Abstract
Young gay, bisexual, and other men who have sex with men (YMSM) are at increased likelihood of experiencing depression and condomless sexual behaviors The goal of the current investigation was to examine the relationship between negative mood and compulsive sexual behavior (CSB) and to assess for their individual and combined influence on sexual risk-taking behavior among a diverse sample of YMSM in New York City (the P18 Cohort Study). We first analyzed sociodemographic, depressive symptoms, CSB, and sexual risk-taking from the cross-sectional data of 509, 18- or 19-year-old YMSM recruited using non-probability sampling. We found a significant positive correlation between CSB and depression and between CSB and frequency of condomless anal sex acts reported over the past 30 days. Multivariate results found that the presence of both depression and CSB contributed to elevated sexual risk-taking among these urban YMSM. Clinical implications include the importance of assessing for CSB when depression is present and vice versa in order to improve HIV prevention. Informed by Minority Stress Theory and Syndemic Theory, our results suggest that interventions focused on the health of YMSM recognize that mental health, CSB and social context all interact to increase physical health vulnerability vis-a-vis sexual behaviors, depression, and CSB. Thus, HIV prevention and intervention programs need to incorporate mental health components and services that address these needs.
Keywords: YMSM, Depression, Compulsive Sexual Behavior, Sexual Risk
INTRODUCTION
Previous studies of adult gay men have found that those who scored higher on measures of compulsive sexual behavior (CSB), defined as frequent or intense sexual fantasies and behaviors that interfere with personal, interpersonal, and vocational pursuits (Muench & Parsons, 2004) also reported higher depressive symptoms (Bancroft et al., 2003; Parsons, Grov, & Golub, 2012). Similarly, those who scored higher on measures of CSB were also more likely to report engaging in condomless intercourse with multiple partners, engaging in condomless sex acts more frequently, engaging in more sex acts with partners of unknown HIV/sexually transmitted infection (STI) status, and also using more illicit drugs concurrently while engaging in sex (Benotsch, Kalichman, & Kelly, 1999; Kalichman & Rompa, 1995; Reece, 2003; Semple, Zians, Grant, & Patterson, 2006). However, previous work on establishing an association between depression and sexual risk-taking has yielded mixed results. While several researchers have previously demonstrated that among some adult gay men there is an increase in sexual interest, and sexual risk-taking during negative mood states (Bancroft et al., 2003; Bancroft & Vukadinovic, 2004; Parsons et al., 2008; Parsons, Grov, & Golub, 2012), Crepaz and Marks (2001) conducted a meta-analysis of 34 studies and found little evidence that negative mood was associated with sexual risk behavior. Beidas and colleagues (2012) found that YMSM who had a diagnosis of major depressive disorder engaged in fewer acts of condomless anal sex. To further complicate matters, Wilson and colleagues (2014) found significant within-person deviations whereby HIV-positive men were more likely to engage in condomless anal sex during weeks that they rated their depression as higher than their average level. Thus, the relationship between negative mood and sexual risk-taking is complicated and nuanced. A better understanding of depression and the effect it may have on the relationship between CSB and sexual risk-taking is currently warranted.
The relationships between CSB, depressive symptoms, and the associated sexual-risk behaviors have yet to be studied among the segment of the gay population with the highest new serocoversion rates, urban young men who have sex with men (YMSM; Halkitis, Wolitski, & Millett, 2013; NYCDHMH, 2011). Investigation of these potentially overlapping conditions is especially important for YMSM since previous research on sexual identity development has shown that YMSM are more likely to experience the need to keep their sexual behavior secret, to have not yet disclosed their sexual identity to family and friends, and to be immersed in social contexts where homophobia and anti-gay sentiments are prevalent (e.g., academic institutions and religious organizations; D’Augelli, Hershberger, & Pinkington, 2010; Dube & Savin-Williams, 1999; Savin-Williams, 2001). Therefore YMSM may be at a particularly vulnerable developmental stage where they are at acute risk for the onset of mood disturbances, CSB, and/or sexual-risk behaviors.
Given this background, the present study sought to assess the individual and combined effects of CSB and depressive symptoms on sexual risk taking among YMSM. Specifically, we sought to assess the extent to which depressive symptoms moderated the established relationship between CSB and sexual risk-taking. This study was guided by two psychological theories, Minority Stress Theory (Meyer, 1995, 2003) and Syndemic Theory (Singer, 1994, 1996). Minority Stress Theory provides one paradigm from which to examine the cumulative effects of minority stressors on the well-being of YMSM. Minority Stress Theory maintains that individuals who have non-mainstream identities, such as gay men and/or racial/ethnic minorities, are at increased risk for mental health problems, which, in turn, influence sexual risk-taking behaviors (Meyer, 1995). Minority Stress Theory asserts that stigma, prejudice, and discrimination create a hostile and stressful social milieu, and that these stressors are evidenced in multiple domains including but not limited to educational environment, political systems, employment and healthcare settings, as well as housing. Meyer attributes the disparities in mental health to the repeated occurrence of injustice among minority populations in these and other contexts. In essence, Minority Stress Theory posits that it is the unequal treatment of minority groups that is responsible for most mental health problems. The Minority Stress model describes stress processes, including the experience of prejudice events, expectations of rejection, hiding and concealing, internalized homophobia, and ameliorative coping processes (Meyer, 2003).
