Abstract
Objectives
To investigate whether the use of antihypertensive and statin medication in very old adults is associated with the level of motor performance.
Design
Cross sectional study.
Settings
A community-based study recruited from over 40 residential facilities across the metropolitan Chicago area.
Participants
Community dwelling very old adults (n=1520; mean age 80.2; SD 7.7).
Measurements
Eleven motor performances were summarized using a composite motor score. All prescription and over the counter medications taken by participants were inspected and coded using the Medi-Span Data Base System. Demographic characteristics and medical history were obtained via detailed interview and medical exams.
Results
In multiple linear regression models, antihypertensive medications were associated with global motor score (β=−0.075, S.E. 0.011, p<0.001). Thus, motor function in an individual with antihypertensive medication, was on average, about 7.5% lower than an age, sex and education matched individual without antihypertensive medication. The number of antihypertensive medications which were being used had an additive effect, such that a reduction in the level of motor function was observed with each additional medication, and receiving three or more antihypertensive medications was associated with about a 15% reduction in the level of motor function. The association between antihypertensive medications and motor function was robust, and remained unchanged after adjusting for confounding by indication using several potentially confounding variables: smoking, hypertension, diabetes, stroke, congestive heart-failure, myocardial infarction, and intermittent claudication (β=−0.05, S.E. 0.015, p=0.001). In contrast, the use of statin medications was not related to motor function (unadjusted: β=0.003, S.E.=0.015, p=0.826; fully adjusted: β=0.018, S.E. 0.014, p=0.216).
Conclusion
The use of antihypertensive medications is associated with a lower level of motor function in very old adults. The nature of this association warrants further investigation.
Keywords: motor performance, medications, antihypertensive, statins, elderly
Introduction
Loss of motor function is common in older adults and associated with a wide range of adverse health outcomes, including increased risk for disability, cognitive decline and mortality.1,2,3 Identifying risk factors for late-life motor impairment is crucial for efforts to mitigate its growing personal and societal burden in our aging population. Several medications commonly used by elderly people can potentially influence the rate and extent of late-life motor impairment.
Cardiovascular and cerebrovascular diseases are common and increase with age, affecting as many as 80% of individuals over the age of 80.4 Cardiovascular risk factors are prevalent among older adults. Age adjusted hypertension prevalence in the U.S. is estimated at 75% for older women, and 65% for older men,4 while dyslipidemia has been reported in 34% of persons over the age of 75.5 Based on clinical trials, over the last 3 decades, public health efforts have focused on treatment for hypertension and dyslipidemia to reduce mortality in older adults. These public health efforts are probably a significant driving force behind the extensive use of prescription medications, particularly antihypertensive and statin medications, among older adults, many of whom report the use of 5 or more medications and supplements.6 Antihypertensive and statin medications are known to affect physiological parameters related to motor function.7,8 Although many older adults receive these medications6 there are few studies which have examined the association between these medications and motor function in very old adults. Furthermore, prior observational studies have not reported a consistent association between individuals who use these medications and motor function in older adults. 7,9,10
We used data from more than 1500 participants in the Rush Memory and Aging Project, a community-based study of risk factors for common chronic conditions of aging, to assess whether the use of antihypertensive or statin medications is associated with the level of motor function in community dwelling older adults.
Methods
Participants
All participants were from the Rush Memory and Aging Project, a community-based, longitudinal clinical-pathologic investigation of chronic conditions of old age. Participants were recruited from more than 40 residential facilities across the metropolitan Chicago area, including subsidized senior housing facilities, retirement communities, and retirement homes, in addition to social service agencies and Church groups. Participants agreed to annual detailed clinical evaluations, and all evaluations were performed at the parent facility or the participants’ homes to reduce burden and enhance participation. The study was conducted in accordance with the latest version of the Declaration of Helsinki and was approved by the Institutional Review Board of Rush University Medical Center.
The Memory and Aging Project began in 1997 and through July, 2013 enrolled 1635 participants. Eligibility for these analyses required completed review of medications and baseline motor assessment. We excluded 115 cases (7%) that had not completed their baseline assessment or were missing a valid motor evaluation or medication review, leaving 1520 individuals for these analyses.
