Abstract
Emotion regulation has been implicated in the etiology of depression. A first step in adaptive emotion regulation involves emotional clarity, the ability to recognize and differentiate one’s emotional experience. As family members are critical in facilitating emotional understanding and communication, we examined the impact of family functioning on adolescent emotional clarity and depressive symptoms. We followed 364 adolescents (ages 12–17; 52.5% female; 51.4 % Caucasian, 48.6% African American) and their mothers over 2 years (3 time points) and assessed emotional clarity, depressive symptoms, and adolescent-reported and mother-reported family functioning. Emotional clarity mediated the relationship between adolescent-reported family functioning and depressive symptoms at all time points cross-sectionally, and according to mother-reported family functioning at Time 1 only. There was no evidence of longitudinal mediation for adolescent- or mother-reported family functioning. Thus, family functioning, emotional clarity, and depressive symptoms are strongly related constructs during various time points in adolescence, which has important implications for intervention, especially within the family unit.
Introduction
Much research has examined emotion regulation deficits in increasing vulnerability to depression (for reviews, see: Hofmann, Sawyer, Fang, & Asnaani, 2012; Kovacs, Joormann, & Gotlib, 2008). However, emotion regulation is a broad, multifaceted construct, thought to comprise multiple intrinsic and extrinsic processes (Gyurak, Gross, & Etkin, 2011), including emotional awareness and appraisal (Boden & Thompson, 2015; Stegge & Terwogt, 2007), arousal (Porges, Doussard-Roosevelt, & Maiti, 1994), and cognitive strategies (Aldao, Nolen-Hoeksema, & Schweizer, 2010). To better understand depression etiology and risk and to inform intervention, there is great utility in examining which components may be most relevant to vulnerability to depression, as well as factors that may give rise to such processes. Given that family members are critical in providing direct and indirect models of emotional understanding and communication (Zeman, Cassano, Perry-Parrish, & Stegall, 2006), the present study sought to examine the influence of family functioning on emotional clarity—one important component thought to underlie emotion regulation—and subsequent depressive symptoms in adolescents. Adolescence may be an important period in which to examine such associations given that adolescence is characterized by significant neurobiological change thought to be particularly relevant for some types of social-affective learning (Crone & Dahl, 2012), and a time when depression rates increase (Lewinsohn, Clarke, Seeley, & Rohde, 1994), particularly for girls (Hankin & Abramson, 2001).
Emotional Clarity
Emotional clarity, the ability to recognize, discriminate, and understand one’s own emotions (Gohm & Clore, 2000), is a component of two prominent multidimensional constructs that are related to depression: alexithymia (Sifneos, 1973) and emotion regulation (Thompson et al., 2009). Low emotional clarity is a central part of alexithymia, broadly defined as the inability to identify emotions in the self (Boden, Thompson, Dizén, Berenbaum, & Baker, 2013; Sifneos, 1973). Alexithymia is characterized by a variety of factors, including difficulties in the ability to describe and identify feelings, challenges in distinguishing between emotional vs. bodily arousal, lack of imagination, and externally-oriented thinking (Bankier, Aigner, & Bach, 2001). As alexithymia has been linked to negative outcomes, including poor executive functioning (Koven & Thomas, 2010) and depression (Honkalampi, Hintikka, Tanskanen, Lehtonen, & Viinamäki, 2000), it may be useful to study how, as a component of alexithymia, low emotional clarity also might be associated with deficits in functioning.
Additionally, emotional clarity is an important aspect of the emotion regulatory process; before engaging in any implicit or explicit methods of emotion modulation, one must be able to identify that he or she is experiencing a particular emotion (for reviews, see Denham 1998, 2007; Halberstadt, Denham, & Dunsmore, 2001). Further, emotional clarity directly calls on the meta-knowledge of one’s own emotional experiences, and has been studied as a distinct construct from other emotional processes, such as emotion differentiation, emotional attention, and emotional expression (Boden et al., 2013; Coffey, Berenbaum, & Kerns, 2003; Gohm & Clore, 2000). In the realm of emotion regulation, emotional clarity also stands alone from other central factors, including emotional acceptance, emotional control, and emotional awareness (Gratz & Roemer, 2004). Emotional clarity may be determined through reflection on these various emotional processes, but also may arise from other factors, such as beliefs about one’s identity (Boden et al., 2013). Research indicates that emotional clarity facilitates adaptive emotion regulation strategies, including reappraisal and acceptance (Boden & Thompson, 2015), whereas deficits in emotional clarity have been linked to poorer coping (Flynn & Rudolph, 2010). Theories suggest that emotional clarity difficulties may impair the interpersonal stress response such that individuals with poor emotional clarity may spend greater effort managing their emotional experiences and, consequently, have more difficulty directing resources toward adaptive coping responses (Gohm & Clore, 2000).
The literature on emotional clarity is limited, and only a small number of studies have examined its association with depression (Cha & Nock, 2009; Flynn & Rudolph, 2010; Hamilton, Hamlat, Stange, Abramson, & Alloy, 2014; Stange, Alloy, Flynn, & Abramson, 2013; Stange, Boccia et al., 2013; Rubenstein et al., 2015). These studies have generally examined emotional clarity as a moderator in the relationship between stress and other personal vulnerability factors and the occurrence of depression. For example, Hamilton et al. (2014) found that early pubertal timing, a major youth stressor, predicted increases in depressive symptoms among adolescents with poor emotional clarity, but only in girls. Cha and Nock (2009) similarly found that, among adolescents with a history of sexual abuse, the ability to understand one’s emotions exerted a protective effect against suicidal ideation and attempts. A study of late adolescents by Stange, Boccia, and colleagues (2013) found that higher emotional clarity buffered against the impact of several types of negative cognitive styles (dysfunctional attitudes, self-criticism, and neediness) on prospective increases in depressive symptoms. In another study by these same investigators, the interaction between negative cognitive styles and life events prospectively predicted depressive symptoms, but only among adolescents with lower emotional clarity (Stange, Alloy, et al., 2013). Finally, Flynn and Rudolph (2010) showed that maladaptive coping responses mediated the association between deficits in emotional clarity and youth depressive symptoms. The relationship between poor emotional clarity and negative outcomes also may have a cyclical pattern; research suggests that depressive symptoms, compounded with rumination, can lead to decreases in emotional clarity over time (Rubenstein et al., 2015). Taken together, these findings suggest that low emotional clarity may engender risk for depression, whereas high emotional clarity may be a protective factor for children and adolescents at risk for depression, perhaps facilitating appropriate implementation of adaptive coping responses, and therefore, buffering the effects of life stress and other vulnerabilities. Hence, efforts to understand the development of emotional clarity in youth may be important in promoting youth resilience and lessening the progression of depression into adulthood.
Family Factors
There is a well-established link between family functioning and adolescent depression, such that depressive symptoms and disorders have shown consistent associations with overall negative family climate, as well as with specific deficits such as low warmth, cohesion, and emotional availability and high conflict and control (Hughes & Gullone, 2008; Restifo & Bögels, 2009; Sander & McCarty, 2005). In fact, family relationships have shown a stronger association with adolescent depression than have peer relationships (e.g., Barrera & Garrison-Jones, 1992; McFarlane, Bellissimo, & Norman, 1995). Researchers have proposed that family dysfunction may impact youth depression by contributing to an environment of increased stress (Nomura, Wickramaratne, Warner, Mufson, & Weissman, 2002; Sander & McCarty, 2005). However, there also may be alternate (or additional) explanations for the relationship between family environment and youth depression (see Sheeber, Hops, & Davis, 2001) that are associated with particular family functional deficits.
One specific way in which family environment may influence depressive symptoms is by shaping a person’s beliefs about the acceptability and expression of emotions, and therefore how he or she copes with and expresses emotions when they occur. For example, children who grow up in environments with low emotional expressiveness and communication are not provided with models of how to accurately interpret and respond to emotions and may be discouraged from displaying and/or discussing their emotional experiences. On the other hand, children from families with high emotional expressiveness and communication may feel comfortable verbalizing and expressing their feelings, receiving the message that emotions are acceptable and welcome. In turn, this may facilitate development of the ability to recognize, discriminate, and understand one’s own emotions.
Although caregivers set the groundwork for children’s emotion regulation during the early years, research suggests that emotional development persists into adolescence, and family factors continue to be influential (cf., Brand & Klimes-Dougan, 2010; Zeman, Perry-Parrish, & Cassan, 2010). Despite normative changes in the parent-child relationship during adolescence, including greater strain and conflict, the family remains a vital source of support, and adolescents continue to use their parents as a guide for understanding and determining how to approach emotions (Morris, Silk, Steinberg, Myers, & Robinson, 2007; Yap, Allen, & Sheeber, 2007). This is true despite adolescents’ greater independence and peer focus (Sheeber, Allen, Davis, & Sorensen, 2000).
