Abstract
Studies have established that grown children’s problems affect parental well-being, but a dearth of research has addressed daily interactions and biological systems that may underlie these associations. This study examined whether parents have different types of daily interactions with adult children who have problems and whether those interactions are associated with variations in parents’ diurnal cortisol rhythms. Middle-aged parents (n = 197) reported their interactions with adult children for seven consecutive days and provided saliva, analyzed for cortisol, three times a day (wake, 30 minutes after wake, bedtime) for four of those days. Parents were more likely to report negative encounters but not less likely to report positive interactions or contact with adult children who suffered from problems. Interactions with adult children who had physical-emotional problems had more immediate same day associations with cortisol whereas interactions with adult children who had lifestyle-behavioral problems had more delayed, or next day associations with cortisol. Daily interactions and their associations with the hypothalamic-pituitary-adrenal-axis may be important mechanisms by which adult children with problems negatively affect parental well-being.
Keywords: adult children, problems, cortisol, daily diary
1. Introduction
The parent-child tie represents one of the longest-lasting and most emotionally intense social relationships (Hagestad and Uhlenberg, 2007). Across the lifespan, the parent-child relationship involves frequent contact, support exchanges, and both positive and negative emotions (Fingerman et al., 2015). Because this tie is often intimate and involves a great deal of contact, parents are especially distraught when their adult children suffer problems such as disabilities, health problems, and trouble with the law (Birditt et al., 2010). Parents with adult children who have problems report more depressive symptoms, greater negative affect, and poorer parent-child relationship quality (Fingerman et al., 2012; Greenfield and Marks, 2006; Pillemer and Suitor, 1991). Indeed, adult children with problems can have long-lasting detrimental effects on parents’ health and well-being (Seltzer et al., 2011); however, the mechanisms by which adult children suffering problems influence parents’ overall health and well-being are unknown. For example, it is unclear whether parents experience different types of daily interactions with their adult children who suffer problems and whether parents consider all of their interactions (positive and negative) with these children to be more distressing.
The research to date has found that having adult children with chronic mental and physical health problems is associated with parents’ cortisol (Bella et al., 2011; Seltzer et al., 2009; Seltzer et al., 2010). There is less work on adult children’s problems more generally (e.g., financial trouble) and whether interacting with adult children who have physical-emotional problems may be more or less distressing than interacting with adult children who have lifestyle-behavioral problems.
The present study examines daily interactions between parents and their adult children to assess whether the emotional qualities of daily interactions and parents’ biological stress responses provide potential clues regarding how adult children’s problems affect parental well-being. Specifically, we addressed two questions: a) Do parents have different types of daily encounters (e.g., positive, negative) with adult children who have problems than adult children without problems? and, b) Are encounters with adult children who have problems associated with parents’ daily cortisol patterns?
1.1. Adult Child Problems Defined
Adult children may suffer problems across several life domains. Parents tend to report greater negative relationship quality with adult children who have lifestyle-behavioral problems (e.g., trouble with the law, drug addiction) and greater closeness with adult children who have physical or emotional problems (e.g., cancer, anxiety disorder) (Pillemer and Suitor, 2002; Suitor and Pillemer, 2000; Suitor et al., 2006). Theorists have suggested that parents may blame their adult children for having lifestyle-behavioral problems whereas physical-emotional problems are perceived as less controllable (Suitor et al., 2006). In the present study we distinguish between these types of problems. Physical-emotional problems include physical and mental health problems as well as developmental disabilities; lifestyle-behavioral problems include financial trouble, drug and alcohol abuse, trouble with the law, and serious relationship trouble (e.g., divorce).
1.2. Theoretical Model
This study used the exposure-reactivity model, which suggests that health varies as a function of both exposure and reactivity to stressors, as a framework for understanding daily interactions with adult children and their implications for cortisol (Almeida, 2005). Parents with adult children who have problems may be exposed to different types of experiences and interactions with these children. Specifically, parents may experience more negative and fewer positive daily interactions with their adult children with problems. Thus, we first considered whether parents had any contact with an adult child suffering problems that day. We also specifically examined: a) positive interactions and b) negative interactions with adult children in order to understand whether parents interact differently with adult children who suffer with problems than with adult children who do not suffer from problems. Examining daily interactions may provide accounts of relationship quality that are less biased by retrospective recall problems and other cognitive biases (e.g., tendency to remember more positive than negative information with age (Reis, 2012; Thomas and Diener, 1990). Thus, we assessed parents’ interactions with adult children close to the time the events occurred to capture negative as well as positive events.
Parents may also react differently to interactions with adult children who suffer problems compared to adult children who do not suffer problems. Although stress reactivity often refers to the measurement of acute cortisol responses in a more controlled laboratory setting, the present study defines reactivity in terms of links between daily social interactions and diurnal cortisol production, a primary indicator of the function of the hypothalamic pituitary adrenal axis (HPA axis; Friedman et al., 2012; Sapolsky et al., 2000; Selye, 1979). Cortisol has a normal diurnal rhythm which begins to increase before waking, reaches a peak level at about 30 minutes after waking (cortisol awakening response [CAR]) and steadily declines thereafter until bedtime (daily decline [DEC] (Fries et al., 2009). Higher cortisol levels over the course of the day are associated with greater negative emotion (e.g., anger, stress, anxiety) and poorer well-being (Adam et al., 2006; Marin et al., 2007). After repeated or chronic stress, individuals show flatter CAR and DEC (Miller et al., 2007). Thus, both hypo and hyper cortisol responses are indicative of poor health. The CAR is often not correlated with daytime cortisol activity (Edwards et al., 2001; Schmidt-Reinwald et al., 1999), indicating that the CAR and daytime cortisol secretion might be influenced by different factors (Clow et al., 2004). In addition, diurnal cortisol rhythms are associated with later negative physical and mental health outcomes (Adam et al., 2010). We therefore consider overall cortisol level, CAR, and DEC.
1.3. Daily Interactions with Adult Children who have Problems
Adult children’s problems have been linked to relationship qualities with parents. For example, mothers reported greater ambivalence (both positive and negative sentiments) regarding adult children with more problems (Pillemer et al., 2007). Birditt et al. (2010) found that parents reported more negative relationships with adult children who suffered problems but reported no less positive quality ties with those offspring. Other studies suggest that parents differentiate between types of problems. For example, Suitor and Pillemer (2000) found that mothers reported greater closeness with adult children who suffered from health problems and less closeness and more conflictual ties with adult children who suffered from lifestyle-behavioral problems (e.g., substance abuse, trouble with the law). We examined whether parents report different types of daily interactions with adult children who suffer from problems (e.g., physical-emotional, lifestyle-behavioral problems) compared to adult children who did not suffer from problems.