Syndemic Theory posits that multiple stressors, stigmas, and experiences of discrimination interact with problems such as poverty, trauma, violence, and drug use, making safer-sex practices more difficult to sustain (Singer, 1994, 1996). In particular, Syndemic Theory asserts that HIV/STIs disproportionately impact individuals and communities already experiencing greater racism, poverty, mental health concerns, and poor access to health care. In 2003, Stall et al. extended the theory by measuring drug use, depression, childhood sexual abuse, and partner violence as components of a syndemic among men who have sex with men and found that it was the additive impact of these factors that exacerbated the vulnerability of health conditions such as HIV/AIDS. Using this model, Stall, Friedman, and Catania (2008) explored the possibility of syndemic production developmentally among gay and bisexual men, and found that the cultural marginalization experienced by sexual minority men alone was enough to produce evidence of a syndemic. In 2007, Mustanski et al. extended Syndemic Theory to urban YMSM by measuring substance use, psychological distress, sexual assault, and partner violence as components of a syndemic and also found that the number of these psychosocial health problems was associated with sexual risk behaviors in an additive way. Similarly, our research team recently found evidence for the synergistic effects of drug use and mental health burden in increasing sexual risk taking among urban YMSM (Halkits et al., 2013). Finally, in 2012, Parsons, Grov, and Golub, adapted Syndemic theory to include compulsive sexual behavior along with substance use, depression, childhood sexual abuse, and partner violence among adult gay and bisexual men, concluding that compulsive sexual behavior could indeed be a component of the syndemic framework.
Informed by the Minority Stress Model, the application of Syndemic Theory to gay and bisexual men, and our previous work investigating syndemic production among urban YMSM, the current study sought to focus on the mental health aspect of the syndemic model. In so doing, we took the analysis of a syndemic among YMSM one step further by investigating the relationship between CSB and depressive symptoms. Specifically, we sought to determine whether depression had an impact on the relationship between CSB and sexual risk-taking behavior among these urban YMSM.
Compared with heterosexual peers, YMSM experience lower levels of self-esteem and higher levels of anxiety, stress, and depression (Meyer, 2003; Rosario, Schrimshaw, & Hunter, 2006; Salomon et al., 2009). YMSM may also experience internalized homophobia (Botvin, Epstein, Schinke, & Diaz, 1994; Newcomb & Mustanski, 2009), negative body image (Siconolfi, Halkitis, Allomong, & Burton, 2009), and stigma (Frost, Parsons, & Nanin, 2007), all of which can contribute to negative affective states. The disproportionate prevalence of these negative states may be attributed to the heightened marginalization, homophobia, and discrimination that YMSM experience. These negative affective states may in turn lead to the development of maladaptive behaviors including CSB in an attempt to regulate mood (Parsons et al., 2008). The current study sought to better delineate the effects that negative mood and CSB have on sexual risk taking among YMSM by examining cross-sectional data drawn from a single point during a prospective cohort study. We used bivariate and regression analysis to test for the individual and interactive effects of negative mood and CSB in sexual risk-taking behavior. In this approach, we sought to take a closer look at the possible confluence of these variables within the overarching theory of syndemic production, in order to explore possible avenues to improve sexual and mental health among YMSM. We hypothesized that depression would be associated with CSB and that depression will moderate the relationship between CSB and condomless anal intercourse.
METHODS
Participants
Participants were recruited via a non-probability sampling procedure between June 2009 and May 2011 using both active and passive methods across the New York City metropolitan area. Active recruitment sites included social media sites on the Internet, New York City streets, New York City parks, college campuses and dormitories, gay-identified events, and community centers. Passive recruitment included snowball sampling where study participants were selected at random to be eligible to receive a ten dollar cash incentive for each eligible participant (maximum ten participants) they referred to the study.
To be enrolled in the P18 Cohort Study participants needed to be 18 or 19 years of age, biologically male, self-report having been sexually active with another man during the six months prior to interview, self-report residing in the New York City area, self-report a seronegative or unknown HIV status at baseline, and agree to study protocol and oral HIV antibody testing. To ensure a sufficient sample of racial and ethnic minorities (Black, Latino, Asian-Pacific Islander, and multiracial) in our cohort, we oversampled these groups during recruitment.
A total of 2,068 individuals were screened for inclusion in the current study, with 598 enrolled in the baseline assessment. The first follow-up assessment occurred 6-months after the baseline assessment and consisted of the 509 YMSM who returned for follow-up at this time-point. It was during this assessment that sexual compulsivity was measured, thus the current analysis consists of these 509 YMSM. Prior to study implementation, all study protocols were approved by the Institutional Review Board (IRB) at New York University and study data are protected by a federal Certificate of Confidentiality.
Study Design
Project 18 is a longitudinal cohort study of YMSM in New York City that seeks to examine the developmental pathways of these young men in order to better understand their specific risk factors for HIV infection (Halkitis et al., 2013). The study design originally consisted of seven waves of data collection at 6-month intervals. However, only data from the first 6-month follow-up assessment was used for this cross-sectional analysis, as this was the specific time-point at which compulsive sexual behavior data were collected. All study participants provided informed consent prior to beginning the baseline interview and were remunerated $35 for their time and effort during the 6-month assessment. The assessment included the collection of demographic, psychosocial, CSB, and depression data using audio computer-assisted self-interview (ACASI) software to reduce biases associated with interviewer-administered surveys and socially-desirable responding. Data on sexual behavior was collected using the Time Line Follow Back methodology (Sobell & Sobell, 1996) which entailed an interviewer-administered 30-day calendar of sexual and substance use behaviors.
Measures
Demographic Characteristics
Participants self-reported their race/ethnicity, educational status, housing status, relationship status, sexual orientation identification and perceived familial socioeconomic status (SES).
Depression
Depression was measured via self-report using the 21-item Beck Depression Inventory, second edition (BDI-II, Beck, Steer, & Brown, 1996). Items determine indicators of depression including experience of loss of pleasure, feelings of worthlessness, and experience of loss of energy. Answers range on a Likert-type scale from 0 “None” through 3 “Very Much.” This measure has been shown to have high internal consistency and test-retest reliability, as well as convergent and construct validity (Beck, Steer, & Brown, 1996). In a previous study (Halkitis et al., 2012) with the P18 baseline data, the inventory demonstrated high internal consistency reliability (α = .91).