No studies to date have examined specifically the role of family factors in promoting adolescents’ emotional clarity, but a few studies have examined cross-sectional associations between adults’ ability to identify and describe feelings and retrospective reports of childhood family environment. For example, retrospective ratings of lower family expressiveness and poorer communication were associated with adults’ own self-reported difficulties with affective identification and communication (Berenbaum & James, 1994). Similarly, Yelsma and colleagues (Yelsma, Hovestadt, Anderson, & Nilsson, 2000) reported that college students who perceived their families of origin as lower in emotional expressiveness showed greater deficits in their ability to identify and describe their feelings on a measure of alexithymia. Lumley and colleagues (Lumley, Mader, Gramzow, & Papineau, 1996) also documented that both general family functioning difficulties and specific deficits in affective involvement were linked with difficulty identifying feelings. In another study that examined the contribution of various dimensions of retrospective family environment (cohesion, expressiveness, conflict, disengagement, sociability, enmeshment, organization, and parenting style) to alexithymia, poor family expressiveness was the only independent predictor (Kench & Irwin, 2000).
Research also shows that family factors are associated more broadly with youth emotion regulation (cf., Morris et al., 2007; Sheeber, Hops, & Davis, 2001; Yap et al., 2007). For example, warm, supportive parent-child relationships show associations with healthy child emotional competence and regulation, whereas negative parenting styles characterized by high conflict and hostility are associated with emotion regulation difficulties (Eisenberg, Cumberland, & Spinrad, 1998; Eisenberg, Losoya, et al., 2001; Morris et al., 2002). Additionally, research indicates that adolescents tend to have fewer emotional problems when parents engage in emotional communication (Ackard, Neumark-Sztainer, Story, & Perry, 2006; Stocker, Richmond, Rhoades, & Kiang, 2007). Given these findings, it is possible that the link between family functioning and adolescent depression is, at least in part, associated with deficits in emotional clarity.
Gender Differences
Gender differences in depression also appear to emerge during adolescence (Hankin & Abramson, 2001). Specifically, beginning around age 13 (or mid-puberty), female adolescents become twice as likely as males to experience depression, and this gender gap persists throughout adulthood (Hankin & Abramson, 2001; Merikangas et al., 2010). Explanations for the emergent gender gap during the transition to adolescence have included girls’ greater sensitivity to interpersonal factors, including family functioning difficulties (e.g., Hops, 1995). Indeed, interpersonal stress and family conflict are stronger predictors of depression for adolescent girls than for boys (Davies & Windle, 1997; Davies & Lindsay, 2004; Rudolph, 2002). Given such findings, Davies and Cummings (2006) recommend that researchers “delineate gender-specific pathways within models that integrate the study of children’s specific reactivity to conflict with indices of their global psychological adjustment” (p. 108). Although girls tend to report greater emotional clarity in general (Ciarrochi, Chan, & Bajgar, 2001), given their increased sensitivity to interpersonal/family processes, they may have lower emotional clarity in the face of family functioning deficits, compared to boys.
Hypotheses
Taken together, the above research suggests that emotional clarity may be an important component of emotion regulation impacting depression, and there may be utility in examining the development of this association in adolescents. Further, given that family members play a salient role in adolescent emotional development, family factors—particularly those associated with affective expression and communication—may impact adolescents’ emotional clarity, which may help to account for the established link between family functioning and youth depression. Finally, the process by which family factors affect emotional clarity and depression may differ between adolescent girls and boys. The present study first examined cross-sectional and longitudinal associations between family functioning, emotional clarity, and adolescent depressive symptoms. We hypothesized that emotional clarity would act as a mediator in the relationship between family functioning and adolescent depressive symptoms contemporaneously and over time. Family functioning was examined in terms of both general family environment and two specific family functioning domains theoretically assumed to shape adolescents’ emotional clarity based on the prior literature: affective expression and communication. Finally, we explored potential gender differences in this mediation model. Given girls’ greater sensitivity to interpersonal factors, including family functioning difficulties (Davies & Windle, 1997; Davies & Lindsay, 2004; Rudolph, 2002; Gore, Aseltine, & Colton, 1993), we hypothesized that family functioning would have a greater impact on depressive symptoms via emotional clarity for girls than for boys. For all analyses, we examined family functioning as reported by both adolescents and their mothers to gather a broader range of viewpoints and account for potential reporter discordance (De Los Reyes, Ohannessian, & Laird, 2015). We also controlled for maternal depressive symptoms given concerns of possible reporting biases by depressed mothers (De Los Reyes & Kazdin, 2005; Richters & Pellegrini, 1989).
Method
Participants and Procedures
Participants included 364 adolescents (ages 14–17 years old) and their primary female caregivers (referred to as “mothers” because 93% of caregivers were biological mothers). The overall sample was recruited as part of an ongoing longitudinal study designed to evaluate the emergence of depressive disorders among adolescents (see Alloy et al., 2012, for further study details). Participants were recruited from Philadelphia and its surrounding neighborhoods, encompassing a racially and socioeconomically diverse community (Caucasian = 45.7%, median income = $37,016, 26.2% below the poverty line; U.S. Census Bureau, 2012). Recruitment was primarily conducted by mailing study details throughout various Philadelphia middle schools (68% of the sample) or advertising in local newspapers (32% of the sample), although some participants were referred to the study by other participants. Dyads were excluded if either the adolescent or mother had restrictions that hindered their ability to adequately complete the regular assessments, including severe developmental or learning disabilities, experiencing psychosis, or the inability to read or speak English. All participants who met inclusion and exclusion criteria were invited to participate in the study, at which time female caregivers and adolescents provided written informed consent and assent, respectively. This study was completed with approval by the Institutional Review Board (IRB) at Temple University.
Eligible participants were invited to the laboratory and were briefed on study procedures and confidentiality. Before completion of study measures, mothers and their children provided written consents and assents, respectively. Adolescents and their mothers completed a baseline assessment, and were invited back once per year for prospective follow-ups. At each follow-up assessment, mothers completed measures of family functioning and their current depressive symptoms. Adolescents completed measures of family functioning, current depressive symptoms, and emotional clarity at each assessment. The family functioning measure was introduced to the study at the first follow-up (year 2); therefore, for the present analyses, Time 1 (T1) corresponds to the second yearly visit.
At the time of the present analysis, of the 364 dyads included in the current sample, 281 mother-youth dyads had completed measures at Time 2 (T2; 77% of T1 sample) and 174 dyads had completed measures at Time 3 (T3; 48% of T1 sample1). Follow-ups occurred roughly one year (T2; M = 340.54 days, SD = 107.27 days) and two years (T3; M = 724.64 days; SD = 144.94 days) after the T1 visit. Adolescents and their mothers were compensated for their participation at each study visit.
At T1, adolescent participants were evenly represented across gender (52.5% female) and self-identified race (51.4 % Caucasian/White, 48.6% African American/Black). Approximately 47% of families were eligible for subsidized school lunch, which takes into account family income and the number of dependents in the household to provide free school lunch to families of low socioeconomic status.
Measures
Emotional clarity
The Emotional Clarity Questionnaire (ECQ; Flynn & Rudolph, 2010) was completed by adolescents to assess their perceived abilities to identify emotional experiences. Adapted from a measure used with adults (Salovey, Mayer, Goldman, Turvey, & Palfai, 1995), the ECQ has seven items endorsed on a 1–5 Likert scale (e.g. “My feelings usually make sense to me”), with lower total scores reflecting greater deficits in emotional clarity. The ECQ has demonstrated significant convergent validity with behavioral tasks that involve processing and discriminating facial expressions of emotion (Flynn & Rudolph, 2010), and is associated with concurrent and prospective reports of adolescent depression (Stange, Alloy, Flynn, & Abramson, 2013). Cronbach’s alpha for our study yielded α’s = .88 (T1), .84 (T2), and .85 (T3).
Family functioning
The Family Assessment Measure III-General Scale (FAM-III G; Skinner, Steinhauer, & Santa-Barbara, 1995) was independently completed by adolescents and their mothers to assess family functioning at a systemic level. The FAM-III is informed by the Process Model of Family Functioning (Steinhauer, 1987), which integrates constructs important for the achievement of various family tasks. The fifty items yield six subscale scores (communication, affective expression, involvement, values and norms, control, role performance) and a Total Score to identify general effectiveness of family functioning. The Total score represents the average of subscale T-scores. For the current study, we utilized the total T-score, Affective Expression scale T-score, and Communication T-score. T-scores of 60 and higher are indicative of disturbances and problematic areas in the family system, whereas T-scores below 40 suggest effective family functioning. The FAM-III has demonstrated an ability to discriminate functioning between normative and problematic (e.g., alcoholic parents, major legal or school problems) families, is consistent with reports from other family functioning measures and the MMPI family scales, and reliably measures treatment outcomes of family therapy (for a review, see Skinner, Steinhaur, & Sitarenios, 2000). Internal consistencies in our study yielded α’s equal to .69 (T1), .65 (T2), and .67 (T3) for youth-reported Total T-score; and mother-reported Total T-score yielded α’s equal to .70 (T1), .69 (T2), and .60 (T3). Internal consistency for the Affective Expression scale yielded α’s equal to .74 (T1), .78 (T2), and .69 (T3) for youth-reported data, and α’s equal to .72 (T1), .75 (T2), and .79 (T3) for mother-reported data. The Communication scale yielded α’s equal to .70 (T1), .73 (T2), and .73 (T3) for youth-reported data, and .80 (T1), .71 (T2), .74 and (T3) for mother-reported data.