1.4. Daily Interactions with Adult Children with Problems and Cortisol
Studies have linked parental well-being to adult children’s problems (Fingerman et al., 2012; Umberson et al., 2010). Parents may be sensitive to their adult children’s problems due to their investment in raising them, their empathy with their child’s distress, or due to conflict and tensions in their relationship associated with those problems. Moreover, parents typically have frequent contact with their adult children, daily or several times a week (Birditt & Fingerman, 2012; Fingerman et al., in press). It is likely that daily encounters with adult children who suffer problems may be a source of stress, and in turn, these encounters may have ramifications for parents’ cortisol.
Research that has considered associations between adult children’s problems and parental cortisol has focused on adult child mental and physical health problems. Parents with adult children who suffered severe mental health problems (e.g., bipolar, major depression, schizophrenia) showed a hypoactive cortisol response to daily stress (Barker et al., 2012); more stressful days were associated with a flatter awakening response and a flatter decline on the next day. Similar findings were reported among parents of adult children with cerebral palsy, disabilities, and autism (Bella et al., 2011, Seltzer et al., 2009; Seltzer et al., 2010). We know little, however, about whether daily interactions with adult children who suffer from a wider range of physical-emotional and/or lifestyle-behavioral problems are associated with parents’ cortisol.
1.5. Other Factors Associated with Cortisol
We considered several additional factors that may influence interpersonal interactions and cortisol including gender, years of education, race, neuroticism, anxiety, depressive symptoms, and number of living children (Almeida, 2005; Birditt et al., 2011; Steptoe et al., 2003). We also controlled for several factors that may influence cortisol levels including medications (e.g., steroids, birth control), smoking, whether the data were collected on a weekend, and sleep quality (Hansen et al., 2012; Stawski et al., 2013).
1.6. Present Study
Examining parents’ daily interactions and biological stress responses provides an important first step for understanding the link between adult children with a range of problems and parental well-being. We addressed the following research questions:
-
a)
Do parents have different types of daily interactions with adult children who have health and lifestyle-behavioral problems compared to adult children who do not have problems? We predicted that parents would report more negative interactions and fewer positive interactions with adult children who had problems compared to adult children who did not have problems.
-
b)
Are daily interactions with adult children who have health or lifestyle-behavioral problems associated with variations in cortisol? We predicted that parents would have higher cortisol and flatter diurnal cortisol rhythms (CAR, DEC) on days in which they had interactions with adult children who had health or lifestyle-behavioral problems compared to days they did not have interactions with adult children who had these problems.
2. Method
2.1. Sample
Participants were middle-aged adults from the Family Exchange Study Wave 2 conducted in 2013. The sample was recruited from the Philadelphia Metropolitan Statistical Area (PMSA) and participated in Wave 1 in 2008. Initial criteria required middle-aged adults to have at least one living parent and one child over age 18. In Wave 2, following completion of a one-hour main survey, a random selection of participants was invited to complete a diary study consisting of brief telephone interviews for 7 evenings. Of those invited, 87% (n = 270) accepted the invitation and 248 participants completed daily interviews before the study was closed. During the diary calls, participants were also invited to participate in saliva collection. The study received approval from the institutional review boards of the universities involved in the project and all procedures were carried out with the adequate understanding and verbal consent of the subjects in accordance with the Declaration of Helsinki.
Collection kits with salivettes to collect saliva were mailed to respondents after they completed a main interview and scheduled their first diary call. Interviewers prompted respondents to collect the saliva on days 2–5 of the diary calls, though allowances were made for deviations from this schedule. Participants were instructed to provide samples when they woke and before they got out of bed, 30 minutes after waking, and before bed and not to eat or drink anything other than water 30 minutes before collecting their samples and particularly to avoid caffeinated products (e.g., coffee, tea, soda). Participants were also instructed not to brush their teeth before providing the 30 minute sample. Participants recorded the time of collection on the tubes and on a daily log. In addition, during the diary call on saliva collection days, respondents were asked to report their collection times and if they had any problems. In the event there were inconsistencies, we used all three data collection time reports (tube, log, interview) to discern the most likely time the saliva was collected. Participants were reminded to store samples in the refrigerator and given instructions and a prepaid express envelope for returning the samples at the end of collection. Participants received $50 for completing the surveys and $50 for providing saliva samples.
A total of 203 participants provided saliva samples. We excluded six participants from the analysis (night shift workers n = 2; participants who did not have any valid saliva samples n = 3; a participant who did not have any living offspring n = 1); therefore, 197 participants (55% women) were analyzed. Table 1 includes participant demographics. Participants had an average of 14.50 years of education (SD = 2.04) and were aged 56.31 (SD = 4.78) on average with an age range from 45 to 65. Participants had an average of 2.6 children aged 18 or older (SD = 1.40; range 1 to 11), and 40% of the participants had at least one adult child living with them. Adult children were on average age 28.56 (SD = 6.73; range 18 to 50) and were 51% female. Participants completed 5 to 7 daily diary interviews with a mean of 6.83 interviews (SD = 0.45); 86% of participants completed all seven days of diaries. Participants provided saliva on average 3.96 (SD = 0.26) of the diary days. A total of 192 participants (97.5%) provided saliva on all four days.
Table 1.
Sample Characteristics
| M (SD) | Range | % (n) | |
|---|---|---|---|
| Parent characteristics | |||
| Age | 56.3 (4.8) | 45–65 | |
| Female | 54.8% (108) | ||
| Education | 14.5 (2.0) | 10–17 | |
| # of adult children | 2.6 (1.4) | 1–11 | |
| White | 73.6% (145) | ||
| Neuroticism | 2.6 (0.7) | 1–4.5 | |
| Anxiety | 13.7% (27) | ||
| Depression | 1.5 (0.6) | 1–4 | |
| Live with adult child(ren) | 39.6% (78) | ||
| Child characteristics | |||
| Child(ren) with physical-emotional problem(s) | |||
| Developmental delay | 12.2% (24) | ||
| Physical disability | 8.7% (17) | ||
| Serious health problem/injury | 15.8% (31) | ||
| Emotional/psychological | 20.0% (39) | ||
| Child(ren) with lifestyle-behavioral problem(s) | |||
| Drinking/drug | 10.7% (21) | ||
| Financial | 41.3% (81) | ||
| Trouble with law | 13.8% (27) | ||
| Divorce/relationship trouble | 23.1% (45) | ||
2.2. Cortisol
Saliva samples were frozen and stored at −80 degrees C until analysis. After thawing, salivettes were centrifuged at 3,000 rpm for 5 minutes, which resulted in a clear supernatant of low viscosity. Salivary concentrations, reported in nmol/l, were measured using commercially available chemiluminescence immunoassay with high sensitivity (IBL International, Hamburg, Germany). The intra and interassay coefficients for cortisol were below 8%.
