The coronary heart disease (CHD) epidemic peaked in the 1960s. Since that time age-adjusted mortality declined steadily in the United States and many other industrialized countries1. Hospitalization for CHD also fell, particularly in the past two decades with CHD severity decreasing as NSTEMIs increased, indicating milder forms of CHD1. Finally, lifestyle factors and associated risk factors improved such as smoking, hypertension and cholesterol1. These changes and the trends over time lead naturally to the question of causality. Are changes in lifestyles, risk factors, or acute and chronic clinical care playing roles in this evolving picture and how does each influence the desired outcomes? In this issue of Circulation, the paper by Mannsverk and colleagues2 in Norway provides insights into the evolving cardiovascular disease epidemic.
The underlying causes of the CHD epidemic are well studied3. Following the World War II, there were major changes in the health habits. Returning war veterans kept their smoking habit and women soon followed. A diet high in fats became prevalent. Physical activity declined as labor saving devices entered work places and automobiles became the dominant form of transportation. The resulting peak in CHD in the mid 60s is now well recognized.
More serious research into the causes of the decline began in the 1970s, highlighted at the NIH conference in 1979 which “discovered” the declining mortality from CHD4. At that conference, numerous explanations from cardiopulmonary resuscitation to Medicare were advanced but few data were available to understand the observations. In subsequent years, a debate ensued with some favoring primary prevention due to changes in lifestyle and risk factor reduction. Others cited secondary prevention with associated acute and chronic medical care. Most agree that many factors played some role in the decline but dispute their relative contributions5. The relative contributions are more than an intellectual exercise as different prevention and treatment approaches have implications for resources and health policy. The debate also affects the so-called ‘epidemiologic transition’ or the anticipated rise of chronic diseases, particularly CHD, in developing countries6.
One reason for the challenges in understanding trends is the lack of comprehensive high-quality data. Population data before 1970 is extremely limited and of poor quality. Even mortality can be a challenge because both the fact of death and the cause of death are frequently misclassified7. Hospitalized morbidity rates are similarly weak depending on discharge diagnoses from administrative data. These are influenced by evolving diagnostic fashion, new technology and reimbursement8. Outpatient clinic morbidity is even more variable and difficult to gather. Some suggest that “big data” from administrative data sets will answer these questions but these data are subject to misclassification and bias. Finally, limited data are available on risk factor patterns and trends. The National Health and Nutrition Examination Survey (NHANES), initiated in the 1960s, uses a national sampling strategy \but the numbers in subgroups are small and the methods changed overtime9.
Nonetheless, there have been numerous attempts to understand the magnitude, causes and relative impact of primary prevention, acute care and secondary prevention on CHD5. Cohort studies such as Framingham are used to describe the impact of risk factor change on outcomes10. Others have evaluated outcomes utilizing clinical trials or epidemiology data to estimate the magnitude of effect of various changes5. More complex models such as IMPACT utilize modeling techniques to include these many factors11,12. This results in proportions attributable to primary prevention or clinical care. The proportion varies by country with the Scandinavian countries finding public health approaches a dominant factor. Others have found proportions closer to half allocated to each in both US and Western European studies13. All suffer from limits of data on the population under study. They also lack information on incidence or first event most likely to be affected by primary prevention and other risk factors such as stress or socioeconomic status. Finally, few have recognized the central role of out-of-hospital sudden death accounting for more than half of all CHD mortality. Sudden death frequently observed in individuals who have no prior history of CHD13.
The article by Mannsverk and colleagues addresses many of the weaknesses in previous studies. Direct population data are collected over 15 years on all of the relevant perimeters needed to make estimates of contributions to the decline. Particularly critical is the availability of incidence data and sudden death data at the population level.
Norway is recognized for the high standards of living and quality of life according to studies by the United Nations14. With universal healthcare and high technology medicine widely available it provides information relevant to similar settings. This study is able to link hospital, clinic, death records with population surveillance as all citizens having a single identification number. The data are collected with standard methods and quality control. The city of Tromsø is relatively compact and isolated with little out migration. Using the three population surveys (1994–95, 2001–02, 2007–08) risk factors were measured in subjects 25 years and older, a total of 29,582 healthy men and women. Follow-up to 2010 resulted in 375,064 person years of experience. These large numbers produce stable estimates of variables.
The Tromsø study finds that age and sex adjusted incidence of total coronary disease decreased by 3% annually over the 15 years of follow-up. The decrease was found primarily in reductions in out-of-hospital sudden death and hospitalized STEMI. Reductions in serum cholesterol accounted for approximately one-third of the event decline but decreases in smoking, blood pressure, heart rate and increased physical activity all contributed. Interestingly, rises in body mass index and diabetes mellitus were associated with modest increases in disease outcomes. Overall, risk factors accounted for 66% of the decline in incidence. These data contain important lessons.