Assessment of Antihypertensive & Statin Medications
At baseline, study personnel recorded data regarding medication use by direct visual inspection of all containers of prescription and over-the-counter medication allowing for the documentation of all medications taken for at least the 2 weeks prior to the evaluation. Medications were subsequently coded using the Medi-Span Drug Data Base system. A master list of medications defined as having antihypertensive properties (including beta blockers, calcium channel blockers, ACE inhibitors, angiotensin receptor blockers, diuretics) and statins was constructed. For these analyses, we stratified participants into two groups. The analysis of antihypertensive medications compared participants who used one or more antihypertensive medications with participants not using any antihypertensive medications. The analysis of statin medication compared participants using statin medication to participants not using statin medication.
Assessment of Motor Function
Motor performance was assessed by a battery of 11 tests including bilateral grip and pinch strength, bilateral Purdue Pegboard score, bilateral tapping score, Gait (time and number of steps to walk 8 feet and turn 360°), and balance (time to stand on each leg and then on toes for 10 seconds and the number of steps off line when walking an 8 foot line in a heel to toe manner). These 11 performances were scaled and averaged to obtain a summary global motor score as previously described.3
Clinical and Cognitive Testing
Subjects underwent a uniform structured clinical evaluation, including a medical history, neurologic examination, and cognitive performance testing. Details of the clinical evaluation have been described.11 Cognitive function was assessed at each evaluation via a battery of 21 tests. Participants were evaluated in person by a physician, who used all available cognitive and clinical testing results to diagnose dementia. The diagnosis of dementia followed the criteria of the joint working group of the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association.12
Other Covariates
Demographic characteristics, such as age, sex and education (reported highest grade or years of education), were obtained at baseline. Medical history (including smoking history, hypertension, diabetes, stroke, congestive heart-failure, myocardial infarction and intermittent claudication) was obtained via detailed interview by trained personnel, as well as medical exams (for stroke) and inspection of medications (for diabetes).
Statistical Analysis
We employed t-test and chi-square to compare the clinical characteristics of individuals who used or did not use antihypertensive or statin medications. We used linear regression models to examine the association between medications and global motor score. To examine the association between the number of medications and global motor score, we employed Kruskal-Wallis with post-hoc Mann-Whitney tests, with Bonferroni corrections for multiple comparisons.
Multiple linear regression models were used to study the association between antihypertensive medication or statin medication, motor function and other covariates. In addition, subgroup analyses were performed to study the associations between the different pharmacological classes of the antihypertensive medications and motor function. Models were examined graphically and analytically and assumptions were judged to be adequately met. Data were analyzed using SPSS Statistics (IBM® Corporation, summers, NY) version 20.
Results
Descriptive Properties of Antihypertensive and Statin Medication use
These analyses included 1520 elderly participants. About 60% of the participants used antihypertensive medication (n=925; 60.9%), 365 (24%) used one medication, 331(22%) used two, and 229 (15%) used 3 or more medications. About 30% used statin medication. Over 20% of the participants used both antihypertensive and statin medications.
Individuals using antihypertensive medication were older than those not receiving medication. Individuals with antihypertensive medication and individuals with statin medications were less educated and had more vascular risk factors and diseases, compared to individuals not using these medications (Tables 1a & 1b). There were no significant differences in terms of gender between the groups.
Table 1a.
Antihypertensive medication users and non-users characteristics
| Variable* | Antihypertensive Users (n=925) | Antihypertensive Non-Users (n=595) |
|---|---|---|
| Age | 80.9 (7.3) | 79.0 (8.2) |
| Female | 666 (72.0) | 462 (77.6) |
| Years of education | 14 | 15 |
| Smoking | 387 (42.0) | 236 (39.7) |
| Hypertension | 682 (73.7) | 132 (22.2) |
| Diabetes mellitus | 169 (18.3) | 38 (6.4) |
| Stroke | 100 (10.8) | 41 (6.9) |
| Congestive heart failure | 58 (6.3) | 9 (1.5) |
| Myocardial infarction | 133 (14.4) | 30 (5.1) |
| Claudication | 78 (8.4) | 28 (4.7) |
Mean (SD) or N (%).