Duplicate assays were conducted with 25% of the samples (n = 194 wake samples, n = 195 30 minute samples, n = 190 bedtime samples) to establish reliability. Intraassay coefficients of variation were calculated (i.e., SD of the two samples divided by the mean of the samples) for each occasion (wake, 30 minutes after wake, bed). The range for the wake and 30 minute intraassay coefficient of variation was 0.00 to 0.16 (M = 0.04, SE = 0.03) and the range for the bedtime sample was 0.00 to 0.24 (M = 0.07, SE = 0.04), indicating excellent reliability.
Cortisol values were removed on a daily basis from the analysis for the following reasons (Table 2): participants did not complete a daily interview, participants did not indicate time of sample collection, at least one cortisol value was over 60, respondents were awake fewer than 12 hours or more than 20, and there was less than 15 or more than 60 minutes between the waking cortisol and the 30 minute cortisol. Of the total 759 days with useable saliva data, 97 were removed from the analysis (12.8 % of the total days). We assessed both the skew and kurtosis of each cortisol value; the natural log was calculated for all cortisol scores due to non-normal distributions in the bedtime cortisol. Distributions of cortisol were checked after the natural log transformation and the skew and kurtosis values were in the acceptable range (less than 3 for skew and less than 9 for kurtosis).
Table 2.
Descriptives for Cortisol Data among Parents
| Time | Cortisol (nmol/l) | Cortisol (natural log) | |||||
|---|---|---|---|---|---|---|---|
| Occasion | M | SD | M | SD | Median | M | SD |
| Wake | 6.43 a.m. | 83 min | 21.50 | 10.88 | 19.48 | 2.93 | 0.57 |
| 30 minutes after wake | 7.16 a.m. | 83 min | 29.59 | 11.94 | 28.78 | 3.29 | 0.50 |
| Bedtime | 11.05 p.m. | 73 min | 4.80 | 5.22 | 3.21 | 1.24 | 0.75 |
Notes. Participant N = 197; Day N = 662.
Participants provided a total of 759 days of useable cortisol data. We removed a total of 97 days of data due to the following: Days without a completed daily interview (n = 1), days with values over 60 nmol/l (n = 50), days with missing time (n = 16), days in which participant was awake less than 12 hours or more than 20 hours (n = 16), and days in which the 30 minute cortisol sample was taken less than 15 minutes after wake or more than 60 minutes after wake (n = 18).
We compared diary participants who provided useable saliva data (n = 197) with those who did not provide useable saliva data (n = 51). A series of t-tests (for continuous variables) and χ2 tests (for categorical variables) revealed no significant differences in participant characteristics (i.e., race, gender, education, neuroticism, depressive symptoms, anxiety) or in the number of adult child problems between individuals who provided useable saliva and individuals who did not provide useable saliva.
2.3. Adult Child Problems
Consistent with past work (Birditt et al., 2010; Greenfield and Marks, 2006), participants answered a series of yes/no questions regarding personal problems for each of their offspring aged 18 and older. We coded problems into two categories. Physical-emotional problems included: an ongoing developmental delay or disability, an ongoing physical disability, a serious health problem, and a serious emotional or psychological problem in the past two years. Lifestyle-behavioral problems included: a drinking or drug problem, financial problems, trouble with the law or police, and divorce or other serious relationship problems in the past two years (Birditt et al., 2010). We dichotomized the scores so that offspring received a 0 if they had no problems and a 1 if they had one or more problems. Thus, each child had two dichotomous scores: lifestyle-behavioral problem and physical-emotional problem. We conducted sensitivity analyses to assess whether adult children with two or more problems were associated with different results and the results were consistent.
2.4. Daily Interactions
Participants answered a series of questions about their interactions with each of their adult children on each day on the following dimensions.
Contact
First, participants indicated whether they had any contact with each of their adult children that day (by phone, email, in person). Each adult child received a 0 (did not have contact) or 1 (had contact) for each day.
Positive interactions
For each adult child participants were asked: “Did you have any positive interactions since (this time/we spoke) yesterday—that is interactions that brought you pleasure or enjoyment or made you feel good?” and “Since (this time/we spoke) yesterday did you share a good laugh?” Each adult child received a 0 (did not have a positive interaction) or 1 (had a positive interaction) for each day.
Negative interactions
Participants were asked two items regarding negative interactions with each adult child: “Did you have any interactions that made you feel irritated, hurt or annoyed?” And “Did you have any interactions in which you could have felt irritated, hurt or annoyed but decided not to be?” Each adult child received a 0 (did not have a negative interaction) or 1 (had a negative interaction) for each day.
2.5. Covariates
We controlled for several parent characteristics including gender (0 = mother, 1 = father), years of education, race (0 = white, 1 = non white), neuroticism, anxiety, depressive symptoms, and number of living children. To assess neuroticism, participants rated the extent to which four characteristics described them (i.e., moody, worrying, nervous, calm (reverse coded)) from 1 (not at all) to 5 (a great deal) (Lachman and Weaver, 1997). An average was created of the four items (α = .67). Participants reported their depressive symptoms with five items from the Brief Symptom Inventory (BSI; Derogatis and Melisaratos, 1983). Participants were asked to report the extent to which they experienced the following symptoms during the last 7 days from 1 (not at all) to 5 (extremely): feeling lonely, blue, no interest in things, hopeless about the future, and feelings of worthlessness. Items were averaged to create a depressive symptoms score (α = .82). Participants reported their anxiety with five items from the patient health questionnaire (Spitzer et al., 1994). Participants were asked whether they experienced an anxiety attack within the past 4 weeks. If so, they were asked four follow-up questions regarding their anxiety. An individual is considered to have an anxiety disorder if he/she answers “yes” to one of the follow-up questions such as “Did this attack bother you a lot or are you worried about having another attack?”
We also controlled for factors that are known to influence cortisol patterns. Each day participants indicated yes (1) or no (0) to whether they were taking the following medications: over the counter/prescription allergy medication, steroid inhaler, other steroid medication, medications/creams containing cortisone, birth control pills, other hormonal medications, or anti-depressants or anti-anxiety medication. We summed the number of these medications. We also controlled for smoking on the particular day (0 = did not smoke, 1 = yes, smoked cigarettes) and whether the data were collected on a weekend day (0 = weekday, 1 = weekend day). Finally, participants rated the quality of their sleep on the night before from 1 (poor) to 5 (excellent).
2.6. Analysis Strategy
Because the data included multiple observations for each respondent (e.g., multiple children, multiple days, multiple within-day cortisol assessments), we used multilevel models to analyze the data. Multilevel models are ideal when data are nested and unbalanced (e.g., unequal numbers of observations per respondent).