United States (US) has similarities and differences from Norway. The Norwegians have the ability to collect comprehensive data at all levels in a population. Universal health care allows the Norwegians to make policy decisions regarding the emphasis and allocation of resources. The United States has a similar high technology environment. However, health disparities in CHD incidence and outcomes adds to the US burden1. The focus of Scandinavia public health approaches is best exemplified in Finland. The Finns were recognized in the 1950s to have among the highest CHD rates in the world. This was associated with elevated levels of risk factors3. A focused public health program resulted in dramatic deductions in cardiovascular risk factors and a parallel decline in CHD morbidity and mortality15,16.
But there are also major changes in the United States. As shown in Figure 1, CHD mortality has been falling steadily since 1979 and before. These changes average a 3% per year decline in the age-adjusted data. The result of this observation is that expected lifespan of American citizens is, on average, rising. A second observation in Figure 1 is found in the bars representing absolute deaths. These were flat for many years as cardiovascular diseases were pushed to growing older populations. However, in the last decade, the absolute number of deaths have also been falling approximately 3% per year. As found in Norway, this suggests that incidence and sudden death are declining in the United States. One might speculate as to the reasons for these declines and there are many postulated contenders. But in the U.S. there are few data to answer the question. Information from the Centers for Disease Control and Prevention (CDC) in their NHANES surveys are not of adequate size to address trends. And these data are not linked to morbidity information from clinic visits and hospitalizations. This renders the analyses ecologic where subjects cannot be connected to individual health characteristics and disease outcomes.
Figure 1.
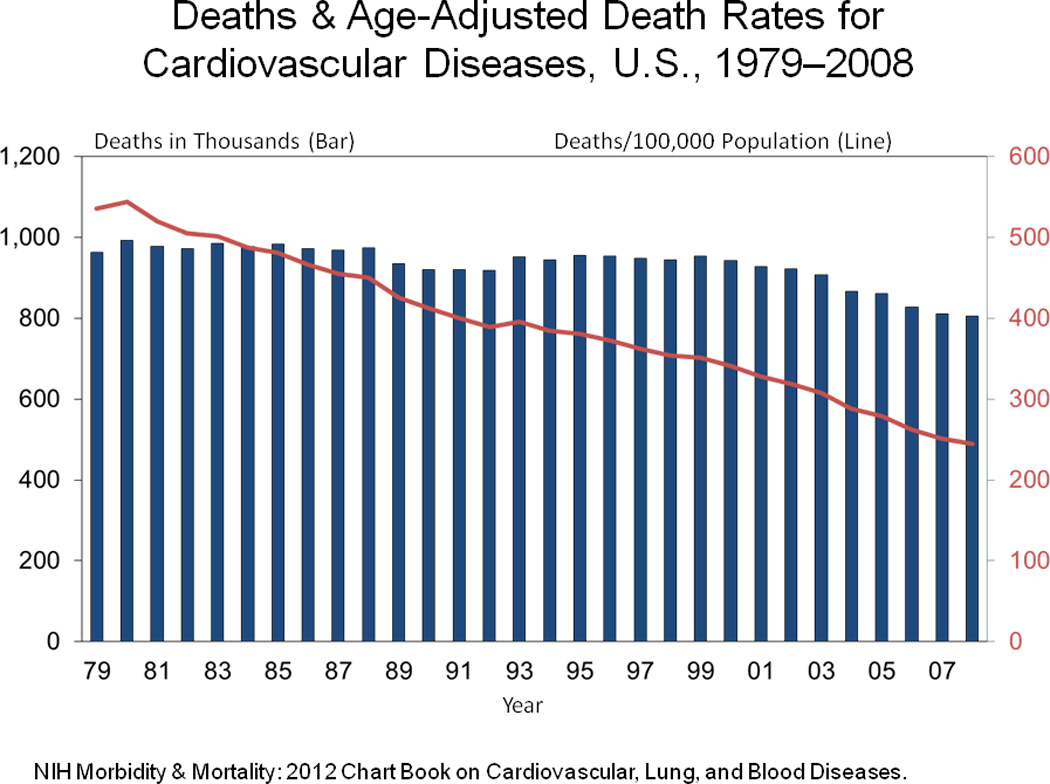
Deaths & Age-Adjusted Death Rates for Cardiovascular Diseases, U.S., 1979–2008.