Compulsive Sexual Behavior
Participants’ experience of CSB was ascertained via self-report using the Compulsive Sexual Behavior Inventory (CSBI; Coleman et al., 2001). The 22-item CSBI measures a constellation of sexual behaviors defined as being extreme in both number and intrusiveness, engaged in as a moderator of emotional issues, and involving a significant disruption in normal interpersonal functioning (Miner et al., 2007). The 22-item CSBI assesses difficulty controlling sexuality, feeling emotionally distant during sex, experiences with physical and sexual aggression in dating relationships, experience giving or receiving pain for sexual pleasure, and legal, financial, or relationship problems stemming from sexual behavior (Coleman, 2003). Items also assess the tendency to use sex to cope with guilt, shame, secretiveness, or other problems surrounding sexual behavior (Miner et al.). The CSBI was selected, in part, as it does not contain items that assess for sexual risk-behavior preventing the possibility of criterion contamination. In our prior psychometric analysis (Storholm et al, 2011), the CSBI was found to be both reliable, with a control factor reliability score of α = .93 and a violence factor reliability score of α = .83, and psychometrically valid.
Sexual Risk-Taking Behavior
Recent history (30 days) of sexual behavior was captured using the interviewer-administered Time Line Follow Back (TLFB) calendar method (Sobell & Sobell, 1995). The TLFB uses a calendar where the participant provides a retrospective account of their sexual behavior over the previous 30 days. Several memory aids such as key dates over the past thirty days serve as anchors for reporting previous sexual behavior. The TLFB method is recommended for use when relatively precise estimates of sexual behavior are necessary, especially when a complete picture of sexual risk-taking is needed. For the purposes of this analysis sexual-risk was measured with the dependent variable: number of acts of condomless anal sex (insertive or receptive) in the past 30 days.
Substance Use
In order to control for drug and alcohol use, recent history (prior 30 days) of substance use was also captured using the interviewer-administered TLFB calendar method (Sobell & Sobell, 1995) described above. The TLFB was used to record the number of days the participant used alcohol, marijuana, inhalant nitrates (poppers), powder cocaine, crack cocaine, ecstasy, GHB, ketamine, heroin, methamphetamine, and rohypnol. For purposes of analysis the number of days each of these substances was used was tallied in order to create a total score for substance use during the past 30 days. For a full analysis of substance use as part of syndemic production among the study participants see Halkitis et al., (2013).
Analytic Plan
As both CSB and depression have been associated with sexual risk-taking; the current study assessed the extent to which the relation between CSB and sexual risk-taking (i.e., condomless anal intercourse) was moderated by depression controlling for alcohol and drug use and those psychosocial and demographic variables shown to be significantly associated with the outcome variable (acts of condomless anal sex). For analytic purposes the level of CSB experienced among participants was measured using composite scores from the CSBI and the level of depression experienced among participants was measured using composite scores from the BDI-II. Sexual risk-behavior data included the number of times (acts) the participant reported engaging in condomless anal intercourse (insertive or receptive) during the 30 days prior to interview. Bivariate analyses were run first in order to assess for associations between psychosocial variables, drug/alcohol use, depression, CSB, and condomless anal sex after trichotomizing anal sex acts to account for the non-normal distribution of this outcome variable.
To test the interaction effect of depression on the relationship between CSB and sexual risk-taking we then modeled counts of condomless anal sex with a negative binomial regression to account for the non-normal distribution of the outcome variable. As a safeguard and to eliminate any possibility of muticollinearity, the continuous variables were centered as well as their product, the interaction term (Aiken & West, 1991). Categorical predictors were dummy-coded with school non-enrollment, not currently being in a relationship, and middle upper to upper SES coded as zero. An interaction term of CSB with depression was used to determine the extent to which depression affected the direction and/or strength of the relationship between CSB and the number of acts of condomless anal sex in the past 30 days.
The negative binomial regression model had a deviance value (619.93/499 = 1.24) which was less than two indicating good overall model fit. The regression model is presented and results are reported as incidence rate ratios (IRR). The models adjusted for drug and alcohol use as well as those psychosocial and demographic predictors found to be significant during bivariate analysis. We used generalized estimating equations to handle repeated measurement. All statistical analyses were carried out using SPSS version 22.0.
RESULTS
The first columns of Table 1 provides the demographics of the current sample (N = 509) of YMSM recruited from the Greater New York City area. All participants were either 18 or 19 years old at the time of assessment. The mean score on the BDI-II was 9.80 (SD = 8.71) with a median score of seven. This score did not differ significantly from non-clinical college samples which have ranged from 8.36 (SD = 7.16) to 12.55 (SD = 9.93) in previous studies (Whisman et al., 2000; Steer & Clark, 1997; Beck et al., 1996). The mean score on the CSBI was 37.41 (SD = 10.12) and the median score was 36. One hundred eighty (35.4%) met the optimal cut-score on the CSBI (≥40) for the assessment of CSB as proposed by Storholm et al. (2011). Regarding sexual risk-taking, 281 (55.2%) reported having engaged in condomless oral sex, 56 (11.0%) reported having engaged in condomless insertive anal sex, and 72 (14.1%) reported having engaged in condomless receptive anal sex, during the 30 days prior to their interview. Among those 107 (21.0%) who reported having engaged in any condomless anal sex during the 30 days prior to interview, the mean number of condomless acts was 4.64 (SD = 7.31) ranging from 1 to 54 acts of condomless anal sex over the 30 days prior to interview.
Table 1.