Table 1b.
Statin medication users and non-users characteristics
| Variable* | Statin Users (n=455) | Statin Non-Users (n=1065) |
|---|---|---|
| Age | 79.1 (7.4) | 80.2 (7.8) |
| Female | 322 (70.8) | 806 (71.5) |
| Years of education | 14 | 15 |
| Smoking | 197 (31.6) | 426 (40.1) |
| Hypertension | 288 (63.3) | 526 (49.4) |
| Diabetes mellitus | 102 (22.4) | 105 (9.9) |
| Stroke | 58 (12.7) | 83 (7.8) |
| Congestive heart failure | 31 (6.8) | 36 (3.4) |
| Myocardial infarction | 89 (19.6) | 74 (7.0) |
| Claudication | 40 (8.8) | 66 (6.2) |
Mean (SD) or N (%).
Antihypertensive Medication and Global Motor Score
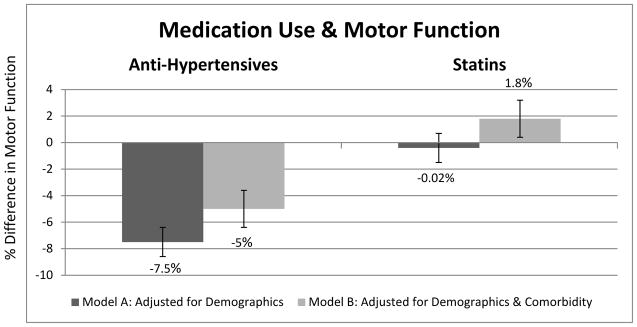
Global motor scores ranged from 0.34 to 1.64 with a higher score indicating better function, (mean 0.99, SD=0.26). In unadjusted analysis, antihypertensive medications were associated with global motor scores (β=−0.11, S.E. 0.013, p<0.001). In a multiple linear regression model which controlled for age, sex and education, antihypertensive medications were associated with global motor score (β=−0.075, S.E. 0.011, p<0.001) (Figure 1). Thus, motor function in an individual with antihypertensive medication, was on average, about 7.5% lower than an age, sex and education matched individual without antihypertensive medication.
Figure 1.
* Figure 1 presents % difference in motor function among users of antihypertensive and statin medication, compared to non-users, using multiple linear regression. Model A (adjusted for demographics) included age, sex, and education. Model B (adjusted for demographics and comorbidity) included age, sex, education smoking, hypertension, diabetes, stroke, congestive heart-failure, myocardial infarction, and intermittent claudication.
** p<0.001 for comparison between antihypertensive users and non-users
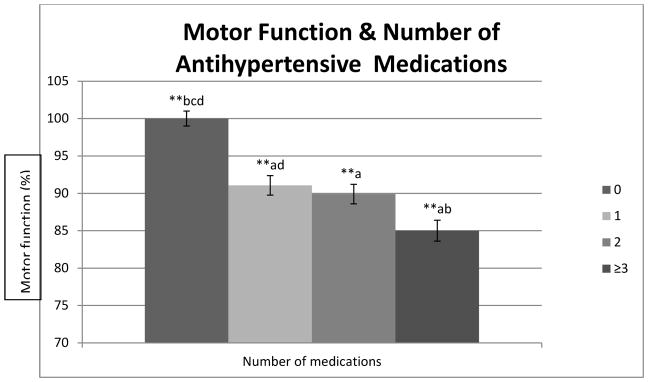
We further examined whether the number of antihypertensive medications affected the association with global motor scores. Kruskal-Wallis analysis revealed that an increase in the number of antihypertensive medications was associated with a greater reduction in global motor score (p<0.001). The reduction in the level of global motor scores is illustrated in Figure 2. Post-hoc analysis indicated non-users of antihypertensive medication had a significantly higher level of motor function compared to all groups of antihypertensive medication users, and users of ≥3 medications had a significantly lower level of motor function compared to non-users and users of 1 medication. Thus, while global motor scores were reduced about 9% in an individual receiving one antihypertensive medication, an individual receiving three or more antihypertensive medications showed a reduction of 15% in global motor score (p<0.001).
