Abstract
Objective
Delay to hospital arrival limits acute stroke treatment. Use of emergency medical service (EMS) is key in ensuring timely stroke care. We aimed to identify low-EMS utilizing neighborhoods and to evaluate whether neighborhood-level factors were associated with (EMS) use.
Methods
We conducted a secondary analysis of data from the Brain Attack Surveillance in Corpus Christi (BASIC) project, a population-based stroke surveillance study of ischemic stroke and intracerebral hemorrhage cases presenting to emergency departments in Nueces County, Texas. The primary outcome was arrival by EMS. The primary exposures were neighborhood resident age, poverty, and violent crime. We estimated the association of neighborhood level factors with EMS use using hierarchical logistic regression, controlling for individual factors (stroke severity, ethnicity and age).
Results
During 2000-2009 there were 4004 identified strokes, with EMS use data available for 3474. Nearly half (49%) of stroke cases arrived by EMS. Adjusted stroke EMS utilization was lower in neighborhoods with higher family income (OR 0.86 95% CI 0.75-0.97) and a larger percentage of older adults (OR 0.70, 95% CI 0.56-0.89). Individual factors associated with stroke EMS use included white race (OR 1.41 95% CI 1.13-1.76) and older age (OR 1.36 per 10-year age increment, 95% CI 1.27-1.46). The proportion of neighborhood stroke cases arriving by EMS ranged from 17% to 71%. The fully adjusted model only explained 0.3% (95% CI 0-1.1%) of neighborhood EMS stroke use variance, indicating that individual factors are more strongly associated with stroke EMS use than neighborhood factors.
Conclusions
While some neighborhood-level factors were associated with EMS use, patient-level factors explained nearly all variability in stroke EMS use. In this community, strategies to increase EMS use should target individuals rather than specific neighborhoods.
Introduction
Background
Stroke is a leading cause of long-term disability in adults and is associated with substantial direct and indirect costs.[1, 2] The stroke “chain of survival” from symptom onset to hospital care has been well described as a key part of optimal stroke management.[3] However, delays along the chain occur for the majority of acute stroke patients.[3] This limits the recovery potential for many stroke victims because earlier treatment of stroke is associated with better outcomes.[4] Arrival to the emergency department (ED) via emergency medical services (EMS) is part of the stroke chain of survival and has been associated with more rapid care and greater access to tissue plasminogen activator.[5-8] Yet, over half of stroke patients fail to use EMS for acute stroke.[9]
Importance
Prior studies show that the neighborhood characteristics may contribute to the development or care of a disease. For example, cardiac arrest victims in economically disadvantaged neighborhoods are less likely to receive bystander cardiopulmonary resuscitation.[10] Residents of higher crime neighborhood may be more likely to use EMS given the frequent need to call 911 to report incidents. In addition, people in higher crime neighborhood may also have increased thresholds for seeking healthcare due to their desire to stay indoors.
Neighborhood characteristics may also potentially influence citizen EMS use. Although individual factors influencing EMS use for acute stroke are known, the associations of neighborhood factors with stroke care and outcomes are less well understood.[11] The identification of vulnerable neighborhoods could enable the delivery of targeted interventions to improve EMS use for stroke. Prior efforts have evaluated county or metropolitan level interventions to improve stroke awareness and care.[12-14] Identifying “high-yield” neighborhoods for targeted interventions could increase EMS use for stroke, with potential for more rapid reperfusion and improved patient outcomes.[15]
Goals of this Investigation
The objective of this investigation was to assess whether neighborhood factors are associated with the use of EMS for acute stroke. We also sought to determine if neighborhood factors were associated with ED arrival within three hours of stroke onset.
Methods
Study Design
We conducted a secondary analysis of data from the Brain Attack Surveillance in Corpus Christi (BASIC) project, a population-based stroke surveillance study.[16, 17] The BASIC project was approved by the University of Michigan Institutional Review Board (IRB), along with the IRBs of engaged hospitals in Nueces County, Texas. Participants or proxies provided written informed consent for interview procedures; a waiver of written informed consent was granted by all relevant entities for medical record review and screening.
Setting
BASIC identifies stroke cases in Nueces County, Texas. The majority of the county population resides in Corpus Christi, a Gulf Coast city with an approximate population of 305,000. The community is primarily urban and bi-ethnic, with approximately 60% Mexican American residents. Approximately 15% of city residents live in poverty.[18] Mexican-American residents are typically second or third generation. Acute stroke care in Nueces County is relatively self-contained; Houston and San Antonio are each over 120 miles away and the surrounding counties are sparsely populated, so that emergency medical care remains in the city. During the study period there were six full service, hospital-based adult emergency departments; no freestanding emergency departments were in operation. There were also no designated primary stroke centers in the community, and thus EMS personnel customarily transported suspected stroke cases to the nearest ED. Within the city of Corpus Christi, the primary EMS agency is the Corpus Christi Fire Department which runs eight paramedic units and responds to all 911 calls for medical complaints.
Participants
BASIC has prospectively identified all cases of ischemic stroke in Nueces County, Texas since 2000. BASIC uses several methods surveillance strategies to identify potential stroke cases. Active surveillance methods include the daily review of ED arrival and hospital admission logs for relevant presenting complaints such as weakness (ED). Passive surveillance methods include review of stroke diagnosis codes from all hospitalizations. BASIC methodology for identifying stroke patients has been validated.[19, 20]
For this study, we included all ischemic stroke and intracerebral hemorrhage (ICH) patients identified in the BASIC study between 2000-2009.[16, 19] Patients with transient ischemic attack or subarachnoid hemorrhage were excluded as they were not captured by BASIC . We excluded patients residing in a nursing home at the time of stroke as our focus was on residential neighborhood exposures. We included only the first ischemic stroke or ICH during the study period for any individual.
Data Sources and Measurements
Trained abstractors collected individual-level information from source documents by trained abstractors using standard procedures. The project manager and study physicians check data quality. Procedures are in place for hierarchy of conflicting source documents (i.e. time of onset from neurology note given precedence over nursing triage note). Repeat review occurs for a proportion of charts to facilitate ongoing quality assurance.