Relationship of Demographic factors to Acts of Condomless Anal Intercourse in the Last 30 Days among Young Men Who Have Sex with Men (N = 509).
| Demographic Variable | Total Sample | 0 Acts | 1 Acts | >1 Acts | X2 | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | (%) | n | (%) | n | (%) | n | (%) | ||
| Race Ethnicity | 9.13 | ||||||||
| Latino | 187 | (36.7) | 144 | (77.0) | 13 | (7.0) | 30 | (16.0) | |
| White | 154 | (30.3) | 122 | (79.2) | 13 | (8.4) | 19 | (12.3) | |
| African American | 80 | (15.7) | 68 | (85.0) | 13 | (6.3) | 7 | (8.8) | |
| Mixed Race/Other | 61 | (12.0) | 45 | (73.8) | 10 | (16.4) | 6 | (9.8) | |
| Asian/Pacific Islander† | 27 | (5.3) | 23 | (85.2) | 2 | (7.4) | 2 | (7.4) | |
| Currently Enrolled in | 9.60* | ||||||||
| High School | 74 | (14.5) | 62 | (83.6) | 7 | (9.6) | 5 | (6.8) | |
| College/Trade School | 366 | (71.9) | 292 | (79.8) | 31 | (8.5) | 43 | (11.7) | |
| Not Currently Enrolled | 69 | (13.6) | 48 | (69.6) | 5 | (7.2) | 16 | (23.2) | |
| Currently in Relationship | 51.39*** | ||||||||
| No | 375 | (73.7) | 323 | (86.1) | 27 | (7.2) | 25 | (6.7) | |
| Yes | 134 | (26.3) | 79 | (59.0) | 16 | (11.9) | 39 | (29.1) | |
| Currently Live with | 6.94 | ||||||||
| Parents/Family | 270 | (53.0) | 219 | (81.1) | 19 | (7.0) | 32 | (11.9) | |
| Friend/Roommate | 184 | (36.1) | 147 | (79.9) | 16 | (8.7) | 21 | (11.4) | |
| Alone/Male Lover | 52 | (10.2) | 34 | (65.4) | 7 | (13.5) | 11 | (21.2) | |
| Shelter/Homeless† | 3 | (0.6) | 2 | (66.7) | 1 | (33.3) | 0 | (0.0) | |
| Perceived Familial SES | 12.74** | ||||||||
| Lower/Lower Middle | 173 | (34.0) | 134 | (77.5) | 8 | (4.6) | 31 | (17.9) | |
| Middle | 185 | (36.3) | 146 | (78.9) | 17 | (9.2) | 22 | (11.9) | |
| Middle Upper/Upper | 151 | (29.7) | 122 | (80.8) | 18 | (11.9) | 11 | (7.3) | |
| Sexual Identification | 7.65 | ||||||||
| Homosexual | 432 | (84.8) | 339 | (78.5) | 35 | (8.1) | 58 | (13.4) | |
| Bisexual | 77 | (15.2) | 63 | (81.8) | 8 | (10.4) | 6 | (7.8) | |
p < .05,
p < .01,
p < .001
Category excluded from pairwise comparison due to expected cell counts <5.
Bivariate Analyses
Table 1 also presents a breakdown of the number of condomless anal sex acts in the 30 days prior to assessment by those demographic characteristics assessed in this study. Given the non-normal distribution for reported frequencies of condomless anal sex, responses were divided into three potential outcomes for analytic purposes: no acts in the last 30 days, one act in the last 30 days, and two or more acts in the last 30 days. Of note, participants indicating that they were not currently enrolled in school and those who reported that they were in a romantic relationship with a male lover or partner reported having significantly more condomless anal sex acts during the 30 days prior to interview than did those who did not. In contrast, participants indicating that they perceived their familial SES as middle/upper to upper status reported having significantly less condomless anal sex acts during the 30 days prior to interview than did those who reported lower to middle SES. However, due to the relatively low proportion (21%) of YMSM who reported any acts of condomless anal sex, combined with previous research indicating that the majority of HIV transmissions among YMSM are from main lovers/partners (Sullivan, Salazar, Buchbinder, & Sanchez, 2009), and the fact that many participants reported having multiple short-term relationships with “main partners” during the period of assessment, we decided to combine the number of condomless sex acts between main partners and casual partners into one overall count and then trichotomize for bivariate analytic purposes.
As hypothesized, depression was significantly associated with level of compulsive sexual behavior (r = .39, p < .001). Table 2 presents participants’ scores on the CSBI by the four levels of depression as measured by the BDI-II. The table shows a steady and significant increase in CSBI scores among YMSM as their level of depression increased. Level of compulsive sexual behavior reported was also significantly associated with the trichotomized variable number of condomless anal sex acts in the past 30 days (ρ = .10, p < .05). Finally, depression severity was also mildly associated with the trichotomized variable number of acts of condomless anal sex in the past 30 days (ρ = .09, p < .05).
Table 2.
Depression and Compulsive Sexual Behavior (N = 509)
| n | (%) | CSBI Score | F | ||
|---|---|---|---|---|---|
| M | (SD) | ||||
| BDI-II Score Level | 17.10, p <.001 | ||||
| Minimal | 300 | (58.9) | 35.3 | (9.1) | |
| Mild | 130 | (25.5) | 37.9 | (8.4) | |
| Moderate | 55 | (10.8) | 43.8 | (13.0) | |
| Severe | 24 | (4.7) | 44.6 | (12.2) | |
Notes. BDI-II scores: 0–9 = minimal, 10–18 = mild, 19–29 = moderate, 30–36 = severe, respectively. Post hoc tests revealed significant differences in CSBI scores for the depression levels as follows: minimal < mild, p <.05; minimal < moderate, p <.001; minimal < severe, p <.01; mild < moderate, p =.01; mild < severe, p <.05. CSBI scores for the moderate and severe depression levels did not differ significantly.
Moderation Analyses
To test whether BDI-II score moderated the relationship between CSBI score and number of acts of condomless anal intercourse in the past 30 days, a negative binomial regression analysis was conducted. To control for the predictor variables shown to be associated with condomless anal sex among this sample, school enrollment, relationship status, SES, and use of drugs and alcohol, were entered into the regression models followed by depression score centered, CSBI score centered, and their product term. Finally, the count data, number of condomless anal intercourse acts, were entered as the outcome variable. Table 3 reports the results of the negative binomial regression model of the count of condomless anal sex acts during the 30 days prior to assessment. The model demonstrated good overall fit and showed that while the main effect of depression did not significantly predict the number of acts of condomless anal sex in the model, the main effect of CSB did. The negative binomial model indicated that these YMSM had 1.03 times more condomless anal sex acts for every one unit increase on the CSBI, holding the other variables constant (p = .001). In addition, these YMSM had 1.02 times more condomless anal sex acts for every one unit increase on the BDI-II and CSBI, indicating that the effect that CSB had on acts of condomless anal sex was different based on the participant’s level of depression (p < .001; from BDI-II X CSBI interaction term).