Three-level models were estimated to examine whether parents reported different types of daily encounters with adult children who had physical-emotional problems and lifestyle-behavioral problems. We estimated models using the SAS GLIMMIX macro with binomial outcomes. Because participants could report on multiple adult children for each day they participated in the diary study, models included days nested in offspring nested in participants. The models included two random effects for the intercepts. We examined physical-emotional and lifestyle-behavioral problems as predictors in three separate models predicting any contact, positive interactions, and negative interactions. Models controlled for gender, education, depressive symptoms, anxiety, neuroticism, and family size. All upper level continuous variables were grand mean centered and lower level continuous variables were group mean centered. Thus, each model assessed whether participants were more likely to have each type of daily interaction with adult children who had a lifestyle-behavioral problem or a physical-emotional problem.
Next, we considered whether daily encounters with adult children were associated with cortisol. We examined social encounters with two types of adult children: a) adult children who had physical-emotional problems and b) adult children who had lifestyle-behavioral problems. We estimated three-level piecewise multilevel models to assess whether cortisol rhythms varied by daily encounters (SAS PROC MIXED). The lowest level referred to the cortisol measurement within day, the second level referred to the day, and the upper level referred to the participant. For these models we collapsed across all adult children and used scores that reflected whether the respondent interacted with an adult child with a physical-emotional problem, and or an adult child with a lifestyle-behavioral problem on the particular day. We estimated models separately for each type of interaction (contact, positive interaction, negative interaction) and each type of problem (physical-emotional, lifestyle-behavioral; total of six models). Piecewise models capture the within-day patterns of cortisol with two predictors (i.e., pieces) that represented the CAR (time difference between waking and 30 minute collection) and the daily decline (time difference between 30 minute collection and bedtime collection) centered on the 30 minute collection. Based on a comparison of models the best fitting model included a random effect for the intercept at the upper level and at the second level. Models also included a quadratic effect for the daily decline. Additional models were estimated to assess whether the quadratic effect of daily decline varied by interactions but since those estimates were not significant they were removed from the model.
In step 1 we included the main effects of daily social encounters to assess whether social encounters with adult children predicted overall cortisol levels and in step 2 we included the pieces (CAR, DEC) and the daily encounters to assess links between daily encounters and the diurnal cortisol curve over the day. The predictors included same day interactions as well as interactions on the day before. For example, to assess whether negative interactions with adult children with physical-emotional problems were associated with cortisol, we estimated models with two dichotomous predictors: same day negative interaction with an adult child who suffered from a physical-emotional problem and previous day negative interaction with an adult child who suffered from a physical-emotional problem. Models controlled for gender, education, neuroticism, family size, medication use, wake time, smoking, and whether the data were collected on a weekend. All upper level continuous variables were grand mean centered and lower level continuous variables were group mean centered.
3. Results
Most parents (64%) reported having at least one adult child with a problem, 34% of parents reported that all of their adult children had at least one problem, and 37% reported that none of their adult children had problems. An examination of the percentage of parents with one or more adult child with each type of physical-emotional and lifestyle-behavioral problem revealed that the most commonly reported problems in each of the categories were emotional/psychological problems and financial, respectively (Table 1).
Of the total diary days completed (N = 1,345), 76% (n = 1,022) included contact with an adult child and 40% (n = 542) included contact with an adult child who had at least one problem. When considering the type of problems separately, 23% (n = 315) of total diary days included an interaction with an adult child with physical-emotional problems and 31% (n = 417) included interactions with an adult child with lifestyle-behavioral problems. See Table 3 for descriptive statistics.
Table 3.
Percentage of Diary Days including Each Type of Interaction by Type of Adult Child
| All adult children % |
Adult Children with physical-emotional problems % |
Adult Children with Lifestyle-behavioral problems % |
|
|---|---|---|---|
| Any contact | 76 | 23 | 31 |
| Positive interactions | 65 | 18 | 25 |
| Negative interactions | 16 | 6 | 7 |
Notes. Participant N = 197; Day N = 1,345.
Numbers reflect the percentage of diary days that included each type of interaction. For example parents had contact with at least one adult child on 76% of the diary days.
Most participants had a normal diurnal cortisol rhythm characterized by a rise in the morning and a decline over the course of the day. See Table 2 for descriptives for the cortisol values for each time point.
3.1. Do Parents Have Different Types of Daily Interactions with Adult Children who Have Problems?
We considered whether physical-emotional problems and lifestyle-behavioral problems suffered by adult children differentially predicted the likelihood of having any contact, positive interactions, and negative interactions (Table 4). Parents were more likely to report negative interactions with adult children who had physical-emotional and lifestyle-behavioral problems. Parents were no more or less likely to have contact or positive interactions with adult children who had problems.
Table 4.
Multilevel Model Predicting Likelihood of Each Type of Interaction as a Function of Adult Child Having a Physical-Emotional or Lifestyle-Behavioral Problem
| Contact | Positive interactions |
Negative interactions |
|
|---|---|---|---|
| Problems | |||
| Physical-emotional | 0.39 | 0.20 | 0.79 ** |
| Lifestyle-behavioral | 0.07 | 0.01 | 0.57 * |
Notes. Models controlled for gender, neuroticism, number of children, education, race, anxiety, and depressive symptoms.
p ≤ .05.
p ≤ .01.
3.2. Are Interactions with Adult Children who Have Problem Associated with Variations in Cortisol?
First, a model was estimated to examine the average CAR, DEC and overall levels of cortisol controlling for covariates. Because the model was centered on the 30 minute collection, the CAR is negative but actually reflects an increase in cortisol over time. These models showed that cortisol increased between the wake and 30 minute collection (b = −0.63; p < .01) and declined until bedtime (b = −0.32, p < .01).
Next, we assessed whether interactions with adult children who had specific types of problems were associated with cortisol. Interactions with adult children who had physical-emotional problems were associated with cortisol (Table 5). Having any contact with an adult child who had a physical-emotional problem was associated with higher cortisol on the same day compared to not having contact with an adult child who had a physical-emotional problem. Negative interactions with adult children who had physical-emotional problems were also associated with same day steeper daily decline compared to not having a negative interaction with an adult child with a physical-emotional problem. Positive interactions with adult children who had physical-emotional problems were not associated with same day or next day cortisol.
Table 5.