Figure 2. Number of medications & motor function*.
* Raw global motor scores have been transformed to illustrate the reduction of the level of global motor scores in individuals with 1 or more medications, compared to individuals not taking any antihypertensive medications.
** Indicate statistically significant difference in post-hoc analysis (p<0.05).
Vascular risks factors and diseases are associated with the level of motor function1,2 and are more prevalent among antihypertensive medication users. In a multiple linear regression analysis, antihypertensive medication remained associated with motor score after adjusting for vascular diseases and vascular disease risk factors, including smoking, hypertension, diabetes, stroke, congestive heart-failure, myocardial infarction, and intermittent claudication, in addition to the demographic factors reported for the initial model (β=−0.05, S.E. 0.015, p=0.001) (Figure 1).
We repeated the above analysis with each of the antihypertensive medication classes and found similar results across classes. Models adjusting for age, sex and education demonstrated significantly reduced motor function with diuretics (β =−0.075, S.E. 0.012, p<0.001, n=490), calcium channel blockers (β =−0.049, S.E. 0.014, p<0.001, n=306), beta blockers (β =−0.047, S.E. 0.013, p<0.001, n=367), and angiotensin related medication (β =−0.058, S.E. 0.012, p<0.001, n=476). In addition, the association between antihypertensive and motor function remained robust in a sensitivity analysis restricted to participants with no evidence of clinical dementia.
Statin Medication and Global Motor Score
In a linear regression model which controlled for age, sex and education, statin medications were not associated with global motor score (unadjusted: β=0.003, S.E. 0.015, p=0.826; fully adjusted: β=0.017, S.E. 0.014, p=0.216).
Discussion
We found that older adults taking antihypertensive medications had a 7.5% lower level of motor function compared to ages, sex and education matched adults not taking antihypertensive medication. The number of antihypertensive medications which were being used had an additive effect, such that a reduction in the level of motor function was observed with each additional medication, and receiving three or more antihypertensive medications was associated with about a 15% reduction in the level of motor function. This association was observed across the different antihypertensive medication classes.
Antihypertensive medications are indicated for the treatment of hypertension, and the treatment threshold and intensity is related to cardiovascular risk. Antihypertensive medications are also indicated in patients without hypertension in several settings, these include: the reduction of morbidity and mortality in patients after myocardial infarction, the reduction of morbidity and mortality in patients suffering from congestive heart failure, the treatment of congestive heart failure symptoms, and for the reduction of microvascular complications of diabetes. These medical conditions are likely linked to the degree of motor function and can therefore confound the observed link between antihypertensive medication and motor function. However, the association we identified between antihypertensive medications and motor function was robust, and remained unchanged after adjusting for demographics, co-morbidity and confounding by indication using several variables. These included – hypertension, diabetes, stroke, congestive heart-failure, myocardial infarction and intermittent claudication – as well as basic demographic characteristics. A similar association was not identified for statin medication, though these are often prescribed to patients with similar cardiovascular risk factors.
Medication use is prevalent among U.S. older adults. A survey in the United States of a representative sampling of 3005 community dwelling adults (aged 57 through 85 years)6 found at least one prescription medication was used by 81 percent, and that five or more prescription medications were used by 36 percent of people aged 75 to 85 years. The most commonly used medications were cardiovascular agents (including antihypertensive and statin medication).
A number of previous observational studies have investigated the association between exposure to antihypertensive medication and motor function in the elderly and have reported conflicting results.7,9,10 Our results extend prior studies in several important ways. First, we report an association between antihypertensive medications as a group and reduced motor function, while previous studies restricted their analysis to single pharmacological classes of antihypertensive medication. Second, the association we identified between antihypertensive medication use and motor function persisted even after controlling for a several important possible confounders. Third, our results indicate the number of antihypertensive medications being used had an additive effect to this link. Fourth, the link between antihypertensive medication and motor function was similar across antihypertensive classes. And lastly, statin medication use was not linked to motor function. Taken together, these findings can help advance our understanding of the relation between medication use and motor function in the very old, and inform interventions designed to maintain motor function in older adults. However, our results require further validation using longitudinal data.