For the neighborhood characteristics, we used summary statistics from the 2000 U.S. Census data for each patient home residence. We obtained home address from the medical record. The Corpus Christi Police Department provided data regarding violent crimes for the year 2008.
Outcomes
The primary outcome was arrival to hospital via EMS. BASIC determined mode of arrival through review of ED triage records. Because mode of arrival was not collected by BASIC in 2008 and 2009, we excluded 475 patients from this time period. The secondary outcome was delayed arrival to the hospital, defined as arrival greater than three hours after witnessed stroke onset or time last known well. We have previously described procedures for determining arrival times in the BASIC project.[21]
Exposure Variables
Neighborhood level
Neighborhood level variables examined in the study included violent crime, proportion older adults within each neighborhood, proportion of Hispanic residents within each neighborhood, and median neighborhood income. We obtained the latter four items from the 2000 Census master file. We included neighborhood violent crime rate because prior fieldwork in Hispanic neighborhoods suggest higher 911 utilization in these communities.[22] While the Hispanic population of Corpus Christi is nearly all Mexican American, the census collects whether respondents are Hispanic, therefore neighborhoods are described as “proportion Hispanic” and individuals are described as “Mexican-American.” We included the neighborhood variables that had both a plausible social influence and a plausible relationship with EMS use for stroke. Larger amounts of older adults within a neighborhood may create a greater familiarity with stroke, since the incidence of stroke increases with age. Mexican American ethnicity is associated with lower EMS use in previous studies. We chose median income instead of proportion with poverty, or neighborhood level of education, as it is intuitively translatable within the U.S. population. We also examined the correlation between crime and median income and found variation (see methodological appendix), notably that some impoverished neighborhoods had higher crime but many did not.
Individual Level
Individual level variables examined in this study included demographics, ethnicity, and characeristics of stroke presentation. Ethnicity (non-Hispanic white and Mexican-American), sex, history of prior stroke/TIA, other past medical history, age and initial stroke severity were abstracted from the medical record using the standardized methods of BASIC.[16, 20] In this community, self-reported ethnicity in the medical record and by interview agree highly (kappa=0.94).[20] We characterized stroke severity using the National Institutes of Health Stroke Scale (NIHSS).[23] Stroke type (ICH versus ischemic stroke) was determined by BASIC project neurologists. Level of education was obtained from an interview with patients or proxies. BASIC used a sampling approach and only a subset of patients had interviews-therefore we used a predictive model based on patient and neighborhood characteristics to impute individual level education. (See methodological appendix for details).
Data Analysis
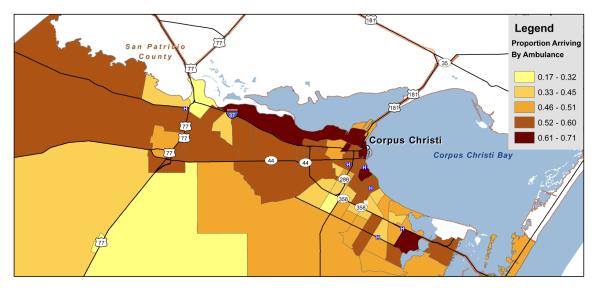
We calculated descriptive statistics of the study population with means and standard deviations or proportions as appropriate. Using a spatial distribution map of census tracts, we graphically depicted the proportion of patients arriving by EMS within each census tract using ArcGIS.
To address our primary aim to describe the relationship between neighborhood-level factors and EMS use, we fitted several models. A priori, we selected individual stroke factors known to be highly associated with either stroke outcome or EMS use to be included in the models. In addition, we selected neighborhood factors that we hypothesized could be related to EMS use including neighborhood socioeconomic status, age, and crime information. Crime conceivably could have exerted influence in either direction (afraid to go out versus very familiar with calling 911; alternatively residents of a higher crime neighborhood might not want to be perceived as requesting police or governmental EMS presence).[22] Some age, economic, and ethnic groups have been more or less likely to use EMS in previous studies.[9, 11] We did not include race in our models as residents of Nueces County are predominantly non-Hispanic white or Mexican-American. In addition, health insurance was common within the BASIC cohort and we did not believe it would strongly influence EMS use.
We examined three nested models to examine 1) the variability in stroke EMS use across neighborhoods, 2) the associations between neighborhood characteristics and stroke EMS use, and 3) individual level covariates. We considered only main effects, as we did not have strong reasons to suspect interactions. We fit these models sequentially to determine the characteristics (neighborhood versus individual) explaining observed variability.
First, we fit a binary logistic regression model with arrival by EMS (yes versus no) as the dependent variable. We fit the model with a random intercept for census tract and no covariate parameters; this allowed estimation of the expected proportion of EMS use within census tracts and described the variation between neighborhood prior to adjusting for any individual or neighborhood level factors. Second, we added neighborhood level covariates (proportion older adult, proportion Hispanic, median household income, and violent crime rate) to the model. Finally, we added individual characteristics (stroke severity, age, sex, ethnicity, history of stroke/TIA, ICH, and years of education) to the model. In each of these models, we calculated the posterior estimation for the expected proportion of stroke patients using EMS within each census tract, along with 95% credible intervals (a range of plausible values for a parameter estimate, similar to a frequentist confidence interval that represents the range of expected values if repeated experiments estimated a parameter). We also calculated the intra-class correlation coefficient to estimate how much variability in the relationship between the outcomes and the predictors was explained by within-neighborhood correlation versus the other reasons for variability (differences across patients and random variation). We used a similar approach for the outcome arrival within three hours of stroke onset.
A secondary goal of this project was to identify neighborhoods that were using EMS less, after adjusting for variation that was attributable to neighborhood and individual stroke characteristics. This approach potentially identifies hotspots of low EMS utilization that could be amenable to interventions or further study. This approach would account for a neighborhood that had less severe strokes (who were thus less likely to use EMS), therefore identifying neighborhoods with lower utilization after adjusting for the strokes presentation characteristics that influence EMS use. (See methodological appendix for further details regarding modeling and statistics.)
