Abstract
Objective
To evaluate the association between adverse family experiences (AFEs) during childhood and adolescent obesity and to determine populations at highest risk for adverse family experiences.
Methods
Cross sectional analysis of the 2011-2012 National Survey of Children’s Health, including children ages 10-17. Weighted estimates of 31,258,575 children were based on interviews with 42,239 caregivers. Caregiver-report of 9 psychosocial risk factors measured AFEs during childhood. Adolescent overweight and obesity were derived by caregiver-report of child height and weight.
Results
Nearly one-third (30.5%) of children had experienced ≥2 AFEs, with geographic variation by state. The prevalence of obesity among children experiencing ≥2 AFEs was 20.4%, compared with 12.5% among children with 0 AFEs. Adjusted survey regression models controlled for child, parent, household, and neighborhood characteristics. Children with ≥ 2 AFEs in childhood were more likely to be obese (AOR 1.8; 95% CI 1.47, 2.17; p<0.001) than those with no AFEs, with Non-Hispanic, White children most affected.
Conclusions
Adolescents in this national sample who were exposed to greater numbers of adverse family experiences in childhood also had higher rates of overweight and obesity. Geographic variation and differential associations based on race/ethnicity identify children at greatest risk.
Keywords: Pediatric Obesity, Family Issues, Stress
Introduction
For decades our society has recognized the adverse health consequences of stress during childhood. In 1998 seminal work by Felitti et al. linked adverse childhood experiences (ACEs) with a broad range of chronic diseases in adulthood, including obesity, mood disorders, ischemic heart disease, and cancer(1). These findings have been replicated in multiple contexts, and additional longitudinal studies have suggested that cumulative adverse experiences in childhood are related to higher risk of adverse adult health outcomes(2, 3). The negative health effects of adverse childhood experiences are not limited to adulthood. Growing evidence is mounting that cumulative stress in childhood is associated with adverse childhood health outcomes, including higher rates of attention deficit hyperactivity disorder (ADHD), asthma, special healthcare needs, and poor overall health(4, 5).
These findings are particularly relevant in the context of the childhood obesity epidemic, which currently affects 17% of children in the United States (6). Children who live in stressful home environments and are exposed to adverse experiences during childhood such as neglect, poor living conditions, financial insecurity, single parents, and low cognitive stimulation are more likely to develop obesity starting in childhood and continuing into adulthood (5, 7, 8, 9, 10, 11, 12). Recent data suggest that cumulative exposure to adverse childhood experiences can increase the risk of obesity as early as age 5 (13, 14). Moreover, traumatic experiences elevate a child’s risk for both developing obesity and the life-long morbidity associated with obesity (15, 16, 17). Given the pervasive and relatively static nature of childhood obesity trends, these long-recognized relationships between adverse experiences in childhood and obesity may be an under-utilized window into developing programs and policies to support the healthy growth of our children.
In 2011 and 2012 the Centers for Disease Control and Prevention conducted the National Survey of Children’s Health (NSCH), which included both a broad range of items that measured psychosocial determinants of health and a newly developed measure of adverse family experiences (AFEs) during childhood. This new measure incorporates an expanded range of AFEs, including individual, family, and neighborhood stressors. Specifically the new AFE measure adds 4 items to previously developed ACEs scales: 1) perceived discrimination, 2) death of a parent, 3) witness/victim of neighborhood violence, and 4) socioeconomic hardship. Recently published work by Bethell et al., demonstrated that children with higher scores on this newly developed composite AFE scale also have lower rates of school engagement and higher rates of chronic disease in adolescence (5). Therefore, this national survey provides an opportunity to characterize the current epidemiological associations between AFEs in childhood and childhood obesity, using a newly developed scale that incorporates a broad range of psychosocial stressors.
Adverse family experiences may or may not be mutable. Instead, the opportunity to improve health comes from how we support our children as they respond to adversity. This study aims to inform future programs and policies that support healthy childhood growth by using a comprehensive AFE measure to further characterize the scope and severity of child exposure to adverse family experiences. In addition, we will test associations between cumulative AFE exposure and overweight/obesity in childhood, controlling for a broad range of psychosocial and sociodemographic characteristics. Finally, we aim to inform targeted efforts at supporting healthy childhood growth by describing sub-populations of children for whom the association between AFEs and childhood overweight/obesity is particularly troubling. Specifically we will describe both the geographic variation in the frequency of AFEs and how race/ethnicity and gender modify the relationship between AFEs and childhood overweight/obesity.
