Abstract
Objective
To study the causes of head injuries among the paediatric population in Singapore, and the association between causes and mortality, as well as the need for airway or neurosurgical intervention.
Design
This is a prospective observational study utilising data from the trauma surveillance system from January 2011 to March 2015.
Setting
Paediatric emergency departments (EDs) of KK Women's and Children's Hospital and the National University Health System.
Participants
We included children aged <16 years presenting to the paediatric EDs with head injuries who required a CT scan, admission for monitoring of persistent symptoms, or who died from the head injury. We excluded children who presented with minor mechanisms and those whose symptoms had spontaneously resolved.
Primary and secondary outcome measures
Primary composite outcome was defined as death or the need for intubation or neurosurgical intervention. Secondary outcomes included length of hospital stay and type of neurosurgical intervention.
Results
We analysed 1049 children who met the inclusion criteria. The mean age was 6.7 (SD 5.2) years. 260 (24.8%) had a positive finding on CT. 17 (1.6%) children died, 52 (5.0%) required emergency intubation in the ED and 58 (5.5%) underwent neurosurgery. The main causes associated with severe outcomes were motor vehicle crashes (OR 7.2, 95% CI 4.3 to 12.0) and non-accidental trauma (OR 5.8, 95% CI 1.8 to 18.6). This remained statistically significant when we stratified to children aged <2 years and performed a multivariable analysis adjusting for age and location of injury. For motor vehicle crashes, less than half of the children were using restraints.
Conclusions
Motor vehicle crashes and non-accidental trauma causes are particularly associated with poor outcomes among children with paediatric head injury. Continued vigilance and compliance with injury prevention initiatives and legislature are vital.
Keywords: child, accidents, TRAUMA MANAGEMENT
Strengths and limitations of this study.
This is the first report comprising combined paediatric data on head injuries from the trauma surveillance databases in both paediatric centres in Singapore.
The causes of injuries were prospectively collected.
Detailed coding of injury data may have differed between the institutions.
This study specifically describes the surveillance and circumstances surrounding paediatric head injuries. This is because paediatric head injuries are especially common and have long-lasting consequences in children.
Introduction
Head injuries continue to impose a large burden on the healthcare system and on society. An estimated 4.8 million patient visits per year in the USA required evaluation for traumatic brain injuries (TBI).1 Injury control initiatives in the past decade have resulted in a change in the injury landscape, reduced deaths from motor vehicle accidents and driven the institution of legislation to promote safety.2 Other advances in the acute care and resuscitation of the severely head-injured patient have improved patient outcomes as a whole. However, severely head-injured patients continue to suffer death and long-term neurological deficits from these injuries.
Children, in particular, are extremely susceptible to head injuries. Significant brain trauma can bring about long-term consequences on the child, as well as on the family unit3 and on society as a whole. Severe injuries may blunt the child's motor development and compromise the child's cognitive abilities.4 Children with moderate—severe TBI generally experience a greater decrease in health-related quality of life immediately after the injury.5 This study demonstrated that the effect was, however, mitigated by 18 months post-TBI. Even among mild head injuries, some have lamented the lack of knowledge surrounding the long-term effects of patients subjected to repeated insults.6
Children suffer head injuries from different causes. In the USA, falls constitute the most frequent mechanism for children aged under 12 years, while adolescents are more prone to assaults, motor vehicle crashes and sports injuries.7 Motorcycles (including off-road motorcycling) in particular have received particular attention,8 with the lack of compliance to helmets disconcerting in some countries.9 Concerning objects associated with significant head injuries, advocates have cautioned especially on (fallen or struck by) television-related injuries10 11 that range from concussion to intracranial bleeds and death. Among the sports that are associated with head injuries, ice hockey, soccer and football feature heavily.12 Abusive head trauma (AHT), or head injuries secondary to non-accidental trauma (NAT), are an especially vulnerable group—these injured children are known to have poor outcomes, with a higher rate of mortality and multiple injuries.13 14
In our own population, falls constitute the most common mechanism among the paediatric head-injured population, especially among those aged <2 years. Motor vehicle crashes independently predict for severe injury.15 16
In this study, we extended the previous work to include both paediatric emergency departments (EDs) in the country. We aim to study the head-injured paediatric population and, in particular, their causes of injuries, correlating these causes with the severity of outcomes. We hypothesise that although falls and sports injuries are common, children who suffer motor vehicle crashes and NAT are more likely to die and suffer brain injuries that require airway and neurosurgical intervention.