We carried out all analyses using SAS 9.2, R (version 2.14.1) and WINBugs.
Results
Characteristics of cohort
From Jan 1,2000 – Dec 31, 2009, BASIC identified a total of 4004 ICH and ischemic strokes presenting to an ED. The characteristics of the overall group are representative of stroke patients from the community with 50% of stroke patients female with a mean age of 70 (Table 1). A total of 530 cases had missing data for EMS use. From the 3474 remaining patients, a total of 1655 (47.6%) arrived by EMS. We excluded an additional 121 cases lacking geocodes and 263 occurring in census tracts outside the city of Corpus Christi.
Table 1.
Characteristics of All Nueces County Stroke Patients 2000-2009
Includes 4004 patients
| Individual | Overall Mean or Proportion |
SD or N | N Missing |
|---|---|---|---|
| Age | 70.1 | 12.8 | 0 |
| NIHSS – (median [IQR]) | 4 | [2 - 8] | 6 |
| Year of Education – (median [IQR]) | 12 | [8-14] | 1931 |
| Female | 49.7% | 1989 | 0 |
| Race/Ethnicity | 6 | ||
| Non-Hispanic White | 40.8% | 1633 | |
| Mexican American | 52.3% | 2103 | |
| African American | 5.6% | 225 | |
| Other / Unknown | 1.3% | 13 | |
| Ischemic Stroke | 85.1% | 3408 | 0 |
| Intracerebral Hemorrhage | 14.9% | 596 | 0 |
| No Health Insurance | 11.8% | 471 | 13 |
| Prior History of Stroke/TIA | 28.8% | 2853 | 0 |
| Tobacco Use | 19.6% | 785 | 90 |
| History of Hypertension | 76.3% | 3055 | 10 |
| History of High Cholesterol | 29.1% | 1166 | 10 |
| History of Coronary Artery Disease | 31.5% | 1262 | 10 |
| History of Atrial Fibrillation | 12.1% | 486 | 10 |
| Neighborhood (N=57) | |||
| Proportion of population older than 65 | 0.12 | 0.04 | |
| Median Neighborhood Income | 34322 | 13043 | |
| Proportion of population Mexican American | 0.6 | 0.24 |
SD= Standard Deviation, NIHSS= National Institutes of Health Stroke Scale, IQR=Interquartile range, TIA= Transient Ischemic Attack.
Main outcome results: arrival by EMS
There was wide variation in EMS use for acute stroke by neighborhood (Figure 1). The proportion of each neighborhood’s stroke patients using EMS ranged from 0.17 to 0.71. For all three hierarchical logistic regression models models the intra-class correlation coefficent (ICC) for the random intercept neighborhood variable was low (0.002 – 0.004) indicating that, despite the notable differences in the spatial distribution maps, only 0.3% of the variation in EMS use was explained by the census tract level, with the remaining variation due to individual level factors or random variation. In the final model (Table 2), adjusting for individual and tract level covariates, lower age, lower stroke severity, Mexican American ethnicity, ischemic stroke (versus ICH), and female gender were associated with decreased odds of EMS use. In this final model, the neighborhood level covariates of median family income and percent of census tract greater than age 65 were associated with lower odds of EMS use.
Figure 1.
Proportion of Stroke Presentations Arriving By Ambulance By Census Tract
Spatial distribution of stroke patients arriving to ED by ambulance by neighborhood (census tract). All shaded areas comprise Nueces County, Texas.
Table 2.
Hierarchical Models of Neighborhood and Individual Factors Associated with EMS Stroke Care
Includes n=2906 patients.
| Adjusted for Neighborhood Factors |
Adjusted for Neighborhood and Individual Factors |
|||||
|---|---|---|---|---|---|---|
| Individual Level | OR | 95% CIL | 95% CIU | |||
| NIHSS(per 5 point increase) | 2.18 | 1.98 | 2.40 | |||
| Age(per 10 year increase) | 1.36 | 1.27 | 1.46 | |||
| NHW versus MA | 1.41 | 1.13 | 1.76 | |||
| ICH versus ischemic | 2.37 | 1.83 | 3.08 | |||
| Male versus female | 1.20 | 1.01 | 1.41 | |||
| History of stroke versus no prior | 1.18 | 0.98 | 1.40 | |||
| Years of education | 1.00 | 0.98 | 1.03 | |||
| Neighborhood Level | OR | 95% CIL | 95% CIU | OR | 95% CIL | 95% CIU |
| Median Family Income (per $10,000 increase) | 0.93 | 0.82 | 1.04 | 0.86 | 0.75 | 0.97 |
| Percent of Census Tract Hispanic (10% increase) | 0.96 | 0.90 | 1.01 | 0.97 | 0.90 | 1.03 |
| Violent Crime (per additional crime per 10 residents) | 2.35 | 0.86 | 6.58 | 2.58 | 0.86 | 7.79 |
| Percent of Census Tract Age > 65 (10 % increase) | 0.88 | 0.71 | 1.11 | 0.70 | 0.56 | 0.89 |
Results of hierarchical logistic models for individual and neighborhood level covariates. NIHSS = National Institutes of Health Stroke Scale; NHW = non-Hispanic white; MA = Mexican American; ICH = Intracerebral hemorrhage; OR = Odds ratio; CIL = lower bound of 95% credible interval; CIU = upper bound of 95% credible interval. The intraclass correlation coefficients were 0.004 (intercept only), 0.002 (neighborhood only model), and 0.003 (neighborhood and individual model).
Secondary outcome results: arrival within three hours
We included 3664 stroke patients with data for onset to ED arrival time and 31.7% of included patients arrived to the ED within three hours of time last known to be well. While the ICC was 0.17 in the unadjusted random intercept model, it was 0.002 in the neighborhood- and fully-adjusted models indicating that only 0.2% of the variability in early arrival was explained by neighborhood factors. In the models evaluating arrival within three hours of stroke onset, individual level variables of age, stroke severity, and ICH were also associated with earlier arrival (Table 3), though non-Hispanic white and male sex were not. None of the neighborhood level covariates were significant.
Table 3.