Table 3.
Negative Binomial Regression for Variables Predicting Acts of Condomless Anal Intercourse in the Last 30 Days among Young Men Who Have Sex with Men (N = 509).
| Variable | IRR | 95% CI | p |
|---|---|---|---|
| Intercept | 0.42 | 0.27, 0.66 | .000 |
| Currently in Relationship | |||
| No | 1.00 | - | - |
| Yes | 6.78 | 5.00, 9.20 | .000 |
| Currently Enrolled in | |||
| Not Enrolled | 1.00 | - | - |
| College/Trade School | 1.10 | 0.72, 1.68 | .656 |
| High School | 0.69 | 0.39, 1.22 | .203 |
| Perceived Familial SES | |||
| Lower/Lower Middle | 1.00 | - | - |
| Middle | 0.64 | 0.45, 0.91 | .012 |
| Middle Upper/Upper | 0.38 | 0.26, 0.56 | .000 |
| Drugs/Alcohol Total Use | 1.05 | 1.04, 1.06 | .000 |
| BDI-II Total Score | 0.99 | 0.97, 1.01 | .228 |
| CSBI Total Score | 1.03 | 1.01, 1.04 | .001 |
| BDI-II X CSBI | 1.02 | 1.01, 1.04 | .000 |
Notes. BDI-II = Beck Depression Inventory; CSBI = Compulsive Sexual Behavior Inventory. Not being in a current relationship with a male partner/lover, not being currently enrolled in school and perceiving one’s familial SES as lower/lower middle were coded as 0.
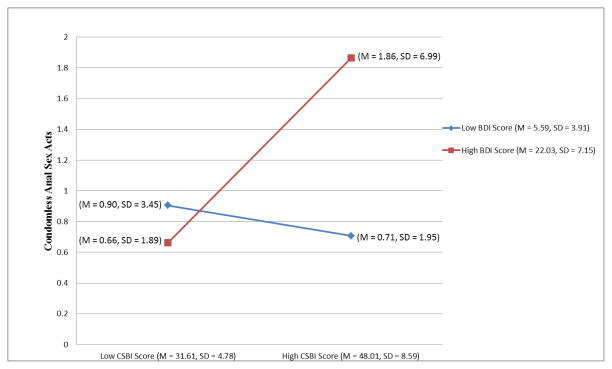
The negative binomial regression model was consistent with the hypothesis that depression moderates the relationship between compulsive sexual behavior and condomless anal intercourse over and above the effects of school enrollment, being in a relationship, SES, and/or use of drugs and alcohol. For the purposes of illustrating the moderation the BDI-II was dichotomized based on a cut score of fourteen on the BDI-II (minimal depression or less; Beck, Steer, & Brown, 1996) was utilized with the majority of YMSM (74.5%) falling below the cutoff in the minimal or less depression range. Similarly, the CSBI was dichotomized based on a cut score of forty as recommended by (Storholm et al., 2011) with the majority of YMSM (64.6%) falling below the cutoff in the low to no CSB range. We then calculated the mean scores for low and high depression and low and high CSB to use as data points to graph the moderation. Figure 1 illustrates that it was the confluence of higher depression scores with higher CSB scores that predicted a significantly higher number of condomless anal intercourse acts than did either higher depression scores or higher CSB scores alone. Therefore, these data suggest that it is the interaction between higher depression and higher compulsive sexual behavior in these urban YMSM that predicts the greatest amount of condomless anal sex.
Figure 1.
Moderation Model: Compulsive Sexual Behavior, Depression, and Condomless Anal Sex.
DISCUSSION
The current study builds on previous studies of mood and sexual behavior by extending the investigation to a new generation of young gay, bisexual, and other YMSM. This cross-sectional analysis aimed to provide a more nuanced understanding of the independent and interacting effects that depression and CSB have, which serve to increase sexual risk-taking behavior among YMSM, putting them at increased risk for the acquisition of HIV and other STIs. This study was timely given the increase in HIV seroconversion rates among urban YMSM (Halkitis et al., 2013; NYCDHMH, 2011). This study utilized a measure of CSB, the Compulsive Sexual Behavior Inventory (CSBI), in order to better understand the specific relation between CSB, depression, and sexual risk-taking behavior among these YMSM. This analysis was unique in that it was the first to investigate CSB among YMSM, and more specifically, the manner in which level of depression influences the relationship between CSB and sexual risk-taking.
In the current analysis CSB was found to be positively correlated with depression among urban YMSM. Consistent with the previous literature on adults (Cooper et al., 1999), CSB was found to also be associated with sexual risk-taking. While past research has shown mixed results regarding the association between depression and sexual risk-taking behavior among YMSM (Crepaz & Marks, 2001; Kosunen et al., 2003; Perdue et al., 2003; Wilson et al., 2014) our analysis indicated that depression was significantly associated with both CSB and condomless anal intercourse. We conducted a moderation analysis to test the hypothesis that depression would influence the relationship between CSB and condomless anal intercourse. This test for moderation was significant, demonstrating that the relationship between CSB and sexual risk-taking was influenced by depression scores among YMSM.
This finding extends previous work that has found mixed results regarding the association between depressive symptomology and sexual risk-taking behaviors (Crepaz & Marks, 2001; Shrier et al., 2001; Strathdee et al., 1998) by providing a more nuanced understanding of the confluence of CSB and negative affect in sexual risk-taking. The current study suggests that sexual risk-taking due to CSB is likely exacerbated among those YMSM with comorbid depressive symptoms. Medical professionals and clinical diagnosticians working with this high-risk segment of the population need to be made aware of the interacting effect of CSB and depression and the acute risk for HIV and STIs to those YMSM who present with both sets of clinical symptoms. Further, clinicians working with depressed YMSM should also assess for the presence of CSB in order to implement appropriate sexual risk-reduction interventions when clinically indicated among this high-risk segment of the population.