Methods
This study is a secondary analysis of the 2011-2012 NSCH, which was funded by the United States Department of Health and Human Services, Health Resources and Services Administration, and the Maternal and Child Health Bureau. The Center for Disease Control and Prevention’s (CDC) National Center for Health Statistics conducted the survey with the purpose of assessing the physical and emotional health of children ages 0 to 17 years. Data were collected between February 28, 2011 and June 25, 2012. The survey administration methods described in this manuscript were taken from publicly available information about the conduct of the NSCH (18).
The survey consisted of a cross-sectional telephone survey of US households using list-assisted random-digit-dialing. A complex sampling design was used including stratification by state and sample type (landline or cell-phone). To determine eligibility, respondents were screened for residential status and the presence of at least one resident child ages 0 to 17 years. The index child was randomly selected from all household children who met inclusion criteria, and the index parent was a parent or guardian with knowledge of the health and health care of the index child.
A total of 847,881 households were screened, and of these 187,442 were eligible. The final sample included 95,677 detailed child-level interviews with at least 1,800 surveys in each of the 50 U.S. states and Washington D.C. The survey completion rate was 54.1% for the landline sample and 41.2% for the cell-phone sample. The survey was conducted in English, Spanish, Mandarin, Cantonese, Vietnamese, and Korean and when appropriate, conducted in the respondent’s language of choice. For the completed surveys, 68.6% of the respondents were mothers, 24.2% were fathers, and 7.2% were other relatives or guardians.
All data were parent-reported, and while parent report tends to overestimate obesity prevalence in younger children, it has shown good reliability in adolescents (19). The NSCH has been administered three separate times (with unique samples); in 2011-2012 there were several measures added to the questionnaire including more detailed information on children with special health care needs, additional information about a child’s access to preventive health care and health insurance, and a child’s exposure to AFEs. The median interview length was between 31 and 32 minutes. The Institutional Review Board of Vanderbilt University Medical Center, Nashville, Tennessee, approved this study. All data from the publicly available dataset are non-identifiable.
The primary predictor for the analyses is a composite measure of AFEs that captures psychosocial risk factors that affect children. A modified version of the Behavioral Risk Factor Surveillance System (BRFSS) Adverse Childhood Experiences (ACE) module was administered (20). Five items/experiences drawn from the original BRFSS included 1) divorce/separation of parent, 2) parent served time in jail, 3) witness to domestic violence, 4) lived with someone who was mentally ill or suicidal, and 5) lived with someone with alcohol/drug problem. Four additional items were added based on feedback from a technical expert panel that consisted of a representative group of experts with a range of expertise, including a period for public comment. These additional items included 1) perceived discrimination, 2) death of a parent, 3) witness/victim of neighborhood violence, and 4) socioeconomic hardship. The final version of the AFE survey is included in Table S1. Response options varied between a dichotomous “yes/no” or a 4 point Likert scale “Very Often” to “Never”. Items with a Likert response option were dichotomized so that a response of “somewhat often” or “very often” was coded as experiencing an AFE and a response of “Rarely” or “Never” was coded as not experiencing an AFE. AFEs were categorized based on previously published methods as a composite ordinal variable coded as 1) never having experienced an AFE 2) having experienced 1 AFE, or 3) having experienced 2 or more AFEs (5). The final scale had a high internal consistency with a Kuder and Richardson (KR20) coefficient (used for dichotomous items) of 0.67.
The primary outcomes for the analyses were 1) pediatric overweight and 2) pediatric obesity as measured by Body Mass Index for age percentile. Parent report of child height and weight was asked of children ages 10-17 years. Responses to questions about a child’s height or weight were not independently verified (e.g., measurement, health records, etc.) (20). Children were categorized as underweight (less than the 5th percentile), healthy weight (5th to 84th percentile), overweight (85th to 94th percentile), or obese (95th percentile or above) based on standardized growth curves published by the CDC (21, 22). For the primary analysis underweight and healthy weight were combined. We also ran a subsequent analysis excluding underweight children, and found nearly identical results (data not shown). Of note, the CDC uses a child’s age in months to calculate BMI, whereas the National Survey for Children’s Health reports age in years; consequently all children were assumed to be at the midpoint of their age-year for the calculation of BMI percentile (20). Because children with cerebral palsy are likely to have altered growth trajectories, any child with cerebral palsy was excluded from the analysis (23).
