Abstract
Posttraumatic stress symptoms (PTSS) are quite prevalent in transplant recipients, although full-scale posttraumatic stress disorder (PTSD) may not be that common. Those symptoms have been linked to poor transplant outcomes, perhaps owing to nonadherence to medications and other recommendations, brought about by the avoidance dimension of the PTSD/PTSS construct (patients may avoid taking their medications because they serve as reminder of the emotionally traumatic event – the transplant). Since it is possible to treat PTSD via specific psychotherapeutic techniques, and the treatment has been shown to be safe and likely effective in other populations, it would appear that the practitioners who treat transplant recipients should be familiar with the presentation and treatment of those symptoms. The present manuscript provides a systematic literature review of the PTSD/PTSS presentation in the pediatric transplant setting, a synthesis of available research findings, and suggestions for current care and future research.
Keywords: PTSD, posttraumatic stress, transplantation, adherence, non-adherence
INTRODUCTION
When faced with terrifying experiences, children and adults may develop symptoms consistent with posttraumatic stress disorder (PTSD). As defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; reference 1), PTSD is precipitated by an emotionally traumatic event and is characterized by re-experiencing symptoms, avoidance of trauma-related stimuli, negative alterations in cognitions and mood, and alterations in arousal and reactivity. The experiences that accompany being diagnosed with serious medical illnesses, or with their treatment (such as surgical interventions, including transplantation) have been shown to be associated with the development of PTSD or sub-diagnostic symptoms of PTSD (called posttraumatic stress symptoms or PTSS) (2-4).
It may be particularly important to recognize and address PTSD/PTSS in solid organ transplant recipients, for two unique reasons (5, 6). First, PTSD/PTSS are thought to be associated with the development of nonadherence to medical treatments because of the avoidance dimension of PTSD (patients avoid reminders of the traumatic event, which may translate to avoidance of medications, see below). Since graft survival is dependent on adequate immunosuppression, the consequences of not taking the medications (nonadherence) in transplant recipients can be particularly devastating. Second, a transplant operation is unique amongst other, more prevalent, potentially traumatic events (such as rape) in that in most cases it can be anticipated; transplantation can be thought of as a “scheduled trauma”. Therefore, the transplant setting provides a unique opportunity to engage in primary and secondary prevention of the development of PTSD/PTSS, in that steps could be taken to mitigate the traumatic nature of the transplant experience. The ability to study prevention of the development of PTSD makes the transplant setting particularly interesting, with potential to inform the broader field of emotional trauma research (3, 5).
We first performed a systematic review to identify all manuscripts pertaining to posttraumatic stress in transplant recipients. However, the aim of this manuscript is to provide more than the results of the systematic review. Since PTSD is a well described and substantially researched construct, we believe that it is imperative to present the findings in transplant recipients in the broad context of insights from the emotional trauma field in general, and we strive to provide this context. This manuscript, therefore, aims to describe the results of the systematic review in a broader context. We attempt to provide information that would be useful to researchers who are interested in studying the impact of emotional trauma on solid organ transplant recipients as well as practitioners who wish to incorporate current knowledge into their clinical management in the transplant setting.
METHOD
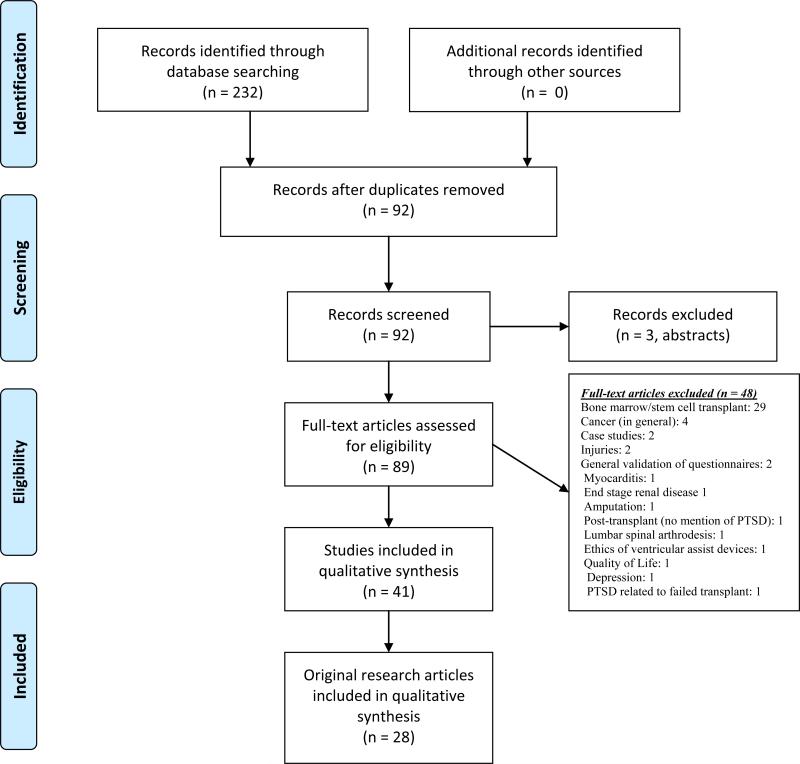
A systematic review of PTSD in transplant recipients was conducted as described below (Figure). Seminal manuscripts from the broader trauma research field are also cited to provide a context when indicated.
Figure 1.
Flow of information through the different phases of the systematic review.
Eligibility criteria
Published, peer-reviewed articles in which the relationship between posttraumatic stress and transplant was examined were eligible for study inclusion. Studies unavailable in English and those involving animals were excluded.
Information sources
Databases used were MEDLINE, PsycINFO, and PILOTS. For articles inaccessible online, authors were contacted. References from included articles were searched for further, additional articles that were considered likely to meet the inclusion criteria.
