Abstract
A 56-year-old man was admitted to hospital with shortness of breath and subsequently sustained a cardiac arrest. In the recovery period, he developed acute urinary retention and haematuria. Imaging suggested an enlarged prostate and he was started on clean intermittent catheterisation. Following further imaging and a transurethral biopsy, he was found to have a bladder leiomyoma. This was treated with laparotomy, cystotomy and enucleation of the tumour. At his 6-week follow-up appointment, he had a satisfactory cystogram and a successful void without catheter.
Background
This case is important as it serves as a reminder that it is always important to thoroughly investigate a patient prior to any surgery. Bladder outflow obstruction surgery, which was initially recommended for this patient, would not have been appropriate.
Case presentation
A 56-year-old man presented to his local accident and emergency department, with shortness of breath and ankle swelling. He had no pre-existent medical history aside from diet-controlled diabetes. He sustained a cardiac event, complicated by a pulseless electrical activity cardiac arrest secondary to pulmonary oedema. He spent 3 weeks in the intensive care unit following which he was stabilised from a medical perspective. He was subsequently treated with anticoagulation therapy for a pulmonary embolism, but this was ceased due to marked visible haematuria requiring a 7-unit blood transfusion.
Prior to admission, the patient had reported voiding lower urinary tract symptoms characterised by hesitancy and urinary frequency. During his hospital stay, he developed urinary retention and was taught clean intermittent self catheterisation (CISC), with no spontaneous voiding. Imaging at that time identified a large pelvic mass thought to be consistent with the prostate gland; transrectal prostate biopsies were benign. He was referred to another unit for consideration of bladder outflow obstruction surgery, but was lost to follow-up. He later represented with visible haematuria and underwent a cystoscopy, bladder washout and anterior bladder wall biopsies. The histology confirmed a bladder leiomyoma so he was referred to a tertiary centre for further management of his bladder tumour.
Investigations
On examination, the patient had a palpable pelvic mass, with an otherwise unremarkable genital examination and a benign feeling prostate on digital rectal examination. Imaging was invaluable in this case, and a repeat CT of his abdomen and pelvis together with MRI of his pelvis (figure 1A, B) revealed a soft tissue mass within the pelvis, with a maximum transverse diameter measuring 9.1 cm. A full blood count was within normal limits, but the patient had some renal impairment with a creatinine of 173 (normal range: 59–104 μmol/L), corresponding to an estimated glomerular filtration rate of 35 mL/min. His prostate specific antigen was within the normal age-specific range. A urine sample collected following CISC demonstrated a raised white cell count with a heavy growth of Escherichia coli, which was treated with an oral course of antibiotics.
Figure 1.

(A) CT showing a coronal view of the pelvic mass. (B) T2-weighted MRI showing an axial view of the pelvic mass.
Differential diagnosis
Bladder cancer, benign prostatic enlargement.
Treatment
An examination under general anaesthetic was performed, which revealed a large pelvic mass on bimanual examination. A rigid cystoscopy under general anaesthetic identified a normal urethra and large bladder mass extending from bladder neck to the trigone, with normal urothelium overlying the tumour. The intention was to insert bilateral ureteric stents, however, the ureteric orifices were not visualised as they were obscured by the bladder tumour.
A laparotomy and open cystotomy were performed (figure 2). The tumour was identified and, using a combination of sharp and blunt dissection, a plane was created allowing enucleation of the bladder tumour (figure 3). Bilateral ureteric stents were inserted and a suprapubic catheter was left as well as an irrigating catheter urethrally. The bladder was closed in two layers with 2.0 vicryl and a pelvic drain was left in-situ.
Figure 2.
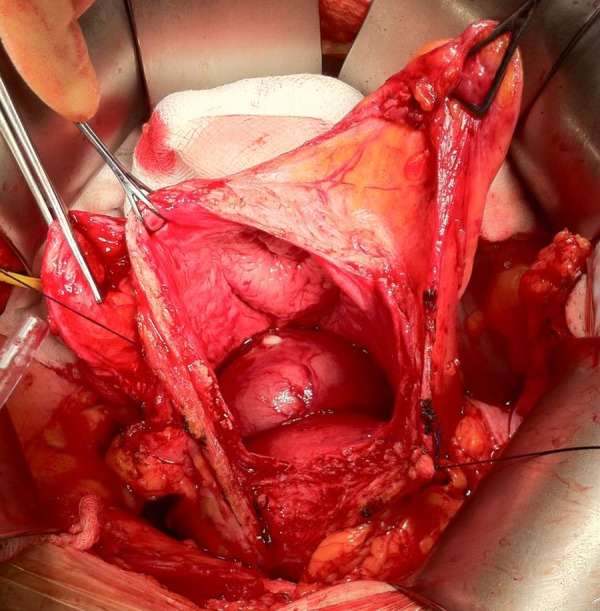
Bladder opened at operation to reveal large leiomyoma.
