Description
An 86-year-old man was evaluated for chronic cough and right lower lobe (RLL) mass. His medical history was significant for severe chronic obstructive lung disease (COPD). He had smoked one pack of cigarettes daily for 55 years. He had a barrel-shaped chest and diminished breath sounds in bilateral lungs were heard. CT of the chest noted RLL mass and abnormal configuration of the trachea (figure 1). Bronchoscopic examination showed an enlarged non-collapsible horseshoe-shaped trachea (figure 2). Endobronchial ultrasound with fine-needle aspiration of the left paratracheal lymph nodes revealed squamous cell carcinoma. A diagnosis of stage IIIb lung cancer was established. The patient was referred to the oncology department, for further management.
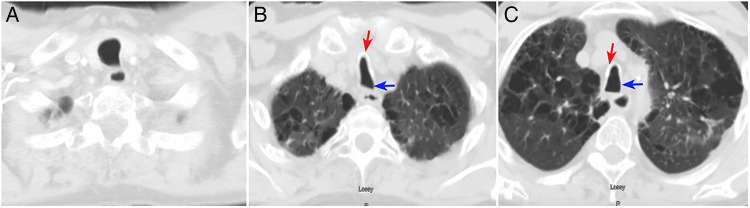
Figure 1.
Axial CT of the chest demonstrates a normal C-shaped extrathoracic trachea (A). Different slice of chest CT from the same patient shows a saber-sheath intrathoracic trachea ((B) and (C), blue arrow) and calcified tracheal cartilage due to a chronic remodelling process ((B) and (C), red arrow). This condition is also known as a horseshoe-shaped trachea.
Figure 2.
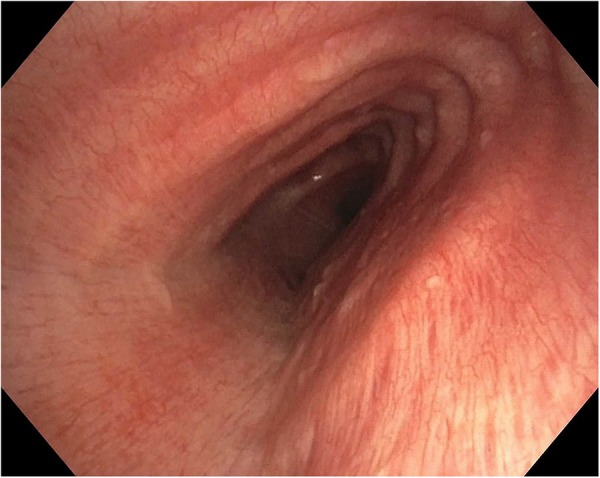
Bronchoscopic examination demonstrates a saber-sheath trachea. Elevated intrathoracic pressure indirectly promotes mechanical microinjury to the non-cartilaginous part of the trachea, subsequently leading to chronic remodelling of the tracheal cartilage.
We demonstrate radiographic and bronchoscopic features of saber-sheath trachea in a patient with severe COPD and concurrent primary lung cancer. Intrathoracic coronal narrowing and sagittal widening of the trachea characterise saber-sheath trachea, which is commonly associated with severe obstructive lung diseases, for example, chronic bronchitis, emphysema, hyperinflation and bronchiolitis obliterans syndrome after lung transplantation.1 A tracheal index (the ratio between coronal and sagittal diameter of the trachea at the same level) of less than two-thirds has 92.9% specificity, but 39.1% sensitivity, to diagnose severe cases of COPD.2 The pathophysiological mechanisms of saber-sheath trachea are due to repetitive cartilaginous injury from excessive coughing, and elevated intrathoracic pressure. These mechanisms cause degeneration and ossification of the cartilage leading to chronic remodelling, calcification and bending of the tracheal cartilage.3 Cases of air leaking during endotracheal intubation were reported because the circular-shaped balloon could not approximate the sagittal elongation of the stiff tracheal wall.3 Laryngeal mask airway is an alternative option to maintain adequate mechanical ventilation. It is important for physicians to recognise this clinical entity for a proper diagnosis. There is no specific treatment for saber-sheath trachea.
Learning points.
A saber-sheath trachea is characterised by a normal C-shaped extrathoracic trachea with abrupt coronal narrowing and sagittal widening of the intrathoracic trachea. This condition is commonly associated with severe obstructive lung diseases, for example, chronic bronchitis, emphysema, hyperinflation and bronchiolitis obliterans syndrome after lung transplantation.
The pathophysiological mechanisms of saber-sheath trachea are due to repetitive cartilaginous injury from excessive coughing, and elevated intrathoracic pressure. These mechanisms cause degeneration and ossification of the cartilage leading to chronic remodelling, calcification and bending of the tracheal cartilage to form a rigid non-collapsible trachea.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hayes D Jr, Ballard HO. Saber-sheath trachea in a patient with bronchiolitis obliterans syndrome after lung transplantation. Chron Respir Dis 2009;6:49–52. doi:10.1177/1479972308099990 [DOI] [PubMed] [Google Scholar]
- 2.Tsao TC, Shieh WB. Intrathoracic tracheal dimensions and shape changes in chronic obstructive pulmonary disease. J Formos Med Assoc 1994;93:30–4. [PubMed] [Google Scholar]
- 3.Ismail SA, Mehta AC. “Saber-sheath” trachea. J Bronchol Intervent Pulmonol 2003;10:296–7. [Google Scholar]