Search
Electronic search strategy example: MEDLINE keywords and nested search items: “Posttraumatic stress OR PTSD OR PTSS” AND “transplant OR transplantation”. Limits (language): English. Limits (species): Humans.
Study selection
Three online databases (MEDLINE, PsycINFO, and PILOTS) were searched systematically.
Data collection process
Data were collected and entered into Excel (Microsoft Office Excel, Version 14.4.3).
RESULTS
Following a systematic procedure (Figure), 41 manuscripts were identified. 13 were review articles, and the rest (28 manuscripts) are included in this review. Summaries of the original research manuscripts (References 11-38) are included in supplemental on-line materials (Tables S1-S4).
Theoretical consideration identified in the review process
One basic and still unanswered question is whether PTSS, which are quite common in some settings (2-5), necessarily represent a clinically significant problem, or are simply a normal response to a stressful situation. Although the number of required symptoms for a diagnosis of PTSD is defined in DSM-5, it is unclear how many PTSD symptoms must be present to reach a clinically significant threshold within a medically ill population. It is also unclear whether any single symptom, or set of symptoms, must be present for dysfunction to occur and how severe the symptoms must be before an intervention is needed. PTSD symptoms, in some cases, might not be dysfunctional. They may be associated with posttraumatic growth, an under-investigated construct that proposes that some traumatic exposure may lead to positive psychological change and resilience (7-9).
Specifically in children, theoretical questions are raised which offer a challenge and opportunity to examine basic concepts related to PTSD. Parents are technically “witnesses” to trauma when a child goes through a life-threatening illness. Parents’ role with regard to their medically ill children is more complicated than witnesses, however, as they are decision-makers and participants in the treatment. For example, parent might be the donor, and under some circumstances, parents may physically hold the protesting child to restrain him or her while receiving a treatment or test. In PTSD that is related to the treatment of medical illness (i.e., a transplant), children may therefore consider the physicians or their parents to be the “perpetrators” of the trauma. In what ways do symptoms differ if one is a “witness”, a “victim”, a “caregiver” or a “perpetrator”? Which of these best describes the role a parent plays, as the decision-maker for painful medical procedures? Developmental considerations will also prove to be important to our understanding of the reactions to this type of trauma as cognitive capacity is known to affect response to traumatic events (10).
Studies of PTSD in pediatric transplant recipients
Rates of approximately 30% of pediatric solid organ transplant recipients endorsing above threshold rates of PTSS have been reported (20, 23). These studies used self-report measures and not a full psychiatric interview tool. For example, 99 recipients of heart, liver, or kidney transplants (23), 12 to 20 years old at time of interview (M=15.7), were assessed for symptoms of PTSD. Of the entire group, 31.3% (31/99) reported diagnostic levels of PTSD symptoms occurring at least twice a month, with 13.3% reporting diagnostic PTSD symptoms occurring at least twice a week. The type of transplant did not influence the rate of PTSD. Another study (N=104) with the same age range reported a lower rate of 16% (12). In this study, no demographic predictors of PTSD could be identified.
While PTSD symptoms are well documented as a result of serious medical illnesses, a few cautionary remarks are due:
Methods of assessing PTSD
Studies vary widely in the methods used to detect PTSD and, with a few exceptions, most do not use a clinical interview but rather a self-report questionnaire that may not accurately reflect a clinical diagnosis. Additionally, there is a great deal of variation in the self-report measures chosen. The use of different tools and different cutoff points make it hard to compare data between studies. Indeed, a small study which compared two self-report measures and structured interviews found substantial discrepancies between methods (39). Table 1 provides a summary of methods that are commonly used to assess for PTSD symptoms or diagnostic status, in decreasing order of common use, in the general traumatic stress research field as compared with solid organ transplant literature. Of note, in children in general as well as in pediatric transplant recipients in particular, the most widely used instrument is the UCLA posttraumatic Stress Reaction Index in its numerous iterations. A notable difference between research related to posttraumatic stress in transplantation as compared with the general PTSD literature is that researchers in the transplant field have been much less likely to use diagnostic tools – research in the transplant setting has concentrated primarily on posttraumatic symptoms rather than the full disorder, whereas PTSD researchers in other fields are more likely to look at the diagnostic threshold. We could find only one small study in pediatric transplant recipients (13) that tried to investigate the differential value of symptom level (“PTSS”) versus diagnostic threshold (“PTSD”)in predicting physical outcomes (medication level variability). That study found that the diagnostic construct is preferred to a simple summation of symptom rates. Those results should be viewed as tentative, given the small sample size and limited analyses used, but the difference in assessment strategies between transplant settings and the general literature is not trivial. It is, on one hand, possible that the transplant setting is special and merits a different conceptualization of posttraumatic symptoms. But on the other hand, PTSD researchers in other settings have serious reasons for preferring to look at the diagnostic construct rather than at the symptoms level. For example, the biological underpinnings of PTSD seem to align with the diagnostic schema (40), and most of the intervention research in PTSD is predicated on the existence of a PTSD diagnosis (not symptom level) as an indication that treatment is needed.
TABLE 1.