Methodology
Design
This is an observational study from January 2011 to March 2015, involving tertiary paediatric centres in Singapore. KK Women's and Children's Hospital (KKH) and National University Health System (NUHS) together see the bulk of paediatric injuries in the country, and are both level 1 trauma centres. The injury surveillance was started in January 2011 as part of the National Trauma Registry, empowering prospective collection of data for all injured children who present to both institutions.
Patients were included from chart review once they fulfilled the necessary ICD diagnosis codes for head injuries.
Inclusion criteria
We included children aged <16 years who presented to the EDs with head injuries and who were admitted for further monitoring. We also included all children who died in the ED due to head injuries.
Exclusion criteria
We excluded children with low-mechanism falls and those who sustained minor contusion injuries to the face and scalp. Children whose symptoms (eg, vomiting, headache) resolved and who were not admitted were excluded from this study.
Standardisation of definitions
Children with a decreased Glasgow Coma Scale (GCS) had a CT of the brain ordered from the ED and were then subsequently admitted. At the start of the study period, both institutions did not practise ordering CT of the brain at the level of the ED with the aim of discharge if the CT was negative. Both institutional protocols required children with symptoms and signs suggestive of traumatic brain injury to be admitted for monitoring instead. Starting January 2013, one of the institutions (NUHS) changed the head injury protocol to allow for monitoring in the ED for up to 6 h, with a CT of the brain ordered from the ED if indicated and, if normal, the patient could be discharged from the ED. Hence, we included the latter group that clinically warranted a CT scan from the ED and were subsequently discharged if the CT was normal. Where there was contention whether the child's presentation was attributed to the head injury or other causes (eg, seizures or altered mental status), this was highlighted to the team and resolved with a review of the medical records and patients’ subsequent investigations.
Data collection
The following were collected as part of the prospective injury surveillance: Demographic details including the child's age, gender and ethnicity. The intent of injury (unintentional, assault, self-harm or unknown) and the primary cause of injury (fall, motor vehicle crash, sports injury, NAT, interpersonal violence or others) were documented. If the child had suffered a fall, the height of the fall was documented. If the child was involved in a motor vehicle crash, it was recorded if he was a pedestrian, cyclist, motor vehicle front or back passenger, motorbike front or back passenger. The use of restraints (car child seat, seat belt and helmet) was included where documented. In our population, we separated the NATs (where the alleged perpetrator is a caregiver/custodian or trusted member in the household) and interpersonal violence—the latter comprised mainly assault incidents in school. Details surrounding the object involved in the trauma and the location of the injury were also studied. We reviewed the disposition from the ED, the specific intracranial injury and the rates of CT of the brain being performed.
Assessment of main outcomes
Severe outcomes were defined as death, the need for intubation or neurosurgical intervention. (We do not perform intubation only for neuroimaging studies in the head-injured child.) Intubation in these patients was specifically performed for the concerns of acute traumatic brain injury—the indications include low GCS, inability to maintain airway, or suspected raised ICP. Specifically, for monitoring of intracranial pressure (ICP), our centre largely follows international guidelines.17 For children who died, we looked at the number of days after the head injury. We reviewed the specific neurosurgical intervention. For children who were admitted, we looked at the length of hospital stay.
