Abstract
Objective
Humanitarian organisations care for burns during crisis and while supporting healthcare facilities in low- and middle-income countries. This study aimed to define the epidemiology of burn-related procedures to aid humanitarian response. In addition, operational data collected from humanitarian organisations are useful for describing surgical need otherwise unmet by national health systems.
Methods
Procedures performed in operating theatres run by MSF Operations Centre Brussels (MSF-OCB) from July 2008 through June 2014 were reviewed. Surgical specialist missions were excluded. Burn procedures were quantified, related to demographics and reason for humanitarian response and described.
Results
A total of 96,239 operations were performed at 27 MSF-OCB projects in 15 countries between 2008 – 2014. Of the 33,947 general surgical operations, 4,280 (11%) were for burns. This proportion steadily increased from 3% in 2008 to 24% in 2014. People receiving surgical care from conflict relief missions had nearly twice the odds of having a burn operation compared to people requiring surgery in communities affected by natural disaster (aOR 1.94, 95%CI 1.46 – 2.58). Nearly 70% of burn procedures were planned serial visits to the theatre. A diverse skill-set was required.
Conclusion
Unmet humanitarian assistance needs increased US$ 400 million dollars in 2013 in the face of an increasing number of individuals affected by crisis and a growing surgical burden. Given the high volume of burn procedures performed at MSF-OCB projects and the resource intensive nature of burn management, requisite planning and reliable funding are necessary to ensure quality for burn care in humanitarian settings.
Keywords: Burns, Humanitarian, Operational research, Developing countries, Conflict, Disasters
Introduction
Humanitarian organisations provide care to ill, injured and vulnerable populations affected by conflict, disaster and disease around the world.(1) When local health systems are disrupted by complex humanitarian emergencies, humanitarian assistance requires treatment of the resultant unmet surgical needs in addition to the injuries and burns attributable to a given crisis.(2) For more than 40 years, Médecins Sans Frontières (MSF; Doctors Without Borders) has been delivering humanitarian assistance in more than 70 countries through over 400 programs.(3) MSF is divided into five operational centres, each capable of providing surgical care One of these operational centres is based in Brusssels, Belgium (MSF-OCB).
Surgical care is vital in early response to crisis and an essential component of fragile health systems.(4) Safe and effective surgery in low- and middle-income countries (LMICs) is made possible by well-trained staff, surgeons and anaesthetistis with a diverse array of skills to meet the need of the populations they serve.(2, 5) Among necessary skills are those needed for the care of burns.
Burns are a major cause of morbidity and mortality worldwide, particularly in LMICs and during crisis.(6) Burn care presents particular challenges for humanitarian organisations given the frequent need for critical care, serial operations, long hospitalizations and rehabilitation (Table 1).(7) Moreover, burn survivors are often left with devastating physical and psychological sequelae that make reintegration to their community difficult.(8) Though the mission of MSF is to deliver quality emergency aid during acute crisis, knowledge of total burn care is important for patients’ ultimate wellbeing.
Table 1.
Procedures and services often required for serious burn injury and challenges faced when developing humanitarian assistance programs in under-resourced settings.
| Phase of Burn Care | Procedures | Services | Under-resourced settings’ challenges |
|---|---|---|---|
| Resuscitation | |||
| Airway management Venous access Escharotomy Wound care Amputation |
Clinician Nursing Nutrition Blood bank Dialysis Critical care |
Prolonged pre-hospital times results in significant physiologic derangements commonly.(20) Lack of anesthetists and specialist clinicians, as well as blood banking, dialysis and critical care capacity.(16, 24–26) |
|
| Excision and grafting | |||
| Debridement Grafting Surgical immobilisation Tissue flap coverage |
Anesthesia Surgery |
Serial operations require significant theatre usage, often one theatre in district hospitals.(24) Clinician performing surgeries are often not trained in burn debridement and skin grafting or lack the necessary equipment.(16) |
|
| Rehabilitation | |||
| Dressing changes Splinting |
Physiotherapy Occupational therapy Mental health |
Specialist therapies (i.e. occupational, hand, speech/language) and mental health are largely absent.(27–29) | |
| Reconstruction | |||
| Contracture release Scar revision |
Plastic surgery | Specialist surgeons are few, particularly during times of humanitarian emergency.(16, 20) | |
| Reintegration | |||
| Social work | Social work often absent, difficult to dedicate resources to reintegration during humanitarian crisis. | ||
With funding not increasing in proportion with the marked increase in humanitarian need, anticipating the cost of providing assistance has never been more important.(9) This study aimed to characterize the volume and types of procedures for burn care provided at MSF-OCB facilities over six years. Understanding this operative epidemiology will aid effective resource allocation and preparation of humanitarian staff likely to care for burned victims.
