Abstract
Gain of function (GOF) mutation in the p110δ catalytic subunit of the phosphatidylinositol-3-OH kinase (PIK3CD) is the cause of a primary immunodeficiency (PID) characterized by recurrent sinopulmonary infections and lymphoproliferation. We describe a family of two adults and three children with GOF mutation in PIK3CD, all with recurrent sinopulmonary infections and varied infectious and non-infectious complications. The two adults have primary sclerosing cholangitis (PSC) without evidence of Cryptosporidium parvum infection and have required liver transplantation. PSC is a novel phenotype of GOF mutation in PI3CKD.
Keywords: PIK3CD, Immunodeficiency, Primary Sclerosing Cholangitis, Recurrent Infections
Introduction
Gain of Function (GOF) mutation in the p110δ catalytic subunit of the phosphatidylinositol-3-OH (PIK3CD) is the cause of a primary immunodeficiency (PID) characterized by recurrent sinopulmonary infections, lymphoproliferation, EBV and CMV viremia as well as EBV and non-EBV driven malignancies (1–3). We describe five family members with GOF PIK3CD characterized by recurrent sinopulmonary infections and Primary Sclerosing Cholangitis (PSC) not associated with Cryptosporidium parvum infection in the adults.
CASE REPORTS
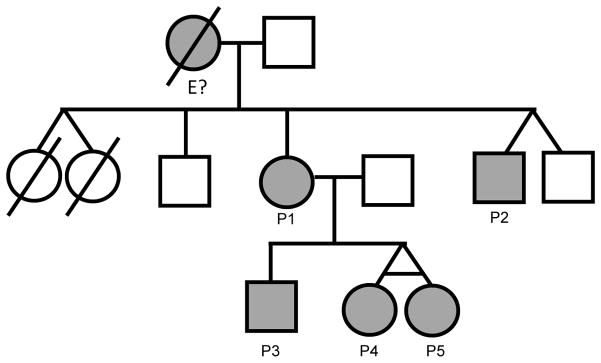
The family is composed of two affected siblings (P1 and P2) and one of the sibling’s three children (P3–5). All affected family members have recurrent sinopulmonary infections and various shared and unique clinical features as outlined in Figure 1. There is no history or evidence of chronic viral replication in the affected family members and at this time no evidence of lymphoproliferation.
Figure 1.
Family pedigree and immune function testing for all affected family members prior to immune replacement. Quantitative Immunoglobulin levels are given with the given lab’s normal values for age at time of evaluation, P1(31yo), P2 (13yo), P3 (5yo), P4 (3yo) P5 (3yo). P1’s flow cytometry, obtained at age 34, is shown post transplantation as she was evaluated post liver transplantation; P2 however was evaluated with flow cytometry pre liver transplant and at age 27. Lymphocyte enumeration of the children was obtained at 10 years of age for P3 and 8 years for P4 and P5. A summary of all infections and systemic symptoms for each of the family members is also provided. Culture positive results for sinopulmonary infections (S. aureus, S. pneumonia, and H. influenzae) were documented for P3, P4 and P5 on different occasions, diagnosis based on clinical symptoms documented for P1 and P2. * indicates data not available. Father of P1 and P2 as well as the 2 unaffected siblings are mutation negative; mother of P1 and P2 was not tested as she is deceased and there is no genetic tissue available for evaluation, as indicated by “E?” in the pedigree. Abbreviations: Varicella zoster virus (VZV), Herpes Simplex virus (HSV). Primary Sclerosing Cholangitis (PSC), Gastroesophageal Reflux (GERD), Ulcerative Colitis (UC)
Patient 1 is a 34 yo Caucasian female with a history of non-infectious diarrhea as a child and recurrent infections. At age 16 she was evaluated with colonoscopy and biopsy, which led to a diagnosis of Ulcerative Colitis (UC) and PSC. Her liver biopsy is seen in Figure 2 showing liver cirrhosis, periductal fibrosis, and ductopenia with neocholangiogensis consistent with PSC. There was no evidence of Cryptosporidium parvum infection of the bile ducts on biopsy or culture. She underwent liver transplantation at age 18 and has had a stable post-transplant course with no recurrence of PSC and resolution of her UC. After liver transplantation she was started on Immunoglobulin (IG) replacement for recurrent sinopulmonary infections. Her respiratory tract infections have improved but she has had dental abscesses and facial cellulitis.