Covariates included in the final model were selected based on theoretical models published by the IOM on social determinants of health.(24) Because the primary predictor is a composite outcome of AFEs, individual covariates were not included if items on the AFE scale captured a similar construct. For example, we did not include income as a percent of the federal poverty level as a covariate because the first item in the AFE asks about how hard it is to get by on the family’s income. Covariates in the adjusted multivariable models used the coding scheme in the publicly available NSCH dataset, and are listed here with the referent group last (noted by [ref]). Covariates included child characteristics of age (continuous), gender (male vs. female [ref]), race/ethnicity (Hispanic; Non-Hispanic, Black; Non-Hispanic, Other vs. Non-Hispanic, White [ref]), depression (currently depressed vs. not currently depressed [ref]), hours of media time (<4 hours/day vs. ≥4 hours/day [ref]), physical activity (<4 days/week vs. ≥4 days/week [ref]) and child with special health care needs (yes vs. no [ref]). Parent/household characteristics included parent education (< High school; High school graduate vs. >High school [ref]), household employment (no vs. yes [ref]), family meals eaten together (≤3 days/week vs. ≥4 days/week [ref]), and region of residence (Midwest; South; West vs. Northeast [ref]). We excluded caregiver age and caregiver relationship in the final analysis due to a high percentage of missing data (9% and 26% respectively). Neighborhood social support was measured by neighborhood support (no vs. yes[ref]). Variables were coded based on recommendations from the National Survey of Children’s Health SAS Codebook (25). We elected to use these suggested categorizations to provide consistent reporting across studies. All analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC) and accounted for the sampling design used in the 2011-2012 NSCH.
Statistical Analysis
Weighted percentages were used to describe child, parent, family, and neighborhood characteristics of the sample. The Taylor series variance estimation method was used to calculate standard errors (26). Differences in the weighted proportions of selected characteristics at each level were assessed by overlap of 95% CI, and bivariate associations of selected characteristics with the outcome and exposure were tested using Wald χ2 statistics. Potential confounders were identified at p<0.10. We developed a proportional odds survey regression model to evaluate the association between AFEs and the categorical outcome of childhood obesity (normal weight vs. overweight vs. obese), adjusting for confounders. Tests for confounding, collinearity, and two factor interactions with AFE were conducted and adjusted odds ratios and 95% CI were reported for all the models. We a priori tested for gender and race/ethnicity as potential effect measure modifiers based on previous work that identified differential relationships between neighborhood characteristics and childhood overweight/obesity in earlier iterations of the NSCH (27). Respondents with missing, refused, or unknown values for variables in the final model were excluded from the multivariable analyses, which resulted in a final analytic sample of 41,616 (3.7% missing). In addition, to specifically address the potential confounding of income, the multivariable analyses were repeated excluding the measure of income as an AFE but including percent of federal poverty level as a covariate. The results of these analyses did not differ from the main model (results not shown). Of note, a child’s total AFE score was negatively correlated with family income as a percent of federal poverty level (spearman’s ρ= −0.33 p<0.001). All statistical tests were two-sided with a significance level of p<0.05. Results from the final model are presented as odds ratios and are subsequently stratified by both gender and race/ethnicity.