With respect to the guiding theoretical models we utilized, Singer (1996) found a positive linear relationship between sexual risk-taking and HIV incidence among men, and the amount of racism, poverty, substance abuse, and violence reported. With regard to YMSM, mental health burden, substance use, physical and sexual abuse, and sexual risk-taking are posited to fuel each other (Halkits, 2010). The current findings complement previous work suggesting that CSB may be an additional key factor in the production of a syndemic (Parsons, Grov, & Golub, 2012) and extend the findings to urban YMSM. Further, these findings are also consistent with Minority Stress Theory (Meyer, 2003), in that the additional stress resulting from the stigma, prejudice, and discrimination experienced by YMSM due to their sexual minority status likely contributed to the high depressive symptoms found among a subsample of the YMSM in the current analysis. The current analysis also extends these findings by providing data that suggest that sexual behavior may be utilized in an attempt to regulate mood among YMSM.
Clinical Implications
Clinicians working with YMSM need to be aware of the likelihood that when both depressive symptoms and CSB are present, risk for HIV seroconversion may be exacerbated. Clinicians should assess for the presence of depression when CSB is indicated and vice versa. The use of brief assessment tools such as the BDI-II and the CSBI may be warranted and useful for these purposes. Further, clinicians employing interventions focused on HIV prevention need to recognize that these complex dynamics do not occur in a vacuum separate from the cultures and contexts that YMSM inhabit, and should consider the impact of factors such as limited social capital and access to resources (Halkitis, Wolitski, & Millett, 2013). Clinicians need focus on education, empowerment, and increasing access to both behavioral (e.g., sexual and substance use risk-reduction) and biomedical (e.g., HIV-testing, treatment as prevention, or pre-exposure prophylaxis PrEP) interventions in conjunction with the psychological and interpersonal problems they are addressing with their patients.
It is important that mental health professionals working with YMSM consistently take into consideration the social and contextual factors at play when working with individuals with depressive symptoms and compulsive sexual behavior. Specifically, clinicians should consider the ways in which heterosexual and male gender norms create psychological burdens for sexual minority men. For example, Hatzenbuehler et al. (2012) found better mental health among sexual minority men in states that have legalized gay marriage, advocating that gay marriage is one example of social change that reduces psychological and psychosocial burdens for gay men solely by moving away from anti-gay legislation. Homophobia and other stigmatizing views of sexual minorities have been known to push YMSM away from their home communities and into larger urban meccas where they find a more tolerant and embracing environment. Clinicians working in such settings should consider the extent to which their urban YMSM clients are identified within the larger gay community, as there is a growing body of literature that suggests gay community affinity may be associated with both positive psychosocial effects as well as higher sexual-risk and drug-related behaviors among YMSM (Holt, 2011; Kapadia et al., 2013; Wong et al., 2005).
Adimora and Auerbach (2010) suggest specific structural approaches that aim to shift harmful social norms, empower communities, and effect policy, social and political change. These specific structural interventions aim to address the important environmental factors that influence the physical, mental, and behavioral health among YMSM. In order to reduce the risk of HIV among these populations, it is not enough for clinicians to simply treat the mental health, substance abuse, or compulsive sexual behavior of YMSM presenting for treatment. Health care providers must consistently address, and seek to change the overarching social, environmental, and contextual factors that place YMSM at risk for HIV and compromise their overall well-being. While the clinical needs of individuals must continue to be assessed and treated, health care providers also must seek to understand and address the specific environmental and contextual factors that contribute to the etiology of these burdens.
Limitations and Strengths of the Study
The current investigation was cross-sectional, and therefore the most salient limitation is the inability to assess temporality in the association between CSB and engagement in condomless anal intercourse with depression as a moderator. Depression that occurs prior to condomless anal intercourse may have different implications for an individual than would depression that occurs after. To account for this the BDI-II and CSBI measures were selected because they ask participants to self-report the overall symptoms they experienced over a specific time period (e.g., two-week period prior to interview). However, future studies should look at these relationships longitudinally in order to establish causality.
Condomless anal intercourse was captured using the Time Line Follow Back calendar method (Sobell & Sobell, 1995). Although this method is recommended when relatively precise estimates of sexual behavior are necessary, there was a minority (n = 105, 20.6%) of YMSM who reported engaging in condomless anal intercourse during the 30 day window prior to interview. The low number of participants reporting condomless anal intercourse may have partly been the result of interviewer effects (e.g., social desirability bias). As such, a more nuanced analyses looking at differences in condomless anal intercourse among those with main partners vs. casual partners was not possible. Further, data on partner’s HIV status were not collected at the six-month assessment of this study. Future work among this population should assess for differences in condomless anal intercourse based on the perceived HIV status of sex partners. The 30 day recall window could also lead to underestimation of overall sexual risk, especially among young participants whose risky sexual behavior was less frequent. Including a broader time window measuring risky sexual-behavior, (e.g., over the past year), may be desirable in future studies.
CSBI scores should be interpreted with caution, since this measure includes items such as “How often have you felt guilty or shameful about aspects of your sexual behavior?” and “How often have you concealed or hidden your sexual behavior from others?” While these items may be accurate in the ascertainment of CSB among adult heterosexual individuals, many YMSM report experiencing shame and guilt over their normative same-sex behavior, and report having tried to hide or conceal their normative same-sex behavior. These items may be endorsed among YMSM irrespective of the presence of CSB. As a result, studies that utilize the CSBI with YMSM may have a disproportionately higher number of false-positives.
Finally, the sample was targeted and stratified to include two-thirds racial/ethnic minorities, and therefore was not randomly selected. Targeting YMSM on the streets, on college campuses, online, and at LGBT events may limit generalizability because younger or older looking individuals may not have been solicited. However, targeted sampling has often been found to be more efficacious than random sampling when the aim of a study is to assess a specific subset of the population by a given characteristic such as age or sexual orientation (Watters & Biernacki, 1989).