There are suggestions that “big data” can solve this problem. Enormous amounts of patient data contained in private insurance, Medicare and other registers are cited as unique opportunity to gather low cost information. However, these data are collected for billing and other administrative purposes and frequently lack the quality to draw scientific inferences. There is also the continuing problem of linking of different data sets with individuals, their care and outcomes in a multisource healthcare system.
The direction of US trends is also evident in Figure 2. This figure depicts trends in CHD hospitalizations in the state of Minnesota. Hospitalizations with CHD discharge codes have steadily fallen about 3% per year in the past decade. This figure contains incidence (new cases) admissions, recurrent (same patient/same year) and the admissions among those who are previously diagnosed. Further analyses of these data find falling of STEMI with a more modest falling trend in NSTEMI.
Figure 2.
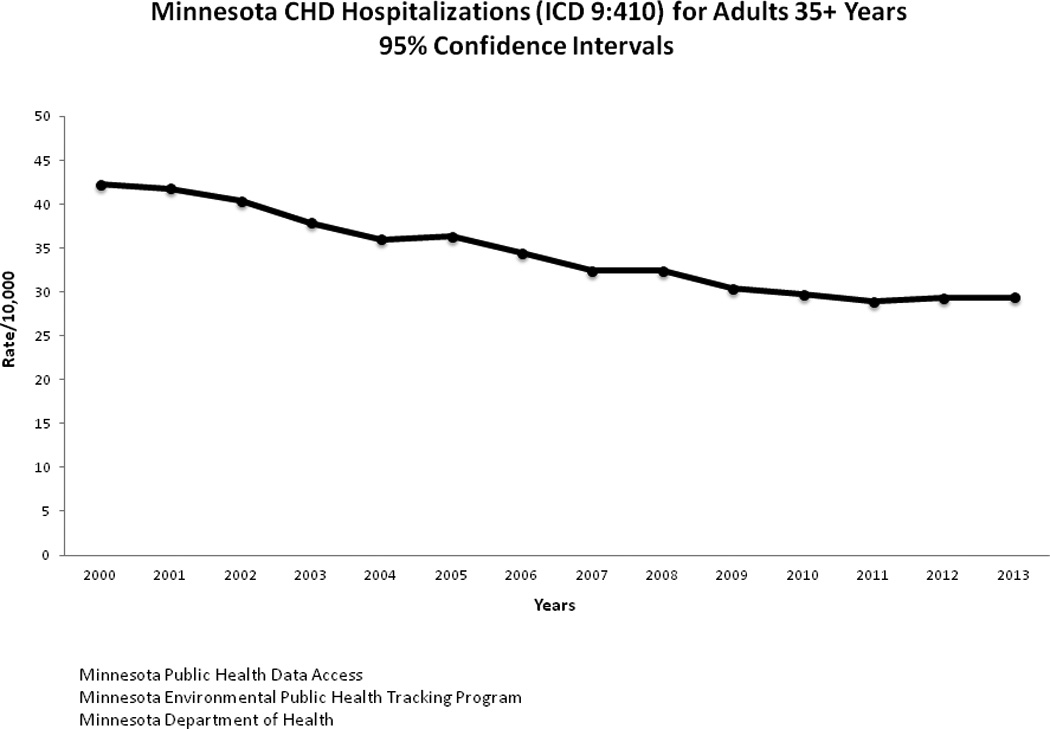
Minnesota CHD Hospitalizations (ICD 9:410) for Adults 35+ Years. 95% Confidence Intervals.
The American Heart Association’s Annual Heart Disease and Stroke Statistics Update is the most comprehensive source of annual estimates of incidence, prevalence and risk factor distribution of the country17. It is a carefully collated report from many federal and private sources of varying designs, populations and sample sizes. It is the best data that we have. However, it is neither nationally representative nor able to provide incidence data on CHD. As it stands, it is only an estimate of important trends. Public health goals targeting improve CHD outcomes include the Millions Heart Initiative, AHA 2020 goals and the Healthy People 2020 goals. With the current systems, it will not be possible to rigorously evaluate the outcomes of these recommendations18.
In 2011, The Institute of Medicine reports recommended a national surveillance program be put in place funded by the Affordable Care Act. As yet, there is not a national surveillance effort to understand the origin of trends occurring in the US18,19.
The Norwegian experience demonstrates that high quality data can be collected in a population and inferences made regarding the roles of public health and medical interventions on population disease outcomes. The need to plan policy and allocate resources, always present, is more imperative as rising costs for care of the chronically ill are becoming unsustainable and much of the potential for prevention is, as yet, unrealized.
Footnotes
Disclosures: None.