Results
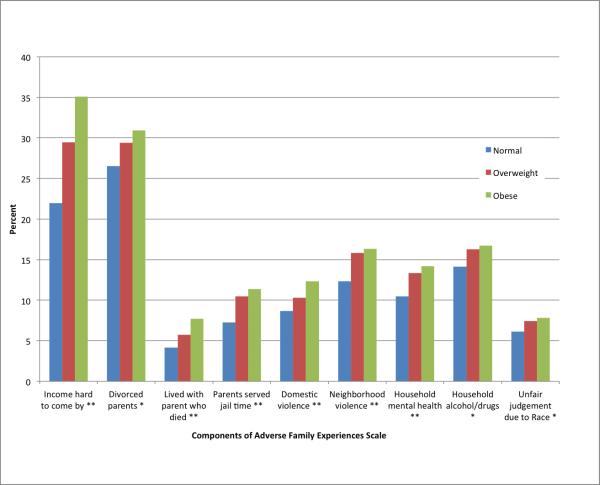
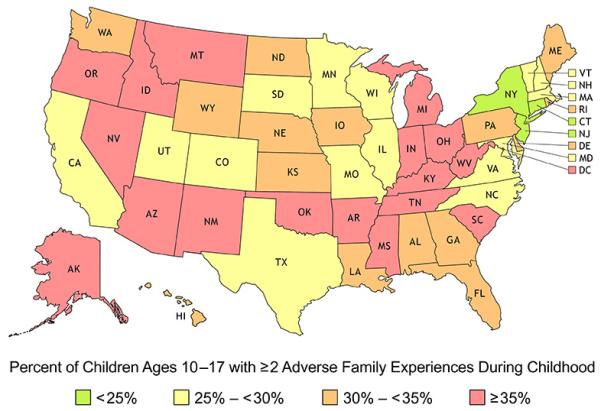
Both AFE and BMI measures were available from interviews conducted with 42,239 caregivers. Weighted estimates based on survey sampling are presented (weighted N=3,1258,575). The demographic characteristics of children ages 10-17 years who had complete data on BMI and the AFE scale are presented in Table 1. Of the children included in the analysis, 68.7% were normal weight, 15.6% were overweight, and 15.7% were obese. While 44.2% of children had never experienced an AFE, 25.3% experienced 1 AFE, 13.4% experienced 2 AFEs, 7.7% experienced 3 AFEs, and 9.5% experienced 4 or more AFEs. The geographic distribution and weighted percentages of AFEs by state are shown in Figure 1. The Northeast region has the lowest prevalence of AFE, while the South region had the highest prevalence: 14.4% of children in the northeast regions had ≥ 2 AFEs compared with 22.9% in the Midwest, 23.5 in the West, and 39.2% in the South. The most common AFEs experienced included financial instability and parent divorce, although there were non-trivial percentages of children in each of the AFE categories (Figure 2).
Table 1.
Demographic Characteristics and Pediatric Overweight/Obesity from the 2011-2012 National Survey of Children’s Health for children ages 10-17.
|
Overall
Sample |
Normal
Weight |
Overweight | Obese | ||
|---|---|---|---|---|---|
| N=43,239 | N= 30,653 | N=6,399 | N= 6,187 | ||
| Characteristics | % (SE) | % (SE) | % (SE) | % (SE) | |
| Adverse Family Experiences |
No adverse family experiences | 44.2 (0.5) | 47.3 (0.7) | 39.4 (1.4) | 35.2 (1.5) |
| 1 adverse family experience | 25.3 (0.5) | 25.2 (0.6) | 25.9 (1.3) | 25.2 (1.2) | |
| ≥2 adverse family experiences | 30.5 (0.5) | 27.5 (0.6) | 34.7 (1.4) | 39.5 (1.5) | |
| Demographics | |||||
| Child Gender | Girls | 48.6 (0.6) | 51.0 (0.7) | 46.5 (1.4) | 40.1 (1.5) |
| Child Age | Mean, SE | 13.6 (0.03) | 13.8 (0.03) | 13.3 (0.06) | 13.0 (0.07) |
| Child Race/ethnicity | Non-Hispanic, White | 56.7 (0.6) | 60.9 (0.7) | 51.3 (1.4) | 43.8 (1.4) |
| Hispanic | 19.3 (0.6) | 16.9 (0.6) | 22.3 (1.5) | 27.0 (1.6) | |
| Non-Hispanic, Black | 14.6 (0.4) | 12.4 (0.4) | 17.2 (1.1) | 21.5 (1.2) | |
| Non-Hispanic, Other | 9.4 (0.3) | 9.8 (0.4) | 9.1 (0.8) | 7.7 (0.7) | |
| Region of Residence | Northeast | 16.9 (0.3) | 17.5 (0.4) | 16.6 (0.9) | 14.6 (0.9) |
| Midwest | 22.2 (0.3) | 22.4 (0.4) | 21.6 (0.9) | 22.2 (1.0) | |
| South | 37.4 (0.5) | 36.0 (0.6) | 38.9 (1.4) | 41.8 (1.4) | |
| West | 23.5 (0.5) | 24.2 (0.6) | 22.9 (1.4) | 21.5 (1.5) | |
| Household Characteristics | |||||
| Household Education | Less than high school | 10.3 (0.4) | 7.9 (0.4) | 13.5 (1.2) | 17.9 (1.3) |
| High school graduate | 20.3 (0.5) | 17.6 (0.5) | 23.5 (1.2) | 29.1 (1.4) | |
| More than high school | 69.4 (0.6) | 74.5 (0.6) | 63.0 (1.5) | 53.0 (1.5) | |