PTSD assessment tools for children & adults
| PTSD assessments | General PTSD literature | Transplant recipients | Caregivers of transplant recipients | Spouses of transplant recipients |
|---|---|---|---|---|
| Children; children & young adults | UCLA Child Post-Traumatic Stress Disorder Reaction Index (CPTS-RI) Child PTSD Symptom Scale (CPSS) |
UCLA CPTS-RI (Walker et al., 11) CPSS (McCormick King et al., 20) DTS (Wallace et al., 21) |
N/A | N/A |
| Trauma Symptom Checklist for Children (TSCC) | Posttraumatic Stress Symptoms Scale (PTSS-10; Rothenhäusler et al., 45) | |||
| Impact of Events Scale - Revised (IES-R) | SCID module for PTSD (Rothenhäusler et al., 45) | |||
| Diagnostic Interview for Children and Adolescents - Revised (DICA-R) - PTSD Module | In German, PTSS-10, in German (Baranyi et al., 30) | |||
| Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children - Present and Lifetime version (K-SADS) - PTSD module | ||||
| Clinician Administered PTSD Scale for Children and Adolescents (CAPS-CA) | ||||
| Adults | Posttraumatic Diagnostic Scale (PDS) IES or IES-R PTSD Checklist (PCL) Trauma Symptom Inventory (TSI) Kean PTSD Scale Symptom Checklist 90-R's PTSD Subscales |
IES-R (Guimaro et al., 37) PCL (Possemato et al., 28,29) SCID modules for PTSD (Favaro et al., 27) SCID module for PTSD specifically asking about PTSD related to transplant experience (Dew et al., 36) Created by authors - PTSD Questionnaire (PTSD-Q; Inspector et al., 35) Created by authors - PTSD assessment, adapted from WHO/ADMHA CIDI and DSM-III criteria-R (Dew et al., 31-34) In Chinese - PTSD Self-Rating Scale (PTSD-SS; Jin et al., 26) |
IES-R (Rossi et al., 24) PDS (Farley et al., 25; Young et al., 23) Created by authors - PTSD assessment, adapted from WHO/ADMHA CIDI and DSM-III criteria-R (22). |
In German, IES-R (Bunzel et al., 16-18) |
Developmental considerations
Developmental differences alter the type of response to trauma at different ages (41). Symptoms depend on the child's understanding of the trauma, and his / her degree of independence. Some medical-illness-related PTSD symptoms appear only around young adulthood (42). Hence, “lumping together” children from different stages of maturity and ages, which is what most studies do, may lead to inability to detect some attributes of traumatization as experienced at different stages. On the other hand, stratifying by age would result in a loss of statistical power and hence require much larger samples which are difficult to achieve in single center studies.
Parents of pediatric transplant recipients
In a study of parents of children who had undergone kidney, heart, or liver transplantation (35), about 27% of parents met full diagnostic criteria for PTSD. The rate of full PTSD was reported as 19% and elevated PTSS rates were detected among 40% of a sample of parents of children who had a heart transplant (25). Results from another study surveying mothers and fathers found far higher rates of PTSD in mothers (52%) and fathers (40%) (24). However, these rates may be spuriously high as a screening tool (the Impact of Event Scale-Revised; IES-R) was used to identify PTSD rather than a diagnostic measure. Of note, PTSD was significantly associated with trait anxiety, suggesting that anxious parents are more susceptible to developing clinically significant distress in the wake of their child's transplant.
Nature of the stressor
Many stressful events happen in the course of a chronic illness, and many of these may be traumatic. Which of these are more likely to be the cause of PTSD has been the focus of recent research. It seems that medical procedures and treatments, such as transplantation and chemotherapy, are more often cited as traumatic events by children who report PTSD symptoms than are any other disease-related traumatic events (5). Hence, the trauma, more often than not, is “inflicted” by caregivers or medical professionals. This view of trauma is consistent with other reports that show that traumatic stress symptoms are more likely to be reported in relation to events that are related to the deeds of other humans (e.g., combat experience, rape) rather than other types of traumatization (43).
Predictors and risk factors for the development of PTSD in medically ill patients
The study of predictors and risk factors for the development of PTSD is rapidly advancing (44), partly because it is widely recognized as an important step on the way to develop effective treatment strategies. Trauma that is associated with the treatment of medical illness (such as transplantation) provides a unique opportunity to study risk factors for PTSD prior to traumatization; indeed, medical-illness related procedures often belong to a rare group of “scheduled” traumas. Such prospective studies are currently under way, and may allow a better understanding of traumatization in general, not only medical-illness related PTSD. At the time of submission of this review, however, most studies looking at predictors for PTSD that is related to transplantation were either cross-sectional or conducted after the trauma has occurred. We have found no robust proof of any specific risk factor for the development of PTSD in pediatric solid organ transplant recipients, and found a few potential risks that appeared to be disproven. Table 2 lists risk factors categorized by the setting in which they were examined (general PTSD literature / transplant literature / recipient vs caregiver). Of note, it is very likely that many of the risks that were proven in the general literature do apply in pediatric transplant settings even if they were not specifically proven in that setting.
TABLE 2.
PTSD risk factors
| Studied risk factors | General PTSD literature (children/young adult) | Child/young adult transplant recipients | General PTSD literature (adult) | Adult transplant recipients | Caregivers of transplant recipients | Spouses of transplant recipients |
|---|---|---|---|---|---|---|
| Associated with PTSD | Prior psychological problems Parental psychological problems Previous negative life events Low IQ Low SES Female Sex Ethnicity Younger age (only if the trauma is a group event, not an individual event) Trauma severity Peritraumatic fear Perceived life threat during traumatic event |
None proven. | Psychiatric history Prior psychological/adjustment problems Previous trauma Reported childhood abuse General childhood adversity Family psychiatric history Lower education Peritraumatic dissociation Peritraumatic emotionality (high emotions) Perceived life threat during traumatic event In some study samples: Gender, younger age at trauma, race. |
Pre-existing psychiatric diagnosis (30). Greater benzodiazepine consumption (30) Younger age at interview (30) History of retransplantation (30) For lung transplant recipients, chronic dyspnea early post-transplant (36) |
None identified. | None identified. |
| Not associated with PTSD | Younger age (only if the trauma is an individual event, not a group event | Gender (12, 21) Age at time of transplant (12) Age at interview (12, 21) Time since transplant (12) Organ type (12) Ethnicity (12) |
In some study samples (63): Gender, Younger age at trauma, Race/ethnicity | Gender (30). Age at interview (Possemato et al., 2009) Alcohol abuse (30) Marital status (30) Years in education and/or vocational training (30) Employment status (30) For heart transplant recipients, presence of VAD (34) |
Gender (recipient) (23) Age at time of transplant (recipient) (23, 24) Time since transplant (24) Organ type (23) Caregiver's age at time of transplant (23, 24) Caregiver's educational level (23) Caregiver's ethnicity (23) Caregiver's level of acculturation (23) |
Age at interview (recipient) (18) Time since transplant (18) Type of assist device for heart transplant recipients (18) Indication for heart transplantation (18) |
Note: To identify risk factors in the general PTSD literature, three relatively recent meta-analyses were used, with only pre- and peri-trauma variables considered (61-63). To determine risk factors in the transplant literature, variables that are static or unrelated to PTSD effects (i.e., age, ethnicity, time since transplant, organ type) or are preoperative were used.