Figure 2.
a) 2X, b) 10X. Liver biopsy of P1 at time of PSC diagnosis showing liver cirrhosis, periductal fibrosis, ductopenia with neocholangiogensis consistent with PSC. Images show obliterated bile duct with inflammation at the hilum of the liver. The only residual epithelium is from peribiliary glands. There was no evidence of cryptosporidium infection on biopsy and multiple stool tests. Abbreviations: Primary Sclerosing Cholangitis (PSC)
Patient 2 is a 27 yo Caucasian male who was hospitalized at age 2 for varicella with superficial skin infection requiring IV antibiotics. At age 6 he developed pancytopenia, lymphadenopathy and hepatosplenomegaly. His bone marrow biopsy was hypercellular, and a lymph node biopsy showed follicles with limited germinal centers. He was started on IG replacement in his teenage years for recurrent sinopulmonary infections with improvement, but discontinued therapy due to insurance reasons. While off IG replacement he was hospitalized at age 23 for varicella pneumonia. One year later he was diagnosed with PSC with no evidence of Inflammatory Bowel Disease (IBD) or Cryptosporidium parvum infection and underwent liver transplantation. Three years after the original transplant, he has had a recurrence of PSC and is awaiting re-transplantation.
Patient 3 is a 10 yo Caucasian male with onset of serious respiratory tract infections at 6 months of age with severe RSV bronchiolitis and recurrent otitis media. At age 6 he was started on IG replacement for recurrent sinopulmonary infections but continued to have sinopulmonary infections despite IG therapy. He has gastroesophageal reflux and vomiting but no evidence of IBD on colonoscopy. He has had cellulitis, impetigo and multiple tooth abscesses as well as dental caries despite good dental hygiene and regular dental care. His skin testing, unlike his siblings, demonstrates specific IgE production to ragweed.
Patients 4 & 5 are identical 8 yo twin Caucasian females. They have recurrent infections with sinusitis and otitis, but without pneumonia. Patient 4 has had eczema with superinfection, cellulitis, plantar warts and cervical lymphadenitis. In addition she has had dental abscesses without dental caries despite excellent dental hygiene. Her twin, Patient 5, has a history of eczema herpeticum at age 1 treated with outpatient acyclovir and was admitted for IV antibiotics for cervical lymphadenitis at the age of 2. She has no history of dental abscesses in contrast to her siblings and mother.
All family members had slightly low to normal IgG, normal IgA with normal to elevated IgM with the exception of patient 3 who had low IgG prior to initiation of immunoglobulin. With the exception of Patient 1, lymphocyte enumeration studies showed mild T and B cell lymphopenia with low total and switched memory B cells and CD4 skewing to memory phenotype when adjusted for age. Results of flow cytometry for Patient 1 were obtained post liver transplantation, which may explain the increased percentage of activated, DR+ T cells (Table 1). Based on their clinical phenotype and initial immune evaluation, the family underwent testing for known causes of Hyper IgM Syndrome (HIGM), which was negative. Whole exome sequencing did not reveal the genetic cause of the immunodeficiency. However, after publication of PIK3CD mutations and clinical similarity to this disorder, the exome data was reanalyzed and the PI3KCD gene was found to exhibit poor coverage. Sanger sequencing of PIK3CD confirmed a known GOF heterozygous mutation c3061G>A, p.E1021K in all affected family members (1, 4).
Table 1.