Methods
Data collection
All procedures performed in an operating theatre managed by MSF-OCB worldwide are recorded using a standardized Patient Surgical Record (PSR). The Record was developed by MSF for operational research needs, not clinical research. Therefore, patient-specific clinical data or burn particulars are not recorded in detail. PSR variables include: age, gender, American Society of Anesthesia physical status score, condition requiring surgery, type of procedure(s) performed, operating theatre time, perioperative death (death from induction of anesthesia to recovery room discharge) and program site. In addition, brief descriptive operative notes were occasionally written and are described where available. The Record is transcribed monthly into a database (Excel; Microsoft, Redmond, WA) and transmitted to MSF-OCB headquarters in Brussels, Belgium. At headquarters, the Surgical, Anesthesia, Gynecology and Emergency Medicine (SAGE) Unit review all data for completeness and accuracy. Discrepancies, missing data and questions are immediately corrected after reconciliation with program personnel.
Data analysis
Orthopedic, obstetric, gynecologic and sub-specialty projects (including plastic and reconstructive projects) were excluded to demonstrate the incidence of burn procedures among general surgical operations. Operations from July 2008 through June 2014 were combined and analyzed with descriptive statistics (Stata; College Station, TX). Logistic regression, adjusted for covariates age, gender and project, was performed to examine the relationship between each covariate and having undergone an operation for burn injury.
The reason for MSF-OCB assistance at each was characterized as natural disaster, hospital support or conflict. Programs not caring for those immediately injured or burned as a result of widespread conflict or natural disaster were considered to be hospital support. There is some overlap between the reasons for assistance. For instance, conflict in fragile states often lead to prolonged complex humanitarian emergencies that require hospital support despite no ongoing conflict.
Ethics
This retrospective description of de-identified, routinely collected data satisfied criteria for exemption from MSF Ethical Review Board. The Johns Hopkins Bloomberg School of Public Health Institutional Review Board provided ethical approval for analysis of the anonymous database.
Results
A total of 96,239 operations were performed at 27 MSF-OCB sites in 16 countries between 2008 and 2014 (Table 2). Specialists in obstetrics and gynaecology, orthopaedics, urology and sub-specialties performed 62,292 operations. Of the 33,947 general surgical operations, 4,280 (11%) were for burns. The proportion of general surgical procedures to care for burns increased annually from 2008 to 2014. In 2008, burn surgeries accounted for 3% of MSF-OCB general surgical operative volume. In 2013 the proportion was 17% and from January to June 2014 24% of general surgical operations were for burns (Figure 1).
Table 2.
Countries in which Médecins Sans Frontières Operations Centre Brussels provided surgical assistance from 2008 – 2014.
| Country |
|---|
| Afghanistan |
| Central African Republic |
| Chad |
| Côte d’Ivoire |
| Democratic Rep. of the Congo |
| Haiti |
| India |
| Kenya |
| Mali |
| Mauritania |
| Pakistan |
| Philippines |
| Somalia |
| South Sudan |
| Sudan |
| Syria |
Figure 1.
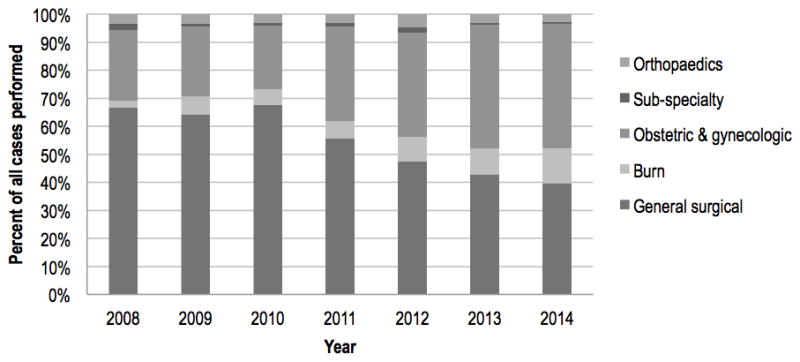
Percent of total operations performed by MSF-Operations Centre Brussels from 2008 to 2014.