Consequences of PTSD
Investigation of sequelae of PTSD in Transplant recipients is difficult because of the need to control for intervening variables that are related to the illness itself. Examples of problems in the investigation of such long-term sequelae include uncertainty about the nature of the stressor, and the distinction between whether symptoms are related to the primary illness or to PTSD.
It is often unclear and difficult to tease out whether symptoms stem from PTSD or the underlying illness. A specific symptom, such as inability to concentrate, may be attributed to the medical illness or to a psychiatric disorder. A study of adult transplant recipients found a relationship between PTSD symptoms and cognitive performance (45). Among pediatric patients we do not yet know if poor school grades are related to PTSD symptoms or, for example, to cognitive deterioration due to the underlying disease process (46).
Despite these difficulties, several studies shed light on the potential importance of this disorder. In a longitudinal, prospective study of 101 adult survivors of heart transplantation, PTSD was the strongest predictor of cardiac morbidity (31). One potential mediator of these poor outcomes is nonadherence to medical recommendations (19). In a study of 19 children and adolescent survivors of liver transplantation, followed for at least a year post transplant, nonadherence to medications was significantly more common in children who displayed above-threshold PTSS (13). Nonadherence to medications may be related to the avoidance dimension of PTSD (patients avoid taking the medication because it is a traumatic reminder of the illness), and indeed the avoidance dimension of PTSD accounted for much of the association with nonadherence in the pediatric transplant study (13). In adults, a correlation between nonadherence and PTSD is considered to be an established finding (47-49).
In the aggregate, these studies suggest that PTSD is associated with serious psychiatric and medical morbidity. It is also plausible that PTSD or PTSS serves as a clear-cut, modifiable predictor of nonadherence to medical recommendations.
Prevention and treatment
Since posttraumatic stress responses may lead to medical as well as psychological morbidity, appropriate interventions for the prevention and treatment of traumatic stress responses to medical life-threat must be developed and tested. The tremendous opportunity for productive intervention is supported by a small case-series reporting significant improvement in the medical adherence of pediatric transplant patients who were treated for PTSD using prolonged imaginal exposure, a cognitive-behavior therapy approach (13).
Many events in the course of transplantation can be anticipated. This offers the opportunity to develop and test preventative strategies. Unfortunately, prevention of PTSD remains an elusive target. Preventative strategies have not been tested rigorously in transplant recipients or in any medically ill individuals. In the broader PTSD research community, prevention has become an important topic. Strategies include prescribing medications before symptoms are present (for example, corticosteroids, to favorably affect the Hypothalamus-Pituitary-Adrenal axis; opioids to reduce discomfort; or beta-blockers to reduce arousal) as well as providing other non-biological interventions, with various degrees of promise (50, 51). In addition, medical life-threat often occurs in a supportive family setting, and appears to lead to significant traumatic responses in the family. It would, therefore, seem to suggest that family interventions might be helpful, but there has been very limited study of family interventions in medically ill populations for the purpose of alleviating PTSS, and one randomized controlled study found that a family intervention did not improve the primary outcome (52).
Both Paroxetine and Sertraline are approved for the treatment of PTSD in adults (53), but no medication has been approved for this indication in children.
With regards to psychotherapy, to date there are only three published prospective, controlled studies of psychotherapeutic treatments for PTSD in medically ill adults, and none in children. Of these, only two used random allocation of the treatment. In one controlled (but not randomized) study of cardiac patients, investigators noted an improvement in medical outcomes and adherence to treatment in a small group of patients who received cognitive-behavioral therapy (CBT), as compared with both a treatment-as-usual control and an enhanced education control (54). DuHamel et al. (55) provided a 10-session, telephone-based, CBT intervention for survivors of hematopoietic stem-cell transplantation (HCST). There was a decrease in PTSS across all follow-up assessments (6, 9 and 12 months afterbaseline), but medical outcomes were not examined. The intervention included relaxation training, guided exposure to cues associated with PTSD symptoms, monitoring and alteration of maladaptive beliefs, communication skills training (for enhancement of social support), and psychoeducation around illness-related PTSD symptoms. Further analysis of the treatment effects demonstrated that the treatment was effective for avoidance and intrusive thoughts but not for hyperarousal and numbing. Another randomized controlled prospective study used an exposure-based paradigm in adults with cardiovascular illness (56). That study established the safety and preliminary efficacy of this cognitive-behavioral psychotherapeutic approach. There are no similar studies in medically ill children. However, research with PTSD due to other causes has shown that it is often a highly treatable condition in children using an imaginal exposure paradigm (57).
Methodological issues with research targeting PTSD in transplant recipients
1. Selection bias
Perhaps the most significant drawback that we have identified in reviewing research efforts to date is that many of the studies that we reviewed were probably unable to enroll a representative sample of patients. Convenience sampling was generally used, and most studies do not cite specific information about the degree of potential bias. Avoidance is an important component of PTSD, and it is likely that convenience sampling will fail to enroll patients who suffer from the most severe form of the disorder.
