Abstract
Objective
We reviewed a multi-institutional database to assess the effect of enteral feeding with human milk on duration from initiation of feeds to discharge after gastroschisis repair.
Study design
Infants who had gastroschisis repair between 1997 and 2012 with data recorded in the Pediatrix Medical Group Clinical Data Warehouse were categorized into 4 groups based on the percentage of days they were fed human milk out of the number of days they were fed enterally. Cox proportional hazards regression modeling was performed to determine the adjusted effect of human milk on duration from initiation of feeds to discharge.
Results
Of 3082 infants, 659 (21%) were fed human milk on 0% of enteral feeding days, 766 (25%) on 1–50% of enteral feeding days, 725 (24%) on 51–99% of enteral feeding days, and 932 (30%) on 100% of enteral feeding days. Following adjustment, being fed human milk on 0% of enteral feeding days was associated with a significantly increased time to discharge compared with being fed human milk on 100% of enteral feeding days (HR for discharge per day: 0.46, 95% CI: 0.40–0.52). The same was found for infants fed human milk on 1–50% of enteral feeding days (HR: 0.37, 95% CI: 0.32–0.41) and for infants fed human milk on 51–99% of enteral feeding days (HR: 0.51, 95% CI: 0.46–0.57).
Conclusion
The use of human milk for enteral feeding of infants following repair of gastroschisis significantly reduces the time to discharge from initiation of feeds.
Keywords: gastroschisis, human milk, nutrition, hospitalization, enteral feeding, infants
Multiple studies have demonstrated the benefits of human milk over formula for the newborn infant1,2; these include improved absorption of nutrients, immunological defenses, and maternal-infant bonding.3–5 Such benefits are of great importance in the preterm infant, who is at a much higher risk for a host of complications, including respiratory difficulties, infections, and in-hospital mortality.6,7 Human milk use is associated with a decreased incidence of necrotizing enterocolitis (NEC), a complication associated with substantial morbidity and mortality.8
Gastroschisis—a congenital defect in the para-umbilical abdominal wall associated with evisceration of abdominal organs—has a much higher incidence in preterm vs. full-term infants.9 Previous work has demonstrated that enteral feeding with human milk after gastroschisis repair is beneficial and may help prevent NEC10. However, additional benefits with regards to the use of human milk in these infants have not been explored fully. Therefore, we investigated the association of enteral feeding with human milk and time to discharge after gastroschisis repair, using time to discharge as a surrogate for the incidence of complications and the ability of the infant to tolerate feeds. We hypothesized that human milk use would be associated with reduced time to discharge.
Methods
The study population was drawn from an electronic medical record that prospectively captures information generated by clinicians on all infants cared for by the Pediatrix Medical Group in neonatal intensive care units (NICUs) in North America. This information includes data on multiple aspects of care taken from admission notes, daily progress notes, and discharge summaries and includes maternal history, demographics, medications, laboratory results, diagnoses, and procedures. The data are then transferred to the Pediatrix Clinical Data Warehouse for quality improvement and research purposes.11 Permission to conduct this analysis was provided by the Duke University Institutional Review Board.
We included infants if they had a report of gastroschisis in the diagnosis table between 1997 and 2012. Infants were excluded if they did not receive human milk or formula at any point after gastroschisis repair, if they were discharged home on day of feeding 0 or 1, or if their postnatal age (PNA) at discharge was missing. Remaining infants were categorized a priori into 4 groups based on the percentage of days they received human milk out of their total days of enteral feeds: 0%, 1–50%, 51–99%, and 100%.