Hierarchical Models of Neighborhood and Individual Factors Associated with Emergency Department Arrival Within Three Hours of Stroke Onset
Includes n=3174 patients.
| Adjusted for Neighborhood Factors |
Adjusted for Neighborhood and Individual Factors |
|||||
|---|---|---|---|---|---|---|
| Individual Level | OR | 95% CIL | 95% CIU | |||
| NIHSS(per 5 point increase) | 1.14 | 1.08 | 1.19 | |||
| Age(per 10 year increase) | 1.09 | 1.02 | 1.16 | |||
| NHW versus MA | 1.10 | 0.91 | 1.37 | |||
| ICH versus ischemic | 2.01 | 1.63 | 2.52 | |||
| Male versus female | 1.07 | 0.92 | 1.24 | |||
| History of stroke versus no prior | 1.13 | 0.95 | 1.33 | |||
| Years of education | 1.02 | 1.00 | 1.04 | |||
| Neighborhood Level | OR | 95% CIL | 95% CIU | OR | 95% CIL | 95% CIU |
| Median Family Income (per $10,000 increase) | 0.95 | 0.84 | 1.06 | 0.92 | 0.81 | 1.03 |
| Percent of Census Tract Hispanic (10% increase) | 0.97 | 0.92 | 1.03 | 0.98 | 0.93 | 1.04 |
| Violent Crime (per additional crime per 10 residents) | 0.51 | 0.20 | 1.36 | 0.46 | 0.15 | 1.28 |
| Percent of Census Tract Age > 65 (10 % increase) | 1.07 | 0.87 | 1.35 | 1.02 | 0.80 | 1.28 |
Results of hierarchical logistic models for individual and neighborhood level covariates. NIHSS = National Institutes of Health Stroke Scale; NHW = non-Hispanic white; MA = Mexican American; ICH = Intracerebral hemorrhage; OR = Odds ratio; CIL = lower bound of 95% credible interval; CIU = upper bound of 95% credible interval. The intraclass correlation coefficients were 0.167 (intercept only), 0.002 (neighborhood only model), and 0.002 (neighborhood and individual model).
Hotspot evaluation: identification of neighborhoods with low EMS utilization
In our hotspot evaluation, we examined how the rankings of neighborhoods changed after we calculated model-adjusted estimates for EMS within each neighborhood. Ten census tracts were identified as having the lowest observed use of EMS. Only three tracts in the ten lowest observed utilizers of EMS were among the tracts with the lowest model-based predicted EMS use, after adjusting for individual and neighborhood level covariates (See Appendix Table). In addition, the range of the probability of using EMS in the lowest compared to highest census tract was narrowed after adjustment (observed range 0.1 to 0.86 versus model-based predicted range 0.28 to 0.52).
Limitations
This work has important limitations. First, we only studied one community. Other communities may have different facilitators, barriers, patterns, and cultural factors related to EMS use for acute stroke. Second, this work did not focus on specific patient-level facilitators and barriers to EMS use.[11] Third, BASIC abstracted certain data elements from the medical record and some opportunity for misclassification may exist. In this investigation, it is unlikely that the distribution of such errors was related to EMS use or neighborhood – and as such should not have a significant impact on our current findings. We did not have information on whether the stroke onset was witnessed. We did not have information on patient living status (alone versus with family). We did not include time of onset in the models. This community did not have many stroke patients who were not Mexican American or non-Hispanic White; therefore, we have limited insights into these important groups. We had partial information on individual level education on a large proportion of our cohort, limiting our ability to fully evaluate this important factor. On the other hand, the observed distribution for education was narrow with a median of high school – it is likely that this variable would not vary enough in this population to be informative within this study design. In addition, BASIC excludes stroke mimics that may prompt EMS activation since only validated strokes are retained in the database. Finally, we assigned cases into neighborhoods by home address. The onset of stroke may have occurred at work or other locations.
Discussion
The growing availability of geospatial disease information is an important resource for public health and epidemiology, both in efforts to improve the health of communities and in understanding risk factors for disease.[24, 25] Our study shows that such analyses must be adjusted for important confounding variables. We found that observed geographic variations in EMS use across neighborhoods were best explained by random variation in the distribution of strokes across the community and the individual characteristics of stroke patients. Even though our spatial distribution maps suggested “hotspots” of EMS underuse, the adjusted analyses found that neighborhood actually contributed very little to the variation in EMS use. Furthermore, the neighborhoods exhibiting low EMS use could be reclassified to average EMS use communities after adjusting for individual and neighborhood factors. Low EMS utilizing neighborhoods frequently had fewer cases with severe stroke, ICH and other individual level factors associated with higher EMS use. Some prior work has demonstrated that lower neighborhood socioeconomic status is associated with a small increase in stroke severity.[26]
Our current findings may provide some explanation of the neutral effects observed in previous location based interventions.[12-14] Boden-Albala et al. used a culturally sensitive interactive educational program in Northern Manhattan to hasten stroke care, but did not detect a change in behavior. In addition, Morgenstern et al focused on middle school children and their parents in Corpus Christi was able to influence teen behavior but not the adults. Tadros et al. conducted a county wide program in West Virginia and their study did not improve knowledge of the need to activate EMS for stroke. To advance this field, further investigation should focus on how stroke severity relates to living location; namely if more severe strokes are induced by neighborhood factors such as crime, pollution, access to food, social cohesion or other characteristics. In addition, interventions in this community that focus on groups (independent of living location) that appear less likely to use EMS may have a greater likelihood of success.