The basis for the association we identified between antihypertensive medication and the level of motor function is uncertain. Our analysis adjusted for several medical conditions associated with the use of these medications, thus largely accounting for confounding by indication. However our analysis could not account for possible confounding by severity of these medical conditions, and therefore the observed differences in motor function between medication users and non-users could be due to differences in the severity of these conditions. In addition, antihypertensive medication may be a surrogate for other unmeasured underlying conditions disposing the individual to reduced motor function. While the use of antihypertensive medications may reduce the risk of vascular complication associated with hypertension, the fact that these individuals were given antihypertensive medication suggests that they may still have more underlying vascular pathology. Thus antihypertensive medication may serve as a marker for individuals at higher risk for the accumulation of a wide range of vascular pathologies in the central-nervous-system and in the periphery.
Alternatively, antihypertensive medications may directly influence motor function via central or peripheral motor pathways.8,13,14,15,16 However, our results indicate a similar association across classes of antihypertensive medication, and thus the underlying mechanism would likely involve an effect common to antihypertensive medication in general. Increasing evidence indicates that among the oldest old, use of antihypertensive medications and lower blood pressure may be associated with increased morbidity and mortality, 17,18,19,20 and paradoxically, that hypertension may actually be beneficial among certain subgroups of this population.21,22,23 Accordingly, there may be a need for higher blood pressure to obtain sufficient target organ perfusion in the elderly, possibly due to a change in auto-regulation mechanisms, or due to a need to overcome advanced arterial stiffness in older age.23 Hence, the link we identified between antihypertensive medication and motor function might represent a causal effect mediated by reduced cerebral, cardiovascular, or muscular perfusion.
This study has several strength and limitations. First, our study included a relatively large sample of both male and female persons with advanced age. Second, motor function was evaluated as part of a uniform clinical evaluation and incorporated many widely accepted and reliable strength and motor performance measures. The aggregation of multiple measures of motor function into a composite measure yielded a more stable measure of motor function and increased the statistical power to identify associations. Third, we did not limit our analysis to a single class of antihypertensive medication, and rather explored the association between the major antihypertensive medication classes and motor function, as a group as well as individually.
Although we attempted to control for potential confounders, it is still possible that the association we identified is a result of confounding by indication or severity, or of residual confounding from an unmeasured latent variable that is related to both antihypertensive medication and decline in motor function. In addition, it is difficult to assess whether the association identified is based on causality due to the cross-sectional model of our analysis. It should also be noted that from a risk-to-benefit perspective, the reduction in cardiovascular events and all-cause mortality reported in patients aged 80 years and older in the HYVET study,24 would likely negate the small reduction in motor performance due to antihypertensive treatment reported in this study, and that reduction in stroke by antihypertensive treatment of elderly persons would likely protect against a reduction in motor performance.
In conclusion, we found a robust association between antihypertensive medication use and the level of motor function in the elderly. Further research replicating our results and evaluating its clinical implications are warranted.
Acknowledgments
We would like to thank the participants and the staff of the Rush Memory and Aging Project and the Rush Alzheimer’s Disease Center for this work. This study was supported by NIH grant R01AG17917. The sponsors had no role in the conception, design, analysis, or interpretation of data or in the drafting, review, or approval of the manuscript. The Memory and Aging Study was approved by the Rush University Medical Center Institutional Review Board. Written informed consent was obtained from all study participants.
Footnotes
Conflicts of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Buchman A, Leurgans S, Boyle P, et al. Combinations of motor measures more strongly predict adverse health outcomes in old age: the rush memory and aging project, a community-based cohort. BMC Med. 2011;9(1):42. doi: 10.1186/1741-7015-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inzitari M, Carlo A, Baldereschi M, et al. Risk and predictors of motor-performance decline in a normally functioning population-based sample of elderly subjects: the Italian Longitudinal Study on Aging. J Am Geriatr Soc. 2006;54(2):318–324. doi: 10.1111/j.1532-5415.2005.00584.x. [DOI] [PubMed] [Google Scholar]
- 3.Buchman AS, Wilson RS, Boyle PA, et al. Change in motor function and risk of mortality in older persons. J Am Geriatr Soc. 2007;55(1):11–19. doi: 10.1111/j.1532-5415.2006.01032.x. [DOI] [PubMed] [Google Scholar]
- 4.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. [Accessed November 24, 2014];National Ambulatory Medical Care Survey: 2009 Summary Tables. http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2009_namcs_web_tables.pdf.
