Abstract
Mesenteric cysts are rare and occur in patients of any age. They are asymptomatic and found incidentally or during the management of their complications. They commonly originate from the small bowel mesentery, although a proportion has been found to originate from the mesocolon (24%) and retroperitoneum (14.5%). A mesenteric cyst originating in the sigmoid mesocolon is a very rare finding.
Background
Mesenteric cysts are rare clinical entities. They commonly originate from the small bowel mesentery, although a proportion has been found to originate from the mesocolon (24%) and retroperitoneum (14.5%).1 They are a rare cause of abdominal pain and are discovered incidentally. If symptomatic, patients with these cysts present with abdominal pain, vomiting and low backache. Performing a thorough physical examination, and conducting radiological investigations such as ultrasonography (USG) and CT, are the key to diagnosis. A mesenteric cyst originating in the sigmoid mesocolon is a very rare finding.2–5 We report the case of a man who presented with right lower quadrant abdominal pain and low backache. USG of the abdomen and pelvis showed a hypoechoic space occupying lesion in the right flank. Contrast CT of the abdomen showed a loculated cystic lesion seen in the right iliac fossa, causing mild compression of the ileocaecal junction. Laparotomy was performed and the cyst resected along with a part of the sigmoid colon. Histopathology identified it as a benign mucinous mesenteric cyst.
Case presentation
A 47-year-old man presented with vague intermittent lower abdominal pain and low backache of 2-month duration. He had no history of abdominal distension, vomiting, diarrhoea, melena or mucoid stools. Nor had he a history of abdominal trauma. His bladder and bowel habits were normal. Vitals were stable and other systemic examinations were normal. On local examination, tenderness was present on deep palpation in the right iliac fossa. There were no abnormalities in the per-rectal examination.
Investigations
Laboratory investigations showed haemoglobin of 10.3 g/dL and erythrocyte sedimentation rate (ESR) 26 mm/1st hour. Serum glucose, liver function tests, blood urea and serum creatinine were normal.
USG of the abdomen showed a 6×5 cm hypoechoic lesion in the right flank below the right kidney, with no other abnormalities.
Coronal (figure 1) and axial (figure 2) contrast enhanced computerised tomography (CECT) sections of the abdomen showed a cystic lesion with a thin enhancing wall showing loculations and enhancing intervening thin septae measuring 6.1×5.4 cm near the ileocaecal junction, likely a lymphangioma or enteric cyst.
Figure 1.

A cystic lesion (arrow) with enhancing wall showing loculations and intervening septa, measuring 6.1×5.4 cm, near ileocaecal junction (coronal view).
Figure 2.
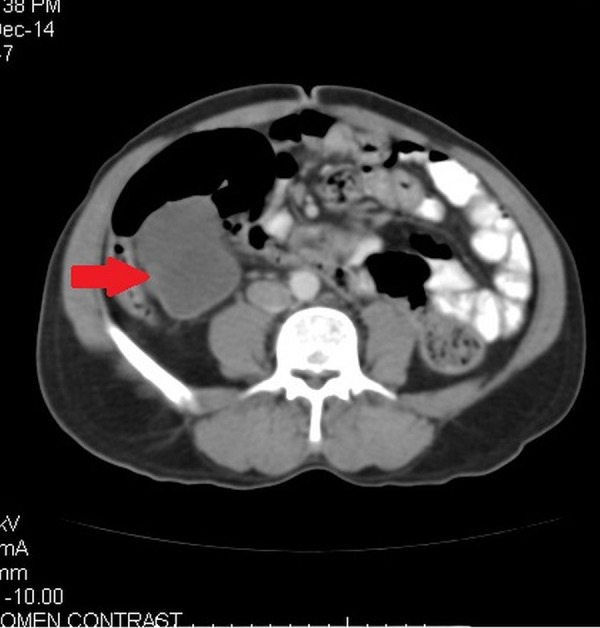
The same cystic lesion with wall enhancement near the ileocaecal region (axial view).