Definitions
We defined percentage of days fed as the percentage of days after gastroschisis repair during which infants received any amount of enteral nutrition. Percentage of human milk exposure was defined as the percentage of days fed during which an infant received any human milk. Human milk included both mother’s human milk as well as donor human milk. Daily inotropic support was considered to be any exposure to amrinone, dobutamine, dopamine, epinephrine, milrinone, or norepinephrine on a given day. We characterized daily mechanical ventilation as any exposure to conventional or high-frequency ventilation on a given day. Percentage of days of inotropic and mechanical ventilator support was calculated as the number of days of inotropic or mechanical ventilator support after the first feed divided by the number of days from first feed until discharge. We determined a positive blood culture to be any blood culture positive for an organism not typically considered a contaminant obtained on a day after the first feed. We defined small for gestational age (SGA) as previously described.12
Statistical Analyses
Baseline characteristics and outcomes were compared between groups using standard summary statistics including median (25th, 75th percentile) and frequency (percentage). Continuous variables were compared with the Kruskal-Wallis test, and categorical variables were compared with Fisher exact test or chi-square tests of association as appropriate. We used Kaplan-Meier estimators, censoring infants lost to follow up and death, to determine the association of human milk and time from first enteral feed to discharge. Time to discharge among groups was compared using the log-rank test. Cox proportional hazards regression modeling was performed to determine the adjusted association between human milk use and time from first feed to discharge. Covariates included in the model were PNA at first feed, number of days the infant was not being fed after starting feeds, GA, SGA, percentage of days the infant was on inotropes, percentage of days the infant was on the ventilator, and any positive blood culture after feeds began. The proportional hazards assumption was tested using goodness-of-fit tests based on Schoenfeld residuals, and all potential covariates were inspected for linearity using visual inspection and goodness-of-fit tests. We also conducted a sensitivity analysis limited to infants who were discharged within 3 weeks of their first feed to better ensure that our findings were not the result of unobserved confounding.
All statistical analyses were performed using Stata13.1 (College Station, TX). A p-value of 0.05 was used to determine statistical significance.
Results
Of 3082 infants, 659 (21%) were fed human milk on 0% of enteral feeding days, 766 (25%) on 1–50% of enteral feeding days, 725 (24%) on 51–99% of enteral feeding days, and 932 (30%) on 100% of enteral feeding days. On only 2.9% of feeding days was an infant fed both human milk and formula during 1 day. Infants in the 0% human milk group were more likely to be premature and African American (Table I). Infants fed 0% human milk were also significantly older on their first day of feeding compared with infants fed 100% human milk (median 13 days vs. 12 days, p<0.01).
Table I.
Baseline characteristics by group
| Variable | Overall N=3082 |
Human milk on 0% of enteral feeding days N=659 |
Human milk on 1– 50% of enteral feeding days N=766 |
Human milk on 51– 99% of enteral feeding days N=725 |
Human milk on 100% of enteral feeding days N=932 |
p |
|---|---|---|---|---|---|---|
| Gestational age (weeks) | <0.01 | |||||
| ≤28 | 20 (0.7%) | 5 (0.8%) | 6 (0.8%) | 5 (0.7%) | 4 (0.4%) | |
| 29–32 | 155 (5.0%) | 43 (6.5%) | 40 (5.2%) | 40 (5.5%) | 32 (3.4%) | |
| 33–36 | 1822 (59%) | 400 (61%) | 478 (62%) | 427 (59%) | 517 (56%) | |
| ≥37 | 1084 (35%) | 211 (32%) | 242 (32%) | 253 (35%) | 378 (41%) | |
| Birth weight <1500 g | 96 (3.1%) | 18 (2.7%) | 36 (4.7%) | 25 (3.4%) | 17 (1.8%) | <0.01 |
| SGA | 598 (19%) | 135 (21%) | 155 (20%) | 141 (19%) | 167 (18%) | 0.55 |
| Female | 1506 (49%) | 303 (46%) | 378 (49%) | 360 (50%) | 465 (50%) | 0.42 |
| Race/ethnicity | <0.01 | |||||
| White | 1622 (55%) | 349 (55%) | 368 (50%) | 382 (55%) | 523 (58%) | |
| Black | 212 (7.2%) | 74 (12%) | 48 (6.6%) | 50 (7.2%) | 40 (4.5%) | |
| Hispanic | 957 (32%) | 183 (29%) | 276 (38%) | 227 (33%) | 271 (30%) | |
| Other | 159 (5.4%) | 26 (5.3%) | 39 (5.3%) | 33 (4.8%) | 61 (6.8%) | |
| PNA at 1st feed | <0.01 | |||||
| <8 | 256 (8.3%) | 46 (7.0%) | 71 (9.3%) | 86 (12%) | 53 (5.7%) | |
| 8–14 | 1141 (37%) | 191 (29%) | 233 (30%) | 246 (34%) | 471 (51%) | |
| 15–21 | 946 (31%) | 180 (27%) | 242 (32%) | 241 (33%) | 283 (30%) | |
| >21 | 739 (24%) | 242 (37%) | 220 (29%) | 152 (21%) | 125 (13%) |
PNA = postnatal age; SGA = small for gestational age.