Recommendations for Future Research
While only one-fifth of the YMSM sampled reported engaging in condomless anal intercourse during the 30 days prior to assessment, over one-third (n = 180, 35.4%) of YMSM met the optimal cut-score criteria (≥ 40) on the CSBI as proposed previously by Storholm et al. (2011). This finding may be suggestive of an overall tendency towards compulsive sexual behavior in general that may not manifest as sexual risk-taking until later in development. Another possible interpretation is that heightened rates of CSB among this sample are due to psychological distress that is not the result of compulsive sexual behavior but simply guilt and shame over same-sex behavior that takes place within stigmatizing and marginalizing social structures such as institutional discrimination (e.g., living in states that ban same-sex marriage; Hatzenbuehler et al., 2012, Hatzenbuehler, Phelan, & Link, 2013). Future studies should focus on teasing CSB apart from distress due to normative same-sex behavior among samples of gender and sexual minority individuals. Longitudinal analyses are warranted to better comprehend the complex etiology of compulsive behavior in general and CSB specifically among YMSM. Future analyses should also focus on the development of complex multivariable and nested models that determine temporal association between variables and better elucidate the contribution of depression in sexual risk-taking among those who present with CSB across time and also within given social structures.
Conclusion
This study was the first to examine the relations between CSB, depression, and sexual risk-taking among urban YMSM. Higher levels of CSB were associated with higher levels depression, and higher levels of sexual risk-taking (i.e., condomless anal sex). However, this study presents evidence that engagement in sexual risk-taking behavior is part of a complex constellation of factors and is not simply the direct result of CSB. For example, depression may moderate the relationship between CSB and sexual risk-taking, suggesting that it is the confluence of CSB and depression that together contribute to sexual risk-taking. Theoretically, the effect of these multiple contributing factors has come to be known as a syndemic. While prevention efforts continue to target specific targets for intervention, such as depression, substance abuse, and unsafe sex, future efforts must address the larger social structures that continue to stigmatize YMSM.
Acknowledgments
This study is funded by a grant from the National Institute of Drug Abuse (R01DA025537) with additional funding for Dr. Storholm provided by the National Institute of Drug Abuse training grant (T32DA007250).
References
- Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. Journal of Acquired Immune Deficiency Syndromes. 2010;55(2):132–135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Bancroft J, Janssen E, Strong D, Vukadinovic Z. The relation between mood and sexuality in gay men. Archives of Sexual Behavior. 2003;32(3):231–242. doi: 10.1023/a:1023461500810. [DOI] [PubMed] [Google Scholar]
- Bancroft J, Vukadinovic Z. Sexual addiction, sexual compulsivity, sexual impulsivity, or what? Toward a theoretical model. Journal of Sex Research. 2004;41(3):225–234. doi: 10.1080/00224490409552230. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Beidas RS, Birkett M, Newcomb MA, Mustanski B. Do psychiatric disorders moderate the relationship between psychological distress and sexual risk-taking behaviors in young men who have sex with men? A longitudinal perspective. AIDS Patient Care and STDs. 2012;26(6):366–374. doi: 10.1089/apc.2011.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in HIV-seropositive men who have sex with men: Prevalence and predictors of high-risk behaviors. Addictive Behaviors. 1999;24(6):857–868. doi: 10.1016/s0306-4603(99)00056-8. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Epstein JA, Schinke SP, Diaz T. Predictors of cigarette smoking among inner-city minority youth. Journal of Developmental & Behavioral Pediatrics. 1994;15(2):67–73. [PubMed] [Google Scholar]
- Coleman E. Compulsive sexual behavior: What to call it, how to treat it? SIECUS Report. 2003;31(5):12–16. [Google Scholar]
- Coleman E, Miner M, Ohlerking F, Raymond N. Compulsive Sexual Behavior Inventory: A preliminary study of reliability and validity. Journal of Sex & Marital Therapy. 2001;27(4):325–332. doi: 10.1080/009262301317081070. [DOI] [PubMed] [Google Scholar]
- Cooper A, Scherer CR, Boies S, Gordon B. Sexuality on the internet: From sexual exploration to pathological expression. Professional Psychology: Research and Practice. 1999;30:154–164. [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20(4):291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, Hershberger SL, Pinkington NW. Lesbian, gay, and bisexual youth and their families: Disclosure of sexual orientation and its consequences. American Journal of Orthopsychiatry. 2010;68(3):361–371. doi: 10.1037/h0080345. [DOI] [PubMed] [Google Scholar]
- Dube EM, Savin-Williams RC. Sexual identity development among ethnic sexual-minority male youths. Developmental Psychology. 2001;35(6):1389–1398. doi: 10.1037//0012-1649.35.6.1389. [DOI] [PubMed] [Google Scholar]
- Frost DM, Parsons JT, Nanin JE. Stigma, concealment and symptoms of depression as explanations for sexually transmitted infections among gay men. Journal of Health Psychology. 2007;12(4):636–640. doi: 10.1177/1359105307078170. [DOI] [PubMed] [Google Scholar]
- Halkitis PN. Reframing HIV prevention for gay men in the United States. American Psychologist. 2010;65(8):753–763. doi: 10.1037/0003-066X.65.8.752. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Hampton MC, Bub K. Measurement model exploring a syndemic in emergent adult gay and bisexual men. AIDS and Behavior. 2013;17(1):662–673. doi: 10.1007/s10461-012-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Wolitski RJ, Millett GA. A holistic approach to addressing HIV infection dipartites in gay, bisexual, and other MSM. American Psychologist. 2013;68(4):261–273. doi: 10.1037/a0032746. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, O’Clerigh C, Grasso C, Mayer K, Safren S, Bradford J. Effect of same-sex marriage laws on health care use and expenditures in sexual minority men: A quasi-natural experiment. American Journal of Public Health. 2012;102(2):285–291. doi: 10.2105/AJPH.2011.300382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt M. Gay men and ambivalence amout ‘gay community’: from gay community attachment to personal communities. Culture, Health and Sexuality. 2011;13(8):857–871. doi: 10.1080/13691058.2011.581390. [DOI] [PubMed] [Google Scholar]