Differential diagnosis
Lymphangioma
Mesenteric cyst
Retroperitoneal cyst
Hydatid cyst
Treatment
After the necessary preoperative work up, laparotomy via a midline incision was performed. Intraoperatively, an 8×6 cm mass with solid and cystic components present in the sigmoid mesocolon close to its mesenteric border, sharing a common blood supply with the segment of the sigmoid colon, was seen (figures 3 and 4). The caecum was found adherent to the mesentery of the sigmoid. The small bowel mesentery and sigmoid mesentery were adherent to each other. There was no ascites and no enlarged lymph nodes in the mesentery. The liver, spleen, colon and stomach were normal. The cystic mass along with a part of the sigmoid colon and its mesentery was resected and intestinal continuity was restored with a colo-colic anastomosis. Haemostasis was achieved and the incision closed.
Figure 3.

Showing a cystic lesion in the sigmoid mesocolon.
Figure 4.
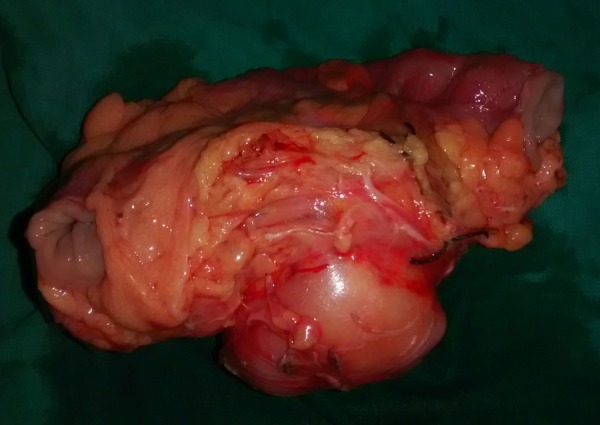
Resected specimen showing the cystic lesion (arrow) along with resected part of the sigmoid colon.
Outcome and follow-up
Post-operative recovery was uneventful; the drain was removed in 48 h and the patient was discharged on the fourth postoperative day. Histopathology evaluation revealed a benign mucinous mesenteric cyst with the wall of the cyst lined by tall columnar mucin secreting cells with a focal collection of lymphomononuclear infiltrate in the wall (figure 5). After 6 months of follow-up, the patient was doing well and postoperative CT scan was insignificant.
Figure 5.
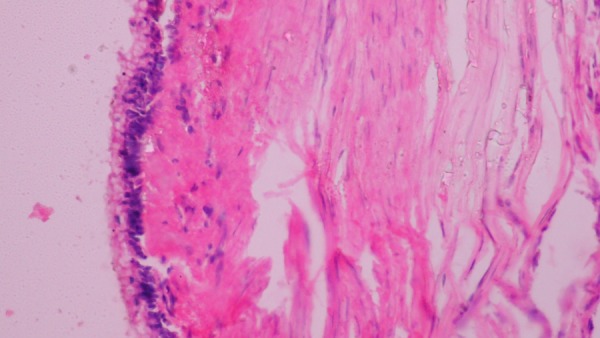
Histopathology study showing cyst wall lined with tall columnar mucin secreting cells with lymphomononuclear infiltrate.
Discussion
Mesenteric cyst is a rare cystic disease that occurs within the abdominal cavity, with a prevalence of 1/100 000 to 250 000 among adult hospitalised patients.6 This cyst is a rare cause of abdominal pain. A mesenteric cyst in the sigmoid mesocolon is even rarer. Mesenteric cysts were first described by Benevieni, a Florentine anatomist, in 1507.7 In 1880, Tillaux performed the first successful resection of a cystic tumour of the mesentery.7 The usual location of the cyst is the mesentery of the small intestine, commonly the mesentery of the ileum. Mesenteric cysts usually occur in the fifth decade, and have a female preponderance. Cystic lymphangioma is the only exception, and that occurs in the first decade of life, and has a male predominance. The aetiology of mesenteric cysts is variable. They usually arise from failure of lymph nodes to communicate with the lymphatics or venous system, or blockage of draining lymphatics as a result of trauma, neoplasm or infection.8 9
Beahrs et al,10 in 1950, classified mesenteric cyst into four categories: embryonic and developmental cysts, traumatic cysts, neoplastic cysts and infective and degenerative cysts. Later, Ros et al9 proposed a histological classification into five groups correlated with radiological findings of the cysts, namely, lymphangiomas, enteric duplication cysts, enteric cysts, mesothelial cysts and non-pancreatic pseudocysts.