Daily Interactions with Adult Children and Parents’ Diurnal Cortisol Rhythms
| Children who have P.E. problems | Children who have L.B. problems | |||||||
|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 1 | Step 2 | |||||
| INT | INT | CAR | DEC | INT | INT | CAR | DEC | |
| Any contact | ||||||||
| Same day interaction | 0.11* | 0.09 | 0.14 | −0.00 | −0.02 | 0.02 | −0.13 | −0.00 |
| Previous day interaction | 0.04 | 0.11 | −0.22 | −0.01 | 0.02 | 0.04 | 0.01 | −0.00 |
| Positive interactions | ||||||||
| Same day interaction | 0.07 | 0.05 | 0.17 | −0.00 | −0.03 | 0.00 | −0.09 | −0.00 |
| Previous day interaction | 0.00 | 0.04 | −0.21 | 0.00 | 0.02 | 0.04 | −0.02 | −0.00 |
| Negative interactions | ||||||||
| Same day interaction | 0.01 | 0.10 | 0.19 | −0.03** | 0.00 | 0.03 | 0.03 | −0.01 |
| Previous day interaction | 0.07 | 0.12 | −0.15 | −0.01 | 0.18** | 0.19* | 0.09 | −0.01 |
Notes. P.E. = physical-emotional; L.B. = lifestyle-behavioral; INT = intercept; CAR = cortisol awakening response; DEC = daily decline. Models include the quadratic decline and controlled for gender, neuroticism, number of children, education, weekend day, wake time, medication use, race, anxiety, depressive symptoms, sleep quality the night before, and smoking.
p ≤ .05.
p ≤ .01.
Interactions with adult children who had lifestyle-behavioral problems were also associated with cortisol (Table 5). Negative interactions with adult children who had lifestyle-behavioral problems were associated with higher cortisol on the next day compared to not having an interaction with an adult child who had a lifestyle-behavioral problem. Contact and positive interactions with adult children who had lifestyle-behavioral problems were not associated with same day or next day cortisol.
3.4. Post Hoc Analyses
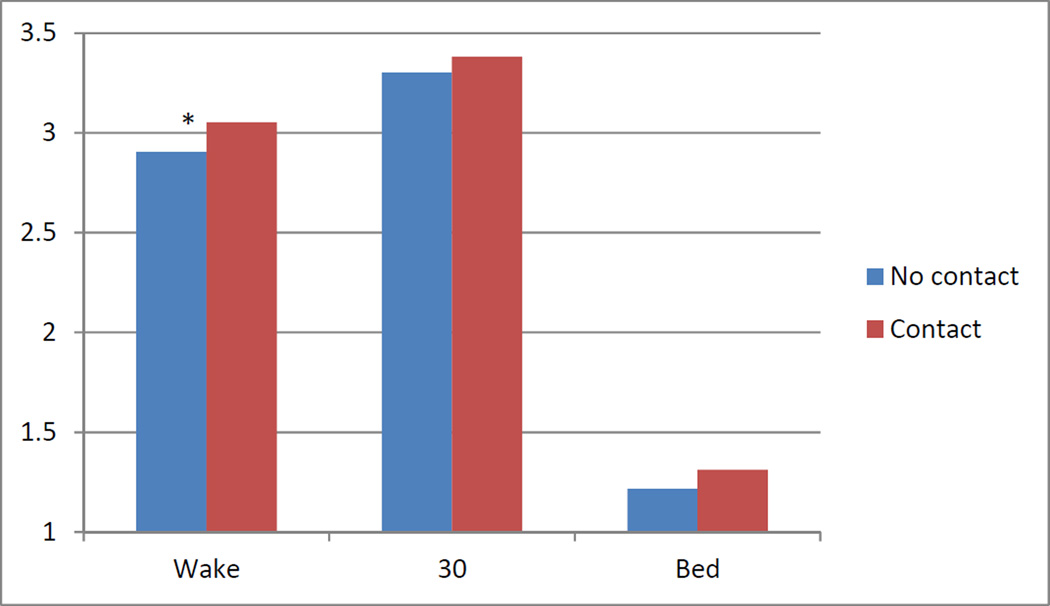
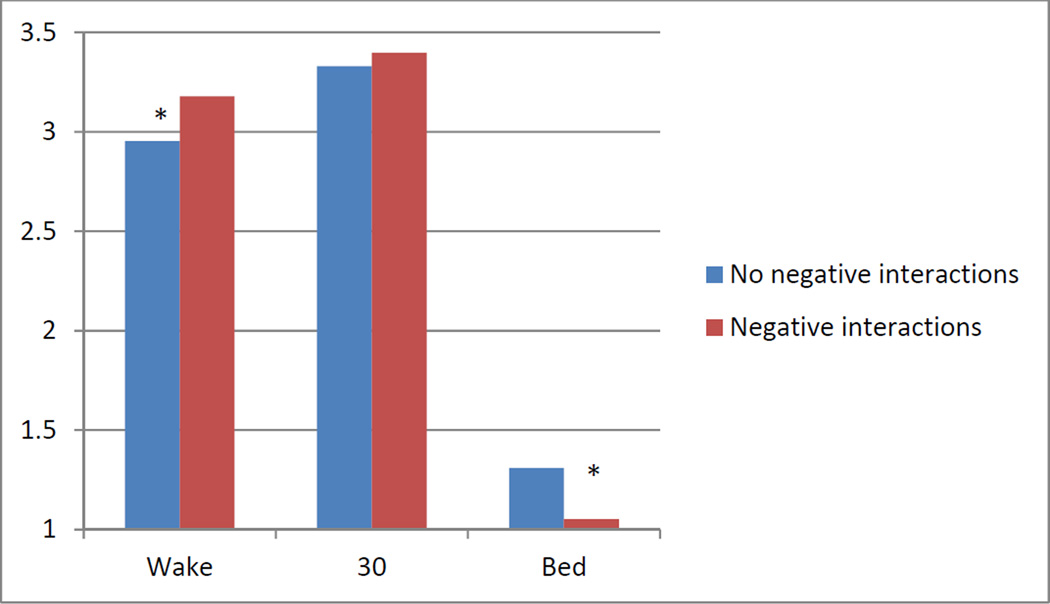
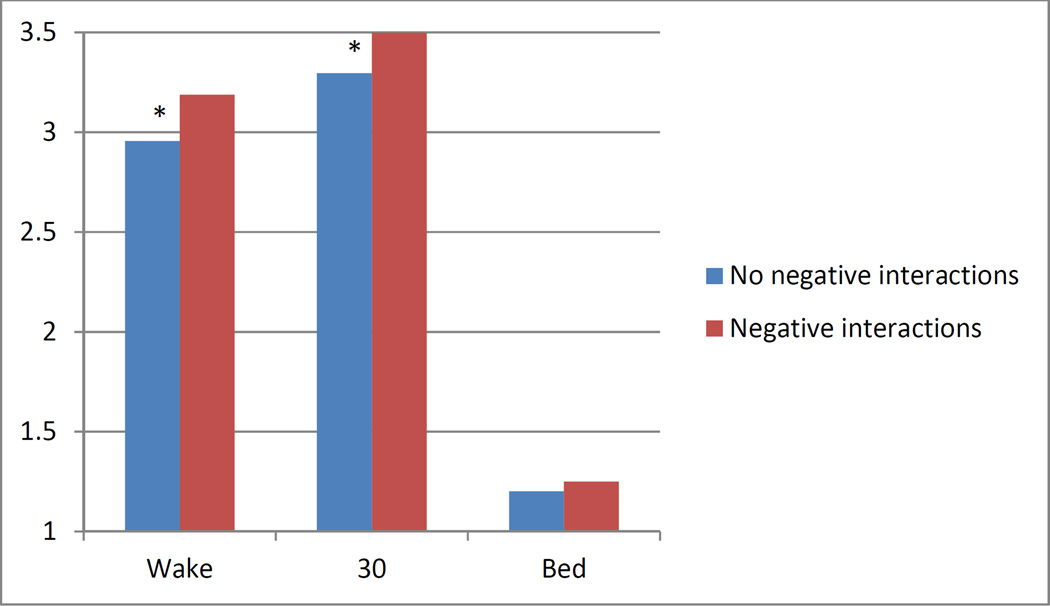
We conducted a series of post hoc analyses to examine associations between interactions with adult children with problems and each of the cortisol measurements (waking, 30 minutes after waking, bedtime) separately along with estimates of the mean cortisol levels in order to understand whether interactions with adult children who suffer problems were associated with elevated values at particular times of the day. This was especially relevant given the associations between daily interactions and steeper rather than flatter cortisol declines. Contact with adult children who had physical-emotional problems was associated with higher same day cortisol at waking (Figure 1). Negative interactions with adult children who had physical-emotional problems were associated with higher waking and lower bedtime cortisol on the same day (Figure 2). Negative interactions with adult children who had lifestyle-behavioral problems were associated with higher waking cortisol and 30 minutes after waking cortisol on the next day (Figure 3).