Adolescent depressive symptoms
The Children’s Depression Inventory (CDI; Kovacs, 1985) assesses depressive symptoms during childhood and adolescence. The 27-item questionnaire, which is based on cognitive, affective, and behavioral symptoms of depression, was completed by adolescents on a 0–2 scale with a possible range of zero to 54 (higher scores reflect more severe symptoms). The CDI was used as a continuous variable in all analyses. The CDI is widely recognized as a valid and reliable measure of depression in adolescents (for reviews, see Klein, Dougherty, & Olino, 2005 and Sitarenios & Kovacs, 1999). If suicidal ideation was endorsed, a trained interviewer conducted a suicide risk assessment following a comprehensive protocol to determine severity and appropriate intervention to ensure participant safety. Internal consistencies in our study yielded α’s = .89 (T1), .85 (T2), and .85 (T3).
Maternal depressive symptoms
The Beck Depression Inventory (BDI; Beck, Rush, Shaw, & Emory, 1979) was completed by mothers. This measure was used as a covariate in all analyses, given past findings that depression in mothers may bias their reporting (see De Los Reyes & Kazdin, 2005; Richters & Pellegrini, 1989). The BDI is a widely used, 21-item questionnaire that assesses the presence and severity of depressive symptoms over the past two weeks. Items are endorsed on a 0 – 3 scale, with higher scores indicating the presence of more severe depressive symptoms (range = 0–63). The BDI has demonstrated good internal and test-retest reliability, and is widely regarded as a valid measure of depressive symptoms in adults (Beck, Steer & Garbin, 1988). In our sample, internal consistency was α = .92 (T1), .91 (T2), and .86 (T3).
Data Analytic Strategy
Data were analyzed using Mplus Version 7.1. We employed Structural Equation Modeling (SEM) to examine the hypothesized relationships among variables. Prior to analyses, we examined assumptions of normality of variables. Given that some variables were not normally distributed (e.g., high kurtosis), robust full information maximum likelihood estimation was used to estimate the models. Our estimation method also permitted including cases with partial missing data. For each of our models, we ran the analysis twice: once in which we included adolescent-reported family functioning (Adolescent-report Model) and once in which we included mother-reported family functioning (Mother-report Model). This allowed for the examination of relationships between perceived family functioning, from both viewpoints, and the outcome variables of interest (i.e., emotional clarity and adolescent depressive symptoms). Prior to running models, we assessed the associations between the variables included in our models and the following potential covariates: adolescent age, race, free lunch eligibility (a proxy for socioeconomic status), and maternal BDI scores. Those variables with significant associations were included as covariates in all analyses.
The models tested: (1) direct cross-sectional relationships between variables at each time point; (2) the indirect relationships between overall family functioning and adolescent depressive symptoms via emotional clarity, at each time point; (3) direct longitudinal associations between measurements of each variable at each time point; (4) and the indirect relationship between T1 overall family functioning and T3 adolescent depressive symptoms via T2 emotional clarity. As indicated above, these analyses were run twice, once for the adolescent-report model, and once for the mother-report model. For exploratory analyses, we then re-ran adolescent- and mother-report models, this time replacing the measure of overall family functioning (FAM-III Total T-score) with T-scores for FAM-III subscales theoretically assumed to shape adolescents’ emotional clarity: Affective Expression and Communication scales (4 additional models). We next conducted moderated mediation analyses (Preacher, Rucker, & Hayes, 2007) to examine gender differences using MPlus syntax created by Stride and colleagues (Stride, Gardner, Catley, & Thomas, 2015). Again, these analyses were each run twice, once for the adolescent-report model, and once for the mother-report model.
We examined goodness of fit using multiple indices: the Root Mean Square Error of Approximation (RMSEA) and its 90% confidence interval (90% CI), the standardized root mean square residual (SRMR), the Comparative Fit Index (CFI), and the Tucker Lewis Index (TLI). Multiple fit indices were used as they assess different types of model fit (e.g., absolute fit, model parsimony), and, when used together, provide a more reliable, conservative evaluation (cf. Brown, 2006). Good model fit was determined based on published guidelines provided by Hu and Bentler (1999): RMSEA less than or equal to 0.06, SRMR less than or equal to 0.08, TLI greater than or equal to 0.95, and CFI greater than or equal to 0.95.
Mediation was confirmed by examining bootstrap confidence intervals (CI) for the indirect effects using BC Bootstrapping (Preacher & Hayes, 2008). With this approach, we can determine that the indirect effect is significantly different from zero, and that mediation is demonstrated, when zero does not lie within the 95% confidence interval (Preacher & Hayes, 2008).
Results
Participant Characteristics
At T1, adolescents ranged in age from 14–17 (M = 14.43, SD = 0.86). They were, on average, approximately 1 year older at T2 (M = 15.42, SD = 0.93) and 2 years older at T3 (M = 16.39, SD = 0.83). The sample was 52.5% female at T1, 51.8% female at T2, and 60.5% female at T3. There were no differences in age between males and females at any time point. Descriptive statistics for all measures are shown in Table 1, for the full sample and for males and females separately. As further shown in Table 1, t-tests indicated that emotional clarity was higher for males compared to females at all time points. Additionally, CDI scores were higher for females compared to males at T1 and T2, but not T3. Family variables did not differ for males versus females, based on adolescents’ or mothers’ reports, at any time point. Correlational analyses (Table 2) indicated that T1 maternal BDI was significantly associated with T1 CDI, T3 CDI, T1 ECQ, and T2 ECQ. T1 maternal BDI therefore was included as a covariate in all SEM analyses. T3 maternal BDI also was correlated with T3 CDI, but given the strong associations between maternal BDI scores at T1 and T3, we did not covary both BDI variables.
Table 1.
Descriptive Statistics for Measures at Each Time Point
| Mean ± SD | ||||
|---|---|---|---|---|
| Full Sample a | Male | Female | t | |
| T1 ECQ | 27.49 ± 5.59 | 28.89 ± 4.47 | 26.23 ± 6.19 | 4.71** |
| T2 ECQ | 27.82 ± 5.08 | 29.49 ± 4.25 | 26.32 ± 5.30 | 5.55** |
| T3 ECQ | 27.47 ± 5.58 | 28.93 ± 4.99 | 26.28 ± 5.78 | 3.19** |
| T1 CDI | 6.91 ± 6.25 | 5.81 ± 4.98 | 7.92 ± 7.10 | −3.09** |
| T2 CDI | 7.18 ± 5.89 | 6.02 ± 4.66 | 8.23 ± 6.67 | −3.14** |
| T3 CDI | 7.72 ± 8.19 | 6.45 ± 8.87 | 8.71 ± 7.51 | −1.78 |
| T1 FAM-III AR | 51.79 ± 7.59 | 51.49 ± 6.98 | 52.07 ± 8.10 | −0.71 |
| T2 FAM-III AR | 52.00 ± 8.68 | 51.48 ± 8.17 | 52.49 ± 9.15 | −0.91 |
| T3 FAM-III AR | 53.03 ± 9.13 | 52.20 ± 9.17 | 53.69 ± 9.13 | −0.80 |
| T1 FAM-III PR | 47.75 ± 7.82 | 46.98 ± 8.19 | 48.46 ± 7.42 | −1.78 |
| T2 FAM-III PR | 48.85 ± 9.04 | 48.19 ± 9.16 | 49.45 ± 8.92 | −1.08 |
| T3 FAM-III PR | 47.94 ± 8.85 | 47.82 ± 9.54 | 48.02 ± 8.44 | −0.10 |
T1 = Time 1, T2 = Time 2, T3 = Time 3, ECQ = Emotional Clarity Questionnaire, CDI = Children’s Depression Inventory, FAM-III AR = Family Assessment Measure-III, Adolescent-report, FAM-III PR = Family Assessment Measure-III, Parent-report.
Sample sizes differed at each time point as follows: T1 n = 364, T2 n = 281, T3 n = 174.
p < 0.05
p < 0.01
Table 2.
Intercorrelations between measures
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 ECQ | ||||||||||||||
| 2. T2 ECQ | .60** | |||||||||||||
| 3. T3 ECQ | .49** | .56** | ||||||||||||
| 4. T1 CDI | −.42** | −.33** | −.29** | |||||||||||
| 5. T2 CDI | −.28** | −.40** | −.35** | .59** | ||||||||||
| 6. T3 CDI | −.17* | −.28** | −.43** | .48** | .54** | |||||||||
| 7. T1 BDI | −.17** | −.13* | −.11 | .18** | .08 | .18* | ||||||||
| 8. T2 BDI | −.07 | −.08 | −.02 | .10 | .09 | .15 | .61** | |||||||
| 9. T3 BDI | −.04 | −.06 | −.15 | .10 | .14 | .21* | .59** | .63** | ||||||
| 10. T1 FAM-III AR | −.34** | −.29** | −.25** | .49** | .43** | .25** | .14* | .07 | .18* | |||||
| 11. T2 FAM-III AR | −.34** | −.34** | −.36** | .47** | .44** | .26** | .21** | .16* | .15 | .59** | ||||
| 12. T3 FAM-III AR | −.30** | −.32** | −.49** | .34** | .36** | .46** | .16 | .10 | .17 | .38** | .66** | |||
| 13. T1 FAM-III PR | −.20** | −.22** | −.26** | .22** | .13* | .11 | .23** | .18** | .20* | .28** | .31** | .18 | ||
| 14. T2 FAM-III PR | −.13* | −.12 | −.21** | .11 | .12 | .14 | .16* | .23** | .24** | .18** | .29** | .24* | .78** | |
| 15. T3 FAM-III PR | −.20 | −.15 | −.21 | .22 | .06 | .02 | .14 | −.01 | .14 | .24* | .36** | .27* | .78** | .87** |
T1 = Time 1, T2 = Time 2, T3 = Time 3, ECQ = Emotional Clarity Questionnaire, CDI = Children’s Depression Inventory, BDI = Beck Depression Inventory, FAM-III AR = Family Assessment Measure-III, Adolescent-report, FAM-III PR = Family Assessment Measure-III, Parent-report.
p < 0.05
p < 0.01
According to ANOVA, baseline depressive symptoms did not differ between adolescents who completed all three waves versus those who completed one or two waves (F = 1.91, p = .15). There also were no differences in race (χ² = .19, p =.66) or eligibility for subsidized school lunch (χ² = 2.62, p = .11) for participants who completed all time points versus those who did not.