Analytical plan
Categorical variables were represented in frequencies and percentages. Normality was assumed for continuous variables, which were represented with mean and SD. χ2 tests were performed for categorical variables and an independent sample t-test was performed for continuous variables. Univariable logistic regression was performed to obtain the OR (and 95% CIs) for severe outcomes as defined by death, intubation and the need for neurosurgical intervention. Specifically, we stratified the analysis to study children aged less than 2 years. We subsequently performed a multivariable logistic regression, adjusting for age and location of injury. Statistical significance was established at a p value of <0.05. All statistical tests were performed using SPSS V.19 (SPSS Inc, Chicago, Illinois, USA). We did not apply imputation or statistical models on missing values.
Ethics Approval was given by the SingHealth Centralised Institutional Review Board (CIRB) E, Paediatrics and mutually recognised by the National Health Group Domain Specific Review Board (DSRB).
Results
A total of 1049 children met the inclusion criteria (refer figure 1). Among these, the mean age was 6.7 years (SD 5.2) with 268 (25.5%) children aged less than 2 years. The demographics are detailed in table 1. In this particular patient population, 501 patients (47.8%) underwent a CT, of whom 260 (24.8%) had positive findings on the CT. These positive findings included focal intracranial bleeds, diffuse axonal injury (DAI) and skull fractures. Seventeen (1.6%) patients died, of whom 7 (0.7%) were pronounced dead in the EDs. Fifty-eight (5.5%) patients underwent neurosurgery. Fifty-two (5.0%) children required emergency intubation in the ED for concerns of low GCS or suspected raised ICP (table 1).
Figure 1.
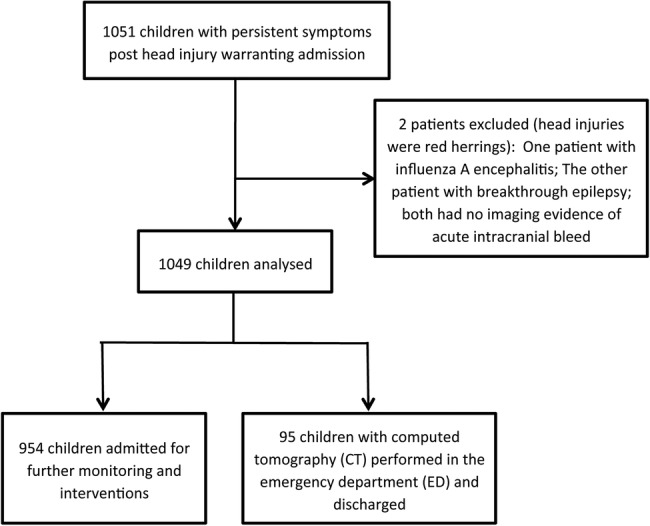
Flow diagram of patients included in the study.
Table 1.
Patient characteristics, patient demographics and clinical outcomes
| Patient age, mean (SD) | 6.7 (5.2) |
| Gender (males), n (%) | 661 (63.0) |
| CT of the brain performed, n (%) | 501 (47.8) |
| Positive finding on CT of the brain, n (%) | 260 (24.8) |
| Subdural haemorrhage (SDH) | 75 (7.1) |
| Extradural haemorrhage (EDH) | 52 (5.0) |
| Intracerebellar haemorrhage | 27 (2.6) |
| Diffuse Axonal Injury (DAI) | 26 (2.5) |
| Subarachnoid haemorrhage (SAH) | 24 (2.3) |
| Brainstem/uncal herniation | 5 (0.5) |
| Pneumocephalus | 4 (0.4) |
| Skull fracture | 176 (16.8) |
| Emergency department (ED) disposition | |
| Intensive care unit | 75 (7.1) |
| High dependency unit | 68 (6.5) |
| General ward | 807 (76.9) |
| Morgue | 7 (0.7) |
| Hospital length of stay | |
| Less than 24 h | 644 (61.4) |
| 24–48 h | 196 (18.7) |
| 48–72 h | 61 (5.8) |
| More than 72 h | 148 (14.1) |
| Death, n (%) | 17 (1.6) |
| Emergency intubation, n (%) | 52 (5.0) |
| Neurosurgical intervention, n (%) | 58 (5.5) |
| Type of neurosurgical intervention, n (%) | |
| Monitoring of intracranial pressure | 47 (4.5) |
| Evacuation of intracranial bleed | 8 (0.8) |
| Elevation of skull fracture | 6 (0.6) |
We did not have any missing information on the intent or causes of injuries. Falls remain the most common cause of head injuries (753, or 71.8%) (table 2). Among the falls specifically, 393 (52.2%) occurred in the home. This was especially prominent among children aged less than 2 years, of whom 227 (84.7%) had injuries attributed to falls and 182 (67.9%) occurred at home. The common objects included furniture (eg, adult bed) and ground surface. With every metre increase in the height of the fall, the likelihood of sustaining a severe outcome was 1.4 times (95% CI 1.3 to 1.6). This was consistent across the individual severe outcomes of death (OR 1.5, 95% CI 1.3 to 1.7) and need for intubation (OR 1.5, 95% CI 1.3 to 1.7).
