10.1016/j.cpr.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Lichtenstein E, McIntyre K. Partner support and relapse in smoking-cessation programs. Journal of Consulting and Clinical Psychology. 1983;51:465–466. doi: 10.1037//0022-006x.51.3.465. [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Cohen S, Lichtenstein E, Baer JS, Kamarck T. Social support and smoking cessation and maintenance. Journal of Consulting and Clinical Psychology. 1986;54:447. doi: 10.1037//0022-006x.54.4.447. [DOI] [PubMed] [Google Scholar]
- O'Farrell TJ, Clements K. Review of outcome research on marital and family therapy in treatment for alcoholism. Journal of Marital and Family Therapy. 2012;38:122–144. doi: 10.1111/j.1752-0606.2011.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Schein AZ. Behavioral couples therapy for alcoholism and drug abuse. Journal of Family Psychotherapy. 2011;22:1–23. [Google Scholar]
- O'Farrell TJ, Murphy M, Alter J, Fals-Stewart W. Behavioral family counseling for substance abuse: A treatment development pilot study. Addictive Behaviors. 2010;35:1–6. doi: 10.1016/j.addbeh.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals Stewart W. Behavioral Couples Therapy for Alcoholism and Drug Abuse. New York, NY: Guilford Publications; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orleans CT, Schoenbach VJ, Wagner EH, Quade D, Salmon MA, Pearson DC, Fiedler J, Porter CQ, Kaplan BH. Self-help quit smoking interventions: effects of self-help materials, social support instructions, and telephone counseling. Journal of Consulting and Clinical Psychology. 1991;59(3):439–448. doi: 10.1037//0022-006x.59.3.439. [DOI] [PubMed] [Google Scholar]
- Park EW, Tudiver F, Schultz JK, Campbell T. Does enhancing partner support and interaction improve smoking cessation? A meta-analysis. The Annals of Family Medicine. 2004;2:170–174. doi: 10.1370/afm.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park EW, Tudiver FG, Campbell T. Enhancing partner support to improve smoking cessation. Cochrane Database of Systematic Reviews. 2012:1–32. doi: 10.1002/14651858.CD002928.pub3. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Baker TB. Any further progress in smoking cessation treatment? Nicotine & Tobacco Research. 2001;3:311–323. doi: 10.1080/14622200110050484. [DOI] [PubMed] [Google Scholar]
- Pollak KI, Mullen PD. An exploration of the effects of partner smoking, type of social support, and stress on postpartum smoking in married women who stopped smoking during pregnancy. Psychology of Addictive Behaviors. 1997;11:182–189. [Google Scholar]
- Pollak KI, Baucom DH, Palmer CA, Peterson BL, Østbye T, Stanton S. Couples' reports of support for smoking cessation predicting women's late pregnancy cessation. American Journal of Health Promotion. 2006;21:90–96. doi: 10.4278/0890-1171-21.2.90. [DOI] [PubMed] [Google Scholar]
- Powers MB, Vedel E, Emmelkamp PMG. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review. 2008;28:952–962. doi: 10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Rayens MK, Hahn EJ, Hedgecock S. Readiness to quit smoking in rural communities. Issues in Mental Health Nursing. 2008;29:1115–1133. doi: 10.1080/01612840802319860. [DOI] [PubMed] [Google Scholar]
- Rayens MK, Hahn EJ, Nicholson D. Psychosocial characteristics of smokers interested in quitting. Journal of Health Psychology. 2011;16:294–302. doi: 10.1177/1359105310373410. [DOI] [PubMed] [Google Scholar]
- Richardson A, Graham AL, Cobb N, Xiao H, Mushro A, Abrams D, Vallone D. Engagement Promotes Abstinence in a Web-based Cessation Intervention: Cohort Study. Journal of Medical Internet Research. 2013;15(1):e14. doi: 10.2196/jmir.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Oncken LS. A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clinical Psychology: Science & Practice. 2001;8:133–142. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schumm JA, O’Farrell TJ, Andreas JB. Behavioral couples therapy when both partners have a current alcohol use disorder. Alcohol Treatment Quarterly. 2012;30:407–421. doi: 10.1080/07347324.2012.718963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales of assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Stanton MD, Shadish WR. Outcome, attrition, and family-couples treatment for drug abuse: A meta-analysis and review of the controlled, comparative studies. Psychological Bulletin. 1997;122:170–191. doi: 10.1037/0033-2909.122.2.170. [DOI] [PubMed] [Google Scholar]
- Sterba KR, Rabius V, Carpenter MJ, Villars P, Wiatrek D, McAlister A. Dyadic efficacy for smoking cessation: preliminary assessment of a new instrument. Nicotine & Tobacco Research. 2011;13:194–201. doi: 10.1093/ntr/ntq236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, DelBoca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol Supplement. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Sutton GS. Do men grow to resemble their wives, or vice versa? Journal of Biosocial Science. 1993;25:25–29. doi: 10.1017/s0021932000020253. [DOI] [PubMed] [Google Scholar]
- Thomas JL, Patten CA, Mahnken JD, Offord KP, Hou Q, Lynam IM, Croghan IT. Validation of the support provided measure among spouses of smokers receiving a clinical smoking cessation intervention. Psychology, Health & Medicine. 2009;14:443–453. doi: 10.1080/13548500903016559. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the surgeon general. 2010 Retrieved from http://www.surgeongeneral.gov. [PubMed]
- United States Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. 2004 Retrieved from http://www.surgeongeneral.gov.
- United States Department of Health and Human Services. Reducing Tobacco Use: Surgeon General Report. 2000 Retrieved from http://www.surgeongeneral.gov.
- Vilchinsky N, Dekel R, Leibowitz M, Reges O, Khaskia A, Mosseri M. Dynamics of support perceptions among couples coping with cardiac illness: The effect on recovery outcomes. Health Psychology. 2011;30:411–419. doi: 10.1037/a0023453. [DOI] [PubMed] [Google Scholar]
- Wei LJ, Lachin JM. Properties of the urn randomization in clinical trials. Controlled Clinical Trials. 1988;9(4):345–365. doi: 10.1016/0197-2456(88)90048-7. [DOI] [PubMed] [Google Scholar]
- Westmaas JL, Bontemps-Jones J, Bauer JE. Social support in smoking cessation: reconciling theory and evidence. Nicotine & Tobacco Research. 2010;12:695–707. doi: 10.1093/ntr/ntq077. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Mattia JI. A self-report scale to help make psychiatric diagnoses: the Psychiatric Diagnostic Screening Questionnaire. Archives of General Psychiatry. 2001;58(8):787–794. doi: 10.1001/archpsyc.58.8.787. [DOI] [PubMed] [Google Scholar]