Mediation Analyses
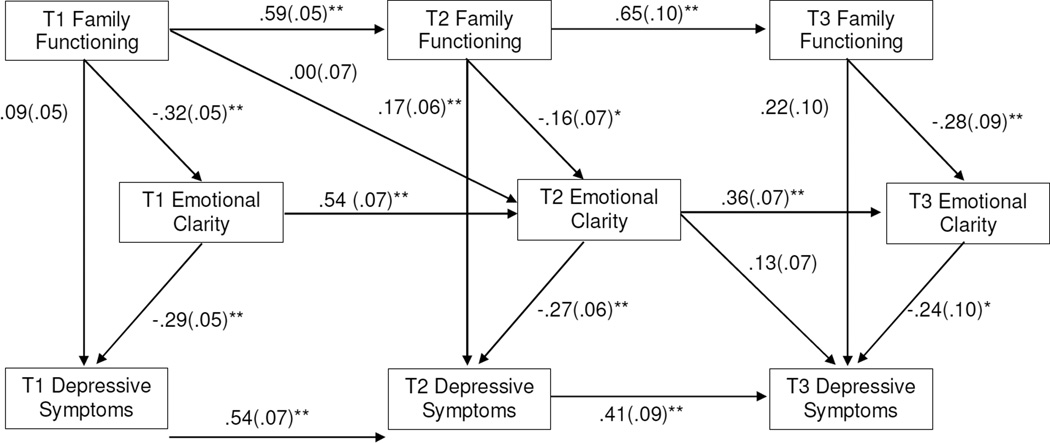
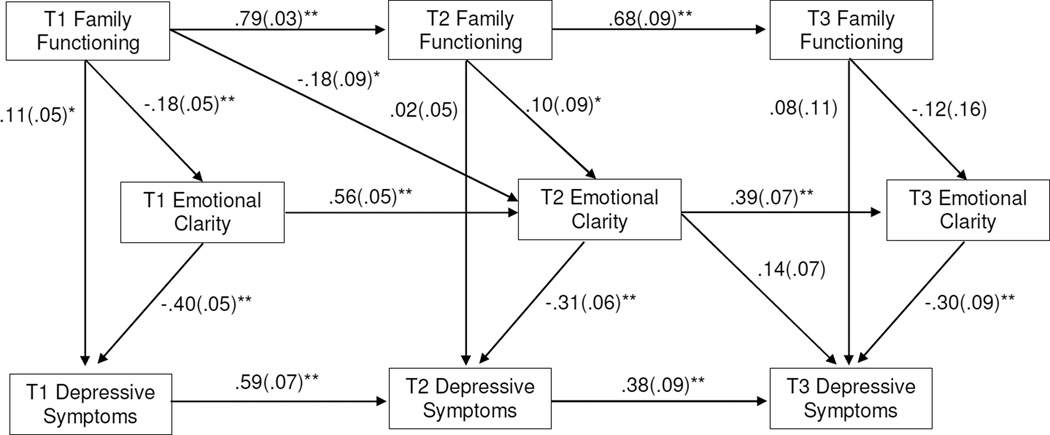
Figures 1 and 2 show the cross-sectional and longitudinal direct and indirect relationships between overall family functioning for adolescent-report and mother-report, respectively, emotional clarity, and adolescent depressive symptoms. Model fit indices are shown in Table 3. We report the standardized coefficients for our models.
Fig 1.
Path model of relationship between adolescent-reported family functioning, emotional clarity, and depressive symptoms. NOTE: Completely standardized results reported, estimate (standard error). For family functioning, higher values indicate worse functioning. * p < 0.05, ** p < 0.01. In the interest of graphical clarity, the following are not shown: covariate (T1 maternal depressive symptoms), paths from other control variables (i.e., variables at prior time points), and indirect paths. Cross-sectional indirect estimates from family functioning to depressive symptoms are as follows: T1 β = .09, SE = .02, p < .01; T2 β = .04, SE = .02, p < .05; T3 β = .07, SE = .03, p < .05. The indirect path from T1 family functioning to T3 depressive symptoms via T2 emotional clarity is as follows: β = .00, SE = .09, p = 1.00
Fig 2.
Path model of relationship between mother-reported family functioning, emotional clarity, and depressive symptoms.
NOTE: Completely standardized results reported, estimate (standard error). For family functioning, higher values indicate worse functioning. * p < 0.05, ** p < 0.01. In the interest of graphical clarity, the following are not shown: covariate (T1 maternal depressive symptoms), paths from other control variables (i.e., variables at prior time points), and indirect paths. Cross-sectional indirect estimates from family functioning to depressive symptoms are as follows: T1 β = .07, SE = .02, p < .01; T2 β = −.03, SE = .03, p = .26; T3 β = .04, SE = .05, p = .43. The indirect path from T1 family functioning to T3 depressive symptoms via T2 emotional clarity is as follows: β = −.03, SE = .02, p = .17
Table 3.
Model Fit Indices for Mediation Models
| FAM-III Score Included | χ2(13) | p-value | CFI | TLI | RMSEA | 90% CI | SRMR |
|---|---|---|---|---|---|---|---|
| Adolescent-Report | |||||||
| Overall | 28.39 | 0.01 | 0.98 | 0.91 | 0.06 | 0.03–0.09 | 0.05 |
| Affective Expression | 40.41 | 0.00 | 0.95 | 0.82 | 0.08 | 0.05–0.10 | 0.07 |
| Communication | 47.07 | 0.00 | 0.95 | 0.82 | 0.09 | 0.06–0.11 | 0.06 |
| Mother-Report | |||||||
| Overall | 20.54 | 0.08 | 0.99 | 0.96 | 0.04 | 0.00–0.07 | 0.03 |
| Affective Expression | 22.81 | 0.04 | 0.98 | 0.93 | 0.05 | 0.01–0.08 | 0.03 |
| Communication | 15.96 | 0.25 | 0.99 | 0.98 | 0.03 | 0.00–0.06 | 0.03 |
FAM-III = Family Assessment Measure-III, CFI = Comparative Fit Index, TLI = Tucker Lewis Index, RMSEA = Root Mean Square Error of Approximation, SRMR = standardized root mean square residual.
Adolescent-report models
Figure 1 shows the SEM model that includes adolescent-reported overall family functioning. This model showed acceptable fit (see Table 3). The cross-sectional direct relationships among variables all were statistically significant. Longitudinal paths for each variable from T1 to T2 to T3 were significant, demonstrating continuity of the constructs over time. The indirect paths from overall family functioning to depressive symptoms via emotional clarity were statistically significant, indicating mediation, at T1 (β = 0.09, SE = 0.02, 95% CI = 0.05–0.12, p < 0.001), T2 (β = 0.0, SE = 0.02, 95% CI = 0.01–0.06, p < 0.05) and T3 (β = 0.07, SE = 0.03, 95% CI = 0.01–0.13, p < 0.05). The 95% Bootstrap CIs for the indirect effects did not include zero and therefore confirmed the cross-sectional mediation. However, the indirect path from T1 family functioning to T3 adolescent depressive symptoms via T2 emotional clarity (while controlling for the previous time point) was not significant (β = 0.00, SE = 0.01, 95% CI = −0.03–0.03, p = 0.99), suggesting that this mediation relationship does not function longitudinally.
As shown in Table 3, when Affective Expression and Communication T-scores were included in their own models, neither model provided a good fit to the data. Despite this, the pattern of results was replicated such that, for both models, cross-sectional direct paths between the three variables (family functioning, emotional clarity, and depressive symptoms) at each time point, and longitudinal paths for each variable over time, remained significant (ps < .05). For the model that included Affective Expression, indirect effects remained significant at each time point: T1 (β = 0.90, SE = 0.02, 95% CI = 0.05–0.13, p = .00), T2 (β = .05, SE = 0.02, 95% CI = 0.01–0.09, p = .02) and T3 (β = 0.06, SE = 0.03, 95% CI = 0.003–0.10, p = 0.02). For the model that included Communication, indirect paths were significant at T1 (β = 0.90, SE = 0.02, 95% CI = 0.04–0.13, p = .00) and T2 (β = .05, SE = 0.02, 95% CI = 0.01–0.09, p = .01) but not T3 (β = 0.06, SE = 0.03, 95% CI = −0.01–0.13, p = 0.07). There was no evidence of longitudinal mediation when either Affective Expression or Communication were included in the model. Full statistical information for the models is available from the authors.