Median (25th, 75th percentile) time from first feed to discharge was shorter in infants fed human milk on 100% of enteral feeding days as compared with those fed human milk on 51–99%, 1–50%, and 0% of enteral feeding days (12 days [8, 17] vs. 19 days [13, 34] vs. 31 days [15, 60] vs. 20 days [11, 38], respectively, p<0.01). Compared with the other groups, infants fed 100% human milk also had significantly reduced rates of positive blood cultures and a reduced percentage of days on inotropes after beginning feeds (Table II). Lastly, infants who were fed 0% human milk had a significantly higher mortality than the other three groups.
Table II.
Outcomes by group
| Variable | Overall N=3082 |
Human milk on 0% of enteral feeding days N=659 |
Human milk on 1– 50% of enteral feeding days N=766 |
Human milk on 51– 99% of enteral feeding days N=725 |
Human milk on 100% of enteral feeding days N=932 |
P |
|---|---|---|---|---|---|---|
| Days from first feed to discharge or death | <0.01 | |||||
| <8 | 179 (5.8%) | 45 (6.8%) | 20 (2.2%) | 16 (2.2%) | 98 (10%) | |
| 8–14 | 949 (31%) | 166 (25%) | 140 (18%) | 187 (28%) | 456 (49%) | |
| 15–21 | 629 (20%) | 121 (18%) | 95 (12%) | 187 (26%) | 226 (24%) | |
| >21 | 1325 (43%) | 327 (50%) | 511 (67%) | 335 (46%) | 152 (16%) | |
| Days infant not fed after 1st feed | 3 (0, 13) | 4 (0, 16) | 12 (3, 27) | 3 (0, 13) | 0 (0, 4) | <0.01 |
| Weight gain from birth to discharge (g/d) | 19 (14, 24) | 20 (14, 26) | 20 (16, 25) | 19 (14, 24) | 17 (11, 22) | <0.01 |
| Positive blood culture after first feed | c318 (10%) | 78 (12%) | 138 (18%) | 70 (10%) | 32 (3.4%) | <0.01 |
| Percent of days on ventilator after 1st feed | <0.01 | |||||
| <25% | 1317 (43%) | 290 (45%) | 302 (40%) | 277 (39%) | 448 (48%) | |
| 25–49% | 920 (30%) | 203 (31%) | 230 (31%) | 205 (29%) | 282 (30%) | |
| 50–100% | 803 (26%) | 155 (24%) | 221 (29%) | 228 (32%) | 199 (21%) | |
| Percent of days on inotrope after 1st feed | 0.02 | |||||
| <25% | 2838 (93%) | 604 (93%) | 695 (92%) | 655 (92%) | 844 (95%) | |
| 25–49% | 145 (4.8%) | 25 (3.9%) | 45 (6.0%) | 38 (5.4%) | 37 (4.0%) | |
| 50–100% | 57 (1.9%) | 19 (2.9%) | 13 (1.7%) | 17 (2.4%) | 8 (0.9%) | |
| Necrotizing Enterocolitis | 1 (0.0%) | 1 (0.2%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.30 |
| Mortality | 31 (1.1%) | 16 (2.6%) | 5 (0.7%) | 6 (0.9%) | 4 (0.4%) | <0.01 |
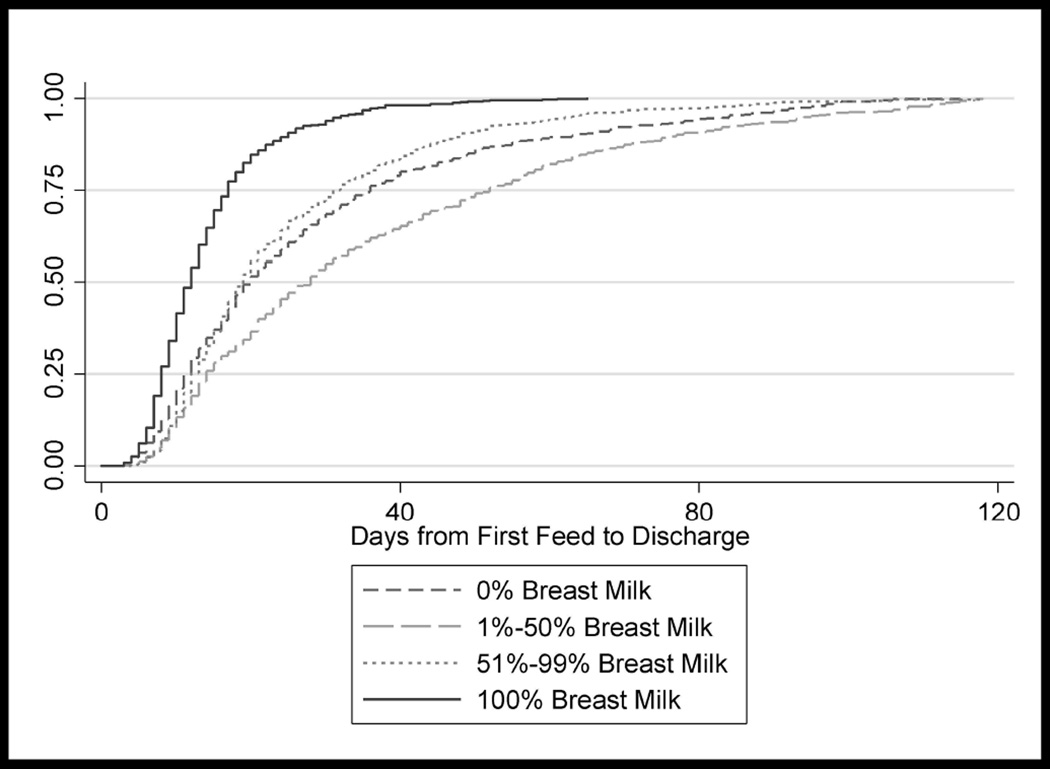
After adjustment, infants fed 0% human milk continued to have a significantly prolonged length of stay following the start of enteral feeding compared with infants fed 100% human milk (adjusted hazard ratio [HR] for discharge per day: 0.46, 95% confidence interval [CI]: 0.40, 0.52), as did infants fed human milk on 1–50% of feeding days (adjusted HR: 0.37, 95% CI: 0.32, 0.41) and those fed human milk on 51–99% of feeding days (adjusted HR: 0.51, 95% CI: 0.46, 0.57) (Figure). However, infants fed human milk on 1–50% of feeding days had a longer adjusted time to discharge than infants fed 0% human milk (adjusted HR: 0.80, 95% CI: 0.71, 0.90).