| P1 | P2 | P3 | P4 | P5 | |
|---|---|---|---|---|---|
| Immunoglobulins (mg/dL) | |||||
| IgG | 1550 (642–1730) | 1220 (700–1500) | 483 (608–1229) | 610 (600–1400) | 564 (423–1090) |
| IgA | 389 (91–499) | 160 (60–350) | 147 (40–200) | 66 (24–121) | 86 (27–195) |
| IgM | 330 (34–342) | 304 (50–300) | 596 (40–250) | 231 (45–190) | 301 (45–190) |
| Vaccination Titers | |||||
| Diphtheria | Non Protective | Protective | Non Protective | Protective | Protective |
| Tetanus | Non Protective | Protective | Non Protective | Protective | Protective |
| Pneumococcus | 0/23 Serotypes | 3/23 Serotypes | 0/23 Serotypes | 3/23 Serotypes | 3/23 Serotypes |
| Lymphocyte Enumeration | |||||
| %CD3+ (mm3) | 84% (1149) | 85 (385) | 85% (1333) | 80% (1178) | 78% (1184) |
| %CD3+ CD4+ (mm3) | 30% (410) | 57.2% (257) | 32% (502) | 47% (692) | 38% (577) |
| %DR+CD4+ | 8% | * | 3% | 2% | 2% |
| %CD4+CD45RA+ | 5% | 4% | 27% | 45% | 40% |
| %CD4+CD45RO+ | 85% | 45% | 63% | 45% | 50% |
| %CD19+ (mm3) | 5% (68) | 11% (51) | 8% (125) | 14% (206) | 15% (228) |
| %CD27+ | 15% | 3.5% | 11% | 6% | 5% |
| %IgD-CD27+ | 7% | * | 2% | 1% | 1% |
|
| |||||
| Sinopulmonary Infections | Otitis Sinusitis Pneumonia |
Otitis Sinusitis Pneumonia |
Otitis Sinusitis Pneumonia |
Otitis Sinusitis |
Otitis Sinusitis |
|
|
|||||
| Viral Infections | VZV Pneumonia | Plantar Warts | Plantar Warts HSV1 |
||
|
|
|||||
| Other Infections | Dental Abscesses Cellulitis |
Dental Abscesses | Dental Abscesses Lymphadenitis |
Lymphadenitis | |
|
|
|||||
| Gastrointestinal Disease | PSC Liver Transplant UC |
PSC Liver Transplant Recurrent Disease |
Vomiting | GERD | Bloody Stools |
|
|
|||||
| Hematological | Thrombocytopenia Anemia |
Pancytopenia | |||
The Mother of P1 and P2 died from complications of dialysis-dependent IgA nephropathy at age 57. She reportedly has a history of recurrent otitis, sinusitis and pneumonia; cytopenias, including anemia and thrombocytopenia; as well as auto-immunity, ANA positive with vasculitis. In addition, she had hypergammaglobulinemia with elevated IgM (IgG 1961mg/dL, IgA 278 mg/dL, IgM 450 mg/dL). She had two infant female twins that died of unknown causes in infancy. Based on her past medical history, we hypothesize she harbored the founder mutation; however there was no genetic material for evaluation.
Discussion
GOF mutation in the p110δ subunit of PIK3CD is an immunodeficiency characterized by recurrent sinopulmonary infections leading to structural lung abnormalities including bronchiectasis, lymphoproliferation, and EBV and CMV viremia (1). Typical laboratory abnormalities include a low to normal IgG, normal to elevated IgM, decreased specific antibody production, decreased total memory and switched memory B cells, and T cell lymphopenia with skewing to a memory phenotype.
The affected family members in our cohort shared many of these clinical and laboratory features. Importantly, both adult affected family members developed PSC. PSC is a known complication in 6–11% of patients with X-linked Hyper IgM Syndromes (HIGM), which is thought to be due to infection with Cryptosporidium parvum (5, 6). Cryptosporidium infections in patients with MHC class II deficiency, as well as IL-21R deficiency, can also lead to development of PSC(7, 8). Neither of our patients with PSC had evidence of Cryptosporidium parvum infection. P1 carried the diagnosis of UC prior to liver transplant which is associated with PSC (9). Post liver transplant and on cyclosporine immunosupression her UC went into remission, which was sustained for over 16 years. P2 had no history of IBD and had a recurrence of the PSC after the original liver transplant. Collectively, these observations suggest that GOF mutations in PI3KD are a cause of PCS.
Apart from PSC, another common phenotype of this family is the occurrence of recurrent dental abscesses. Three patients (P1, P3 and P4) had recurrent dental abscesses despite appropriate dental hygiene and regular professional dental care. Patients with PIK3CD can have autoimmune cytopenias, which could predispose them to the dental abscesses. However, in our cases there was no evidence of immune cytopenias (1). Therefore, the explanation if, or how, GOF PIK3CD predisposes to dental abscesses is unclear.