- Kafka MP, Prentky R. Fluoxetine treatment of nanparaphilic sexual addictions and paraphilias in men. Journal of Clinical Psychiatry. 1992;53(10):351–358. [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: Reliability, validity, and predicting HIV risk behavior. Journal of Personality Assessment. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- Kapadia F, Siconolfi DE, Barton S, Olivieri B, Lombardo L, Halkitis PN. Social support network characteristics and sexual risk taking among a racially/ethnically diverse sample of young, urban, men who have sex with men. AIDS and Behavior. 2013;17(5):1819–1828. doi: 10.1007/s10461-013-0468-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosunen E, Haltiala-Heino R, Rimpela M, Laippala P. Risk-taking sexual behaviour and self-reported depression in middle adolescence-a school based survey. Child: Care, Health and Development. 2003;29(5):337–344. doi: 10.1046/j.1365-2214.2003.00357.x. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36(1):38–56. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner MH, Coleman E, Center BA, Ross M, Rosser BR. The Compulsive Sexual Behavior Inventory: Psychometric properties. Archives of Sexual Behavior. 2007;36(4):579–587. doi: 10.1007/s10508-006-9127-2. [DOI] [PubMed] [Google Scholar]
- Muench F, Parsons JT. Sexual compulsivity and HIV: Identification and treatment. Focus. 2004;19(6):1–5. [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene. New HIV diagnoses rising in New York City among men who have sex with men. New York, NY: 2007. DOH Press Release No. 079–07. [Google Scholar]
- New York City Department of Health and Mental Hygiene. HIV Epidemiology and Field Services Program. New York, NY: 2011. HIV/AIDS among men who have sex with men in New York City 2009. [Google Scholar]
- Newcomb ME, Mustanski B. Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: A meta-analysis. Archives of Sex Behavior. 2009;40(1):189–199. doi: 10.1007/s10508-009-9573-8. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health. 2012;102(1):156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Archives of Sexual Behavior. 2008;37(5):817–826. doi: 10.1007/s10508-007-9218-8. [DOI] [PubMed] [Google Scholar]
- Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among Seattle-Area injection drug users and young men who have sex with men. AIDS Education and Prevention. 2003;15(1):81–92. doi: 10.1521/aeap.15.1.81.23842. [DOI] [PubMed] [Google Scholar]
- Reece M. Sexual Compulsivity and HIV serostatus disclosure among men who have sex with men. Sexual Addiction and Compulsivity. 2003;10:1–11. [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education & Prevention. 2006;18(5):444–460. doi: 10.1521/aeap.2006.18.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, et al. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: Implications for age-specific interventions. AIDS and Behavior. 2009;13:811–821. doi: 10.1007/s10461-008-9439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savin-Williams RC. A critique of research on sexual minority-youths. Journal of Adolescents. 2001;24(1):5–13. doi: 10.1006/jado.2000.0369. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Zians J, Grant I, Patterson TL. Sexual compulsivity in a sample of HIV-positive methamphetamine-using gay and bisexual men. AIDS and Behavior. 2006;10(5):587–598. doi: 10.1007/s10461-006-9127-1. [DOI] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Sternberg M, Beardslee WR. Association of depression, self-esteem, and substance use with sexual risk among adolescents. Preventive Medicine. 2001;33:179–189. doi: 10.1006/pmed.2001.0869. [DOI] [PubMed] [Google Scholar]
- Siconolfi DE, Halkitis PN, Allomong TA, Burton CL. Body dissatisfaction & eating disorders in a sample of gay and bisexual men. International Journal of Men’s Health. 2009;8(3):254–264. [Google Scholar]
- Singer M. AIDS and the health crisis of the U.S. urban poor: The perspective of critical medical anthropology. Social Science and Medicine. 1994;39(7):931–48. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology. 1996;24:99–110. [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto: Addiction Research Foundation; 1996. [Google Scholar]
- Stall R, Friedman MS, Cantania JA. Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. New York: Oxford Univerisity Press; 2008. pp. 251–274. [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occuring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, Clark DA. Psychometric characteristics of the Beck Depression Inventory-II with college students. Measurement and Evaluation in Counseling and Development. 30:128–136. [Google Scholar]
- Storholm ED, Fisher DG, Napper LE, Reynolds GL, Halkitis PN. Proposing a tentative cut point for the compulsive sexual behavior inventory. Archives of Sexual Behavior. 2011;40(6):1301–1308. doi: 10.1007/s10508-010-9712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storholm ED, Fisher DG, Napper LE, Reynolds GL, Halkitis PN. A psychometric analysis of the compulsive sexual behavior inventory. Sexual Addiction & Compulsivity. 2011;18(2):86–103. doi: 10.1080/10720162.2011.584057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Hogg RS, Martindale SL, Cornelisse PGA, Craib KJP, Montaner JSG, et al. Determinants of sexual risk-taking among young HIV-negative gay and bisexual men. Journal of Acquired Immune Deficiency Syndromes. 1998;19(1):61–66. doi: 10.1097/00042560-199809010-00010. [DOI] [PubMed] [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- Watters JK, Biernacki P. Targeted sampling: Options for the study of hidden populations. Social Problems. 1989;36(4):416–430. [Google Scholar]
- Whisman MA, Perez JE, Ramel W. Factor structure of the Beck Depression Inventory-Second Edition (BDI-II) in a student sample. Journal of Clinical Psychology. 2000;56:545–551. doi: 10.1002/(sici)1097-4679(200004)56:4<545::aid-jclp7>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Wilson PA, Stadler G, Boone MR, Bolger N. Fluctuations in depression and well-being are associated with sexual risk episodes among HIV-positive men. Health Psychology. 2014;33(7):681–685. doi: 10.1037/a0035405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sexually Transmitted Diseases. 2005;32(7):458–463. doi: 10.1097/01.olq.0000168280.34424.58. [DOI] [PubMed] [Google Scholar]