Proposed updated classification of mesenteric cysts and cystic tumours11 is as follows:
Classification of mesenteric cysts:
- Cyst of lymphatic origin
- Simple lymphatic cyst
- Lymphangiomas
- Cysts of mesothelial origin
- Simple mesothelial cysts
- Benign cystic mesotheliomas
- Malignant cystic mesotheliomas
- Cysts of enteric origin
- Enteric duplication cysts
- Enteric cysts
Cysts of urogenital origin
- Non-pancreatic pseudocysts
- Cysts of traumatic origin
- Cysts of infectious origin
- Non-neoplastic cysts
- Hydatid
- Tuberculous cyst
-
Mucinous cystic neoplasms
Mucinous cystadenoma- Borderline malignant mucinous cystic neoplasm
- Mucinous cyst adenocarcinoma
Miscellaneous neoplasms
As most mesenteric cysts have no symptoms, they are frequently discovered by chance, on USG or CT, and their detection is unlikely on a physical examination or by haematological tests.6 Sometimes, they may manifest with symptoms such as diffuse abdominal pain, sensation of fullness or pressure in the abdomen, or due to other complications such as torsion, rupture, haemorrhage of cysts, herniation of bowel into abdominal defect and obstruction. Malignant transformation is rare but has been described in up to 3% of cases.1
Accurately diagnosing a mesenteric cyst depends on performing a thorough physical examination and appropriate radiological studies.9 12 13
Diagnostic laparoscopy is another modality at the surgeon’s disposal, if the location and characteristics of the lesion cannot be assessed adequately with radiological evaluation. Surgical excision is the mainstay of treatment for both, benign and malignant cysts. The surgical procedure differs according to the range of the lesion and extent of intrusion into the surrounding organs.6 Enucleation is adequate in the majority of mesenteric cysts but, sometimes, bowel resection may be necessary in cases where cysts are close to bowel structures or involving blood vessels that supply the bowel.9 Mesenteric cysts have a very low recurrence rate (0–13.6%) and patients have an excellent prognosis.14 Laparoscopic resection has a high success rate with low incidence of postoperative complications.
Although mesenteric cysts are rare and difficult to diagnose prior to surgery, attributable to absence of symptoms, in most cases, they must be considered in the differential diagnosis of a cystic lesion within the abdominal cavity.6 Although most are benign, surgical resection needs to be considered because these cysts have the possibility of malignant transformation.6
After an extensive literature research, we could find only five previously reported cases of mesenteric cysts of the sigmoid mesocolon (table 1).15
Table 1.
Reported cases of mesenteric cysts in sigmoid mesocolon
| Sl No | Author | year | Age/sex | Presentation | Management | Histopathology |
|---|---|---|---|---|---|---|
| 1. | Smith et al | 1995 | 29/F | Lump | Excision | Urogenital remnant of Müllerian type |
| 2. | Lida et al | 2003 | 31/F | Abdominal pain | Excision | pseudocyst |
| 3. | Wang et al | 2012 | 26/M | Abdominal pain | Lap excision | Duplication cyst |
| 4. | Bhandarwar et al | 2013 | 42/M | Abdominal pain | Lap excision | Lymphatic cyst |
| 5. | Kumar et al (2 cases) | 2014 | 48/F | Abdominal pain | Lap excision | Lymphatic cyst |
| 62/F | Abdominal pain | Lap excision | Lymphatic cyst | |||
| 6. | Our case | 2015 | 45/M | Abdominal pain | Resection of the cyst along with a part of the sigmoid colon | Mucinous cyst |
Learning points.