2. Post-hoc analyses
Another important drawback is the apparent failure to pre-specify endpoints in many of the studies that we examined. In addition, under the current system it is not mandatory to register studies that do not involve an intervention. Even when authors contend that they did had a directional hypothesis which was pre-specified before the study commenced, in the absence of registration, it is impossible to verify whether authors’ claims are in fact warranted. Post-hoc analyses of studies with small sample sizes are very likely to result in spurious results.
3. Confusion between association and cause-and-effect relationships
Since PTSD symptoms are more likely to emerge when the trauma itself is more severe, the finding that PTSD is associated with poor outcomes cannot be taken to mean that PTSD symptoms in fact cause those poor outcomes. Mechanistic and treatment studies are essential in order to determine whether in fact treatment of PTSD improves medical outcomes.
4. Failure to account for mental health comorbidity, especially depression
Since PTSD is highly comorbid with depression (48), any association between PTSD and poor outcomes could be due to depression or other factors. Few studies tried to disentangle the effects of depression and PTSD on outcomes, and those that did found mixed results. The potential relationship between PTSD symptoms, depression, and poor outcomes, may be complex or linear. One intriguing schema (48) posits that the experience of the trauma (the transplant) can lead to PTSD symptoms which lead, through nonadherence, to poor outcomes and then to depression (because of the poor outcomes). If this is the case, although both depression and PTSD would be associated with poor outcomes, treatment of PTSD but not depression would be expected to improve those outcomes. It is not clear whether this association pattern is in fact correct.
Clinical approaches to the assessment, prevention, and treatment children with PTSS in medical settings
In the absence of rigorous evidence, the following suggestions are offered to help clinicians develop a sensible approach to intervention in pediatric transplant recipients.
-
1)
As the perception of life threat is critically important in the development of PTSD, it appears prudent to recommend that clinicians try to provide clarity about the transplant procedure, as well as strive to evaluate the child's (and parent's) understanding of this information, and interact to modify this understanding, if needed. This approach may be more effective if delivered in an interactive and patient-centered format.
-
2)
Enhancing physical comfort during and after the operation might mitigate the traumatic impact of the transplant. While aggressive prescription of opioids seems to have some promise in alleviating PTSS in burn victims (45), it is not clear to what extent it applies in the transplant setting.
-
3)
Negative premorbid life events have also been associated with PTSD symptoms. Therefore, helping the caregiver obtain referrals, resources, and/or work on pre-existing vulnerabilities may be helpful.
-
4)
Not all transplant recipients develop PTSD. Our reading of the evidence suggests that those symptoms are not “normal”, and their presence may well be associated with poor outcomes. Pending more conclusive evidence, we believe that the presence of those symptoms in the transplant setting should not be ignored, especially since effective interventions for PTSD do exist. If substantial PTSD symptoms are noted in a transplant setting, we believe that prompt referral to a mental health professional familiar with the treatment of PTSD is indicated...
-
5)
Caretakers may be more at risk for PTSS than patients (e.g., 17, 18). Caretakers’ symptoms and well-being should not be ignored and interventions should probably include caretakers or even target them.
Summary and recommendations for future research
Posttraumatic stress symptoms have been reported in response to a variety of life threatening medical illnesses in adults and children, including organ transplant recipients. Data suggest that children often experience life-saving medical procedures as traumatic. Trauma symptoms are also reported as quite common and severe in the caregivers. Developmental considerations, the nature and severity of the event itself, social support, and premorbid exposure to negative life events are important issues to consider in developing appropriate interventions. It is important to continue to study which assessment methods may be used for screening for as well as diagnose PTSS and PTSD. Are self-reports sufficient as a first tier screening? Can one use self-report “symptom scores” for diagnostic purposes? Can interview tools be used by providers who are not mental health professionals? – all of those questions have important implications for resource allocation decisions in the transplant setting. It is also important to consider sample size and recruitment strategies in future studies so as to ensure that samples are representative and results can provide generalizable information. Hypotheses should be pre-specified and not post-hoc. Registration of studies (even if they do not include an intervention) is one method that can be used by authors to prove that a study did indeed include a pre-specified primary hypothesis.
The transplant setting is uniquely suited for the study of PTSD, its consequences, its prevention, and its treatment. This is because outcome measures for transplant recipients are relatively well-defined and some are even reported nationally (thus, it is relatively easy to follow outcome data in this population), the trauma usually can be anticipated (and therefore potentially prevented), and the consequences may be dire (thus creating an imperative to provide treatment). Over the past decade or so, the transplant field has recognized the importance of those symptoms in recipients. However, interventions have not yet been developed or studied. It is time to move forward towards a better definition of the target of the intervention (what is the trauma), the group of patients who are likely to benefit most, and the type of outcomes that are most likely to be improved (e.g., adherence). Once those are known, intervention research can proceed. In our opinion, since there is a plausible mechanistic explanation linking PTSD, medication nonadherence, and poor outcomes (through the avoidance dimension of PTSD), intervention strategies that address avoidance may be promising, with the caveat that it may be hard to engage avoidant patients in treatment. A remotely delivered psychotherapeutic approach that does not require that a patient be actually present in the clinic and yet does include interaction with a skilled therapist that would allow real engagement in treatment might prove to be helpful. Since patients who suffer from PTSD are already at risk for not taking their medications, it would appear that psychopharmacologic interventions should not constitute the first line of treatment.
We hope that ultimately, PTSD interventions will have a positive impact on transplant outcomes and the quality-of-life of recipients, and also shed light on efforts to prevent the emotional consequences of traumatization in the overall traumatic stress field.
Supplementary Material
Acknowledgments
Supported by NIH/NIDDK award # R01DK080740 (ES) and # R01DK080740-S (CS)
Footnotes
No conflict of interest.