While we observed large neighborhood differences in stroke EMS use, little of the variability was explained by neighborhood factors. Rather, individual-level factors explained much of the variation in EMS use for acute stroke. Across neighborhoods, we found that lower household income was associated with increased use of EMS for acute stroke. This finding of lower median income being associated with EMS use suggests that more disadvantaged populations, despite potentially having a lower level of education and stroke awareness[27], more frequently use EMS to access acute treatment for stroke. Additionally, such individuals may have fewer alternative transportation options. The borderline association between proximate violent crime and increased EMS use suggests that individuals living within high-crime neighborhoods may be more accustomed to accessing the emergency dispatch system through 911, although other potential explanations for this relationship are also plausible including greater incidence and severity of stroke in areas of higher violent crime.[28] We found that an increased number of older adults within a neighborhood tended to be associated with a decreased probability of using EMS for stroke, whereas for individual patients EMS use was associated with increasing age. Neighborhoods with a higher density of older adults may have more individuals living alone, providing less opportunity for recognition of symptoms and activation of EMS by a bystander.[29, 30]
Select studies highlight the potential influence of neighborhood factors upon EMS utilization and care. For example, in a registry based study of out of hospital cardiac arrest patients in sites across the United States, Sasson et al. found that impoverished or minority neighborhoods exhibited lower rates of bystander CPR.[31] Treno, et al. showed that neighborhood-focused alcohol abuse intervention could result in reduced crime, EMS use, and injury.[32] In contrast, our study shows neighborhood factors do not influence stroke EMS use or care as strongly as individual factors do – particularly severity. Initiatives to improve stroke EMS use should focus on individual factors such as encouraging better recognition and prompt action for milder stroke symptoms. One method to accomplish this would be to use census data to find neighborhoods with high proportions of individuals who would have low expected EMS use based on models that incorporate the likely contributions of important individual and neighborhood level factors, in contrast to simply looking at neighborhoods with low observed EMS use that is likely to be more attributable to random spatial variation in stroke severity.
An important observation in our study was that despite higher EMS use, stroke patients in the lower income neighborhoods did not arrive earlier at the ED after adjusting for individual- and neighborhood-level factors. One potential explanation would be the combined contribution of lack of education regarding stroke awareness and/or lack of transportation resources. A family may not know how to respond to a stroke initially, leading to a delay in EMS activation. The potential exists for other delays in the time between symptom onset and ED arrival by the patient, although some past work suggested that delays after EMS activation were minimal but measureable for low-income neighborhoods.[33] Another potential explanation is that low-EMS utilizing neighborhoods may have more cases who are younger, female, and Mexican American. Such clustering of individuals who have a lower odds of EMS use overall, would decrease our ability to detect a significant, small neighborhood effect. Additional research should explore the reasons for delayed presentation of patients from low-income neighborhoods in spite of EMS use.
Conclusion
In summary, in this study neighborhood variations in stroke EMS use were small after adjusting for differences in patient level factors. Patient factors accounted for a substantial amount of variation in EMS use and explained the low observed rates of EMS use in many neighborhoods. Interventions to improve stoke EMS use should focus on individuals, not neighborhoods. groups less likely to use EMS such as younger adults, women, and Mexican Americans, and it may be of high yield to focus such interventions on neighborhoods with high proportions of individuals at risk for low EMS.
Supplementary Material
Acknowledgments
Disclosures: Grant funding: (Significant) NINDS,FDA, AHRQ; Expert Witness: Modest and unrelated);
Grant funding: (Significant) NIA; Consultant (modest)
Grant funding: (significant) NIDCD
Grant funding: (significant) NIA
Grant funding: (significant) NINDS
Disclosures: Grant Funding: NIH (Significant, related), St Jude Medical Corp (Significant and unrelated), Expert witness (Modest and unrelated)
Grant funding: (significant) NINDS (related)
Appendix Table.
Observed and predicted probability of Ambulance Arrival by neighborhood