Mesenteric cysts arising from the sigmoid colon are very rare, and benign in most cases; however, they should be considered as a possibility in cases of cysts occurring in the abdominal cavity.
Patients who are symptomatic generally present with pain, abdominal distress or low backache, a palpable mass, nausea and vomiting.
Cysts are misdiagnosed as some other more common abdominal conditions.
Ultrasonography and CT are the most useful imaging modalities for diagnosing mesenteric cysts.
Complete surgical excision is the treatment of choice. Following surgery, prognosis is excellent and recurrence is low.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kurtz RJ, Heimann TM, Beck AR et al. Mesenteric and retroperitoneal cysts. Ann Surg 1986;203:109–12. 10.1097/00000658-198601000-00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith GL, Thorpe PA, Karimjee S et al. An abdominal cyst. Postgrad Med J 1995;71:637–8. 10.1136/pgmj.71.840.637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iida T, Suenaga M, Takeuchi Y et al. Mesenteric pseudocyst of the sigmoid colon. J Gastroentrol 2003;38:1081–5. 10.1007/s00535-003-1200-1 [DOI] [PubMed] [Google Scholar]
- 4.Wang JH, Lin JT, Hsu CW. Laparoscopic excision of mesenteric duplication enteric cyst embedded in sigmoid mesocolon mimicking retroperitoneal neurogenic tumor in adults. Surg Laparosc Endosc Percutan Tech 2012;22:e294–6. 10.1097/SLE.0b013e3182611d07 [DOI] [PubMed] [Google Scholar]
- 5.Bhandarwar AH, Tayade MB, Borisa AD et al. Laproscopic excision of mesenteric cyst of sigmoid mesocolon. J Minim Access Surg 2013;9:37–9. 10.4103/0972-9941.107138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park SE, Jeon TJ, Park et al. Mesenteric pseudocyst of the transverse colon: unusual presentation of more common pathology. BMJ Case Rep 2014;2014 pii: bcr2013202682 10.1136/bcr-2013-202682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dursun AS, Gokhan A, Volkan S et al. Laparoscopic enucleation of mesenteric cyst: a case report. Mt Sinai J Med 2006;73:1019–20. [PubMed] [Google Scholar]
- 8.Walker AR, Putnam TC. Omental, mesenteric and retroperitoneal cysts: a clinical study of 33 new cases. Ann Surg 1973;178:13–9. 10.1097/00000658-197307000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ros PR, Olmsted WW, Moser RP Jr et al. Mesenteric and omental cysts: histologic classification with imaging correlation. Radiology 1987;164:327–32. 10.1148/radiology.164.2.3299483 [DOI] [PubMed] [Google Scholar]
- 10.Beahrs OH, Judd ES Jr, Dockerty MB. Chylous cysts of the abdomen. Surg Clin North Am 1950;30:1081–96. [DOI] [PubMed] [Google Scholar]
- 11.Metaxas G, Tangalos A, Pappa P et al. Mucinous cystic neoplasms of the mesentery: a case report and review of literature. World J Surg Oncol 2009;7:47 10.1186/1477-7819-7-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hassan M, Dobrilovic N, Korelitz J. Large gastric mesenteric cyst: case report and literature review. Am Surg 2005;71:571–3. [PubMed] [Google Scholar]
- 13.Egozi EI, Ricketts RR. Mesenteric and omental cysts in children. Am Surg 1997;63:287–90. [PubMed] [Google Scholar]
- 14.Bliss DP Jr, Coffin CM, Bower RJ et al. Mesenteric cysts in children. Surgery 1994;115:571–7. [PubMed] [Google Scholar]
- 15.Kumar A, Jakhmola CK, Arora NC et al. Mesenteric cyst in sigmoid mesocolon—a rare location and its laproscopic excision. Med J Armed Forces India 2015;71(Suppl 2):S425–8. 10.1016/j.mjafi.2014.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]