Table 2.
Causes involved in injury
| All patients (n=1049) | Children <2 years (n=268) | |
|---|---|---|
| Primary cause of injury, n (%) | ||
| Fall | 753 (71.8) | 227 (84.7) |
| Motor vehicle crash | 123 (11.7) | 10 (3.7) |
| Sports | 64 (6.1) | 0 (0.0) |
| Interpersonal violence | 24 (2.3) | 0 (0.0) |
| Non-accidental trauma | 17 (1.6) | 7 (2.6) |
| Others | 68 (6.5) | 24 (9.0) |
| If fall, height (m), mean (SD) | 0.7 (2.0) | 0.6 (1.0) |
| If Motor vehicle crash | ||
| Pedestrian | 67 (54.5) | 0 (0.0) |
| Cyclist | 20 (16.3) | 0 (0.0) |
| Motor vehicle front passenger | 9 (7.3) | 3 (30.0) |
| Motor vehicle back passenger | 24 (19.5) | 7 (70.0) |
| Motorbike rider/pillion | 3 (2.4) | 0 (0.0) |
| Location of injury | ||
| Home | 430 (41.0) | 199 (74.3) |
| School/childcare centres | 139 (13.3) | 3 (1.1) |
| Public places | 141 (13.4) | 21 (7.8) |
| Roadways | 137 (13.1) | 9 (3.4) |
One hundred and twenty-three (11.7%) children suffered a head injury as a result of a motor vehicle crash. Among these, 67 (54.5%) were pedestrians, 24 (19.5%) were motor vehicle back passengers and 20 (16.3%) were cyclists. In this population, there was no statistically significant risk of severe outcomes among the pedestrians when compared to motor vehicle back passengers (OR 1.3, 95% CI 0.5 to 3.7). We did note, however, that among 56 road users (cyclists or occupants of motor vehicles), 42 or 75% of the children were not using helmets or restraints (infant capsules, car booster seats or seat belts). Three patients did not have complete records on the use of restraints.
Among the 17 children subject to NAT, the mean age was 6.2 years (SD 6.4). Four had a subdural haemorrhage (SDH), one had DAI, one had an extradural haemorrhage and one child had an isolated skull fracture. Four patients suffered a severe outcome (2 children died) and 11 patients required a hospital stay of more than 72 h.
Among the 17 deaths, the mean age was 4.9 years (SD 5.9) with the mean number of days between injury and death being 5.9 days (SD 11.6). Among these, eight patients died within 24 h of arrival in the ED.
Table 3 shows the univariable logistic regression on cause of injury associated with severe outcome. Compared to falls, motor vehicle crashes (OR 7.2, 95% CI 4.3 to 12.0) and NAT (OR 5.8, 95% CI 1.8 to 18.6) were more likely to result in death, need for airway or neurosurgical intervention. This remained statistically significant when we stratified the analysis to patients aged under 2 years. We performed a multivariable logistic regression comprising age, cause of injury and location of injury. The above two causes, as well as an injury occurring outside the home, remained statistically significant for poor outcome (table 4).
Table 3.