References
- 1.National Institutes of Health. National Heart, Lung, and Blood Institute. [Accessed November 3, 2015];Morbidity & Mortality: 2012 Chart Book on Cardiovascular, Lung, and Blood Diseases. www.nhlbi.nih.gov/files/docs/research/2012_ChartBook.pdf.
- 2.Mannsverk J, Wilsgaard T, Mathiesen E, Løchen ML, Rasmussen K, Thelle D, Njølstad I, Hopstock L, Bønaa K. Trends in modifiable risk factors are associated with declining incidence of hospitalized and non-hospitalized acute coronary heart disease in a population. Circulation. 2016;133 doi: 10.1161/CIRCULATIONAHA.115.016960. XX-XX. [DOI] [PubMed] [Google Scholar]
- 3.Keys A. A Multivariate Analysis of Death and Coronary Heart Disease. Cambridge, Massachusetts: Harvard University Press; 1980. Seven Countries. [Google Scholar]
- 4.Havlik RJ, Feinleib M. Proceedings of the Conference on the Decline in Coronary Heart Disease Mortality. National Heart, Lung and Blood Institute Public Health Service, National Institutes of Health, Publication No. 79-1610. 1979 [Google Scholar]
- 5.Jones DS, Greene JA. The contributions of prevention and treatment to the decline in cardiovascular mortality: Lessons from a forty-year debate. Health Affairs. 2012;31:2250–2258. doi: 10.1377/hlthaff.2011.0639. [DOI] [PubMed] [Google Scholar]
- 6.Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases. Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 7.Mikkelsen L, Phillips DE, AbouZahr C, Setel PW, de Savigny D, Lozano R, Lopez AD. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet. 2015;386:1395–1406. doi: 10.1016/S0140-6736(15)60171-4. [DOI] [PubMed] [Google Scholar]
- 8.Assaf AR, Lapane KL, McKenney JL, Carleton RA. Possible influence of the prospective payment system on the assignment of discharge diagnoses for coronary heart disease. N Engl J Med. 1993;329:931–935. doi: 10.1056/NEJM199309233291307. [DOI] [PubMed] [Google Scholar]
- 9.National Health and Nutrition Examination Survey - Official Site. [Accessed November 5, 2015]; www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 10.Beaglehole R, Larosa JC, Heiss G, Davis CE, Williams OD, Tyroler HA, Rifkind BM. Serum-cholesterol, diet and the decline in coronary heart disease mortality. Prev Med. 1979;8:538–547. doi: 10.1016/0091-7435(79)90329-3. [DOI] [PubMed] [Google Scholar]
- 11.Capewell S, Morrison CE, McMurray JJ. Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart. 1999;81:380–386. doi: 10.1136/hrt.81.4.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 13.Adabag AS, Peterson G, Apple FS, Titus J, King R, Luepker RV. Etiology of sudden death in the community: results of anatomical, metabolic and genetic evaluation. Am Heart J. 2010;159:33–39. doi: 10.1016/j.ahj.2009.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The World Post. A Partnership of the Huffington Post and Berggruen Institute. [Accessed November 2, 2015];Norway Best Place to Live: UN Report. http://www.Huffingtonpost.com/2009/10/05norway-best-place-live_n_309698.html.
- 15.Borodulin K, Vartiainen E, Peltonin M, Jousilahti P, Joulevi A, Laatikainen T, Männistö S, Salomaa V, Sundvall J, Puska P. Forty-year trends in cardiovascular risk factors in Finland. Eur J Public Health. 2015;25:539–546. doi: 10.1093/eurpub/cku174. [DOI] [PubMed] [Google Scholar]
- 16.Degano IR, Salomaa V, Veronesi G, Ferriéres J, Kirchberger I, Laks T, Havulinna AS, Ruidavets JB, Ferrario MM, Meisinger C, Elosua R, Marrugat J Acute Mycardial Infarction Trends in Europe (AMITIE) Study Investigators. Twenty-five-year trends in myocardial infarction attack and mortality rates, and case-fatality, in six European populations. Heart. 2015;101:1413–1421. doi: 10.1136/heartjnl-2014-307310. [DOI] [PubMed] [Google Scholar]
- 17.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart Disease and Stroke Statistics—2015 Update: A Report From the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 18.A Nationwide Framework for Surveillance of Cardiovascular and Lung Diseases. Washington, DC: The National Academics Press; 2011. Committee on a National Surveillance System for Cardiovascular and Select Chronic Diseases; Institute of Medicine of the National Academies. [Google Scholar]
- 19.Sidney S, Rosamund WD, Howard VJ, Luepker RV. The “heart disease and stroke statistics - 2013 update” and the need for a national cardiovascular disease surveillance system. Circulation. 2013;127:21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]