Figure 1.
Time to discharge by percent enteral feeding days on which the infant was given human milk. P < 0.01.
In the sensitivity analysis, which grouped infants by percent enteral feed days the infant was fed human milk during the first 21 days of feeds, infants fed human milk on 0% of feeding days continued to have significantly increased time to discharge as compared with those fed human milk on 100% of feeding days (adjusted HR for discharge per day: 0.59, 95% CI: 0.50, 0.69). The same was true for infants fed human milk on 1–50% of enteral feeding days (adjusted HR: 0.61, 95% CI: 0.52, 0.72) and those fed human milk on 51–99% of enteral feeding days (adjusted HR: 0.59, 95% CI: 0.52, 0.68).
Discussion
Gastroschisis is associated with a long hospital stay following surgical repair.13 Previous studies have demonstrated a beneficial effect in feeding these infants with human milk compared with formula after repair. However, these studies involved single-center retrospective reviews and were limited by small sample sizes.14 Using a database containing data from over 300 NICUs, we have demonstrated that feeding with human milk is associated with significantly decreased time to discharge following repair of gastroschisis, after adjusting for patient characteristics and other factors related to severity of illness.
It was important to adjust for patient factors, as at baseline, patients who received only human milk appeared to be less sick than those who received some enteral feeding days with only formula. This was supported by the finding that infants fed human milk were fed at an earlier postnatal age, as well as the finding that infants in the no human milk group had larger weight gains from birth to discharge. By adjusting for surrogates for severity of illness, including time to first feed as well as days on inotropes and days on the ventilator, we attempted to take this into account. Despite these baseline differences, after adjustment, we still found that the increasing utilization of human milk was associated with reduced time to discharge.
The use of time to discharge as our outcome of interest is important for many reasons. First, it acts as a composite for the real variables of interest, including the incidence of complications as well as the tolerability of enteral feeds. Second, time to discharge is also related to hospital costs, an important concern in the current health care environment. Caring for infants in the NICU is expensive, especially for preterm and low-birth-weight infants.15 Reductions in NICU length of stay by a day or two can result in large savings. Lastly, using time to discharge allowed us to perform an analysis that included censoring for death, which prevented bias from early mortality.