Univariable logistic regression for cause of injury predicting for severe outcome
| Cause of injury | OR | 95% CI | p Value |
|---|---|---|---|
| Motor vehicle crash | 7.2 | 4.3 to 12.0 | <0.001 |
| Sports | 0.6 | 0.1 to 2.6 | 0.498 |
| Non accidental trauma | 5.8 | 1.8 to 18.6 | 0.003 |
| Others | 1.5 | 0.6 to 3.9 | 0.417 |
| For children aged <2 years | |||
| Motor vehicle crash | 31.4 | 7.3 to 134.0 | <0.001 |
| Non accidental trauma | 12.6 | 2.1 to 76.4 | 0.006 |
| Others | 4.5 | 1.1 to 18.7 | 0.039 |
Taking fall as the reference for cause of injury.
Table 4.
Multivariable logistic regression for age, cause of injury and location
| Adjusted OR | 95% CI | p Value | |
|---|---|---|---|
| Cause of injury | |||
| Motor vehicle crash | 6.0 | 3.3 to 10.6 | <0.001 |
| Sports | 0.6 | 0.1 to 2.5 | 0.461 |
| Non accidental trauma | 6.7 | 2.0 to 21.2 | 0.002 |
| Others | 1.3 | 0.5 to 3.4 | 0.626 |
| Age | 1.0 | 0.9 to 1.0 | 0.057 |
| Injury outside the home | 2.4 | 1.3 to 4.7 | 0.007 |
Statistically significant results are highlighted in bold, after adjustment for age and location of injury.
Discussion
Our study showed that motor vehicle crashes and NAT are associated with severe head injury outcomes. This association remained statistically significant after adjusting for age and the location of the injury. This should assist the ED physician in risk stratification when facing children with head injuries from various causes, alerting the need for early intervention and closer monitoring. Also, this allows for careful prioritisation of injury prevention strategies.
In this study, we focused on head injuries. Even though various causes of injuries can result in different anatomical injuries, paediatric head injuries are particularly important because of the following: (1) paediatric patients have a relatively larger head and are prone to head injuries, especially among the younger age groups; (2) children are at a stage of rapid brain growth and neurocognitive development; therefore, they are especially sensitive to brain injuries, and (3) TBIs result in death, as well as in lifelong physical, emotional, financial and social sequelae on the patient, caregivers, family and society.
The causes of injuries among this patient population in Singapore are largely consistent with prior reports.16 While falls are common, road traffic accidents tend to be associated with larger forces and more severe injuries. Our study showed that this effect was evident regardless of age or location of injury. In Singapore, it is mandatory for children riding bicycles on roadways to don helmets. It is also mandatory for children in motor vehicles to be appropriately restrained.18 In this population of head-injured children presenting to the ED, compliance with road safety laws is still found wanting. Similarly, this was recently reported in the USA where only about half of the children with motor vehicle crash fatalities wore any child restraints.19 Child safety programmes initiated at the ED20 have been reported and should be explored. Pedestrians, on the other hand, are known to be at high risk of severe injuries compared to other motorway users—this is especially applicable to older children who may not be supervised when crossing the roads.
In our patient population, the presence of abuse portended a more severe outcome and a longer hospital stay. NAT in our country is diagnosed and managed along international standards.21 These are confirmed at case conference, civil, family or criminal court proceedings, or by stated criteria, including multidisciplinary assessment.21 Since they are associated with worse outcomes, they must therefore be promptly recognised by all first-line physicians who must also rapidly activate social help services and the corresponding law enforcement agencies.
We chose to study those aged less than 2 years separately. This special group of young children is especially vulnerable to head injuries, the interventions (eg, radiation from CT) imposed on them,22 and has non-specific complaints. Although young children tend to have closer supervision in public areas, they are most prone to injuries in the home, as evident in our results. Falls from adult beds, sofas and other furniture can result in TBIs in this group. Child injury prevention strategies must therefore take an age-targeted approach. Although falls in the home were less likely to be associated with severe outcome, a greater awareness of the dangers at home would reduce the overall number of head injuries.
