Abstract
Cavernous haemangiomas are the most common tumour of the liver; they are benign in nature and have an incidence of up to 7.3% at autopsy. Occasionally, they may cause symptoms necessitating intervention. We report the case of a woman who presented with non-specific abdominal pain and evidence of a giant hepatic haemangioma on abdominal imaging. She underwent selective hepatic arteriography with transcatheter arterial embolisation followed by same-day left hemi-hepatectomy, making an uneventful recovery. We discuss the management of giant hepatic haemangiomas and present same day transcatheter arterial embolisation prior to hepatic resection as a safe and viable treatment strategy in selected cases.
Background
Cavernous haemangiomas are the most common benign liver tumours, representing 73% of all benign hepatic lesions, and have an incidence of 0.4–7.3% at autopsy.1 Haemangiomas are mesoderm-derived tumours consisting of cavernous vascular spaces lined by dysfunctional endothelial cell layers, separated by fibrous septae.2 The pathogenesis of cavernous haemangiomas is not well elucidated. However, a higher incidence in females and preponderance to enlargement during pregnancy suggest female sex hormones may be a contributing factor. Indications for surgical resection include accidental haemorrhage and abdominal discomfort. Although uncommon, patients can also present with obstructive jaundice and gastric outlet obstruction due to the mass effect of large tumours, and these are indications to consider surgery. Other indications for intervention include Kasabach-Merritt syndrome (consumptive thrombocytopaenia), haemorrhage and/or diagnostic uncertainty.3
Most hepatic haemangiomas are small and require no further intervention. Giant cavernous haemangiomas (>4 cm) are more likely to be symptomatic, with patients typically presenting with abdominal pain and/or fullness,1 as was present in this case. While surgical resection remains the definitive curative treatment, other treatments exist for unresectable lesions in the form of liver transplantation, transcatheter arterial embolisation (TAE), arterial ligation and chemotherapy.1
Case presentation
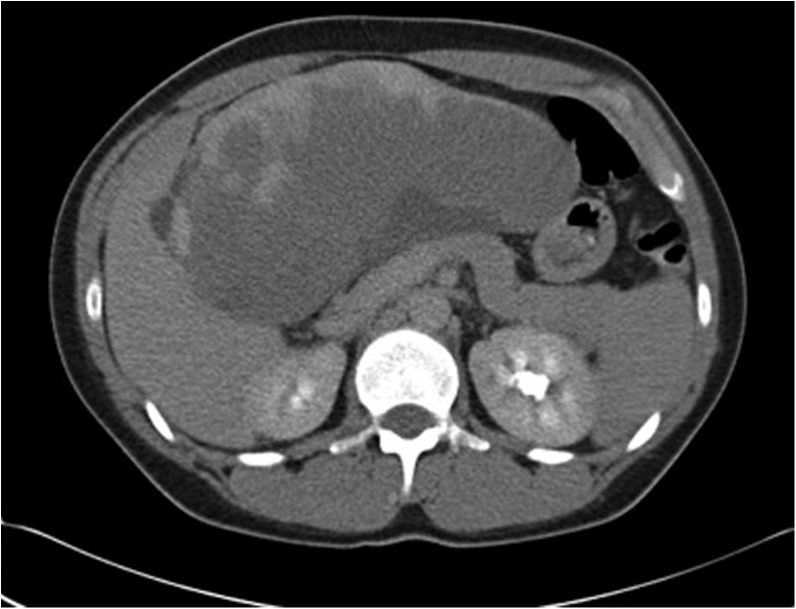
A 33-year-old Caucasian woman, with no significant medical history and no relevant social history, presented as an emergency with non-specific abdominal pain ongoing for 2 months. Clinical examination revealed a palpable epigastric mass and laboratory analyses were all within normal limits. Abdominal ultrasound showed a large hepatic mass. Contrast-enhanced CT undertaken at the time of referral revealed a 17×15 cm mass associated with the left lobe of the liver (figure 1). MRI further characterised the lesion, clearly demonstrating peripheral enhancement in the arterial phase with gradual central filling, confirming the diagnosis of a hypervascular giant cavernous haemangioma (figure 2). Owing to the size of the tumour and ongoing symptomatology, the case was discussed at the multidisciplinary team (MDT) meeting. After reviewing literature confirming TAE as a recognised technique for benign hypervascular liver lesions,1–5 the patient was offered hepatic resection. With input from the interventional radiology team it was felt that TAE could target the main vessel supplying the tumour, facilitating hepatic resection. TAE was performed with Contour 500–710 µm polyvinyl alcohol particles and Tornado platinum micro coils, with no complication on the morning of surgery. Following embolisation, the patient was transferred to theatre and underwent laparotomy. A large mass was identified in the left lobe of the liver, and a left hemihepatectomy was performed (figure 3). Following surgery, the patient made an uneventful recovery and was clinically well at 6-week follow-up. Histopathological analysis showed the mass to be 21×14×5 cm in size, with sections of the mass demonstrating vascular channels separated by fibrous tissue filled with erythrocytes with no evidence of malignancy. These features were consistent with a giant haemangioma. In addition, four other microhaemangiomas were identified and the surrounding liver tissue showed changes of mild, chronic inflammation and congestion.
Figure 1.
CT showing a large liver mass in the left lobe of the liver.
Figure 2.