| Observed(raw) | Observed Rank |
Random Intercept Only Model Post. Pred. Probability |
Intercept Only Model Rank |
95% CIL | 95% CIU | Intercept Plus Tract Covariate Model Post. Pred. Probability |
Intercept Plus Tract Covariate Model Rank |
95% CIL | 95% CIU | Fully Adjusted Model Post. Pred. Probability |
Full Model Rank |
95% CIL | 95% CIU |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.10 | 1 | 0.49 | 9 | 0.43 | 0.54 | 0.48 | 18 | 0.42 | 0.54 | 0.47 | 43 | 0.40 | 0.54 |
| 0.32 | 2 | 0.49 | 4 | 0.42 | 0.53 | 0.48 | 13 | 0.42 | 0.52 | 0.41 | 17 | 0.34 | 0.47 |
| 0.33 | 3 | 0.49 | 10 | 0.42 | 0.54 | 0.46 | 3 | 0.41 | 0.52 | 0.43 | 22 | 0.37 | 0.49 |
| 0.37 | 4 | 0.48 | 2 | 0.41 | 0.53 | 0.49 | 24 | 0.43 | 0.53 | 0.43 | 23 | 0.36 | 0.49 |
| 0.39 | 5 | 0.48 | 1 | 0.41 | 0.51 | 0.45 | 1 | 0.39 | 0.50 | 0.38 | 8 | 0.31 | 0.45 |
| 0.40 | 6 | 0.49 | 7 | 0.43 | 0.53 | 0.47 | 8 | 0.42 | 0.54 | 0.35 | 2 | 0.27 | 0.42 |
| 0.41 | 7 | 0.49 | 5 | 0.42 | 0.53 | 0.47 | 6 | 0.42 | 0.52 | 0.41 | 18 | 0.35 | 0.48 |
| 0.42 | 8 | 0.49 | 14 | 0.44 | 0.54 | 0.47 | 5 | 0.40 | 0.53 | 0.36 | 3 | 0.29 | 0.44 |
| 0.42 | 9 | 0.48 | 3 | 0.42 | 0.53 | 0.48 | 15 | 0.43 | 0.52 | 0.46 | 35 | 0.39 | 0.52 |
| 0.42 | 10 | 0.49 | 8 | 0.43 | 0.53 | 0.47 | 7 | 0.42 | 0.52 | 0.44 | 29 | 0.38 | 0.50 |
| 0.42 | 11 | 0.49 | 11 | 0.43 | 0.54 | 0.48 | 14 | 0.43 | 0.52 | 0.40 | 11 | 0.34 | 0.46 |
| 0.43 | 12 | 0.49 | 6 | 0.43 | 0.53 | 0.48 | 16 | 0.43 | 0.52 | 0.40 | 15 | 0.35 | 0.46 |
| 0.44 | 13 | 0.49 | 12 | 0.43 | 0.53 | 0.51 | 39 | 0.45 | 0.55 | 0.46 | 36 | 0.38 | 0.53 |
| 0.44 | 14 | 0.49 | 13 | 0.44 | 0.53 | 0.47 | 10 | 0.43 | 0.52 | 0.44 | 30 | 0.38 | 0.50 |
| 0.45 | 15 | 0.49 | 15 | 0.44 | 0.54 | 0.46 | 2 | 0.40 | 0.51 | 0.42 | 21 | 0.35 | 0.48 |
| 0.45 | 16 | 0.50 | 17 | 0.44 | 0.54 | 0.49 | 28 | 0.43 | 0.55 | 0.37 | 7 | 0.30 | 0.45 |
| 0.45 | 17 | 0.50 | 21 | 0.44 | 0.55 | 0.48 | 17 | 0.41 | 0.56 | 0.40 | 12 | 0.32 | 0.49 |
| 0.47 | 18 | 0.49 | 16 | 0.44 | 0.54 | 0.51 | 45 | 0.46 | 0.56 | 0.44 | 33 | 0.37 | 0.52 |
| 0.48 | 19 | 0.50 | 18 | 0.44 | 0.55 | 0.50 | 36 | 0.45 | 0.55 | 0.46 | 38 | 0.40 | 0.53 |
| 0.48 | 20 | 0.50 | 19 | 0.44 | 0.54 | 0.51 | 40 | 0.45 | 0.56 | 0.50 | 50 | 0.43 | 0.58 |
| 0.48 | 21 | 0.50 | 20 | 0.45 | 0.54 | 0.48 | 21 | 0.43 | 0.54 | 0.38 | 9 | 0.31 | 0.45 |
| 0.49 | 22 | 0.50 | 23 | 0.45 | 0.55 | 0.51 | 41 | 0.45 | 0.56 | 0.49 | 46 | 0.42 | 0.55 |
| 0.49 | 23 | 0.50 | 22 | 0.44 | 0.55 | 0.52 | 46 | 0.46 | 0.57 | 0.44 | 32 | 0.37 | 0.52 |
| 0.49 | 24 | 0.50 | 25 | 0.44 | 0.56 | 0.47 | 4 | 0.41 | 0.52 | 0.37 | 6 | 0.31 | 0.43 |
| 0.50 | 25 | 0.50 | 24 | 0.45 | 0.55 | 0.54 | 52 | 0.45 | 0.63 | 0.40 | 10 | 0.29 | 0.52 |
| 0.50 | 26 | 0.50 | 27 | 0.45 | 0.56 | 0.64 | 56 | 0.53 | 0.75 | 0.63 | 57 | 0.52 | 0.75 |
| 0.50 | 27 | 0.50 | 28 | 0.45 | 0.56 | 0.54 | 50 | 0.47 | 0.60 | 0.55 | 53 | 0.47 | 0.63 |
| 0.50 | 28 | 0.50 | 26 | 0.45 | 0.56 | 0.50 | 32 | 0.45 | 0.54 | 0.43 | 24 | 0.37 | 0.49 |
| 0.52 | 29 | 0.50 | 30 | 0.46 | 0.55 | 0.47 | 9 | 0.42 | 0.54 | 0.34 | 1 | 0.28 | 0.42 |
| 0.52 | 30 | 0.50 | 31 | 0.46 | 0.55 | 0.48 | 19 | 0.43 | 0.54 | 0.40 | 13 | 0.34 | 0.47 |
| 0.52 | 31 | 0.50 | 32 | 0.45 | 0.56 | 0.49 | 25 | 0.42 | 0.54 | 0.47 | 40 | 0.39 | 0.55 |
| 0.52 | 32 | 0.50 | 35 | 0.45 | 0.56 | 0.48 | 20 | 0.44 | 0.53 | 0.41 | 19 | 0.36 | 0.48 |
| 0.52 | 33 | 0.50 | 36 | 0.46 | 0.55 | 0.50 | 33 | 0.46 | 0.55 | 0.48 | 44 | 0.41 | 0.54 |
| 0.53 | 34 | 0.50 | 37 | 0.46 | 0.56 | 0.47 | 11 | 0.43 | 0.53 | 0.37 | 5 | 0.31 | 0.43 |
| 0.53 | 35 | 0.51 | 41 | 0.45 | 0.56 | 0.50 | 31 | 0.44 | 0.55 | 0.43 | 27 | 0.37 | 0.51 |
| 0.53 | 36 | 0.50 | 38 | 0.46 | 0.56 | 0.52 | 49 | 0.46 | 0.58 | 0.50 | 49 | 0.43 | 0.57 |
| 0.54 | 37 | 0.51 | 42 | 0.46 | 0.57 | 0.48 | 22 | 0.41 | 0.56 | 0.41 | 16 | 0.32 | 0.50 |
| 0.54 | 38 | 0.51 | 43 | 0.46 | 0.56 | 0.55 | 53 | 0.48 | 0.61 | 0.51 | 51 | 0.43 | 0.60 |
| 0.54 | 39 | 0.50 | 33 | 0.45 | 0.56 | 0.51 | 44 | 0.47 | 0.57 | 0.49 | 47 | 0.43 | 0.56 |
| 0.54 | 40 | 0.51 | 46 | 0.46 | 0.57 | 0.50 | 34 | 0.45 | 0.56 | 0.48 | 45 | 0.42 | 0.54 |
| 0.54 | 41 | 0.50 | 39 | 0.45 | 0.56 | 0.51 | 42 | 0.45 | 0.57 | 0.46 | 37 | 0.39 | 0.53 |
| 0.55 | 42 | 0.50 | 29 | 0.45 | 0.55 | 0.48 | 12 | 0.42 | 0.54 | 0.36 | 4 | 0.29 | 0.43 |
| 0.55 | 43 | 0.51 | 45 | 0.46 | 0.56 | 0.49 | 27 | 0.45 | 0.55 | 0.47 | 42 | 0.41 | 0.54 |
| 0.55 | 44 | 0.51 | 44 | 0.46 | 0.55 | 0.49 | 26 | 0.45 | 0.53 | 0.43 | 28 | 0.38 | 0.49 |
| 0.55 | 45 | 0.51 | 49 | 0.46 | 0.57 | 0.51 | 43 | 0.47 | 0.56 | 0.43 | 26 | 0.37 | 0.49 |
| 0.56 | 46 | 0.51 | 50 | 0.47 | 0.57 | 0.50 | 35 | 0.46 | 0.55 | 0.47 | 41 | 0.41 | 0.53 |
| 0.56 | 47 | 0.51 | 51 | 0.47 | 0.57 | 0.52 | 47 | 0.47 | 0.57 | 0.46 | 39 | 0.40 | 0.53 |
| 0.57 | 48 | 0.51 | 52 | 0.47 | 0.57 | 0.48 | 23 | 0.44 | 0.54 | 0.43 | 25 | 0.38 | 0.49 |
| 0.57 | 49 | 0.50 | 40 | 0.45 | 0.56 | 0.49 | 29 | 0.44 | 0.55 | 0.40 | 14 | 0.34 | 0.47 |
| 0.58 | 50 | 0.51 | 47 | 0.46 | 0.57 | 0.52 | 48 | 0.47 | 0.58 | 0.49 | 48 | 0.42 | 0.57 |