Figure 1.
Estimated means of cortisol by having at least one contact with an adult child with a physical-emotional problem on the same day *p ≤ .05.
Figure 2.
Estimated means of cortisol by having at least one negative interaction with an adult child with a physical-emotional problem on the same day *p ≤ .05.
Figure 3.
Estimated means of cortisol by having at least one negative interaction with a child with a lifestyle-behavioral problem on the previous day *p ≤ .05.
Finally, we estimated additional models to examine whether negative experiences were buffered by positive experiences. We did this by including interactions between negative encounters and positive interactions predicting overall cortisol. Interestingly, the association between negative encounters with adult children who had physical-emotional problems and cortisol was moderated by having positive interactions with these children. Parents who reported having a negative encounter in the absence of positive encounters had the highest cortisol levels whereas having both positive and negative interactions with these children was associated with lowest levels of cortisol. However it is important to note that the experience of negative interactions in the absence of positive interactions was relatively rare (n =14 days) compared to having both types of encounters on the same day (n = 69 days). There was no evidence that negative interactions with adult children who had lifestyle-behavioral problems were moderated by positive interactions with those adult children.
4. Discussion
A burgeoning literature shows that adult children with problems have lasting negative effects on parents’ health and well-being. We specifically explored whether parents have different types of daily interactions with adult children who have problems and whether interactions with adult children who suffer from problems are differentially associated with daily cortisol rhythms. Parents reported more negative encounters with adult children with problems but no fewer positive interactions or less contact. Interestingly, interactions with adult children who had physical-emotional problems had more immediate same day associations with cortisol whereas interactions with adult children who had lifestyle-behavioral problems had more delayed, or next day associations with cortisol.
4.1. Daily Interactions with Adult Children who Have Problems
The first aim of this study was to examine whether parents have different types of interactions with their adult children who have problems. Previous literature examining parents’ overall perceptions of relationships with their adult children has shown that parents report more negative quality ties with children who have problems but no less positive feelings toward these children (Birditt et al., 2010). This study confirmed these associations at the daily level. Parents were more likely to have negative interactions with adult children who had lifestyle-behavioral and/or physical-emotional problems but there were no associations between problems and positive interactions or contact. This finding is important because daily interaction data often do not confirm retrospective or overall reports (Charles et al., 2015). Daily interaction data are often considered more accurate because they are less affected by biases in reporting (Reis, 2012). In addition, this study showed that there were no differences in the types of daily interactions parents reported with adult children who had lifestyle-behavioral vs. physical-emotional problems (Suitor et al., 2006). This is somewhat surprising given the research indicating that lifestyle-behavioral problems are associated with worse parent-child relationship quality than physical-emotional problems (Pillemer and Suitor, 1991).
4.2. Interactions with Adult Children who Have Problems and Diurnal Cortisol Rhythms
Overall, interactions with adult children with physical-emotional problems tended to have same day associations with cortisol whereas interactions with adult children with lifestyle-behavioral problems were associated with more delayed effects on cortisol on the next day. Having contact with adult children who had physical-emotional problems was associated with higher cortisol overall and negative interactions with these children predicted steeper declines. Post hoc tests revealed that contact with these children predicted higher waking cortisol and that negative interactions predicted higher waking and lower bedtime cortisol. It is interesting that daily encounters with these children were associated with higher waking cortisol which most likely occurred prior to the interaction. Previous research shows this same effect with regard to events that are highly anticipated (Fries et al., 2009). People tend to have higher morning cortisol before they compete, for example (Rohleder et al., 2007). Thus, parents may be anticipating stressful interactions with adult children who have physical-emotional problems which may be associated with an increase in cortisol. However, it is also possible that higher levels of cortisol lead to more negative interactions due to increased sensitivity or negative mood, for example. The findings regarding same day steeper declines and lower bedtime cortisol on days in which parents had negative interactions with these children imply that parents may experience some solace from contact with children regardless of the quality of those interactions.
In contrast, interactions with adult children who had lifestyle-behavioral problems were associated with next day rather than same day cortisol. In particular, negative interactions were associated with higher cortisol overall on the next day. Post hoc tests revealed that parents had higher wake and 30 minute cortisol on days after they had negative interactions with adult children who had these problems. Thus, in the case of lifestyle-behavioral problems parents’ negative interactions with adult children appear to result in a higher next day cortisol, which may reflect worries and preoccupation with these children that persist into the next day. This finding is in line with our prior work which shows that stressful thoughts (e.g., worries) regarding grown children predict increased negative mood (Fingerman et al., in press).