| Eating meals together | Eat together < 4 days/week | 27.3 (0.5) | 28.4 (0.6) | 26.3 (1.2) | 23.2 (1.1) |
| Parent Unemployment | No job 50/52 weeks | 14.0 (0.4) | 12.0 (0.5) | 15.9 (1.1) | 20.8 (1.2) |
| Child Health and Health Behaviors | |||||
| Media time | ≥ 4 hours /day | 84.2 (0.4) | 15.5 (0.5) | 15.0 (1.0) | 18.4 (1.2) |
| E-devices in bedroom | Has TV, e-devices in the bedroom |
62.2 (0.5) | 61.6 (0.6) | 62.8 (1.4) | 64.6 (1.5) |
| Physical activity | Exercise ≥ 4 days/week | 62.7 (0.5) | 64.4 (0.6) | 62.2 (1.4) | 56.0 (1.5) |
| Child depression | Currently has depression | 3.7 (0.2) | 3.2 (0.3) | 3.6 (0.5) | 6.0 (0.7) |
| Child with special healthcare needs |
Child has special healthcare need |
25.4 (0.5) | 23.9 (0.6) | 27.2 (1.3) | 30.1 (1.3) |
| Neighborhood Social Support | |||||
| Neighborhood support | No neighborhood support | 15.6 (0.4) | 13.1 (0.4) | 19.4 (1.3) | 22.6 (1.4) |
Weighted estimates representing 31,258,575 children were based on interviews with 42,239 caregivers.
Weighted percentages are shown with accompanying standard errors (SE).
With the exception of e-devices in bedroom, all variables are significantly different by weight status at p<0.05 using Wald Χ2.
Figure 1.
Geographic Distribution of Adverse Family Experiences During Childhood from the 2011-2012 National Survey of Children’s Health for children ages 10-17. Weighted estimates representing 31,258,575 children were based on interviews with 42,239 caregivers.
Figure 2.
Distribution of each item on the Adverse Family Experiences scale for children ages 10-17 by child body mass index category from the 2011-2012 National Survey of Children’s Health. Wald χ2 p value for the bivariate association between each AFE component and adolescent BMI category. *p <0.05, ** p< 0.001.
Children who had experienced AFEs were more likely to be overweight or obese (Figure 2). Each of the individual AFE items had a significant unadjusted association with a higher prevalence of overweight and obesity (p <0.05 for all 9 items). The prevalence of obesity among children experiencing 2 or more AFEs was 20.4%, compared with 15.6% among children with 1 AFE, and 12.5% among those who reported no exposure to an AFE. Adjusting for child, parent, household, and neighborhood characteristics, children with 1 AFE vs. 0 AFEs had increased odds of being both overweight (AOR 1.3, 95% Confidence Interval [CI] 1.15, 1.52, p <0.001) and obese (AOR 1.3, 95% CI 1.12, 1.50, p<0.001). Similarly in adjusted multivariable models, children with 2 AFE vs. 0 AFEs had increased odds of being both overweight (AOR 1.8, 95% CI 1.49, 2.16, p <0.001) and obese (AOR 1.8, 95% CI 1.47, 2.17, p<0.001). There was a significant interaction between gender and AFEs (p=0.02 for child overweight, p=0.1 for child obesity) and child race/ethnicity and AFEs (p=0.03 for child overweight and p=0.003 for child obesity). The main results and stratified analyses are shown in Table 2.
Table 2.