These findings are similar to those found in previous studies. Kohler et al performed a single-center study of 90 infants born with gastroschisis, and as in our study, separated them into 4 groups with 1 group receiving no human milk, 1 group receiving exclusively human milk, and the other 2 groups receiving mixed amounts of formula and human milk.14 The authors found on unadjusted analysis that the infants fed exclusively human milk had a significantly decreased time from initiation of feeds to full feeding. However, after adjusting for other factors, no significant difference between groups remained, likely due to the small sample size. We used a much larger sample size to show significant differences in time from feeding initiation to discharge between groups, even after adjustment for other factors. In this type of retrospective analysis, this adjustment is extremely important, as sicker children will be much less likely to continually tolerate feeds, making it much more difficult to keep a continuous supply of human milk on hand. Our ability to control for days during which an infant was not being fed helps decrease this risk of bias.
There are many reasons why human milk may be beneficial over formula in this population. Preterm infants are at extremely high risk for infections, and human milk contains important antibodies and other immunologic factors that may help decrease the incidence of these infections.3 Furthermore, it improves the absorption of vital nutrients and may be important for gastrointestinal health.4 Jayanthi et al performed a single-center review of their outcomes following repair of gastroschisis and found that, of 60 infants, 8 developed NEC.10 None of the infants who developed NEC had been fed exclusively human milk.
Although there was a clear benefit of being fed exclusively human milk or being fed human milk on 51–99% of feeding days over receiving no human milk, being fed human milk on 1–50% of feeding days was associated with even longer time from initiation of feeds to discharge than being fed 0% human milk. This is likely due to incomplete adjustment for the infants’ severity of illness, as evidenced by the significantly higher number of days that infants in this group were not fed enterally after feeding initiation as compared with the other groups. Holding feeds after initiation may be a sign of poor tolerance but often is secondary to an underlying medical problem, and although we adjusted for the holding of feeds, we likely did not fully adjust for the underlying cause.
Our results demonstrated a significantly higher mortality among infants who were fed no human milk as compared with infants fed any amount of human milk. However, the inability to adjust for important characteristics such as the complexity of the gastroschisis must be taken into account. It is unclear whether mortality is associated directly with human milk or just a marker of more severe baseline disease in this patient population.
Although the results of our study are important for the care of the preterm infant following gastroschisis repair, there are limitations that should be acknowledged. First, as a retrospective review of a multi-center database, there are missing variables that would assist in adjustment for patient-related factors, as the data were not collected specifically for this study. These include reasons for holding feeds, post-repair complications, reasons for not using human milk, methods of feeding, and fortification strategies. Second, although donor human milk can provide many of the same advantages as maternal human milk, it likely does not have the same magnitude of effect, and, unfortunately, we could not differentiate the two. Lastly, there may be other covariates that could not be adjusted for that may be partially responsible for the differences in outcomes between groups. For instance, socioeconomic status has been demonstrated to be associated with the use of human milk in newborn infants.16
In conclusion, after adjustment for patient characteristics and factors related to severity of illness, the use of human milk for enteral feeding of preterm infants following repair for gastroschisis significantly decreased the time from feeding initiation to discharge. This outcome is likely a surrogate for a reduction in post-repair complications and an improvement in tolerability of enteral feeding. Future research should focus on methods for increasing the use of human milk among these infants.
Acknowledgments
Funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; HHSN275201000003I for the Pediatric Trials Network and 1R25HD076475). B.G. receives support from the National Institutes of Health funded Cardiothoracic Surgery Trials Network (5U01HL088953-05). M.L. receives support from the US government for his work in pediatric and neonatal clinical pharmacology (HHSN267200700051C under the Best Pharmaceuticals for Children Act [PI: Benjamin]) and NICHD (K23HD068497). P.B.S. receives salary support for research from the National Center for Advancing Translational Sciences (UL1TR001117), NICHD (HHSN2752010000031 and 1R01-HD081044-01), the Food and Drug Administration (1R18-FD005292-01), and Cempra Pharmaceuticals (subaward to HHS0100201300009C). C.H. receives salary support from the National Center for Advancing Translational Sciences (UL1TR001117).