In sum, although daily interactions did not vary by type of adult child problem (e.g., lifestyle-behavioral vs. physical-emotional), differences were found at a biological level, which may lead to a more nuanced understanding of how adult children’s problems are associated with parents’ health and well-being. These results have some implications for practice. Because lifestyle-behavioral problems are associated with more delayed effects on cortisol, parents with adult children who have these types of problems may need to learn effective coping strategies for reducing stress. In contrast, for parents with children who have physical-emotional problems, parents may need to develop strategies for reducing the anticipation of stress. Another approach may be for parents to balance negative interactions with more positive exchanges, which appear to buffer the effects of the negative interactions with these adult children on cortisol. Similarly our prior work shows that negative interactions with grown children are buffered by positive interactions when predicting with daily mood (Fingerman et al., in press).
4.3. Limitations and Future Directions
There are limitations to the present study that should be addressed in future work. First, parents’ cortisol levels may be affecting the types of interactions that they have with their adult children. Furthermore, although we controlled for many individual differences (neuroticism, anxiety, depressive symptoms) there may be third variables that are driving the link between interactions with adult children with problems and cortisol (e.g., transmission of problems from parent to adult child, which are both linked to altered cortisol rhythms).
There were also limitations in the measurement of problems. We were not able to assess the specific types of problems adult children experienced, the timing, or the severity of the problems. Thus, there is some possibility of overlap across problem types (e.g., alcohol problem and physical/emotional problem), some problems may be current whereas others may have been resolved, and some problems may be severe whereas others are less troubling. Future research should consider these more nuanced issues with regard to adult child problems. We also only considered the parent’s reports of whether the adult child had problems. In future work, researchers should examine both the adult child’s reports of whether they have problems as well as offspring’s cortisol levels. For example, it would be interesting to explore whether adult children find these interactions as stressful as do parents.
We also did not consider how parents cope with the interactions experienced with their adult children who suffer problems. It is most likely that the negative effects adult child problems may be attenuated by some forms of coping or exacerbated by others. We also were not able to examine whether variations in daily cortisol may account for variations in parents’ overall health and well-being. Once we have additional waves of data we can explore these types of mediation models. Future work should consider other aspects of daily interactions that explain the same day effects of physical-emotional problems and the next day effects of lifestyle-behavioral problems such as variations in parental caregiving and support exchange (Gilligan et al., 2015).
Our measurement of cortisol has limitations due to its intra-individual variability and the fact that we relied on self-reported collection time which could be inaccurate. However, previous research using this method along with electronic time recording has found that participants accurately report time (Almeida et al., 2002). Furthermore, future work is needed to explore the multiple additional pathways by which adult children’s problems “get under parent’s skin.” For example, adult children with problems most likely affect parent’s immune system and cardiovascular system in addition to the HPA axis.
Overall, this study shows that while parents may be just as likely to experience positive interactions with adult children who suffer problems compared to their adult children without problems, parents experience more negative interactions with these children and those interactions are associated with the biological stress response. Interacting with children who have lifestyle-behavioral problems appears to have more delayed effects on the physiological stress response whereas interactions with children who suffer from physical-emotional problems are associated with more anticipatory and same day cortisol. We hope that this study inspires even more detailed research on the effects of adult children’s problems on parental daily well-being and stress to understand how children affect parents into old age.
Highlights.
We conducted a daily diary study in which middle aged respondents reported their daily social interactions with their adult children and provided saliva which was assayed for cortisol.
We examined whether daily social interactions (negative and positive) with children who suffer problems (e.g., health problems, trouble with the law, financial trouble) were associated with parents’ diurnal cortisol rhythms.
Parents have more negative interactions with children who suffer problems but no fewer positive interactions with those children.
Negative interactions were associated with cortisol but differentially for interactions with children who suffer health vs. lifestyle problems (e.g. trouble with the law).
Interactions with children who suffer lifestyle problems appear to have more lingering effects on parents’ cortisol responses.
Acknowledgments
This study was supported by grants from the National Institute on Aging (NIA), R01AG027769, Family Exchanges Study II, Psychology of Intergenerational Transfers (Karen L. Fingerman, Principal investigator). The MacArthur Network on an Aging Society (John W. Rowe, Network director) provided funds. This research also was supported by grant, 5 R24 HD042849 awarded to the Population Research Center (PRC) at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Role of the Funding Source
The data collection for this study was supported by Grant R01AG027769 from the National Institute on Aging, the Family Exchanges Study II and the Psychology of Intergenerational Transfers (Karen L. Fingerman, Principal Investigator). The MacArthur Network on an Aging Society (John W. Rowe, Network Director) also provided funds.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
The contributors for this project include the coauthors Kyungmin Kimb, Steven H. Zaritc, Karen Fingermanb, and Timothy Lovingb
Conflict of Interest
The authors have no conflict of interest.
References
- Adam EK, Doane LD, Zinbarg RE, Mineka S, Craske MG, Griffith JW. Prospective prediction of major depressive disorder from cortisol awakening responses in adolescence. Psychoneuroendocrino. 2010;35:921–931. doi: 10.1016/j.psyneuen.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience-cortisol associations in a population-based sample of older adults. P. Natl. Acad. Sci. USA. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM. Resilience and vulnerability to daily stressors assessed via diary methods. Curr. Dir. .Psychol. Sci. 2005;14:64–68. [Google Scholar]
- Almeida DM, Wethington E, Kessler RC. The daily inventory of stressful events an interview-based approach for measuring daily stressors. Assessment. 2002;9:41–55. doi: 10.1177/1073191102091006. [DOI] [PubMed] [Google Scholar]
- Barker ET, Greenberg JS, Seltzer MM, Almeida DM. Daily stress and cortisol patterns in parents of adult children with a serious mental illness. Health Psychol. 2012;31:130. doi: 10.1037/a0025325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bella G, Garcia M, Spadari-Bratfisch R. Salivary cortisol, stress, and health in primary caregivers (mothers) of children with cerebral palsy. Psychoneuroendocrino. 2011;36:834–842. doi: 10.1016/j.psyneuen.2010.11.005. [DOI] [PubMed] [Google Scholar]