Children requiring surgical care ages 6 months to 3 years had the greatest odds of needing a burn operation (aOR 7.82, 95%CI 4.23 – 14.51) compared to infants less than 6 months of age. Having a burn operation was less common with increasing age. Of those undergoing an operation, females were more likely to require a burn procedure than males (aOR 1.58, 95%CI 1.40 – 1.77). People receiving surgical care from missions acutely affected by conflict had nearly twice the odds of having a burn operation compared to people in communities affected by natural disaster (aOR 1.94, 95%CI 1.46 – 2.58). (Table 3)
Table 3.
Characteristics of general surgical and burn operations performed by MSF-Operations Centre Brussels from 2008 to 2014.
| General operations
|
Burns
|
Adj. odds ratios
|
||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | OR | 95% CI | |
|
Age
| ||||||
| <6 months | 367 | (92) | 30 | (8) | Referent | |
| 6 mos – 3 yrs | 1,384 | (61) | 876 | (39) | 7.82 | (4.23 – 14.51) |
| 3 – 12 yrs | 5,475 | (76) | 1,735 | (24) | 3.25 | (1.76 – 6.00) |
| 13 – 18 yrs | 2,761 | (91) | 261 | (9) | 1.21 | (0.64 – 2.31) |
| 18 – 50 yrs | 18,433 | (94) | 1,252 | (6) | 0.70 | (0.38 – 1.29) |
| ≥50 yrs | 5,514 | (98) | 138 | (2) | 0.28 | (0.15 – 0.56) |
|
| ||||||
|
Gender
| ||||||
| Male | 22,127 | (90) | 2,343 | (10) | Referent | |
| Female | 11,807 | (86) | 1,950 | (14) | 1.58 | (1.40 – 1.77) |
|
| ||||||
|
Mission type
| ||||||
| Natural disaster | 2,718 | (94) | 168 | (6) | Referent | |
| Hospital support | 18,897 | (91) | 1,923 | (9) | 1.17 | (0.88 – 1.55) |
| Conflict | 12,041 | (84) | 2,201 | (16) | 1.94 | (1.46 – 2.58) |
|
| ||||||
| Total | 33,934 | (89) | 4,293 | (11) | ||
Adj – adjusted for age, gender, cause for humanitarian response and site; OR – odds ration; CI – confidence interval
Of the 4,280 burn procedures, 1,261 (29%) were initial operations, 3,043 (69%) were planned serial procedures and 6 (<1%) were unplanned returns to the operating theatre. Consistent with the age distribution, most burn procedures were performed on otherwise healthy patients (62%) or those with only mild systemic disease (34%). Ninety percent of burn procedures were done safely under general anesthesia without a definitive airway. The median operating theatre time was 30 minutes (IQR 10 – 210 min). There were only two perioperative deaths (0.05%) (Table 4).
Table 4.
Operative details of burn operations performed by MSF-Operations Centre Brussels from 2008 to 2014.