REFERENCES
- 1.AMERICAN PSYCHIATRIC ASSOCIATION . Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; Washington DC: 2013. [Google Scholar]
- 2.STUBER ML, SHEMESH E. Post-traumatic stress response to life-threatening illnesses in children and their parents. Child Adolesc Psychiatr Clin N Am. 2006;15(3):597–609. doi: 10.1016/j.chc.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 3.SHEMESH E, STUBER ML. Posttraumatic stress disorder in medically ill patients: what is known, what needs to be determined, and why is it important? CNS Spectr. 2006;11(2):106–17. doi: 10.1017/s1092852900010646. [DOI] [PubMed] [Google Scholar]
- 4.CAVALCANTI-RIBEIRO P, ANDRADE-NASCIMENTO M, MORAIS-DE-JESUS, et al. Post-traumatic stress disorder as a comorbidity: impact on disease outcomes. Expert Rev Neurother. 2012;12(8):1023–1037. doi: 10.1586/ern.12.77. [DOI] [PubMed] [Google Scholar]
- 5.STUBER ML, SHEMESH E, SAXE GN. Posttraumatic stress responses in children with life-threatening illnesses. Child Adolesc Psychiatr Clin N Am. 2003;12(2):195–209. doi: 10.1016/s1056-4993(02)00100-1. [DOI] [PubMed] [Google Scholar]
- 6.SHEMESH E, ANNUNZIATO RA, YEHUDA R, et al. Childhood abuse, nonadherence, and medical outcome in pediatric liver transplant recipients. J Am Acad Child Adolesc Psychiatry. 2007;46(10):1280–9. doi: 10.1097/chi.0b013e3180f62aff. [DOI] [PubMed] [Google Scholar]
- 7.NELSON D. The posttraumatic growth path: An emerging model for prevention and treatment of trauma-related behavioral health conditions. J Psychother Integr. 2011;1(21):1–42. [Google Scholar]
- 8.MANNE S, OSTROFF J, WINKEL G, GOLDSTEIN L, FOX K, GRANA G. Posttraumatic growth after breast cancer: patient, partner, and couple perspectives. Psychosom Med. 2004;66(3):442–54. doi: 10.1097/01.psy.0000127689.38525.7d. [DOI] [PubMed] [Google Scholar]
- 9.TEDESCHI RG, CALHOUN LG, CANN A. Evaluating resource gain: Understanding and misunderstanding posttraumatic growth. Applied Psychology. 2007;11:608–614. [Google Scholar]
- 10.DANIELS JK, FREWEN P, MCKINNON MC, LANIUS RA. Default mode alterations in posttraumatic stress disorder related to early-life trauma: a developmental perspective. J Psychiatry Neurosci. 2011;36(1):56–9. doi: 10.1503/jpn.100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WALKER AM, HARRIS G, BAKER A, KELLY D, HOUGHTON J. Post-traumatic stress responses following liver transplantation in older children. J Child Psychol Psychiatry. 1999;40(3):363–74. [PubMed] [Google Scholar]
- 12.MINTZER LL. Traumatic stress symptoms in adolescent organ transplant recipients. Pediatrics. 2005;115(6):1640–4. doi: 10.1542/peds.2004-0118. [DOI] [PubMed] [Google Scholar]
- 13.SHEMESH E, LURIE S, STUBER ML, et al. A pilot study of posttraumatic stress and nonadherence in pediatric liver transplant recipients. Pediatrics. 2000;105(2):E29. doi: 10.1542/peds.105.2.e29. [DOI] [PubMed] [Google Scholar]
- 14.SHEMESH E, ANNUNZIATO RA, SHNEIDER BL, et al. Parents and clinicians underestimate distress and depression in children who had a transplant. Pediatr Transplant. 2005;9(5):673–9. doi: 10.1111/j.1399-3046.2005.00382.x. [DOI] [PubMed] [Google Scholar]
- 15.ROTHENHÄUSLER HB, EHRENTRAUT S, KAPFHAMMER HP, LANG C, et al. Psychiatric and psychosocial outcome of orthotopic liver transplantation. Psychother Psychosom. 2002;71(5):285–97. doi: 10.1159/000064811. [DOI] [PubMed] [Google Scholar]
- 16.BUNZEL B, ROETHY W, ZNOJ H, LAEDERACH-HOFMANN K. Psychological consequences of life-saving cardiac surgery in patients and partners: measurement of emotional stress by the Impact of Event Scale. Stress Health. 2008;24(5):351–63. [Google Scholar]
- 17.BUNZEL B, LAEDERACH-HOFMANN K. Mechanical circulatory support as a bridge to heart transplantation: what remains? Long-term emotional sequelae in patients and spouses. J Heart Lung Transplant. 2007;26(4):384–9. doi: 10.1016/j.healun.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 18.BUNZEL B, LAEDERACH-HOFMANN K, WIESELTHALER GM, ROETHY W, DRESS G. Posttraumatic stress disorder after implantation of a mechanical assist device followed by heart transplantation: evaluation of patients and partners. Transplant Proc. 2005;37(2):1365–8. doi: 10.1016/j.transproceed.2004.12.248. [DOI] [PubMed] [Google Scholar]
- 19.KERKAR N, ANNUNZIATO RA, FOLEY L, et al. Prospective analysis of nonadherence in autoimmune hepatitis: a common problem. J Pediatr Gastroenterol Nutr. 2006;43(5):629–34. doi: 10.1097/01.mpg.0000239735.87111.ba. [DOI] [PubMed] [Google Scholar]
- 20.MCCORMICK-KING ML, MEE LL, GUTIERREZ-COLINA AM, EATON CK, LEE JL, BLOUNT RL. Emotional functioning, barriers, and medication adherence in pediatric transplant recipients. J Pediatr Psychol. 2014;39(3):283–93. doi: 10.1093/jpepsy/jst074. [DOI] [PubMed] [Google Scholar]
- 21.WALLACE J, YORGIN PD, CAROLAN R, et al. The use of art therapy to detect depression and post-traumatic stress disorder in pediatric and young adult renal transplant recipients. Pediatr Transplant. 2004;8(1):52–9. doi: 10.1046/j.1397-3142.2003.00124.x. [DOI] [PubMed] [Google Scholar]