- Birditt KS, Cichy KE, Almeida D. Age differences in exposure and reactivity to interpersonal tensions among black and white individuals across adulthood. Race and social problems. 2011;3:225–239. doi: 10.1007/s12552-011-9058-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, Fingerman KL, Zarit SH. Adult children’s problems and successes: Implications for intergenerational ambivalence. J. of Gerontol. B-Psychol. 2010;65:145–153. doi: 10.1093/geronb/gbp125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, Fingerman KL. Parent/child and intergenerational relationships across adulthood. Family theories: A content-based approach. 2012:71–86. [Google Scholar]
- Charles ST, Piazza JR, Mogle JA, Urban EJ, Sliwinski MJ, Almeida DM. Age Differences in Emotional Well-Being Vary by Temporal Recall. J. of Gerontol. B-Psychol. 2015 doi: 10.1093/geronb/gbv011. gbv011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress: The International Journal on the Biology of Stress. 2004;7:29–37. doi: 10.1080/10253890410001667205. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol. Med. 1983;13:595–605. [PubMed] [Google Scholar]
- Edwards S, Clow A, Evans P, Hucklebridge F. Exploration of the awakening cortisol response in relation to diurnal cortisol secretory activity. Life Sci. 2001;68:2093–2103. doi: 10.1016/s0024-3205(01)00996-1. [DOI] [PubMed] [Google Scholar]
- Fingerman KL, Kim K, Zarit SH, Birditt KS. The ties that bind: Middle-aged parents’ daily experiences with grown children. J. Marriage Fam. doi: 10.1111/jomf.12273. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman KL, Cheng Y-P, Birditt K, Zarit S. Only as happy as the least happy child: Multiple grown children’s problems and successes and middle-aged parents’ well-being. J. of Gerontol. B-Psychol. 2012;67:184–193. doi: 10.1093/geronb/gbr086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman KL, Kim K, Tennant PS, Birditt KS, Zarit SH. Intergenerational Support in a Daily Context. Gerontologist:gnv035. 2015 doi: 10.1093/geront/gnv035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Karlamangla AS, Almeida DM, Seeman TE. Social strain and cortisol regulation in midlife in the US. Soc. Sci. Med. 2012;74:607–615. doi: 10.1016/j.socscimed.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): facts and future directions. Int. J. Psychophysiol. 2009;72:67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Gilligan M, Suitor JJ, Rurka M, Con G, Pillemer K. Adult Children’s Serious Health Conditions and the Flow of Support Between the Generations. Gerontologist:gnv075. 2015 doi: 10.1093/geront/gnv075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA, Marks NF. Linked Lives: Adult children’s problems and their parents’ psychological and relational well-being. J. Marriage Fam. 2006;68:442–454. doi: 10.1111/j.1741-3737.2006.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagestad GO, Uhlenberg P. Social structures: Demographic changes and the well-being of older persons. New York: Springer Publishing Co; 2007. The impact of demographic changes on relations between age groups and generations: A comparative perspective; pp. 239–261. [Google Scholar]
- Hansen ÅM, Thomsen JF, Kaergaard A, Kolstad HA, Kaerlev L, Mors O, Rugulies R, Bonde JP, Andersen JH, Mikkelsen S. Salivary cortisol and sleep problems among civil servants. Psychoneuroendocrino. 2012;37:1086–1095. doi: 10.1016/j.psyneuen.2011.12.005. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Waltham, MA: Brandeis University; 1997. [Google Scholar]
- Marin TJ, Martin TM, Blackwell E, Stetler C, Miller GE. Differentiating the impact of episodic and chronic stressors on hypothalamic-pituitary-adrenocortical axis regulation in young women. Health Psychol. 2007;26:447. doi: 10.1037/0278-6133.26.4.447. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol. Bull. 2007;133:25. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Pillemer K, Suitor JJ. “ Will I Ever Escape My Child’s Problems?” Effects of Adult Children’s Problems on Elderly Parents. J. Marriage Fam. 1991:585–594. [Google Scholar]
- Pillemer K, Suitor JJ. Explaining mothers’ ambivalence toward their adult children. J. Marriage Fam. 2002;64:602–613. [Google Scholar]
- Pillemer K, Suitor JJ, Mock SE, Sabir M, Pardo TB, Sechrist J. Capturing the Complexity of Intergenerational Relations: Exploring Ambivalence within Later-Life Families. J. Soc. Issues. 2007;63:775–791. [Google Scholar]
- Reis H. Why researchers should think “real-world”: A conceptual rationale. Handbook of research methods for studying daily life. 2012:3–21. [Google Scholar]
- Rohleder N, Beulen SE, Chen E, Wolf JM, Kirschbaum C. Stress on the dance floor: the cortisol stress response to social-evaluative threat in competitive ballroom dancers. Pers. Soc. Psychol. B. 2007;33:69–84. doi: 10.1177/0146167206293986. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions 1. Endocr. Rev. 2000;21:55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Schmidt-Reinwald A, Pruessner J, Hellhammer D, Federenko I, Rohleder N, Schürmeyer T, Kirschbaum C. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999;64:1653–1660. doi: 10.1016/s0024-3205(99)00103-4. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Almeida DM, Greenberg JS, Savla J, Stawski RS, Hong J, Taylor JL. Psychosocial and biological markers of daily lives of midlife parents of children with disabilities. J. Health Soc. Behav. 2009;50:1. doi: 10.1177/002214650905000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer MM, Floyd F, Song J, Greenberg J, Hong J. Midlife and aging parents of adults with intellectual and developmental disabilities: impacts of lifelong parenting. Ajidd-Am J. Intellect. 2011;116:479–499. doi: 10.1352/1944-7558-116.6.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer MM, Greenberg JS, Hong J, Smith LE, Almeida DM, Coe C, Stawski RS. Maternal cortisol levels and behavior problems in adolescents and adults with ASD. J. Autism Dev. Disord. 2010;40:457–469. doi: 10.1007/s10803-009-0887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selye H. The stress concept and some of its implications. Human stress and cognition: An information processing approach. 1979:11–32. [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Linzer M, Verloin deGruy F, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. Jama. 1994;272:1749–1756. [PubMed] [Google Scholar]
- Stawski RS, Cichy KE, Piazza JR, Almeida DM. Associations among daily stressors and salivary cortisol: Findings from the National Study of Daily Experiences. Psychoneuroendocrino. 2013;38:2654–2665. doi: 10.1016/j.psyneuen.2013.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Kunz-Ebrecht S, Owen N, Feldman PJ, Willemsen G, Kirschbaum C, Marmot M. Socioeconomic status and stress-related biological responses over the working day. Psychosom. Med. 2003;65:461–470. doi: 10.1097/01.psy.0000035717.78650.a1. [DOI] [PubMed] [Google Scholar]
- Suitor JJ, Pillemer K. Did mom really love you best? Developmental histories, status transitions, and parental favoritism in later life families. Motiv. Emotion. 2000;24:105–120. [Google Scholar]
- Suitor JJ, Pillemer K, Sechrist J. Within-family differences in mothers’ support to adult children. J. of Gerontol. B-Psychol. 2006;61:S10–S17. doi: 10.1093/geronb/61.1.s10. [DOI] [PubMed] [Google Scholar]
- Thomas DL, Diener E. Memory accuracy in the recall of emotions. J. Pers. Soc. Psychol. 1990;59:291. [Google Scholar]
- Umberson D, Pudrovska T, Reczek C. Parenthood, childlessness, and well-being: A life course perspective. J. Marriage Fam. 2010;72:612–629. doi: 10.1111/j.1741-3737.2010.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]