| Burns
|
||
|---|---|---|
| n | (%) | |
|
Operation
| ||
| Initial | 1,261 | (29) |
| Planned return | 3,043 | (71) |
| Unplanned return | 6 | (<1) |
|
| ||
|
ASA class
| ||
| I | 2,569 | (11) |
| II | 1,407 | (13) |
| III | 174 | (8) |
| IV | 15 | (4) |
| V | 1 | (2) |
|
| ||
|
Anesthetic
| ||
| GA without airway | 3,893 | (90) |
| GA with airway | 134 | (3) |
| Spinal or regional | 83 | (2) |
| Other | 200 | (5) |
|
| ||
| OT time; median (IQR) | 30 | (10 – 210) |
|
| ||
| Perioperative deaths | 2 | (<1) |
ASA – American Society for Anesthesia; GA – general anaesthesia; OT – operating theatre; Perioperative deaths are those that occurred in the operating theatre or in the post-anaesthetic recovery area; IQR – interquartile range
There were only 1,941 burn procedures with brief operative notes (45%). Burns ranged from 1 to 95% total burn surface area. There were 1,060 skin grafting procedures (1% of general surgical operations), 22 major amputations, 16 sub-specialist reconstructive procedures and 9 escharotomies. On January 31st 2009 a fuel-tanker exploded in Nakuru, Kenya. MSF-OCB responded and cared for 89 patients. In addition to the above procedures, MSF-OCB performed 80 operations on 31 people, including 39 split-thickness skin grafts, 21 debridements, 7 escharotomies, 4 contracture releases and 3 amputations. This experience has been described.(10)
Discussion
Burns procedures are among the most common reasons for theatre usage in humanitarian settings. Given the burden of burns and frequent need for serial operations, burn injuries require significant infrastructure, human and material resources. In addition, burns demand multidisciplinary care and surgical knowledge of an array of procedures, which is challenging in austere environments.
Consistent with usual burn epidemiology in LMICs, children and women remain the groups most likely to require burn procedures in the humanitarian context.(11) Though burn procedures were more common in conflict-related missions, they are also common among MSF-OCB-supported hospitals and during natural disasters reflecting the high background incidence of burns in LMICs.(12–18) Operational decisions of national and humanitarian organisations undertaking surgical programs should consider the burden and distribution of burns within their community. This is particularly important for programs operating in conflict settings, where burn procedures account for up to a quarter of the operative volume. In addition, areas with extraordinary burn burden and frequent burn disasters, like sub-Saharan Africa and South Asia, require special attention.(10, 12, 19, 20) Given the high incidence and prevalence of burn injury and complications in LMICs, allocating resources essential for burn care is important for effective humanitarian assistance.
In LMICs, nearly 40% of burned don’t present for medical treatment.(18) Of those that seek and have access to care, a high-proportion requires surgical management.(15, 17, 18) Though the majority of LMIC hospitals have capacity to provide basic burn resuscitation, only a third of hospitals are able to provide excision and grafting and care for burn complications.(16) Given that severe injury, delayed presentation and burn sequelae are prevalent in LMICs, particularly those affected by conflict, providing humanitarian assistance to hospitals may significantly reduce burn death and disability.
Unlike other conditions that are treated by a single operation, burns often require serial procedures. In addition, even small burns across joints or on the hands, face or genitals can require specialized and resource-intensive care.(21) Therefore, humanitarian surgical programs should be prepared for the disproportionate operative volume burn injuries require. Moreover, clinicians preparing for humanitarian missions should ensure they are equipped with the basic knowledge and skills necessary for burn management. Lastly, national and humanitarian organisations expert in healthcare capacity development should have burn prevention and rehabilitation services incorporated into their surgical programs. Under-resourcing burn injury risks an unacceptably high rate of morbidity and mortality and compounds the challenges of functional recovery in LMICs.(22)
This study analysed routinely collected operational data making description of clinical specifics, burn details and outcomes not possible. However, the data are useful for those assessing surgical capacity needs in LMICs and humanitarian settings. Burn care requires a comprehensive program, ideally including prevention, critical care, rehabilitation and mental health services. This study was unable to describe MSF-OCB’s other burn-related activities given the procedural data. However, multidisciplinary strategy is an integral part of programs caring for burns in any context. Although the lack of granularity and significant number of missing operative notes precluded detailed assessment of specific burn procedures, this is the largest examination of humanitarian surgical burn treatment published and contributes to the operationalization of burn care in equivalent settings.
Conclusion
Unmet humanitarian assistance needs increased US$ 400 million dollars in 2013 in the face of an increasing number of individuals affected by crisis and a growing surgical burden.(4, 9, 23) Characterizing the volume and nature of procedures performed by humanitarian programs in LMICs using operational data can estimate requirements for providing care. Given the high volume of burn procedures performed at MSF-OCB projects and the resource intensive nature of burn management, requisite planning and reliable funding are necessary to ensure quality for burn care in humanitarian settings.