Figure 3.

Bladder leiomyoma enucleated intact.
Outcome and follow-up
The patient's pelvic drain was left for 24 h postoperatively. The irrigating urethral catheter was removed on postoperative day 4 and the patient was discharged on day 6. The ureteric stents were subsequently removed 6 weeks later under flexible cystoscopic guidance with no complication; a follow-up cystogram performed 6 weeks postoperatively demonstrated no leaks. The patient's suprapubic catheter was removed following successful voiding with an insignificant post void residual. The histology confirmed a leiomyoma of the bladder.
Discussion
Most bladder tumours are malignant and less than 1% of presenting tumours are benign. Leiomyomas are the commonest non-epithelial benign tumours of the bladder and are composed of smooth muscle. The exact aetiology of leiomyomas is unknown, although it is postulated that hormonal influences, perivascular inflammation, chromosomal abnormalities and localised infection may contribute to its development.1 Leiomyomas may occur in intravesical, intramural or extravesical locations; the intravesical form has been reported in 63% of cases, the intramural form in 7% and the extravesical form in 30%.2 The presenting symptoms may reflect the size and location of the tumour, ranging from asymptomatic to storage or voiding lower urinary tract symptoms in the intravesical type, as well as haematuria.
Definitive diagnosis is accomplished by typical findings on histopathological assessment: fascicles of smooth muscle fibres separated by connective tissues, non-infiltrative smooth muscle tumour lacking mitotic activity, cellular atypia and necrosis. Radiological investigations, especially with MRI, may confirm the diagnosis and avoid invasive procedures.3 In the presented case, imaging modalities were unable to give an exact diagnosis, and transrectal prostate biopsies were equivocal. Superficial biopsies taken from surface mucosa for diagnostic purposes can lead to misleading results hence careful pathological assessment is crucial.4 Likewise, it is sometimes difficult to evaluate these bladder tumours on imaging, leading to misinterpretation and confusion with other diagnoses.5
There is a varied approach to managing leiomyomas, with surgery being the standard approach. Notably, there is no evidence in the published literature to suggest malignant transformation of these tumours, although there are case reports suggesting that they can recur.6 Hence, conservative management is an option in asymptomatic patients.7 The ideal surgical approach should be tailored to the patient so that it offers the greatest exposure and separation from adjacent structures during the procedure. In an analysis of 90 cases, a laparotomy was performed in 62.2% patients, with enucleation in 32.2%, partial cystectomy in 27.8% and a total cystectomy in 2.2% of cases. A transurethral approach was performed in 30% patients and a transvaginal approach in 5.6% of patients. Two patients were managed conservatively.
Management was successful in this patient, allowing for a successful trial of voiding 6 weeks following surgery. However, this case serves as a reminder that no imaging technique can safely exclude malignancy, and careful extensive pathological assessment is fundamental in predicting the potential prognosis and guiding the appropriate management. In this case, a laparotomy was the optimal surgical approach due to the size of the tumour, but patient management must be individualised.
Learning points.
Careful scrutiny of imaging may be helpful in suspecting a diagnosis of bladder leiomyoma.
Superficial biopsies taken from the surface mucosa of the tumour may be misleading and non-diagnostic.
Prior to the consideration of any invasive procedure, detailed history-taking and a thorough examination are essential, as well as careful review of available imaging and histopathology.
Footnotes
Contributors: OE and MSK: involved in the write-up of the case.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Erdem H, Yildirim U, Tekin A et al. Leiomyoma of the urinary bladder in asymptomatic women. Urol Ann 2012;4:172–4. 10.4103/0974-7796.102667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knoll LD, Segura JW, Scheithauer BW. Leiomyoma of the bladder. J Urol 1986;136:906–8. [DOI] [PubMed] [Google Scholar]
- 3.Fasih N, Prasad Shanbhogue AK, Macdonald DB et al. Leiomyomas beyond the uterus: unusual locations, rare manifestations. Radiographics 2008;28:1931–48. 10.1148/rg.287085095 [DOI] [PubMed] [Google Scholar]
- 4.Mammadov R, Musayev J, Hasanov A. Endovesical leiomyoma of bladder: a case report. Georgian Med News 2013;(218):7–10. [PubMed] [Google Scholar]
- 5.Wu S. Imaging findings of atypical leiomyoma of the urinary bladder simulating bladder cancer: a case report and literature review. Med Ultrason 2013;15:161–3. 10.11152/mu.2013.2066.152.sw1 [DOI] [PubMed] [Google Scholar]
- 6.Lake MH, Kossow AS, Bokinsky G. Leiomyoma of the bladder and urethra. J Urol 1981;125:742–3. [DOI] [PubMed] [Google Scholar]
- 7.Cornella JL, Larson TR, Lee RA et al. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am J Obstet Gynecol 1997;176:1278–85. 10.1016/S0002-9378(97)70346-6 [DOI] [PubMed] [Google Scholar]