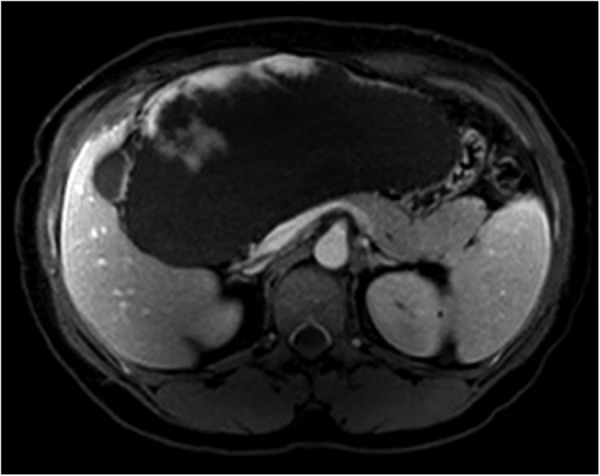
MRI of the liver demonstrating a large haemangioma in the left lobe of the liver.
Figure 3.

Liver specimen with a shrunken haemangioma in the left lobe, following embolisation.
Investigations
Abdominal USS, CT scan (figure 1) and MRI scan (figure 2) were carried out.
Treatment
Same day selective hepatic arteriography was performed with TAE and surgical hemihepatectomy.
Outcome and follow-up
The patient made an uneventful recovery from the operation and had resumed normal activity when reviewed at 6-week follow-up appointment.
Discussion
Over the last decade, the morbidity and mortality from major liver surgery has improved significantly and, hence, patients with symptomatic, large haemangiomas can be safely considered for major liver resection. Nevertheless, certain variables such as tumour size and position can present technical difficulties in resection, as well as exposing the patient to potential ischaemia-reperfusion injury if inflow vascular occlusion is required. Recent reports have suggested TAE as a treatment for giant haemangiomas.3 Although TAE may bring about tumour shrinkage and resolution of symptoms, these results are not consistent in all patients; this may be due to vascular recanalisation.2 Srivastava et al3 reported success with TAE as a definitive therapy in seven out of eight patients with giant hepatic haemangioma, although one patient required subsequent surgery after TAE brought about only partial resolution of symptoms. In this case, due to the size of the tumour and patient's wish for definitive treatment, coupled with MDT discussion, TAE was performed prior to surgery rather than as a single therapy. There are conflicting opinions with regard to the interval between performing the TAE and hepatic resection. Some clinicians have suggested performing the TAE and re-evaluation with interval imaging to ensure there has been appropriate volume reduction of the haemangioma prior to considering hepatic resection for this benign condition.5 However, the groups of Vassiou et al2 and Seo et al4 suggested that delaying the liver resection exposes the patients to the long-term sequelae of TAE, which include: risks of post-TAE pain; migration of the embolisation agent; and possible inoperability.2 4 Recently, Zhou et al5 reported a case of intestinal obstruction secondary to inflammatory adhesions 1 month following TAE. In the present case, TAE was performed on the morning of surgery as it was thought that performing this procedure any earlier could lead to an inflammatory response in the portal triad, which could make the dissection around these structures more difficult. In addition, performing a TAE earlier also has a theoretical risk of causing a systemic inflammatory response syndrome. In this case, the TAE on the day of surgery shrank the haemangioma and facilitated the resection and probably decreased the blood loss during the transection phase, as previously reported by other authors.2 4
Patient's perspective.
Symptom onset: It came on so suddenly. I woke up with back pain that just would not settle. It did not improve with painkillers and that night I had to go to A and E.
Diagnosis: They told me that it was a tumour the night I went to the hospital, and told me I would need to go to Nottingham to see one of the liver surgeons there.
Referral: My appointment at Queen's Medical Centre was made nearly 6 weeks after I first went to hospital, which was difficult, not knowing what was going on.
Decision to embolise: I spoke to the surgeon shortly before the operation and he told me that he would like to embolise the tumour just before the operation. I understand this was to shrink the tumour to make the operation easier.
Recovery: There was not any pain during or after the embolisation, and after the operation I had an epidural. I spent 6 days in hospital in total.
Health now: I would describe myself as symptom-free.
Learning points.
Although rare, giant haemangioma can present with non-specific abdominal pain in otherwise healthy young patients.
Transcatheter arterial embolisation (TAE) should be considered prior to surgical resection of giant haemangioma.
Same day arterial embolisation and surgical resection was safely carried out in this patient with the expert consensus being that prior TAE aided the successful outcome.
Footnotes
Contributors: DG was the responsible consultant and operating surgeon along with SDC. All the authors were involved in elements of writing, and editing and submitting of this case.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Toro A, Mahfouz AE, Ardiri A et al. What is changing in indications and treatment of hepatic hemangiomas. A review. Ann Hepatol 2014;13:327–39. [PubMed] [Google Scholar]
- 2.Vassiou K, Rountas H, Liakou P et al. Embolization of a giant hepatic hemangioma prior to urgent liver resection. case report and review of the literature. Cardiovasc Intervent Radiol 2007;30:800–2. [DOI] [PubMed] [Google Scholar]
- 3.Srivastava DN, Gandhi D, Seith A et al. Transcatheter arterial embolization in the treatment of symptomatic cavernous hemangiomas of the liver: a prospective study. Abdom Imaging 2001;26:510–14. 10.1007/s00261-001-0007-x [DOI] [PubMed] [Google Scholar]
- 4.Seo HI, Jo HJ, Sim MS et al. Right trisegmentectomy with thoracoabdominal approach after transarterial embolization for giant hepatic hemangioma. World J Gastroenterol 2009;15:3437–9. 10.3748/wjg.15.3437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou JX, Huang JW, Wu H et al. Successful liver resection in a giant hemangioma with intestinal obstruction after embolization. World J Gastroenterol 2013;19:2974–8. 10.3748/wjg.v19.i19.2974 [DOI] [PMC free article] [PubMed] [Google Scholar]