The cumulative effect of adverse family experiences on Adolescent Overweight and Obesity from the 2011-2012 National Survey of Children’s Health. Results are given for the overall model, then stratified by gender and race/ethnicity†.
| Overweight | Obese | |||
|---|---|---|---|---|
|
| ||||
| Overall Model | ||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| 1 AFE vs. none | 1.3** | 1.15, 1.52 | 1.3** | 1.12, 1.50 |
| 2 AFEs vs. none | 1.8** | 1.49, 2.16 | 1.8** | 1.47, 2.17 |
|
| ||||
|
Stratified Analysis Comparing ≥ 2 AFEs vs. None for Each Sub-Group
| ||||
|
Stratified Analysis by Gender
| ||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Male | 1.3* | 1.07, 1.48 | 1.4** | 1.14, 1.59 |
| Female | 1.5** | 1.28, 1.84 | 1.5** | 1.25, 1.84 |
|
| ||||
|
Stratified Analysis by Child Race/Ethnicity
| ||||
| Hispanic | 1.1 | 0.79, 1.51 | 1.2 | 0.85, 1.68 |
| Non-Hispanic Black |
0.95 | 0.71, 1.28 | 1.0 | 0.72, 1.27 |
| Non-Hispanic Other | 1.8* | 1.26, 2.58 | 1.9** | 1.30, 2.74 |
| Non-Hispanic White |
1.7** | 1.44, 1.91 | 1.7** | 1.50, 2.00 |
Adjusted for child characteristics including age, gender, race/ethnicity, physical activity, media time, depression, and child with special healthcare needs; parent/household characteristics including education, employment status, eating family meals together, neighborhood support, and region.
p < 0.05,
p <0.001,
AFE=Adverse Family Experience
Discussion
Data from the 2011-2012 National Survey of Children’s Health demonstrate that adolescents ages 10-17 years in the United States who experience ≥2 adverse family experiences in childhood have 80% higher odds of obesity relative to children who do not experience such events. Importantly, this association persists even after controlling for other social determinants of health, including education, unemployment, race/ethnicity, neighborhood social support, and child health behaviors. These data identify a startling pattern that suggests AFEs in childhood are contributing to childhood obesity early in life, which has the potential to contribute to the already damaging trend of children with obesity becoming adults with obesity. These findings suggest that the association between AFEs and childhood obesity presents an opportunity to improve child health through the development of state or local social policies and research programs that specifically support stable home environments and resilience in our children.
The association of adverse family experiences and adolescent overweight/obesity is consistent with previous work that has shown adverse childhood experiences are associated with obesity in adulthood (1). Whereas those studies indicated that 4 AFEs increased the risk of adult obesity, here we report that ≥2 AFEs in childhood is associated with increased odds of child obesity. Our findings are also consistent with previous findings by Bethell et al., who identified associations between AFEs from the 2011-2012 NSCH and several health outcomes, using a more limited set of covariates (5). Data from the 2011-2012 National Survey of Children’s Health show a slightly lower percentage of childhood obesity than previously described. The most recent National Health and Nutrition Examination Survey (NHANES) indicated that between 17% and 20% of children between ages 6-19 were obese, whereas the percentage reported in this survey was closer to 16%. This points to the validity of the NSCH, with these parent report data approximating objectively measured national obesity prevalence. Finally, while there was a statistically significant interaction between gender and AFEs, the magnitude of the effect in stratified analyses did not appear to have clinically relevant implications.
This study highlights the unique contribution of AFEs to adolescent obesity, but that association cannot be viewed in isolation. In fact, many psychosocial determinants of health have been associated with higher rates of obesity (28). Perhaps most notably, poverty and low socioeconomic status are often cited as driving causes of pediatric obesity (29, 30, 31). While there is a modest correlation between poverty and AFEs (spearman’s ρ= −0.33), the current analysis suggests an association between AFEs and obesity independent of income, education, and employment. As our society develops programs and policies to support healthy childhood growth and reduce childhood obesity, a comprehensive view of psychosocial determinants of health will be necessary to address both mutable and treatable causes of obesity.
Both the widespread prevalence and the state-level variation in the prevalence of AFEs provide a new framework through which policy makers may wish to consider state-level interventions to support childhood health. Nearly 56% of adolescents in the United States have ever experienced ≥1 AFE. In the best circumstances one in six children are exposed to the cumulative stress of ≥2 AFEs. In the states with the highest prevalence of AFEs, that ratio is as high as one in three. Any speculation about the causative factors that are responsible for the state-level variation in AFE prevalence would be premature. Rather, this newly described geographic variation presents a pressing opportunity for future work to identify the determinants of adverse family experiences for children who are most affected by them. Even though there are not regional differences in the associations between AFEs and adolescent obesity, the state-level variation in AFE prevalence should inform policy development to prevent these AFEs and to support children who have already experienced them, especially in states that are hardest hit.