- 22.DEW MA, MYASKOVSKY L, DIMARTINI AF, SWITZER GE, SCHULBERG HC, KORMOS RL. Onset, timing and risk for depression and anxiety in family caregivers to heart transplant recipients. Psychol Med. 2004 Aug;34(6):1065–82. doi: 10.1017/s0033291703001387. [DOI] [PubMed] [Google Scholar]
- 23.YOUNG GS, MINTZER LL, SEACORD D, CASTAÑEDA M, MESRKHANI V, STUBER ML. Symptoms of posttraumatic stress disorder in parents of transplant recipients: incidence, severity, and related factors. Pediatrics. 2003;111(6 Pt 1):725–31. doi: 10.1542/peds.111.6.e725. [DOI] [PubMed] [Google Scholar]
- 24.ROSSI A, DE RANIERI C, TABARINI P, et al. The department of psychology within a pediatric cardiac transplant unit. Transplant Proc. 2011;43(4):1164–7. doi: 10.1016/j.transproceed.2011.01.119. [DOI] [PubMed] [Google Scholar]
- 25.FARLEY LM, DEMASO DR, D'ANGELO E, et al. Parenting stress and parental post-traumatic stress disorder in families after pediatric heart transplantation. J Heart Lung Transplant. 2007;26(2):120–6. doi: 10.1016/j.healun.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 26.JIN SG, YAN LN, XIANG B, et al. Posttraumatic stress disorder after liver transplantation. Hepatobiliary Pancreat Dis Int. 2012;11(1):28–33. doi: 10.1016/s1499-3872(11)60122-7. [DOI] [PubMed] [Google Scholar]
- 27.FAVARO A, GEROSA G, CAFORIO AL, et al. Posttraumatic stress disorder and depression in heart transplantation recipients: the relationship with outcome and adherence to medical treatment. Gen Hosp Psychiatry. 2011;33(1):1–7. doi: 10.1016/j.genhosppsych.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 28.POSSEMATO K, GELLER PA, OUIMETTE P. Posttraumatic stress and quality of life in kidney transplantation recipients. Traumatol. 2009;15(3):34–9. [Google Scholar]
- 29.POSSEMATO K, OUIMETTE P, GELLER PA. Internet-based expressive writing for kidney transplant recipients: effects on posttraumatic stress and quality of life. Traumatol. 2010;16(1):49–54. [Google Scholar]
- 30.BARANYI A, KRAUSENECK T, ROTHENHÄUSLER HB. Posttraumatic stress symptoms after solid-organ transplantation: preoperative risk factors and the impact on health-related quality of life and life satisfaction. Health Qual Life Outcomes. 2013;11:111. doi: 10.1186/1477-7525-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DEW MA, ROTH LH, SCHULBERG HC, et al. Prevalence and predictors of depression and anxiety-related disorders during the year after heart transplantation. Gen Hosp Psychiatry. 1996;18(6):48S–61S. doi: 10.1016/s0163-8343(96)00077-1. [DOI] [PubMed] [Google Scholar]
- 32.DEW MA, KORMOS RL, ROTH LH, MURALI S, DIMARTINI A, GRIFFITH BP. Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. J Heart Lung Transplant. 1999;18(6):549–62. doi: 10.1016/s1053-2498(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 33.DEW MA, KORMOS RL, DIMARTINI AF, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. 2001;42(4):300–13. doi: 10.1176/appi.psy.42.4.300. [DOI] [PubMed] [Google Scholar]
- 34.DEW MA, KORMOS RL, WINOWICH S, et al. Quality of life outcomes after heart transplantation in individuals bridged to transplant with ventricular assist devices. J Heart Lung Transplant. 2001;20(11):1199–212. doi: 10.1016/s1053-2498(01)00333-3. [DOI] [PubMed] [Google Scholar]
- 35.INSPECTOR Y, KUTZ I, DAVID D. Another person's heart: magical and rational thinking in the psychological adaptation to heart transplantation. Isr J Psychiatry Relat Sci. 2004;41(3):161–73. [PubMed] [Google Scholar]
- 36.DEW MA, DIMARTINI AF, DEVITO-DABBS AJ, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychiatry. 2012;34(2):127–38. doi: 10.1016/j.genhosppsych.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.GUIMARO MS, LACERDA SS, AGUILAR MR, KARAM CH, KERNKRAUT AM, FERRAZ-NETO BH. Post-traumatic stress disorders, mood disorders, and quality of life in transplant recipients with acute liver failure. Transplant Proc. 2011;43(1):187–8. doi: 10.1016/j.transproceed.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 38.KABA E, THOMPSON DR, BURNARD P, EDWARDS D, THEODOSOPOULOU E. Somebody else's heart inside me: a descriptive study of psychological problems after a heart transplantation. Issues Ment Health Nurs. 2005;26(6):611–25. doi: 10.1080/01612840590959452. [DOI] [PubMed] [Google Scholar]
- 39.EINSLE F, KRAFT D, KÖLLNER V. Post-traumatic stress disorder (PTSD) in cardiology and oncology--which diagnostic tools should be used? J Psychosom Res. 2012;72(6):434–8. doi: 10.1016/j.jpsychores.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 40.Yehuda R. Biology of posttraumatic stress disorder. J Clin Psychiatry. 2001;62(Suppl 17):41–6. [PubMed] [Google Scholar]
- 41.STUBER ML. Psychiatric aspects of organ transplantation in children and adolescents. Psychosomatics. 1993;34(5):379–87. doi: 10.1016/S0033-3182(93)71840-X. [DOI] [PubMed] [Google Scholar]