Of note, the CT rate in this study was particularly high (47.8%) because we had chosen to exclude children subject to lower forces of injuries, minor contusions and those whose symptoms had resolved spontaneously while monitoring in the ED. We had previously reported that our CT rate (for overall paediatric head injuries) in one institution was closer to 1%.23
We recognise the limitations of this study. First, this study combined data between two tertiary institutions’ trauma surveillance systems—there may have been differences in the details of documentation, especially surrounding the object involved in the injury and the location. Second, the numbers of injuries secondary to road traffic accidents were relatively low in our population—this itself could be a result of legislature and increasing awareness, meaning that children who were appropriately restrained may have been protected from injuries, in the first place. Third, we recognise that studying only head-injured children and their corresponding causes may result in certain differences from all-encompassing injury surveillance. We believe, however, that this group warrants special attention and necessary action to reduce overall childhood mortality and morbidity. Finally, we were unable to obtain complete long-term follow-up data in this study population, which would have added value to the outcome assessment.
Childhood injuries are still an ever-growing problem in many parts of the world.24 In this study, motor vehicle crashes and NAT causes are particularly associated with poor outcomes among children with paediatric head injury. We look forward to extending this work to other centres in the Asian region, in the hope that a common platform for childhood injury surveillance will meet the current needs for robust surveillance, sharing of injury prevention strategies and evaluation of programmes.
Acknowledgments
The authors would like to thank Ms Dianna Sri and Ms Lau Yew Ping for their contribution to the head injury surveillance work in KK Women's and Children's Hospital (KKH).
Footnotes
Contributors: S-LC, SYC, JXYF, STC, NL and MEHO contributed to the conception and design of the study, analysis and interpretation of data. S-LC, SYC, JXYF, PYLT and STC were directly involved in data acquisition. All authors were involved in the drafting of the article and its critical revision for important intellectual content; they have read and approved the final manuscript.
Funding: The head injury surveillance work in KK Women's and Children's Hospital is funded by the SingHealth DUKE-NUS Paediatrics Academic Clinical Programme.
Competing interests: None declared.
Ethics approval: SingHealth Centralised Institutional Review Board (CIRB) E, Paediatrics and National Health Group Domain Specific Review Board (DSRB).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Korley FK, Kelen GD, Jones CM et al. Emergency department evaluation of traumatic brain injury in the United States, 2009–2010. J Head Trauma Rehabil 2015. Published Online First: 10 Sep 2015 10.1097/HTR.0000000000000187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston BD, Ebel BE. Child injury control: trends, themes, and controversies. Acad Pediatr 2013;13:499–507. 10.1016/j.acap.2013.04.016 [DOI] [PubMed] [Google Scholar]
- 3.Bray L. Parents’ experiences of hope following a child's brain injury. Nurs Child Young People 2015;27:22–6. [DOI] [PubMed] [Google Scholar]
- 4.Ransom DM, Vaughan CG, Pratson L et al. Academic effects of concussion in children and adolescents. Pediatrics 2015;135:1043–50. 10.1542/peds.2014-3434 [DOI] [PubMed] [Google Scholar]
- 5.Brown EA, Kenardy J, Chandler B et al. Parent-reported health-related quality of life in children with traumatic brain injury: a prospective study. J Pediatr Psychol 2016;41: 244–55. 10.1093/jpepsy/jsv090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levin HS, Diaz-Arrastia RR. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol 2015;14:506–17. 10.1016/S1474-4422(15)00002-2 [DOI] [PubMed] [Google Scholar]