Acknowledgments
Funding: Operational and data collection funding was done through Médecins Sans Frontières. Data analysis and manuscript preparation was done with funding from the Fogarty International Center through the Northern Pacific Global Health Research Fellows Training Consortium under grant number R25TW009345.
We thank the dedicated national and international staff who provided the expertise and care for these patients. In addition, we thank all of those involved in data collection and management for their contribution to those who will require humanitarian surgical care in the future.
Footnotes
Conflict of interest: Outside of the authors’ relationship with Médecins Sans Frontières there are no conflicts of interest.
References
- 1.Chu K, Rosseel P, Trelles M, Gielis P. Surgeons without borders: a brief history of surgery at Medecins Sans Frontieres. World journal of surgery. 2010;34(3):411–4. doi: 10.1007/s00268-009-0187-z. [DOI] [PubMed] [Google Scholar]
- 2.Wong EG, Trelles M, Dominguez L, Gupta S, Burnham G, Kushner AL. Surgical skills needed for humanitarian missions in resource-limited settings: Common operative procedures performed at Medecins Sans Frontieres facilities. Surgery. 2014 doi: 10.1016/j.surg.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 3.International Activity Report: 2012. Médecins Sans Frontières 2012.
- 4.Mock C. Confronting the global burden of surgical disease. World journal of surgery. 2013;37(7):1457–9. doi: 10.1007/s00268-013-2102-x. [DOI] [PubMed] [Google Scholar]
- 5.Watters DA, Hollands MJ, Gruen RL, Maoate K, Perndt H, McDougall RJ, et al. Perioperative Mortality Rate (POMR): A Global Indicator of Access to Safe Surgery and Anaesthesia. World journal of surgery. 2014 doi: 10.1007/s00268-014-2638-4. [DOI] [PubMed] [Google Scholar]
- 6.Spinella PC, Borgman MA, Azarow KS. Pediatric trauma in an austere combat environment. Critical care medicine. 2008;36(7 Suppl):S293–6. doi: 10.1097/CCM.0b013e31817da99f. [DOI] [PubMed] [Google Scholar]
- 7.Roudsari BS, Shadman M, Ghodsi M. Childhood trauma fatality and resource allocation in injury control programs in a developing country. BMC public health. 2006;6:117. doi: 10.1186/1471-2458-6-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rossi LA, da Vila VS, Zago MM, Ferreira E. The stigma of burns Perceptions of burned patients’ relatives when facing discharge from hospital. Burns : journal of the International Society for Burn Injuries. 2005;31(1):37–44. doi: 10.1016/j.burns.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Buston O, Smith K, Stirk C, Sparks D, Malerba D, Sweeney H, et al. Global Humanitarian Assistance Report 2013. Bristol, UK: Global Humanitarian Assistance: A Development Initiative; 2013. [Google Scholar]
- 10.van Kooij E, Schrever I, Kizito W, Hennaux M, Mugenya G, Otieno E, et al. Responding to major burn disasters in resource-limited settings: lessons learned from an oil tanker explosion in Nakuru, Kenya. The Journal of trauma. 2011;71(3):573–6. doi: 10.1097/TA.0b013e3181febc8f. [DOI] [PubMed] [Google Scholar]
- 11.Daisy S, Mostaque AK, Bari TS, Khan AR, Karim S, Quamruzzaman Q. Socioeconomic and cultural influence in the causation of burns in the urban children of Bangladesh. The Journal of burn care & rehabilitation. 2001;22(4):269–73. doi: 10.1097/00004630-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 12.IHME. Data Visualizations. Seattle, WA: 2013. [cited 2014 2/7/2014]. Available from: http://vizhub.healthdata.org/gbd-cause-patterns/ [Google Scholar]
- 13.Ahuja RB, Goswami P. Cost of providing inpatient burn care in a tertiary, teaching, hospital of North India. Burns : journal of the International Society for Burn Injuries. 2013;39(4):558–64. doi: 10.1016/j.burns.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Edwards MJ, Lustik M, Burnett MW, Eichelberger M. Pediatric inpatient humanitarian care in combat: Iraq and Afghanistan 2002 to 2012. Journal of the American College of Surgeons. 2014;218(5):1018–23. doi: 10.1016/j.jamcollsurg.2013.12.050. [DOI] [PubMed] [Google Scholar]