Mother-report models
Figure 2 shows the SEM model that includes mother-reported overall family functioning. This model fit the data well (see Table 3). The cross-sectional direct relationships among variables all were statistically significant, with one exception: the path from T3 family functioning to T3 adolescent depressive symptoms. Additionally, longitudinal paths for each variable from T1 to T2 to T3 all were significant, again demonstrating continuity of the constructs over time. The indirect paths from overall family functioning to depressive symptoms via emotional clarity were statistically significant at T1 (β = 0.07, SE = 0.02, 95% CI = 0.03– 0.12, p < 0.01)). The cross-sectional indirect paths were non-significant at T2 (β = −0.03, SE = 0.03, 95% CI = −0.09–0.03, p = 0.26) and T3 (β = 0.04, SE = 0.05, 95% CI = −0.06–0.02, p = 0.43). Again, the indirect path from T1 family functioning to T3 adolescent depressive symptoms via T2 emotional clarity (while controlling for the previous time point) was not significant (β = −0.03, SE = 0.02, 95% CI = −0.06–0.01, p = 0.17).
Models including mother-reported Affective Expression and Communication scale scores also each provided a good fit for the data (Table 3), and the pattern of results was replicated. For both models, cross-sectional direct paths between the three variables (family functioning, emotional clarity, and depressive symptoms) at each time point, and longitudinal paths for each variable over time, remained significant (ps < .05). For the model that included Affective Expression, indirect effects remained significant at T1 (β = 0.06, SE = 0.02, 95% CI = 0.01–0.11, p = .02) but not T2 or T3. For the model that included Communication, indirect paths were also significant at T1 (β = 0.05, SE = 0.02, 95% CI = 0.03–0.12, p = .00) but not T2 or T3. There was no evidence of longitudinal mediation when either Affective Expression or Communication were included in the model. Full statistical information for the models is available from the authors.
Moderated Mediation Analyses
We next re-ran the models to test for gender differences by testing for moderated mediation. The model that included adolescent-reported family functioning showed acceptable fit: χ² (28) = 55.87, p < 0.01; CFI = 0.98, TLI = 0.94, RMSEA = 0.05 (90% CI = 0.03 – 0.07), SRMR = 0.05. The model that included mother-reported family functioning also showed acceptable fit: χ² (28) = 51.17, p < 0.01; CFI = 0.98, TLI = 0.95, RMSEA = 0.05 (90% CI = 0.03 – 0.07), SRMR = 0.06. However, in both models, the indirect paths for males and females were not significantly different for any time point (all ps > .05), indicating that indirect effects did not differ by gender.
Post-hoc Analyses
Given that our longitudinal mediation analyses were non-significant, we investigated alternate directionality regarding the relationship among variables. Specifically, we assessed two additional models: 1) family functioning as a mediator in the relationship between emotional clarity and adolescent depressive symptoms over time (Post-hoc Model 1); 2) and emotional clarity as a mediator in the relationship between adolescent depressive symptoms and family functioning over time (Post-hoc Model 2). Both models were identical to the original models except that the variables were re-arranged as appropriate. Each post-hoc model was run twice, once for adolescent-reported family functioning, and once for mother-reported family functioning.
Post-hoc Model 1 provided a poorer fit for the data compared to the original model for adolescent-reported family functioning (χ2 [13] = 38.02, p < 0.01; CFI = 0.96, TLI = 0.86, RMSEA = 0.07 [90% CI = 0.05 – 0.10], SRMR = 0.07), and mother-reported family functioning χ2 [13] = 28.41, p < 0.01; CFI = 0.98, TLI = 0.92, RMSEA = 0.06 [90% CI = 0.03 – 0.09], SRMR = 0.05). For Post-hoc Model 1, the indirect paths from emotional clarity to depressive symptoms via family functioning were statistically significant at T1 for both the adolescent-report model (β = −0.13, SE = 0.04, p < 0.001; 95% CI = −0.24 – −0.05) and the mother-report model (β = −0.02, SE = 0.01, p < 0.05; 95% CI = −0.04–0.00), but not at other time points. The indirect path from T1 emotional clarity to T3 adolescent depressive symptoms via T2 family functioning (while controlling for the previous time point) was not significant for either adolescent- or mother-report.
For Post-hoc Model 2, the fit indices were slightly better than for the original model for both adolescent-reported family functioning χ2 [13] = 26.05, p < 0.05; CFI = 0.98, TLI = 0.93, RMSEA = 0.053 [90% CI = 0.02 −0.08], SRMR = 0.04) and mother-reported family functioning χ2 [13] = 17.69, p < 0.17; CFI = 0.99, TLI = 0.98, RMSEA = 0.03 [90% CI = 0.00 – 0.07], SRMR = 0.04). For Post-hoc Model 2, the indirect paths from adolescent depressive symptoms to family functioning via emotional clarity were statistically significant at T1 for both the adolescent-report model (β = 0.06, SE = 0.02, p < 0.05; 95% CI = 0.01 – 0.11) and the mother-report model (β = 0.05, SE = 0.02, p < 0.05; 95% CI = 0.00 – 0.10), but not at other time points. The longitudinal mediation analyses for Post-hoc Model 2, testing T2 emotional clarity as a mediator in the relationship between T1 adolescent depressive symptoms and T3 family functioning (while controlling for the previous time point), were non-significant for both the adolescent- and mother-report models.
Discussion
Given that family environment plays a major role in adolescent development, the present study examined the impact of family functioning on adolescent emotional clarity and depressive symptoms. As adolescence is a period of much change and growth, this investigation stretched across a period of about two years to clarify the relationships among the study variables at each of three time points separately and across time. Chiefly, the current study found that emotional clarity mediated the relationship between poor overall family functioning and depressive symptoms according to adolescents’ reports of family functioning at all time points contemporaneously, and according to mothers’ reports of family functioning at Time 1 only. There was no evidence of longitudinal mediation for adolescent- or mother-reported family functioning. Examining affective expression and communication, particular domains of family functioning hypothesized to be particularly linked with emotional clarity, did not improve the models. These results reveal important connections between the family environment, adolescent emotional understanding, and adolescent depressive symptoms at different points during adolescence.
The significant cross-sectional mediation models indicate that general family functioning is linked to the degree to which adolescents are able to understand and label their own emotional experiences, which, in turn, is associated with lower levels of depressive symptoms. The present findings are in accordance with three separate lines of research showing that: 1) interpersonal/family factors are consistent predictors of depression (McLeod, Weisz, & Wood, 2007; Sheeber, Hops, & Davis, 2001); 2) family factors are linked to youth emotion regulation, including the ability to understand and label emotions (Morris et al., 2007; Yap et al., 2007); and 3) low emotional clarity is associated with depressive symptoms (Flynn & Rudolph, 2010; Hamilton et al., 2014; Stange, Alloy, et al., 2013; Stange, Boccia et al., 2013). According to our mediation models, the relationship between family functioning and depression may be explained, at least in part, by deficits in emotional clarity. An alternate model conducted post-hoc indeed suggested that emotional clarity mediated the relationship between depressive symptoms and family functioning, and provided a slightly better fit for the data, but mediation was significant only at Time 1 (for both adolescent- and mother-reported family functioning). Similarly, a second post-hoc model indicated that family functioning mediated the relationship between emotional clarity and depressive symptoms at Time 1 only, but this model (for both reporters) provided a poor fit for the data. Thus, it is likely that a bi-directional relationship exists between depression and poor family functioning; indeed, past investigations often conceptualize links between children’s behavior and family dynamics in this way (Keenan-Miller, Peris, Axleson, Kowatch, & Miklowitz, 2012). Depressive symptoms in youth are associated with poor emotional clarity (e.g., Flynn & Rudolph, 2010), which may trigger dysfunction within the family unit and cause familiar relationships to suffer. Notably, this relationship may further perpetuate depressive symptoms by maintaining emotional clarity deficits, due to dysfunctional parenting or other issues within the family, such as poor communication. As family factors continue to be important throughout adolescent development, it is possible that poor family functioning exacerbates depression and impaired emotion regulation for youth who already experience these deficits.
Further, in an effort to determine whether particular family functioning domains were more relevant to our model compared to a measure of general family functioning, we examined affective expression and communication in separate models. We chose to examine these two family functioning domains given that prior research suggests that deficits in family affective expression and communication in childhood may predict adults’ difficulties with affective identification and communication (Berenbaum & James, 1994; Kench & Irwin, 2000; Yelsma et al., 2000). There was no improvement in the models when examining these individual domains (and for adolescent-report the model fit was worse), and patterns of associations were similar, compared to examining general family functioning. It is possible that the overall quality of the family environment is more important than any specific family factors. However, we also note that affective expression and communication were highly correlated with the general family functioning score; although these individual family functioning domains may be distinct factors (Skinner, Steinhauer, & Santa-Barbara, 1995), families that are functioning well in certain domains are likely also functioning well in other domains.
It is important to consider why the variables under study were interconnected only when measured together at the same time, but not longitudinally over adolescence. It may be the case that these relationships are only associated contemporaneously and do not influence one another over time. However, we recognize that all three variables were quite stable over time with strong positive correlations between time points, suggesting there may not have been enough variability over the two-year period to detect influences of the variables on one another. It also may be the case that emotional clarity is consolidated earlier in development and, by adolescence, is less malleable by environmental influences. Unfortunately, the vast majority of research on emotional development is focused on younger children. Although it is clear that use of more sophisticated emotion regulation strategies emerges in adolescence (Zeman et al., 2006), the literature provides little insight into how the ability to identify emotions changes as youth reach this stage. Future research assessing the prospective link between family functioning and emotional clarity earlier in development might help to answer this question.