- 42.OGLE CM, RUBIN DC, SIEGLER IC. The impact of the developmental timing of trauma exposure on PTSD symptoms and psychosocial functioning among older adults. Dev Psychol. 2013;49(11):2191–200. doi: 10.1037/a0031985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.YEHUDA R. Risk factors for posttraumatic stress disorder. American Psychiatric Press; Washington DC: 1999. [Google Scholar]
- 44.MEESKE KA, RUCCIONE K, GLOBE DR, STUBER ML. Posttraumatic stress, quality of life, and psychological distress in young adult survivors of childhood cancer. Oncol Nurs Forum. 2001;28(3):481–9. [PubMed] [Google Scholar]
- 45.ROTHENHÄUSLER HB, EHRENTRAUT S, KAPFHAMMER HP, et al. Psychiatric and psychosocial outcome of orthotopic liver transplantation. Psychother Psychosom. 2002;71(5):285–97. doi: 10.1159/000064811. [DOI] [PubMed] [Google Scholar]
- 46.SORENSEN LG, NEIGHBORS K, MARTZ K, ZELKO F, BUCUVALAS JC, ALONSO EM, Studies of Pediatric Liver Transplantation (SPLIT) Research Group and the Functional Outcomes Group (FOG) Longitudinal study of cognitive and academic outcomes after pediatric liver transplantation. J Pediatr. 2014;165(1):65–72. doi: 10.1016/j.jpeds.2014.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.SHEMESH E, RUDNICK A, KALUSKI E, et al. A prospective study of posttraumatic stress symptoms and nonadherence in survivors of a myocardial infarction (MI). Gen Hosp Psychiatry. 2001;23(4):215–22. doi: 10.1016/s0163-8343(01)00150-5. [DOI] [PubMed] [Google Scholar]
- 48.COTTER G, MILO-COTTER O, RUBINSTEIN D, SHEMESH E. Posttraumatic stress disorder: a missed link between psychiatric and cardiovascular morbidity? CNS Spectr. 2006;11(2):129–36. doi: 10.1017/s109285290001066x. [DOI] [PubMed] [Google Scholar]
- 49.SHEMESH E, YEHUDA R, MILO O, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosom Med. 2004;66(4):521–6. doi: 10.1097/01.psy.0000126199.05189.86. [DOI] [PubMed] [Google Scholar]
- 50.YEHUDA R. Treating trauma survivors with PTSD. 1st edition Amer Psychiatric Pub; Arlington, VA, USA: May, 2002. [Google Scholar]
- 51.AMOS T, STEIN DJ, IPSER JC. Pharmacological interventions for preventing post-traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2014;8(7):CD006239. doi: 10.1002/14651858.CD006239.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.STEHL ML, KAZAK AE, ALDERFER MA, et al. Conducting a randomized clinical trial of an psychological intervention for parents/caregivers of children with cancer shortly after diagnosis. J Pediatr Psychol. 2009;34(8):803–16. doi: 10.1093/jpepsy/jsn130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.PTSD / NIMH [April 1, 2015]; http://www.nimh.nih.gov/health/publications/post-traumatic-stress-disorder-ptsd/index.shtml.
- 54.SHEMESH E, KOREN-MICHOWIZ M, YEHUDA R, et al. Symptoms of posttraumatic stress disorder in patients who have had a myocardial infarction. Psychosomatics. 2006;47(3):231–9. doi: 10.1176/appi.psy.47.3.231. [DOI] [PubMed] [Google Scholar]
- 55.DUHAMEL KN, MOSHER CE, WINKEL G, et al. Randomized clinical trial of telephone-administered cognitive-behavioral therapy to reduce post-traumatic stress disorder and distress symptoms after hematopoietic stem-cell transplantation. J Clin Oncol. 2010;28(23):3754–61. doi: 10.1200/JCO.2009.26.8722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.SHEMESH E, ANNUNZIATO RA, WEATHERLEY BD, et al. A randomized controlled trial of the safety and promise of cognitive-behavioral therapy using imaginal exposure in patients with posttraumatic stress disorder resulting from cardiovascular illness. J Clin Psychiatry. 2011;72(2):168–74. doi: 10.4088/JCP.09m05116blu. [DOI] [PubMed] [Google Scholar]
- 57.COHEN JA, MANNARINO AP. Psychotherapeutic options for traumatized children. Curr Opin Pediatr. 2010;22(5):605–9. doi: 10.1097/MOP.0b013e32833e14a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.BREWIN CR. Systematic review of screening instruments for adults at risk of PTSD. J Traum Stress. 2005;18(1):53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- 59.ELHAI JD, GRAY MJ, KASHDAN TB, FRANKLIN CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects?: A survey of traumatic stress professionals. J Traum Stress. 2005;18(5):541–545. doi: 10.1002/jts.20062. [DOI] [PubMed] [Google Scholar]
- 60.HAWKINS SS, RADCLIFFE J. Current measures of PTSD for children and adolescents. J Pediatr Psychol. 2006;31(4):420–430. doi: 10.1093/jpepsy/jsj039. [DOI] [PubMed] [Google Scholar]
- 61.TRICKEY D, SIDDAWAY AP, MEISER-STEDMAN R, SERPELL L, FIELD AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psych Rev. 2012;32(2):122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 62.BREWIN CR, ANDREWS B, VALENTINE JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. JCCP. 2000;68(5):748. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 63.OZER EJ, BEST SR, LIPSEY TL, WEISS DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Trauma. 2008;S(1):3–36. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.