To the Editor
Perinatal hyperoxia in preterm infants is associated with several well-known sequelae, including bronchopulmonary dysplasia and retinopathy of prematurity. Hyperoxia also induces alterations in cardiopulmonary control (e.g., preterm infants treated with hyperoxia lack normal ventilatory responses to hypoxia and hyperoxia).1,2 It has not been determined whether these impairments diminish with age. Thus, we sought to determine whether or not ventilatory dysfunction persists in adults who were born prematurely.
We measured the ventilatory responses to 5 minutes of isocapnic, isobaric hypoxia (in which the fraction of inspired oxygen [FIO2] was 0.12) and hyperoxia (in which the Fio2 was 1.0) in 13 adults born prematurely who were recruited from the Newborn Lung Project3 (a cohort with a mean [±SD] age of 21±1 years, a gestational age of ≤32 weeks, and a gestational weight of ≤1500 g) and from age-matched adults born at full term. Preterm adults were clinically indistinguishable from full-term adults, having similar pulmonary function and exercise capacity (see the Supplementary Appendix, available with the full text of this letter at NEJM.org). However, the hypoxic ventilatory response was substantially reduced in preterm adults (0.13±0.25 liters per minute per −ΔSpO2, where −ΔSpO2 denotes a negative change in oxygen saturation as measured by pulse oximetry) as compared with full-term adults (0.42±0.30 liters per minute per −ΔSpO2; P = 0.008) (Fig. 1). Moreover, two preterm adults hypoventilated, which resulted in an increase in the partial pressure of end-tidal carbon dioxide (PETCO2). As expected, 60 seconds of hyperoxia induced respiratory depression from baseline in all full-term adults (−29.6±20.1%) but in only 8 of 13 preterm adults. The mean response was also reduced in the preterm population (−3.0±26.9%; P = 0.01).
Figure 1. Ventilatory Responses to Hypoxia and Hyperoxia in Adults Born Prematurely as Compared with Adults Born at Full Term.
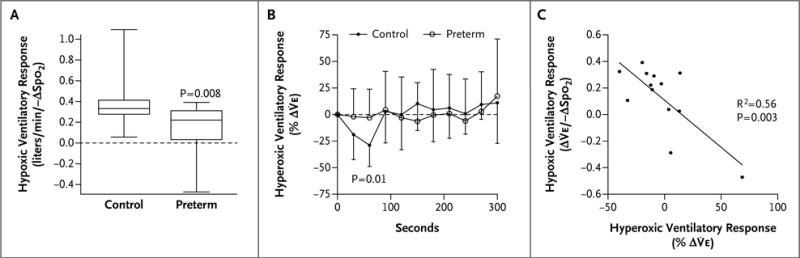
All full-term adults (controls) had increased ventilation in response to hypoxia (fraction of inspired oxygen [FIO2] = 0.10); paradoxically, some preterm adults hypoventilated in response to hypoxia and reported presyncopal symptoms at the end of the trial (Panel A; boxes depict the median and first and third interquartile ranges, with whiskers indicating maximum and minimum responses). After 60 seconds of hyperoxia (FIO2 = 1.0), ventilation was depressed in all full-term adults, but this response was blunted in preterm adults (Panel B; points represent the mean ±SD). The blunting of hyperoxic and hypoxic ventilatory responses was correlated in preterm adults, suggesting a common cause of ventilatory dysfunction (Panel C). The Δ symbol denotes change, SpO2 oxygen saturation as measured by pulse oximetry, and volume expired.
In rodents, perinatal hyperoxia disrupts the development of carotid chemoreceptors.4 The strong relationship between the hypoxic and hyperoxic ventilatory dysfunction in the preterm adults (Fig. 1) suggests a common impairment in chemoreceptor function that may be due to carotid chemoreceptor dysfunction. Our most compelling finding is that abnormal ventilatory responses were manifested only when these preterm adults, who appeared to be clinically normal, were stressed by breathing hypoxic and hyperoxic gas. This finding may have important clinical implications.5 We found that some preterm adults paradoxically hypoventilate with hypoxia.
In summary, adults with a history of preterm birth have abnormal ventilatory responses to hypoxia and hyperoxia, possibly due to disrupted chemoreceptor development. We speculate that these underappreciated abnormalities in ventilatory control may have important clinical consequences, including an increased risk of disordered breathing during sleep and in response to high altitude and anesthesia. Additional investigations into the mechanisms and long-term disease risks of this population are warranted.
Supplementary Material
Acknowledgments
Supported by grants from the National Institutes of Health (5R01HL086897, to Drs. Eldridge and Farrell, and 5T32HL007654, to Dr. Bates) and a postdoctoral fellowship from the American Heart Association (to Dr. Bates).
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.Calder NA, Williams BA, Smyth J, Boon AW, Kumar P, Hanson MA. Absence of ventilatory responses to alternating breaths of mild hypoxia and air in infants who have had bronchopulmonary dysplasia: implications for the risk of sudden infant death. Pediatr Res. 1994;35:677–81. doi: 10.1203/00006450-199406000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Katz-Salamon M, Lagercrantz H. Hypoxic ventilatory defence in very preterm infants: attenuation after long term oxygen treatment. Arch Dis Child Fetal Neonatal Ed. 1994;70:F90–5. doi: 10.1136/fn.70.2.f90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinstein MR, Peters ME, Sadek M, Palta M. A new radiographic scoring system for bronchopulmonary dysplasia. Pediatr Pulmonol. 1994;18:284–9. doi: 10.1002/ppul.1950180504. [DOI] [PubMed] [Google Scholar]
- 4.Bisgard GE, Olson EB, Jr, Wang ZY, Bavis RW, Fuller DD, Mitchell GS. Adult carotid chemoafferent responses to hypoxia after 1, 2, and 4 wk of postnatal hyperoxia. J Appl Physiol (1985) 2003;95:946–52. doi: 10.1152/japplphysiol.00985.2002. [DOI] [PubMed] [Google Scholar]
- 5.Bates ML, Pillers D-AM, Palta M, Farrell ET, Eldridge MW. Ventilatory control in infants, children, and adults with bronchopulmonary dysplasia. Respir Physiol Neurobiol. 2013;189:329–37. doi: 10.1016/j.resp.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