Additionally, it is possible that other mechanisms may play more robust roles than emotional clarity in explaining the link between family functioning and depression. Past studies indicate that family environments that are less supportive and more conflict-ridden lead to depressive symptoms in youth over time (Sheeber et al., 1997). Consistently, youth tend to be more depressed in families where there is less attachment to and approval from parents (Sheeber et al., 2001). Other factors associated with the child may connect dysfunctional family environments to youth depression, such as poor perceptions of parents, negative cognitive style, and low self-esteem. Further, research indicates that parental characteristics may also impact these relationships, including psychopathology, stress, ineffective problem-solving skills, cognitive style, and parenting strategies (e.g., use of punishment). External factors, such as socioeconomic status, may also link poor family functioning with child depression (Sheeber et al., 2001). In the realm of emotion regulation, children often adopt strategies from their parents; thus, the link between poor family functioning and child depression may be mediated more strongly by parent emotion regulation strategies than youth emotion regulation (Sheeber et al., 2001). Thus, although emotional clarity may contribute to the relationship between familial dysfunction and child depression, other factors involving the child or parent might create a stronger link.
We also must consider why Time 1 was the only time point that the mediation model was significant for both adolescent- and mother-reports of family functioning, when the adolescents were 14 years of age on average. Over time, mother-reported family functioning did not predict depressive symptoms via emotional clarity levels. It is possible that as they aged, adolescents’ reports of poor family functioning were more reflective of low mood instead of actual family dynamics. Consistent with this, past research demonstrates that suicidal adolescents perceived their family functioning to be significantly worse than did their caregivers (Lipschitz, Yen, Weinstock, & Spirito, 2012). Additionally, parent-youth discrepancies in perceptions of family functioning are associated with higher levels of depressive symptomatology in youth (Ohannessian, Lerner, Lerner, & von Eye, 1995). We controlled for maternal depressive symptoms in all analyses, so mother-reported family functioning is less likely to have been influenced by such bias. Therefore, any reporter discrepancies may represent parents documenting more accurate versions of family functioning over time than their children. If this is true, it would make sense that findings were only significant at a younger age, given speculation (above) that emotional clarity might be less malleable over time.
Results from the moderated mediation analyses did not yield any gender differences in family functioning’s association with depressive symptoms via emotional clarity levels. We hypothesized that family functioning would have a greater impact on depressive symptoms via emotional clarity for girls than for boys given that girls tend to be more sensitive to interpersonal factors, such as difficulties in family relationships (Hops, 1995). However, gender did not moderate this association. Analyses of the main study variables revealed key gender differences in emotional clarity (higher for boys at all time points) and depressive symptoms (higher for girls at T1 and T2), but not in family functioning. Thus, adolescent girls are not only more vulnerable to experiencing depression, but (unexpectedly) also are more susceptible to having poorer abilities to understand and label their own emotions than their male peers. Although some past research indicates that girls tend to rate their emotional intelligence as higher than boys (Ciarrochi, Chan, & Bajgar, 2001), in the context of depression, girls generally experience more risk factors than do boys, such as ruminating in response to depressed mood, engaging in passive coping strategies, and experiencing stressful life events (Hankin et al., 1998; Jose & Brown, 2008; Nolen-Hoeksema, Larson, & Grayson, 1999). Rumination and emotional clarity may be especially linked for girls; Rubenstein and colleagues (2015) found that, for adolescent girls, rumination mediated the link between depression and poor emotional clarity over time.
The current study has several key strengths. Foremost, we measured the primary study variables at three distinct time points across a salient developmental period for the participants. By capturing family functioning, emotional clarity, and depressive symptoms at three times, we were able to identify how these variables are related both cross-sectionally and temporally. Measuring the study variables over time allowed for testing fully prospective mediation models that accounted for about two years’ time in the adolescents’ lives, which accounts for a period of significant life change. Further, family functioning was measured through both mothers’ reports and adolescents’ reports. Thus, the current study was able to collect a multi-faceted understanding of family dynamics, given that different members of the family, especially parents and children, have distinctive perspectives about the ways in which their families interact. This is an improvement on past research that has tended to rely solely on adolescents’ reports of both the mood and family variables (Sheeber et al., 2001). Additionally, the sophisticated statistical analysis allowed us to test a number of relationships simultaneously. Finally, the study included a large group of adolescents and their mothers and was inclusive of diverse racial and socioeconomic backgrounds, which contributes to the generalizability of the findings.
The study’s limitations provide opportunities for future research. First, this investigation relied solely on self-reports to gather information. It is possible that our cross-sectional mediation findings occurred because of adolescents’ mood-dependent reporting. Using a multi-method approach (e.g., questionnaires, interviews, observations, behavioral tasks) to capture family functioning, emotional clarity, and depressive symptoms might bolster the validity of the study and provide a more detailed understanding of the variables at hand. Second, the youth in our sample were in the early adolescent years at the start of our study. As noted above, it is possible that 1) family factors have a more significant impact on emotional clarity earlier in development, and 2) emotional clarity is consolidated earlier in development, and by adolescence becomes a more stable characteristic, regardless of changes in family environment. Future research would do well to examine these processes earlier in development, continuing to follow youth through adolescence when depression risk tends to increase. It also may be important to explore the influence of peers on emotional clarity given the increased salience of peer relationships during the adolescent years. Third, depressive symptoms were mild in our community sample of adolescents, which limited the ability to understand how these processes may interact in more severe psychopathology. Predictors of moderate depressive symptomatology may not be the same as those that predict clinical disorder (Sheeber et al., 2001). Future research might test our models in clinical samples. Finally, we only assessed female caregivers of the adolescents in our study. Additional studies could examine how fathers’/male caregivers’ assessments of family functioning impact adolescent emotional clarity and mood. However, it may be the case that mothers’ reports are more reliable than fathers’, as research suggests that mothers tend to be more engaged in their children’s emotional lives (Klimes-Dougan et al., 2007) and are more involved in parenting their adolescent children, compared to fathers (Paulson & Sputa, 1996).
Conclusion
Overall, the present study found that family functioning, emotional clarity, and depressive symptoms are strongly related constructs during various time points in adolescence. Specifically, low family functioning is indirectly associated with high depressive symptoms via low levels of emotional clarity in a cross-sectional manner. These results have important implications for parenting and adolescent mental health. Inasmuch as the way a family functions is immediately related to depressive symptoms via emotional clarity, it may be important for parents to promote the understanding and awareness of emotional experiences for children, especially during early adolescence. If parents recognize that their adolescent children may rely on them to be immediate guides for how to interpret emotional experiences, they may promote more emotional awareness and understanding in the moment, which could, in turn, lead to decreases in depressive symptoms for their children. Given that family functioning is intimately tied to adolescent depression, interventions such as family therapy that focus on parent-child dynamics may be useful to alleviate adolescent depression (Asarnow, Tompson, & Berk, 2005). Treatment interventions that emphasize improving family communication, especially communication about feelings, might be especially useful (e.g., Tompson, Boger, & Asarnow, 2012). Also, prevention programs for youth at risk for depression that focus on family communication about depression have shown promise (e.g., Beardslee, Wright, Gladstone, & Forbes, 2007). By incorporating family factors into our understanding of emotion regulation and the onset and maintenance of depressive symptoms during adolescence, we can gain deeper insight into adolescent mood and mental health.
Acknowledgments
Funding
This work was supported by National Institute of Mental Health grants MH79369 and MH101168 to Lauren B. Alloy.
Biographies
Rachel D. Freed, Ph.D., Temple University
Rachel D. Freed is a postdoctoral fellow at Temple University. She received her doctoral degree in clinical psychology from Boston University in 2014. Her research focuses on identifying factors impacting vulnerability to mood disorders in youth at familial risk, with a particular focus on family environmental factors.
Liza M. Rubenstein, M.A., Temple University
Liza M. Rubenstein is a doctoral student in clinical psychology at Temple University. Her research interests include examining risk and resilience to depression during adolescence, with a focus on the development of emotional clarity and its impact on psychopathology.
Issar Daryanani, M.A., Temple University
Issar Daryanani is a doctoral student in clinical psychology at Temple University. His major research interests include understanding protective/risk factors associated with psychosocial development of youth in single-mother families.
Thomas M. Olino, Ph.D., Temple University
Thomas M. Olino is an Assistant Professor at Temple University. He received his doctorate in Clinical Psychology from Stony Brook University. His major research interests include the role of positive emotionality and reward-related brain functioning in the development of depressive disorders and, more broadly, understanding the developmental psychopathology of depressive disorders in children and adolescents.
Lauren B. Alloy, Ph.D., Temple University
Lauren B. Alloy is Laura H. Carnell Professor and Joselph Wolpe Distinguished Faculty in the Department of Psychology at Temple University and is currently the Director of Clinical Training for the Temple Clinical Psychology Ph.D. program. Her major research interests are in understanding the cognitive, developmental, psychosocial, and biological mechanisms involved in the onset, course, and treatment of unipolar depression and bipolar disorder.