| 0.58 | 51 | 0.51 | 53 | 0.47 | 0.57 | 0.54 | 51 | 0.49 | 0.59 | 0.51 | 52 | 0.45 | 0.59 |
| 0.60 | 52 | 0.51 | 48 | 0.45 | 0.58 | 0.49 | 30 | 0.44 | 0.55 | 0.45 | 34 | 0.39 | 0.52 |
| 0.62 | 53 | 0.50 | 34 | 0.45 | 0.56 | 0.55 | 54 | 0.48 | 0.63 | 0.55 | 54 | 0.46 | 0.65 |
| 0.64 | 54 | 0.52 | 56 | 0.47 | 0.58 | 0.50 | 37 | 0.46 | 0.56 | 0.41 | 20 | 0.35 | 0.49 |
| 0.64 | 55 | 0.51 | 54 | 0.47 | 0.58 | 0.51 | 38 | 0.46 | 0.56 | 0.44 | 31 | 0.38 | 0.52 |
| 0.69 | 56 | 0.52 | 57 | 0.47 | 0.60 | 0.68 | 57 | 0.53 | 0.82 | 0.56 | 56 | 0.39 | 0.74 |
| 0.86 | 57 | 0.51 | 55 | 0.47 | 0.59 | 0.57 | 55 | 0.49 | 0.65 | 0.56 | 55 | 0.47 | 0.66 |
For the 57 census tracts within Corpus Christi, the observed proportion of stroke cases arriving by ambulance is given. The 10 lowest EMS utilizing tracts are highlighted in blue. Rankings are given in subsequent columns for the models taking into account neighborhood level factors, and neighborhood plus individual level factors. The lowest 10 tracts in the fully adjusted model are highlighted in yellow. Three tracts which were in the lowest 10 for both are highlighted green. This demonstrates that some neighborhoods appear to have very low utilization of ambulance -but this may be explained by the stronger individual level factors (stroke severity and presence of ICH) within the community. The model estimates assume all continuous covariates are at the mean, and each categorical covariate is at the reference level (ischemic stroke, male, Mexican-American, no past history of stroke). Note that the overall proportion arriving by ambulance in this table ranges from 0.10-0.86 (which differs from the countywide range of 0.17-071) as all cases who were not non-Hispanic white or Mexican American were excluded from these models.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Brown D, Boden-Albala B, Langa K, Lisabeth L, Fair M, Smith M, et al. Projected costs of ischemic stroke in the United States. Neurology. 2006;67:1390–5. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- [2].Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart Disease and Stroke Statistics—2012 Update A Report From the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jauch EC, Cucchiara B, Adeoye O, Meurer W, Brice J, Chan Y, et al. Part 11: Adult Stroke: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S818–S28. doi: 10.1161/CIRCULATIONAHA.110.971044. [DOI] [PubMed] [Google Scholar]
- [4].Lees KR, Bluhmki E, Von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- [5].Katzan IL, Graber TW, Furlan AJ, Sundararajan S, Sila CA, Houser G, et al. Cuyahoga County Operation Stroke Speed of Emergency Department Evaluation and Compliance With National Institutes of Neurological Disorders and Stroke Time Targets. Stroke. 2003;34:994–8. doi: 10.1161/01.STR.0000060870.55480.61. [DOI] [PubMed] [Google Scholar]
- [6].Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency Medical Service Hospital Prenotification Is Associated With Improved Evaluation and Treatment of Acute Ischemic Stroke. Circulation: Cardiovascular Quality and Outcomes. 2012;5:514–22. doi: 10.1161/CIRCOUTCOMES.112.965210. [DOI] [PubMed] [Google Scholar]
- [7].Nadeau JO, Shi S, Fang J, Kapral MK, Richards JA, Silver FL, et al. TPA use for stroke in the Registry of the Canadian Stroke Network. The Canadian Journal of Neurological Sciences. 2005;32:433–9. doi: 10.1017/s0317167100004418. [DOI] [PubMed] [Google Scholar]
- [8].Deng YZ, Reeves MJ, Jacobs BS, Birbeck GL, Kothari RU, Hickenbottom SL, et al. IV tissue plasminogen activator use in acute stroke: Experience from a statewide registry. Neurology. 2006;66:306–12. doi: 10.1212/01.wnl.0000196478.77152.fc. [DOI] [PubMed] [Google Scholar]
- [9].Smith MA, Lisabeth LD, Bonikowski F, Morgenstern LB. The Role of Ethnicity, Sex, and Language on Delay to Hospital Arrival for Acute Ischemic Stroke. Stroke. 2010;41:905–9. doi: 10.1161/STROKEAHA.110.578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sasson C, Keirns CC, Smith D, Sayre M, Macy M, Meurer W, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter? Annals of internal medicine. 2010;153:19. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of Use of Emergency Medical Services in a Population With Stroke Symptoms: The Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;31:2591–6. doi: 10.1161/01.str.31.11.2591. [DOI] [PubMed] [Google Scholar]
- [12].Boden-Albala B, Carman H, Moran M, Doyle M, Paik MC. Perception of Recurrent Stroke Risk among Black, White and Hispanic Ischemic Stroke and Transient Ischemic Attack Survivors: The SWIFT Study. Neuroepidemiology. 2011;37:83–7. doi: 10.1159/000329522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Morgenstern LB, Gonzales NR, Maddox KE, Brown DL, Karim AP, Espinosa N, et al. A Randomized, Controlled Trial to Teach Middle School Children to Recognize Stroke and Call 911 The Kids Identifying and Defeating Stroke Project. Stroke. 2007;38:2972–8. doi: 10.1161/STROKEAHA.107.490078. [DOI] [PubMed] [Google Scholar]