Stratified sub-group analyses show that children whose caregivers identify them as Non-Hispanic, White or Non-Hispanic, Other have the strongest association between AFEs and childhood obesity. Conversely children who are Hispanic or Non-Hispanic, Black do not have an association between AFE and childhood obesity. This finding was contrary to what we would have expected, and it is difficult to interpret this result, as there is a paucity of literature that directly addresses the role of AFEs in childhood in minority populations. Some of the best data come from the Chicago Longitudinal Study, which consists of 93% African American and 7% Hispanic individuals. This study demonstrated an association between adverse childhood experiences and a composite measure of adult self-reported health and quality of life, but did not assess childhood obesity (32). Therefore, future work should seek to identify both the mechanism by which AFEs are associated with childhood obesity with particular attention to how AFEs contribute to perceived stress in the households of traditionally underserved minorities.
Limitations of the study include that the data were cross sectional, so no causal inference can be drawn. Furthermore, the data were exclusively based on parent report, which may have been subject to multiple biases, including social desirability and recall bias. Another limitation is that child BMI data were only available on children between the ages of 10 and 17 years old, limiting our ability to draw conclusions about the preschool age, which is an extremely important period in childhood growth and development. Also, degree and duration of exposure to AFEs could not be measured, as the questions asked if a child had ever experienced the AFE and did not account for when that event happened. This is consistent with previous research that has measured adverse childhood experiences (1), but does provide an opportunity for further research to better characterize how the duration of exposure to AFEs relates to adverse childhood health outcomes. The survey was conducted using random digit dialing, so only people who have a phone could be included. This may have biased the sample to a demographic representative of a higher socioeconomic status, although the inclusion of cell-phones in this administration of the survey likely mitigated that bias as cell-phones are now nearly ubiquitous (33). Finally, this research did not address the mechanism by which AFEs are associated with pediatric obesity, and future research in this area is needed.
Conclusions
Adverse experiences during childhood have significant geographic distribution and contribute to the ongoing pediatric obesity epidemic. This should be considered in the development of a wide range of policies and research approaches to mitigate the occurrence of those experiences. Supporting the development of resilient responses may be an important component of ameliorating the unhealthy weight trajectory that affects so many of our children.
Supplementary Material
What’s Known on This Subject
Adverse childhood experiences have been linked to a wide range of poor health outcomes in childhood and adulthood.
Children who live in stressful home environments with financial insecurity and low cognitive stimulation are more likely to develop obesity as adults.
What This Study Adds
Using a newly developed metric, these data describe the current epidemiological link between adverse family experiences in childhood and adolescent obesity, adjusting for child, caregiver, household, and neighborhood factors.
The scope and geographic variation of adverse family experiences in childhood provides a new framework for shaping policy and practice to support a resilient generation of children.
Acknowledgments
Funding: Dr. Heerman’s time was supported by a K12 grant from the AHRQ (1K12HS022990), and Dr. Barkin’s time was supported by grant number 5P30DK092986 from the NIDDK.
Footnotes
Disclosure: The authors have no financial relationships or potential conflicts of interest relevant to this article to disclose.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Negl. 2010;34:454–464. doi: 10.1016/j.chiabu.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 3.Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: A systematic review. J Am Assoc Nurse Pract. 2015 doi: 10.1002/2327-6924.12215. [DOI] [PubMed] [Google Scholar]
- 4.Flaherty EG, Thompson R, Litrownik AJ, Zolotor AJ, Dubowitz H, Runyan DK, et al. Adverse childhood exposures and reported child health at age 12. Acad Pediatr. 2009;9:150–156. doi: 10.1016/j.acap.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health affairs. 2014;33:2106–2115. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Flegal KM. Prevalence of obesity in the United States. JAMA : the journal of the American Medical Association. 2014;312:189–190. doi: 10.1001/jama.2014.6228. [DOI] [PubMed] [Google Scholar]