In summary, we report an association of GOF mutations in PIK3CD gene and the development of PSC in both adult patients with the PIK3CD mutation. Multiple genes, have been previously associated with PSC. Not surprisingly, key components of the adaptive and innate immunity are among those genes (e.g., IL2RA, IL21R, CD28 and MST1 among others)(10) and several of them converge at the PI3K/Akt signaling pathway (11). The observation that PSC developed in 2 adult patients with GOF mutations in PIK3CD gene raises difficult diagnostic decisions for the optimal treatment of the affected children. GOF mutations of PIK3CD lead to activation of the mTOR pathway, which can be inhibited by rapamycin, allowing for a currently available specific therapy. However the lung toxicity and cancer risk makes rapamycin not an optimal choice for lifelong therapy (1). Hematopoietic stem cell transplantation had been used in one patient successfully, however there is no long-term data at this time regarding its clinical efficacy. Additionally clinical trials are underway to study the effectiveness of new biological agents inhibiting the p110δ subunit for the treatment of chronic lymphocytic leukemia (4). The optimal treatment of these patients, whether that be conventional immunosuppressants, mTOR inhibition, p110 inhibition, or stem cell transplant, is unknown.
Acknowledgments
We thank the Medical College or Wisconsin Clinical & Translational Science Institute (CTSI) for their clinical research support, Dr. Henry Appelman at the University of Michigan Department of Pathology for obtaining images of P1’s initial biopsies and Audrey Harrington for editing the manuscript.
References
- 1.Lucas CL, Kuehn HS, Zhao F, Niemela JE, Deenick EK, Palendira U, et al. Dominant-activating germline mutations in the gene encoding the PI(3)K catalytic subunit p110delta result in T cell senescence and human immunodeficiency. Nature immunology. 2014;15(1):88–97. doi: 10.1038/ni.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crank MC, Grossman JK, Moir S, Pittaluga S, Buckner CM, Kardava L, et al. Mutations in PIK3CD can cause hyper IgM syndrome (HIGM) associated with increased cancer susceptibility. Journal of clinical immunology. 2014;34(3):272–6. doi: 10.1007/s10875-014-0012-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kracker S, Curtis J, Ibrahim MA, Sediva A, Salisbury J, Campr V, et al. Occurrence of B-cell lymphomas in patients with activated phosphoinositide 3-kinase delta syndrome. The Journal of allergy and clinical immunology. 2014;134(1):233–6. doi: 10.1016/j.jaci.2014.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Angulo I, Vadas O, Garcon F, Banham-Hall E, Plagnol V, Leahy TR, et al. Phosphoinositide 3-kinase delta gene mutation predisposes to respiratory infection and airway damage. Science. 2013;342(6160):866–71. doi: 10.1126/science.1243292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winkelstein JA, Marino MC, Ochs H, Fuleihan R, Scholl PR, Geha R, et al. The X-linked hyper-IgM syndrome: clinical and immunologic features of 79 patients. Medicine (Baltimore) 2003;82(6):373–84. doi: 10.1097/01.md.0000100046.06009.b0. [DOI] [PubMed] [Google Scholar]
- 6.Levy J, Espanol-Boren T, Thomas C, Fischer A, Tovo P, Bordigoni P, et al. Clinical spectrum of X-linked hyper-IgM syndrome. The Journal of pediatrics. 1997;131(1 Pt 1):47–54. doi: 10.1016/s0022-3476(97)70123-9. [DOI] [PubMed] [Google Scholar]
- 7.Hanna S, Etzioni A. MHC class I and II deficiencies. The Journal of allergy and clinical immunology. 2014;134(2):269–75. doi: 10.1016/j.jaci.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Kotlarz D, Zietara N, Uzel G, Weidemann T, Braun CJ, Diestelhorst J, et al. Loss-of-function mutations in the IL-21 receptor gene cause a primary immunodeficiency syndrome. The Journal of experimental medicine. 2013;210(3):433–43. doi: 10.1084/jem.20111229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsaitas C, Semertzidou A, Sinakos E. Update on inflammatory bowel disease in patients with primary sclerosing cholangitis. World journal of hepatology. 2014;6(4):178–87. doi: 10.4254/wjh.v6.i4.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henriksen EK, Melum E, Karlsen TH. Update on primary sclerosing cholangitis genetics. Current opinion in gastroenterology. 2014;30(3):310–9. doi: 10.1097/MOG.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 11.Yuan Z, Kim D, Shu S, Wu J, Guo J, Xiao L, et al. Phosphoinositide 3-kinase/Akt inhibits MST1-mediated pro-apoptotic signaling through phosphorylation of threonine 120. The Journal of biological chemistry. 2010;285(6):3815–24. doi: 10.1074/jbc.M109.059675. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]