Footnotes
As the larger study is ongoing, many participants had not yet been scheduled for their T2 and T3 assessments at the time of the present analyses.
Conflicts of Interest
The authors report no conflicts of interest.
Authors’ Contribution
RDF conceived of the study, designed and performed the statistical analysis, and wrote sections of the manuscript; LMR wrote sections of the manuscript; ID wrote sections of the manuscript; TMO assisted with the statistical design and analysis and edited drafts of the manuscript; LBA designed the larger study from which the current sample was drawn and helped to draft the manuscript. All authors read and approved the final manuscript.
Ethical Standards
Ethical approval
This study was approved by the institution’s internal review board and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
All persons gave their informed consent prior to their inclusion in the study.
References
- Ackard DM, Neumark-Sztainer D, Story M, Perry C. Parent-child connectedness and behavioral and emotional health among adolescents. Am J Prev Med. 2006;30(1):59–66. doi: 10.1016/j.amepre.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Black SK, Young ME, Goldstein KE, Shapero BG, Stange JP, Abramson LY. Cognitive vulnerabilities and depression versus other psychopathology symptoms and diagnoses in early adolescence. J Clin Child Adolesc Psychol. 2012;41(5):539–560. doi: 10.1080/15374416.2012.703123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Tompson MC, Berk M. Adolescent depression: Family focused treatment strategies. In: Pinsof W, Lebow J, editors. Family Psychology: The Art of the Science. New York: Oxford University Press; 2005. [Google Scholar]
- Bankier B, Aigner M, Bach M. Alexithymia in DSM-IV disorder - comparative evaluation of somatoform disorder, panic disorder, obsessive-compulsive disorder, and depression. Psychosomatics. 2001;42(3):235–240. doi: 10.1176/appi.psy.42.3.235. [DOI] [PubMed] [Google Scholar]
- Barrera M, Garrison-Jones C. Family and peer social support as specific correlates of adolescent depressive symptoms. Journal of Abnormal Child Psychology. 1992 Feb;20(92):1–16. doi: 10.1007/BF00927113. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Wright EJ, Gladstone TRG, Forbes P. Long-term effects from a randomized trial of two public health preventive interventions for parental depression. Journal of Family Psychology. 2007;21(4):703–713. doi: 10.1037/0893-3200.21.4.703. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BK, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. [Google Scholar]
- Berenbaum H, James T. Correlates and retrospectively reported antecedents of alexithymia. Psychosom Med. 1994;56(4):353–359. doi: 10.1097/00006842-199407000-00011. [DOI] [PubMed] [Google Scholar]
- Boden MT, Thompson RJ. Facets of emotional awareness and associations with emotion regulation and depression. Emotion. 2015;15(3):399–410. doi: 10.1037/emo0000057. [DOI] [PubMed] [Google Scholar]
- Boden MT, Thompson RJ, Dizén M, Berenbaum H, Baker JP. Are emotional clarity and emotion differentiation related? Cognition & Emotion. 2013;27(6):961–978. doi: 10.1080/02699931.2012.751899. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory Factor Analysis for Applied Research. New York: Guilford Press; 2006. [Google Scholar]
- Burklund LJ, Creswell JD, Irwin MR, Lieberman MD. The common and distinct neural bases of affect labeling and reappraisal in healthy adults. Front Psychol. 2014;5:221. doi: 10.3389/fpsyg.2014.00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha C, Nock M. Emotional intelligence is a protective factor for suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2009;48(4):422–430. doi: 10.1097/CHI.0b013e3181984f44. [DOI] [PubMed] [Google Scholar]
- Ciarrochi J, Chan AYC, Bajgar J. Measuring emotional intelligence in adolescents. Personality and Individual Differences. 2001;31(7):1105–1119. [Google Scholar]
- Coffey E, Berenbaum H, Kerns JG. The dimensions of emotional intelligence, alexithymia, and mood awareness: Associations with personality and performance on an emotional Stroop task. Cognition and Emotion. 2003;17:671–679. doi: 10.1080/02699930302304. [DOI] [PubMed] [Google Scholar]
- Crone EA, Dahl RE. Understanding adolescence as a period of social-affective engagement and goal flexibility. Nature Reviews Neuroscience. 2012;13(9):636–650. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]
- Davies PT, Cummings EM. Interparental discord, family process, and developmental psychopathology. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology, Vol 3: Risk, Disorder, and Adaptation. Hoboken, NJ, US: John Wiley & Sons Inc; 2006. [Google Scholar]
- Davies PT, Lindsay LL. Interparental conflict and adolescent adjustment: why does gender moderate early adolescent vulnerability? Journal of Family Psychology. 2004;18(1):160–170. doi: 10.1037/0893-3200.18.1.160. [DOI] [PubMed] [Google Scholar]
- Davies PT, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Dev Psychol. 1997;33(4):657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131(4):483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Ohannessian CM, Laird RD. Developmental changes in discrepancies between adolescents’ and their mothers’ views of family communication. Journal of Child and Family Studies. 2015 doi: 10.1007/s10826-015-0275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denham SA. Emotional development in young children. New York: Guilford Press; 1998. [Google Scholar]
- Denham SA. Dealing with feelings: How children negotiate the worlds of emotions and social relationships. Cognition, Brain, Behavior. 2007;11(1):1. [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychol Inq. 1998;9(4):241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Losoya S, Fabes RA, Guthrie IK, Reiser M, Murphy B, Padgett SJ. Parental socialization of children’s dysregulated expression of emotion and externalizing problems. Journal of Family Psychology. 2001;15(2):183–205. doi: 10.1037//0893-3200.15.2.183. [DOI] [PubMed] [Google Scholar]
- Flynn M, Rudolph KD. The contribution of deficits in emotional clarity to stress responses and depression. J Appl Dev Psychol. 2010;31(4):291–297. doi: 10.1016/j.appdev.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner PW, Dunsmore JC, Southam-Gerrow M. Mother-child conversations about emotions: Linkages to child aggression and prosocial behavior. Social Development. 2008;17(2):259–277. [Google Scholar]
- Garside RB, Klimes-Dougan B. Socialization of discrete negative emotions: Gender differences and links with psychological distress. Sex Roles. 2002;47(3-4):115–128. [Google Scholar]
- Gohm CL, Clore GL. Individual differences in emotional experience: Mapping available scales to processes. Personality and Social Psychology Bulletin. 2000;26(6):679–697. [Google Scholar]
- Gores S, Aseltine RH, Colten ME. Gender, social-relational involvement and depression. Journal of Research on Adolescence. 1993;3(2):101–125. [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotional refulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotional Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Gyurak A, Gross JJ, Etkin A. Explicit and implicit emotion regulation: a dual-process framework. Cogn Emot. 2011;25(3):400–412. doi: 10.1080/02699931.2010.544160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halberstadt AG, Denham SA, Dunsmore JC. Affective social competence. Social Development. 2001;10(1):79–119. [Google Scholar]
- Halberstadt AG, Eaton KL. A meta-analysis of family expressiveness and children’s emotion expressiveness and understanding. Marriage & Family Review. 2002;34(1-2):35–62. [Google Scholar]
- Hamilton JL, Hamlat EJ, Stange JP, Abramson LY, Alloy LB. Pubertal timing and vulnerabilities to depression in early adolescence: differential pathways to depressive symptoms by sex. J Adolesc. 2014;37(2):165–174. doi: 10.1016/j.adolescence.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: an elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127(6):773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hare AL, Marston EG, Allen JP. Maternal acceptance and adolescents’ emotional communication: a longitudinal study. J Youth Adolesc. 2011;40(6):744–751. doi: 10.1007/s10964-010-9586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis a regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depress Anxiety. 2012;29(5):409–416. doi: 10.1002/da.21888. [DOI] [PubMed] [Google Scholar]
- Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. Journal of Psychosomatic Research. 2000;48(1):99–104. doi: 10.1016/s0022-3999(99)00083-5. [DOI] [PubMed] [Google Scholar]
- Hops H. Age-specific and gender-specific effects of parental depression: A commentary. Developmental Psychology. 1995;31(3):428–431. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Hughes EK, Gullone E. Internalizing symptoms and disorders in families of adolescents: A review of family systems literature. Clinical Psychology Review. 2008;28(1):92–117. doi: 10.1016/j.cpr.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Jose PE, Brown I. When does the gender difference in rumination begin? Gender and age differences in the use of rumination by adolescents. Journal of Youth and Adolescence. 2008;37(2):180–192. [Google Scholar]
- Kench S, Irwin HJ. Alexithymia and childhood family environment. Journal of Clinical Psychology. 2000;56(6):737–745. doi: 10.1002/(sici)1097-4679(200006)56:6<737::aid-jclp4>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Peris T, Axelson D, Kowatch RA, Miklowitz DJ. Family functioning, social impairment, and symptoms among adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(10):1085–1094. doi: 10.1016/j.jaac.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, Olino TM. Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):412–432. doi: 10.1207/s15374424jccp3403_3. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Brand AE, Zahn-Waxler C, Usher B, Hastings PD, Kendziora K, Garside RB. Parental emotion socialization in adolescence: Differences in sex, age and problem status. Social Development. 2007;16(2):326–342. [Google Scholar]