- 7.Quayle KS, Powell EC, Mahajan P et al. Epidemiology of blunt head trauma in children in U.S. emergency departments. N Engl J Med 2014;371:1945–7. 10.1056/NEJMc1407902 [DOI] [PubMed] [Google Scholar]
- 8.Daniels DJ, Clarke MJ, Puffer R et al. High occurrence of head and spine injuries in the pediatric population following motocross accidents. J Neurosurg Pediatr 2015;15:261–5. 10.3171/2014.9.PEDS14149 [DOI] [PubMed] [Google Scholar]
- 9.Nnadi MO, Bankole OB, Fente BG. Motorcycle-related traumatic brain injuries: helmet use and treatment outcome. Neurosci J 2015;2015:696787 10.1155/2015/696787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Befeler AR, Daniels DJ, Helms SA et al. Head injuries following television-related accidents in the pediatric population. J Neurosurg Pediatr 2014;14:414–7. 10.3171/2014.7.PEDS1433 [DOI] [PubMed] [Google Scholar]
- 11.Cusimano MD, Parker N. Toppled television sets and head injuries in the pediatric population: a framework for prevention. J Neurosurg Pediatr 2016;17:3–12. 10.3171/2015.2.PEDS14472 [DOI] [PubMed] [Google Scholar]
- 12.Cusimano MD, Cho N, Amin K et al. Mechanisms of team-sport-related brain injuries in children 5 to 19 years old: opportunities for prevention. PLoS ONE 2013;8:e58868 10.1371/journal.pone.0058868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hinds T, Shalaby-Rana E, Jackson AM et al. Aspects of abuse: abusive head trauma. Curr Probl Pediatr Adolesc Health Care 2015;45:71–9. 10.1016/j.cppeds.2015.02.002 [DOI] [PubMed] [Google Scholar]
- 14.Ward A, Iocono JA, Brown S et al. Non-accidental trauma injury patterns and outcomes: a single institutional experience. Am Surg 2015;81:835–8. [PubMed] [Google Scholar]
- 15.Chong SL, Liu N, Barbier S et al. Predictive modeling in pediatric traumatic brain injury using machine learning. BMC Med Res Methodol 2015;15:22 10.1186/s12874-015-0015-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chong SL, Barbier S, Liu N et al. Predictors for moderate to severe paediatric head injury derived from a surveillance registry in the emergency department. Injury 2015;46:1270–4. 10.1016/j.injury.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 17.Kochanek PM, Carney N, Adelson PD et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents--second edition. Pediatr Crit Care Med 2012;13(Suppl 1):S1–82. 10.1097/PCC.0b013e31823f435c [DOI] [PubMed] [Google Scholar]
- 18.http://statutes.agc.gov.sg/aol/search/display/view.w3p;ident=a098480b-5fbe-4841-b679-e397ebe31335;page=0;query=DocId%3A%22ba3acbce-2ce4-4b3f-8011-5bfae19cfbbc%22%20Status%3Apublished%20Depth%3A0;rec=0#pr74-he-. (accessed 30 Oct 2015).
- 19.Lee LK, Farrell CA, Mannix R. Restraint use in motor vehicle crash fatalities in children 0 year to 9 years old. J Trauma Acute Care Surg 2015;79(Suppl 1):S55–60. 10.1097/TA.0000000000000673 [DOI] [PubMed] [Google Scholar]
- 20.Kiley K, Damian F, MacClaren W et al. A computerized child passenger safety screening program in the emergency department. Pediatr Emerg Care 2014;30:631–5. 10.1097/PEC.0000000000000210 [DOI] [PubMed] [Google Scholar]
- 21.Maguire SA, Kemp AM, Lumb RC et al. Estimating the probability of abusive head trauma: a pooled analysis. Pediatrics 2011;128:e550–64. 10.1542/peds.2010-2949 [DOI] [PubMed] [Google Scholar]
- 22.Kuppermann N, Holmes JF, Dayan PS et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009;374:1160–70. 10.1016/S0140-6736(09)61558-0 [DOI] [PubMed] [Google Scholar]
- 23.Thiam DW, Yap SH, Chong SL. Clinical decision rules for paediatric minor head injury: are CT scans a necessary evil? Ann Acad Med Singap 2015;44:335–41. [PubMed] [Google Scholar]
- 24.Peden M, Oyegbite K, Ozanne-Smith J et al. World report on child injury prevention. World Health Organization 2008. [PubMed]