- 6.Qato DM, Alexander GC, Conti RM, et al. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300(24):2867–2878. doi: 10.1001/jama.2008.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott D, Blizzard L, Fell J, Jones G. The epidemiology of sarcopenia in community living older adults: what role does lifestyle play? J Cachexia Sarcopenia Muscle. 2011;2(3):125–134. doi: 10.1007/s13539-011-0036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wittbrodt ET. Drugs and myasthenia gravis. An update. Arch Intern Med. 1997;157(4):399–408. [PubMed] [Google Scholar]
- 9.Cao Y-J, Mager DE, Simonsick EM, et al. Physical and cognitive performance and burden of anticholinergics, sedatives, and ACE inhibitors in older women. Clin Pharmacol Ther. 2008;83(3):422–429. doi: 10.1038/sj.clpt.6100303. [DOI] [PubMed] [Google Scholar]
- 10.Ashfield TA, Syddall HE, Martin HJ, et al. Grip strength and cardiovascular drug use in older people: findings from the Hertfordshire Cohort Study. Age Ageing. 2010;39(2):185–191. doi: 10.1093/ageing/afp203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bennett DA, Schneider JA, Buchman AS, et al. The Rush Memory and Aging Project: study design and baseline characteristics of the study cohort. Neuroepidemiology. 2005;25(4):163–175. doi: 10.1159/000087446. [DOI] [PubMed] [Google Scholar]
- 12.McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 13.Ozkul Y. Influence of calcium channel blocker drugs in neuromuscular transmission. Clin Neurophysiol. 2007;118(9):2005–2008. doi: 10.1016/j.clinph.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Van Mil HG, Geukes Foppen RJ, Siegenbeek van Heukelom J. The influence of bumetanide on the membrane potential of mouse skeletal muscle cells in isotonic and hypertonic media. Br J Pharmacol. 1997;120(1):39–44. doi: 10.1038/sj.bjp.0700887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang DW, Mistry AM, Kahlig KM, et al. Propranolol blocks cardiac and neuronal voltage-gated sodium channels. Front Pharmacol. 2010;1:144. doi: 10.3389/fphar.2010.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker MR, Baker SN. Beta-adrenergic modulation of tremor and corticomuscular coherence in humans. PLoS One. 2012;7(11):e49088. doi: 10.1371/journal.pone.0049088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kamaruzzaman S, Watt H, Carson C, Ebrahim S. The association between orthostatic hypotension and medication use in the British Women’s Heart and Health Study. Age Ageing. 2010;39(1):51–56. doi: 10.1093/ageing/afp192. [DOI] [PubMed] [Google Scholar]
- 18.Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 19.Sabayan B, van Vliet P, de Ruijter W, et al. High blood pressure, physical and cognitive function, and risk of stroke in the oldest old: the Leiden 85-plus Study. Stroke. 2013;44(1):15–20. doi: 10.1161/STROKEAHA.112.663062. [DOI] [PubMed] [Google Scholar]
- 20.Mattila K, Haavisto M, Rajala S, Heikinheimo R. Blood pressure and five year survival in the very old. Br Med J (Clin Res Ed) 1988;296(6626):887–889. doi: 10.1136/bmj.296.6626.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rastas S, Pirttilä T, Viramo P, et al. Association between blood pressure and survival over 9 years in a general population aged 85 and older. J Am Geriatr Soc. 2006;54(6):912–918. doi: 10.1111/j.1532-5415.2006.00742.x. [DOI] [PubMed] [Google Scholar]
- 22.Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304(1):61–68. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sabayan B, Oleksik AM, Maier AB, et al. High blood pressure and resilience to physical and cognitive decline in the oldest old: the Leiden 85-plus Study. J Am Geriatr Soc. 2012;60(11):2014–2019. doi: 10.1111/j.1532-5415.2012.04203.x. [DOI] [PubMed] [Google Scholar]
- 24.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]