Abbreviations
- CI
confidence interval
- GA
gestational age
- HR
hazard ratio
- NEC
necrotizing enterocolitis
- NICU
neonatal intensive care unit
- PNA
postnatal age
- SGA
small for gestational age
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The other authors declare no conflicts of interest.
References
- 1.Andres A, Cleves MA, Bellando JB, Pivik R, Casey PH, Badger TM. Developmental status of 1-year-old infants fed human milk, cow’s milk formula, or soy formula. Pediatrics. 2012;129:1134–1140. doi: 10.1542/peds.2011-3121. [DOI] [PubMed] [Google Scholar]
- 2.Walker A. Human milk as the gold standard for protective nutrients. J Pediatr. 2010;156:S3–S7. doi: 10.1016/j.jpeds.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 3.Narayanan I, Prakash K, Bala S, Verma RK, Gujral VV. Partial supplementation with expressed breast-milk for prevention of infection in low-birth-weight infants. Lancet. 1980;2:561–563. doi: 10.1016/s0140-6736(80)91994-7. [DOI] [PubMed] [Google Scholar]
- 4.McMillan JA, Oski FA, Lourie G, Tomarelli R, Landaw SA. Iron absorption from human milk, simulated human milk, and proprietary formulas. Pediatrics. 1977;60:896–900. [PubMed] [Google Scholar]
- 5.Feldman R, Eidelman AI. Direct and indirect effects of human milk on the neurobehavioral and cognitive development of premature infants. Dev Psychobiol. 2003;43:109–119. doi: 10.1002/dev.10126. [DOI] [PubMed] [Google Scholar]
- 6.Gould S, Smith N. Complications of prematurity. The Pediatric and Perinatal Autopsy Manual with DVD-ROM. 2014:284. [Google Scholar]
- 7.Regev RH, Lusky A, Dolfin T, Litmanovitz I, Arnon S, Reichman B. Excess mortality and morbidity among small-for-gestational-age premature infants: a population-based study. J Pediatr. 2003;143:186–191. doi: 10.1067/S0022-3476(03)00181-1. [DOI] [PubMed] [Google Scholar]
- 8.Lucas A, Cole TJ. Human milk and neonatal necrotising enterocolitis. Lancet. 1990;336:1519–1523. doi: 10.1016/0140-6736(90)93304-8. [DOI] [PubMed] [Google Scholar]
- 9.Hunter AG, Stevenson RE. Gastroschisis: clinical presentation and associations. American Journal of Medical Genetics Part C: Seminars in Medical Genetics. Wiley Online Library. 2008:219–230. doi: 10.1002/ajmg.c.30178. [DOI] [PubMed] [Google Scholar]
- 10.Jayanthi S, Seymour P, Puntis JW, Stringer MD. Necrotizing enterocolitis after gastroschisis repair: a preventable complication? J Pediatr Surg. 1998;33:705–707. doi: 10.1016/s0022-3468(98)90191-9. [DOI] [PubMed] [Google Scholar]
- 11.Spitzer AR, Ellsbury DL, Handler D, Clark RH. The Pediatrix BabySteps Data Warehouse and the Pediatrix QualitySteps improvement project system—tools for "meaningful use" in continuous quality improvement. Clin Perinatol. 2010;37:49–70. doi: 10.1016/j.clp.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–e224. doi: 10.1542/peds.2009-0913. [DOI] [PubMed] [Google Scholar]
- 13.Driver C, Bruce J, Bianchi A, Doig C, Dickson A, Bowen J. The contemporary outcome of gastroschisis. J Pediatr Surg. 2000;35:1719–1723. doi: 10.1053/jpsu.2000.19221. [DOI] [PubMed] [Google Scholar]
- 14.Kohler JA, Sr, Perkins AM, Bass WT. Human milk versus formula after gastroschisis repair: effects on time to full feeds and time to discharge. J Perinatol. 2013;33:627–630. doi: 10.1038/jp.2013.27. [DOI] [PubMed] [Google Scholar]
- 15.Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120:e1–e9. doi: 10.1542/peds.2006-2386. [DOI] [PubMed] [Google Scholar]
- 16.Merewood A, Brooks D, Bauchner H, MacAuley L, Mehta SD. Maternal birthplace and breastfeeding initiation among term and preterm infants: a statewide assessment for Massachusetts. Pediatrics. 2006;118:e1048–e1054. doi: 10.1542/peds.2005-2637. [DOI] [PubMed] [Google Scholar]