- [14].Tadros A, Crocco T, Davis SM, Newman J, Mullen J, Best R, et al. Emergency Medical Services-Based Community Stroke Education: Pilot Results From a Novel Approach. Stroke. 2009;40:2134–42. doi: 10.1161/STROKEAHA.108.532762. [DOI] [PubMed] [Google Scholar]
- [15].Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. The Lancet. 375:1695–703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- [16].Morgenstern LB, Smith MA, Lisabeth LD, Risser JMH, Uchino K, Garcia N, et al. Excess Stroke in Mexican Americans Compared with Non-Hispanic Whites: The Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–83. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Morgenstern LB, Smith MA, Sánchez BN, Brown DL, Zahuranec DB, Garcia N, et al. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Annals of neurology. 2013;74:778–85. doi: 10.1002/ana.23972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].US Census Bureau . Corpus Christi (city) State and County QuickFacts; Texas: 2014. [Google Scholar]
- [19].Piriyawat P, Šmajsová M, Smith MA, Pallegar S, Al-Wabil A, Garcia NM, et al. Comparison of Active and Passive Surveillance for Cerebrovascular Disease: The Brain Attack Surveillance in Corpus Christi (BASIC) Project. American Journal of Epidemiology. 2002;156:1062–9. doi: 10.1093/aje/kwf152. [DOI] [PubMed] [Google Scholar]
- [20].Smith M, Risser J, Moyé L, Garcia N, Akiwumi O, Uchino K, et al. Designing multi-ethnic stroke studies: the Brain Attack Surveillance in Corpus Christi (BASIC) project. Ethnicity & disease. 2004;14:520. [PubMed] [Google Scholar]
- [21].Majersik J, Smith MA, Zahuranec DB, Sánchez BN, Morgenstern LB. Population-Based Analysis of the Impact of Expanding the Time Window for Acute Stroke Treatment. Stroke. 2007;38:3213–7. doi: 10.1161/STROKEAHA.107.491852. [DOI] [PubMed] [Google Scholar]
- [22].Sasson C, Haukoos JS, Ben-Youssef L, Ramirez L, Bull S, Eigel B, et al. Barriers to Calling 911 and Learning and Performing Cardiopulmonary Resuscitation for Residents of Primarily Latino, High-Risk Neighborhoods in Denver, Colorado. Annals of Emergency Medicine. 2015;65:545–52.e2. doi: 10.1016/j.annemergmed.2014.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective Assessment of Initial Stroke Severity With the NIH Stroke Scale. Stroke. 2000;31:858–62. doi: 10.1161/01.str.31.4.858. [DOI] [PubMed] [Google Scholar]
- [24].Branas CC, MacKenzie EJ, Williams JC, et al. ACcess to trauma centers in the united states. JAMA. 2005;293:2626–33. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- [25].Cromley EK. GIS AND DISEASE. Annual Review of Public Health. 2003;24:7–24. doi: 10.1146/annurev.publhealth.24.012902.141019. [DOI] [PubMed] [Google Scholar]
- [26].Kleindorfer D, Lindsell C, Alwell KA, Moomaw CJ, Woo D, Flaherty ML, et al. Patients Living in Impoverished Areas Have More Severe Ischemic Strokes. Stroke. 2012;43:2055–9. doi: 10.1161/STROKEAHA.111.649608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Jones SP, Jenkinson AJ, Leathley MJ, Watkins CL. Stroke knowledge and awareness: an integrative review of the evidence. Age and Ageing. 2010;39:11–22. doi: 10.1093/ageing/afp196. [DOI] [PubMed] [Google Scholar]
- [28].Augustin T, Glass TA, James BD, Schwartz BS. Neighborhood Psychosocial Hazards and Cardiovascular Disease: The Baltimore Memory Study. American Journal of Public Health. 2008;98:1664–70. doi: 10.2105/AJPH.2007.125138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Yanagida T, Fujimoto S, Inoue T, Suzuki S. Causes of prehospital delay in stroke patients in an urban aging society. Journal of Clinical Gerontology and Geriatrics [Google Scholar]
- [30].Auchincloss AH, van Nostrand JF, Ronsaville D. Access to Health Care for Older Persons in the United States: Personal, Structural, and Neighborhood Characteristics. Journal of Aging and Health. 2001;13:329–54. doi: 10.1177/089826430101300302. [DOI] [PubMed] [Google Scholar]
- [31].Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, et al. Association of Neighborhood Characteristics with Bystander-Initiated CPR. New England Journal of Medicine. 2012;367:1607–15. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Treno AJ, Gruenewald PJ, Lee JP, Remer LG. The Sacramento Neighborhood Alcohol Prevention Project: Outcomes From a Community Prevention Trial. Journal of studies on alcohol and drugs. 2007;68:197–207. doi: 10.15288/jsad.2007.68.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kleindorfer DO, Lindsell CJ, Broderick JP, Flaherty ML, Woo D, Ewing I, et al. Community Socioeconomic Status and Prehospital Times in Acute Stroke and Transient Ischemic Attack: Do Poorer Patients Have Longer Delays From 911 Call to the Emergency Department? Stroke. 2006;37:1508–13. doi: 10.1161/01.STR.0000222933.94460.dd. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.