- Kovacs M. The Childrens Depression Inventory. Psychopharmacology Bulletin. 1985;21(4):995–998. [PubMed] [Google Scholar]
- Kovacs M, Joormann J, Gotlib IH. Emotion (dys)regulation and links to depressive disorders. Child Development Perspectives. 2008;2(3):149–155. doi: 10.1111/j.1750-8606.2008.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koven NS, Thomas W. Mapping facets of alexithymia to executive dysfunction in daily life. Personality and Individual Differences. 2010;49(1):24–28. [Google Scholar]
- Kuebli J, Butler S, Fivush R. Mother-child talk about past emotions: Relations of maternal language and child gender over time. Cognition & Emotion. 1995;9(2-3):265–283. [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(6):809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Lieberman MD, Inagaki TK, Tabibnia G, Crockett MJ. Subjective responses to emotional stimuli during labeling, reappraisal, and distraction. Emotion. 2011;11(3):468–480. doi: 10.1037/a0023503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipschitz J, Yen S, Weinstock L, Spirito A. Adolescent and caregiver perception of family functioning: Relation to suicide ideation and attempts. Psychiatry Research. 2012;200(2-3):400–403. doi: 10.1016/j.psychres.2012.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, Mader C, Gramzow J, Papineau K. Family factors related to alexithymia characteristics. Psychosomatic Medicine. 1996;58(3):211–216. doi: 10.1097/00006842-199605000-00003. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Weisz JR, Wood JJ. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007;27(8):986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- McFarlane AH, Bellissimo A, Norman GR. The role of family and peers in social self-efficacy: Links to depression in adolescence. American Journal of Orthopsychiatry. 1995;65(3):402. doi: 10.1037/h0079655. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui LH, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16(2):361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Sessa FM, Avenevoli S, Essex MJ. Temperamental vulnerability and negative parenting as interacting predictors of child adjustment. Journal of Marriage and Family. 2002;64(2):461–471. [Google Scholar]
- Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77(5):1061–1072. doi: 10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- Nomura Y, Wickramaratne PJ, Warner V, Mufson L, Weissman MM. Family discord, parental depression and psychopathology in offspring: Ten-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(4):402–409. doi: 10.1097/00004583-200204000-00012. [DOI] [PubMed] [Google Scholar]
- Ohannessian CM, Lerner RM, Lerner JV, von Eye A. Discrepancies in adolescents’ and parents’ perceptions of family functioning and adolescent emotional adjustment. Journal of Early Adolescence. 1995;15(4):490–516. [Google Scholar]
- Otterpohl N, Wild E. Cross-lagged relations among parenting, children’s emotion regulation, and psychosocial adjustment in early adolescence. J Clin Child Adolesc Psychol. 2015;44(1):93–108. doi: 10.1080/15374416.2013.862802. [DOI] [PubMed] [Google Scholar]
- Paulson SE, Sputa CL. Patterns of parenting during adolescence: perceptions of adolescents and parents. Adolescence. 1996;31(122):369–381. [PubMed] [Google Scholar]
- Porges SW, Doussard-Roosevelt JA, Maiti AK. Vagal tone and the physiological regulation of emotion. Monographs of the Society for Research in Child Development. 1994;59(2/3):167–186. [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Raikes HA, Thompson RA. Conversations about emotion in high-risk dyads. Attach Hum Dev. 2008;10(4):359–377. doi: 10.1080/14616730802461367. [DOI] [PubMed] [Google Scholar]
- Restifo K, Bögels S. Family processes in the development of youth depression: Translating the evidence to treatment. Clinical Psychology Review. 2009;29(4):294–316. doi: 10.1016/j.cpr.2009.02.005. [DOI] [PubMed] [Google Scholar]
- Richters J, Pellegrini D. Depressed mothers’ judgments about their children: an examination of the depression-distortion hypothesis. Child Development. 1989;60(5):1068–1075. doi: 10.1111/j.1467-8624.1989.tb03537.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein LM, Hamilton JL, Stange JP, Flynn M, Abramson LY, Alloy LB. The cyclical nature of depressed mood and future risk: Depression, rumination, and deficits in emotional clarity in adolescent girls. J Adolesc. 2015;42:68–76. doi: 10.1016/j.adolescence.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. J Adolesc Health. 2002;30(4 Suppl):3–13. doi: 10.1016/s1054-139x(01)00383-4. [DOI] [PubMed] [Google Scholar]
- Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional attention, clarity, and repair: Exploring emotional intelligence using the Trait Meta-Mood Scale. In: Pennebaker J, editor. Emotion, Disclosure, & Health. Washington, DC: American Psychological Association; 1995. pp. 125–154. [Google Scholar]
- Sander JB, McCarty CA. Youth depression in the family context: Familial risk factors and models of treatment. Clinical Child and Family Psychology Review. 2005;8(3):203–219. doi: 10.1007/s10567-005-6666-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25(4):333–344. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Allen N, Davis B, Sorensen E. Regulation of negative affect during mother-child problem-solving interactions: adolescent depressive status and family processes. J Abnorm Child Psychol. 2000;28(5):467–479. doi: 10.1023/a:1005135706799. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4(1):19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Sifneos PE. The prevalence of ‘alexithymic’ characteristics in psychosomatic patients. Psychotherapy and Psychosomatics. 1973;22:255–262. doi: 10.1159/000286529. [DOI] [PubMed] [Google Scholar]
- Sitarenios G, Kovacs M. Use of the Children’s Depression Inventory. In: Maruish ME, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. Mahwah, NJ: Erlbaum; 1999. pp. 267–298. [Google Scholar]
- Skinner H, Steinhauer P, Sitarenios G. Family Assessment Measure (FAM) and process model of family functioning. Journal of Family Therapy. 2000;22(2):190–210. [Google Scholar]
- Skinner HA, Steinhauer PD, Santa-Barbara J. Family Assessment Measure – III Manual. Toronto, Canada: Multi Health Systems; 1995. [Google Scholar]
- Stange JP, Boccia AS, Shapero BG, Molz AR, Flynn M, Matt LM, Alloy LB. Emotion regulation characteristics and cognitive vulnerabilities interact to predict depressive symptoms in individuals at risk for bipolar disorder: A prospective behavioural high-risk study. Cognition & Emotion. 2013;27(1):63–84. doi: 10.1080/02699931.2012.689758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Alloy LB, Flynn M, Abramson LY. Negative inferential style, emotional clarity, and life stress: Integrating vulnerabilities to depression in adolescence. Journal of Clinical Child and Adolescent Psychology. 2013;42(4):508–518. doi: 10.1080/15374416.2012.743104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, Hamilton JL, Abramson LY, Alloy LB. A vulnerability-stress examination of response styles theory in adolescence: Stressors, sex differences, and symptom specificity. Journal of Clinical Child and Adolescent Psychology. 2014;43(5):813–827. doi: 10.1080/15374416.2013.812037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegge H, Terwogt MM. Awareness and regulation of emotion in typical and atypical development. In: Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford Press; 2007. [Google Scholar]
- Steinhauer PD. The family as a small group: the Process Model of Family Functioning. In: Jacob T, editor. Family Interaction and Psychopathology. New York: Plenum; 1987. pp. 67–115. [Google Scholar]
- Stocker CM, Richmond MK, Rhoades GK, Kiang L. Family emotional processes and adolescents’ adjustment. Social Development. 2007;16(2):310–325. [Google Scholar]
- Stride CB, Gardner S, Catley N, Thomas F. Mplus code for mediation, moderation, and moderated mediation models. 2015 Retrieved from http://www.offbeat.group.shef.ac.uk/FIO/mplusmedmod.htm.
- Sturge-Apple ML, Davies PT, Boker SM, Cummings EM. Interparental discord and parenting: Testing the moderating roles of child and parent gender. Parenting-Science and Practice. 2004;4(4):361–380. [Google Scholar]
- Tompson MC, Boger KD, Asarnow JR. Enhancing the developmental appropriateness of treatment for depression in youth: Integrating the family in treatment. Child and Adolescent Psychiatric Clinics of North America. 2012;21(2):345. doi: 10.1016/j.chc.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. State & county Quickfacts: Philadelphia County, PA. 2012 Retrieved from http://quickfacts.census.gov/qfd/states/42/42600000.html.
- Yap MBH, Allen NB, Sheeber L. Using an emotion regulation framework to understand the role of temperament and family processes in risk for adolescent depressive disorders. Clinical Child and Family Psychology Review. 2007;10(2):180–196. doi: 10.1007/s10567-006-0014-0. [DOI] [PubMed] [Google Scholar]
- Yelsma P, Hovestadt AJ, Anderson WT, Nilsson JE. Family-of-origin expressiveness: measurement, meaning, and relationship to alexithymia. Journal of Marital and Family Therapy. 2000;26(3):353–363. doi: 10.1111/j.1752-0606.2000.tb00304.x. [DOI] [PubMed] [Google Scholar]
- Zeman J, Cassano M, Perry-Parrish C, Stegall S. Emotion regulation in children and adolescents. J Dev Behav Pediatr. 2006;27(2):155–168. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]
- Zeman J, Perry-Parrish C, Cassano M. Parent-child discussions of anger and sadness: the importance of parent and child gender during middle childhood. New Dir Child Adolesc Dev. 2010;(128):65–83. doi: 10.1002/cd.269. [DOI] [PubMed] [Google Scholar]