- 7.Biehl A, Hovengen R, Groholt EK, Hjelmesaeth J, Strand BH, Meyer HE. Parental marital status and childhood overweight and obesity in Norway: a nationally representative cross-sectional study. BMJ open. 2014;4:e004502. doi: 10.1136/bmjopen-2013-004502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garasky S, Stewart SD, Gundersen C, Lohman BJ, Eisenmann JC. Family stressors and child obesity. Soc Sci Res. 2009;38:755–766. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann JC. Adolescent overweight and obesity: links to food insecurity and individual, maternal, and family stressors. J Adolesc Health. 2009;45:230–237. doi: 10.1016/j.jadohealth.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103:e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 11.Wilson SM, Sato AF. Stress and paediatric obesity: what we know and where to go. Stress Health. 2014;30:91–102. doi: 10.1002/smi.2501. [DOI] [PubMed] [Google Scholar]
- 12.Lissau I, Sorensen TI. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343:324–327. doi: 10.1016/s0140-6736(94)91163-0. [DOI] [PubMed] [Google Scholar]
- 13.Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Cumulative social risk and obesity in early childhood. Pediatrics. 2012;129:e1173–1179. doi: 10.1542/peds.2011-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Social and behavioral risk factors for obesity in early childhood. Journal of developmental and behavioral pediatrics : JDBP. 2013;34:549–556. doi: 10.1097/DBP.0b013e3182a509c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353:1802–1809. doi: 10.1056/NEJMoa044160. [DOI] [PubMed] [Google Scholar]
- 16.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. International journal of obesity. 2011;35:891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 17.Bauer NS, Gilbert AL, Carroll AE, Downs SM. Associations of early exposure to intimate partner violence and parental depression with subsequent mental health outcomes. JAMA pediatrics. 2013;167:341–347. doi: 10.1001/jamapediatrics.2013.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention NCfHS. State and Local Area Integrated Telephone Survey 2011-2012 National Survey of Children's Health Frequently Asked Questions April 2013. Available from: http://www.cdc.gov/nchs/slaits/nsch.htm.
- 19.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity (Silver Spring) 2009;17:1574–1580. doi: 10.1038/oby.2009.1. [DOI] [PubMed] [Google Scholar]
- 20.Child and Adolescent Health Measurement Initiative (CAHMI) In: 2011-2012 NSCH: Child Health Indicator and Subgroups SAS Codebook, Version 1.0. Data Resource Center for Child and Adolescent Health sbtMaCHB, editor. 2013. [Google Scholar]
- 21.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 22.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics Series 11, Data from the national health survey. 2002:1–190. [PubMed] [Google Scholar]
- 23.Day SM, Strauss DJ, Vachon PJ, Rosenbloom L, Shavelle RM, Wu YW. Growth patterns in a population of children and adolescents with cerebral palsy. Dev Med Child Neurol. 2007;49:167–171. doi: 10.1111/j.1469-8749.2007.00167.x. [DOI] [PubMed] [Google Scholar]
- 24.Medicine Io . Capturing Social and Behavioral Domains in Electronic Health Records: Phase 1. The National Academies Press; Washington, DC: 2014. [PubMed] [Google Scholar]
- 25.Child and Adolescent Health Measurement Initiative (CAHMI) 2011-2012 NSCH: Child Health Indicator and Subgroups SAS Codebook, Version 1.0. In: Health DRCfCaA, editor. 2011/12 National Survey of Children's Health. 2013. [Google Scholar]
- 26.Woodruff RS. Simple Method for Approximating Variance of a Complicated Estimate. J Am Stat Assoc. 1971;66:411–414. [Google Scholar]
- 27.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health affairs. 2010;29:503–512. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- 28.Stein D, Weinberger-Litman SL, Latzer Y. Psychosocial perspectives and the issue of prevention in childhood obesity. Front Public Health. 2014;2:104. doi: 10.3389/fpubh.2014.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Demment MM, Haas JD, Olson CM. Changes in family income status and the development of overweight and obesity from 2 to 15 years: a longitudinal study. BMC public health. 2014;14:417. doi: 10.1186/1471-2458-14-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee H, Andrew M, Gebremariam A, Lumeng JC, Lee JM. Longitudinal associations between poverty and obesity from birth through adolescence. American journal of public health. 2014;104:e70–76. doi: 10.2105/AJPH.2013.301806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nau C, Schwartz BS, Bandeen-Roche K, Liu A, Pollak J, Hirsch A, et al. Community socioeconomic deprivation and obesity trajectories in children using electronic health records. Obesity (Silver Spring) 2015;23:207–212. doi: 10.1002/oby.20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl. 2013;37:917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pew Research Center's Internet & American life Project [Accessed 4/9/15];April 17-May 19, 2013 Tracking Survey. Available at http://www.pewresearch.org/fact-tank/2013/06/06/cell-phone-ownership-hits-91-of-adults/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.