- 15.Groohi B, Alaghehbandan R, Lari AR. Analysis of 1089 burn patients in province of Kurdistan, Iran. Burns : journal of the International Society for Burn Injuries. 2002;28(6):569–74. doi: 10.1016/s0305-4179(02)00099-2. [DOI] [PubMed] [Google Scholar]
- 16.Gupta S, Wong E, Mahmood U, Charles AG, Nwomeh BC, Kushner AL. Burn management capacity in low and middle-income countries: A systematic review of 458 hospitals across 14 countries. International journal of surgery. 2014 doi: 10.1016/j.ijsu.2014.08.353. [DOI] [PubMed] [Google Scholar]
- 17.Lau YS. An insight into burns in a developing country: a Sri Lankan experience. Public health. 2006;120(10):958–65. doi: 10.1016/j.puhe.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Wong EG, Groen RS, Kamara TB, Stewart KA, Cassidy LD, Samai M, et al. Burns in Sierra Leone: A population-based assessment. Burns : journal of the International Society for Burn Injuries. 2014 doi: 10.1016/j.burns.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Carlson LC, Rogers TT, Kamara TB, Rybarczyk MM, Leow JJ, Kirsch TD, et al. Petroleum pipeline explosions in sub-Saharan Africa: A comprehensive systematic review of the academic and lay literature. Burns : journal of the International Society for Burn Injuries. 2014 doi: 10.1016/j.burns.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Ahuja RB, Bhattacharya S. Burns in the developing world and burn disasters. Bmj. 2004;329(7463):447–9. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mandal A. Quality and cost-effectiveness--effects in burn care. Burns : journal of the International Society for Burn Injuries. 2007;33(4):414–7. doi: 10.1016/j.burns.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 22.Mashreky SR, Rahman A, Chowdhury SM, Giashuddin S, Svanstrom L, Linnan M, et al. Consequences of childhood burn: findings from the largest community-based injury survey in Bangladesh. Burns : journal of the International Society for Burn Injuries. 2008;34(7):912–8. doi: 10.1016/j.burns.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Stewart B, Khanduri P, McCord C, Ohene-Yeboah M, Uranues S, Vega Rivera F, et al. Global disease burden of conditions requiring emergency surgery. The British journal of surgery. 2014;101(1):e9–22. doi: 10.1002/bjs.9329. [DOI] [PubMed] [Google Scholar]
- 24.Galukande M, von Schreeb J, Wladis A, Mbembati N, de Miranda H, Kruk ME, et al. Essential surgery at the district hospital: a retrospective descriptive analysis in three African countries. PLoS medicine. 2010;7(3):e1000243. doi: 10.1371/journal.pmed.1000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kingham TP, Kamara TB, Cherian MN, Gosselin RA, Simkins M, Meissner C, et al. Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Archives of surgery. 2009;144(2):122–7. doi: 10.1001/archsurg.2008.540. discussion 8. [DOI] [PubMed] [Google Scholar]
- 26.Ozgediz D, Jamison D, Cherian M, McQueen K. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bulletin of the World Health Organization. 2008;86(8):646–7. doi: 10.2471/BLT.07.050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawkins Z, Tilman T. “The family is the clinic, the community is the hospital”: community mental health in Timor-Leste. Australasian psychiatry : bulletin of Royal Australian and New Zealand College of Psychiatrists. 2011;19(Suppl 1):S95–7. doi: 10.3109/10398562.2011.583067. [DOI] [PubMed] [Google Scholar]
- 28.McBain R, Salhi C, Morris JE, Salomon JA, Betancourt TS. Disease burden and mental health system capacity: WHO Atlas study of 117 low- and middle-income countries. The British journal of psychiatry : the journal of mental science. 2012;201(6):444–50. doi: 10.1192/bjp.bp.112.112318. [DOI] [PubMed] [Google Scholar]
- 29.O’Brien L, Hardman A. Developing hand therapy skills in Bangladesh: experiences of Australian volunteers. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2014;27(1):30–7. doi: 10.1016/j.jht.2013.09.006. [DOI] [PubMed] [Google Scholar]


