Summary
The common assumption that population sleep duration has declined in the past few decades has not been supported by recent reviews, which have been limited to self-reported data. The aim of this review was to assess whether there has been a reduction in objectively recorded sleep duration over the last 50+ years.
The literature was searched for studies published from 1960–2013, which assessed objective sleep duration (TST) in healthy normal-sleeping adults. The search found 168 studies that met inclusion criteria, with 257 data points representing 6,052 individuals ages 18–88 years. Data were assessed by comparing the regression lines of age vs. TST in studies conducted between 1960–1989 vs. 1990–2013. Weighted regression analyses assessed the association of year of study with age-adjusted TST across all data points. Regression analyses also assessed the association of year of study with TST separately for 10-year age categories (e.g., ages 18–27 years), and separately for polysomnographic and actigraphic data, and for studies involving a fixed sleep schedule and participants’ customary sleep schedules.
Analyses revealed no significant association of sleep duration with study year. The results are consistent with recent reviews of subjective data, which have challenged the notion of a modern epidemic of insufficient sleep.
Keywords: Normal sleeper, polysomnography, actigraphy
Introduction
It has been widely stated that modern industrialized societies have become sleep-deprived. Some studies have suggested that average sleep duration has declined over the last few decades [1–4]. Such findings, combined with extensive epidemiologic evidence associating short sleep with health risks [5–7] and experimental evidence of adverse effects of sleep deprivation [8–10], have provoked widespread concern that chronic insufficient sleep has become a public health crisis.
However, recent reviews of self-reported data have cast doubt on whether nighttime sleep or 24-h sleep has decreased in recent decades, and whether there has been an increased prevalence of short sleep (<6 h), for which risks have been most clearly established. For example, a review of eight studies by Knutson et al. found no significant 31-year trend (1975–2006) towards a higher prevalence of self-reported nighttime sleep of ≤ 6 h [11]. Bin et al. reviewed 12 studies from 15 countries assessed from the 1960s–2000s, and found that sleep duration had increased in 7 countries, decreased in 6 countries, and had not clearly changed in 2 countries [12]. In a subsequent meta-analysis of 38 studies conducted in 10 countries in the 1970s–2000s, Bin et al. [13] found that average 24-h sleep duration had increased in most countries (including the US), and that the prevalence of sleeping ≤ 6 h had decreased in most countries (including the US). Rowshan Ravan et al. studied 36-year trends (1968–2004) in sleep duration among Swedish women, and found no change in 50-year old women, and a decline of only 15 minutes in 38-year old women [14]. Moreover, Bonke reviewed five representative time-use studies spanning 1964–2009, and concluded that “the same number of hours is slept today as in the mid-1960s, with nearly the same prevalence of short and long sleepers” [15].
Discrepancies between studies of population temporal trends in sleep duration can be attributed to multiple factors, including characteristics and representativeness of the respondents, wording of the questions, and instructions given to respondents [16, 17]. Perhaps the biggest limitation of this literature is that it has been limited to self-reports of sleep duration (some of which were retrospective), which can be inaccurate [18, 19] due in part to response biases. The aim of this review was to examine whether there has been a decline over the past 5 decades in sleep duration, as indexed by objective data.
Methods
The search of the literature was modeled after a previous meta-analysis by Ohayon et al., which assessed objective sleep patterns across age [20]. PubMed, PsychLit, selected journals, and reference lists of located manuscripts were searched for studies published between 1960–2013 which met the following criteria: 1) inclusion of presumably healthy adults (as described by the authors), participant ages ≥18 y without sleep problems; 2) report of all-night average total sleep time (TST) measured by polysomnography (PSG) or actigraphy; 3) assessment of sleep under minimally-disturbed conditions, including baseline or placebo conditions, and not involving particularly invasive procedures (e.g., catheterization). Many of the studies included a control group of presumably normal sleepers who had been compared with participants with sleep disorders. Studies involving individuals with extremely high levels of physical fitness were excluded under the assumption that sleep of such individuals might not be representative of the population. Key search words were sleep with normal, normative, healthy, controls, and adults.
The literature searches were performed by two of the authors: either EEG or NK. Questions regarding whether a study met inclusion criteria were resolved in discussions between EEG and SDY or AMR and SDY. Data from the studies were extracted by EEG and AMR.
The search identified >3,500 studies, of which 168 met the inclusion criteria, generating 257 data points across 6,052 individuals. Studies were separated into PSG (Table 1) and actigraphic studies (Table 2). Citations for all included studies are listed in the reference list (#55–222). Coding for each study included the mean sample age (or mid-point of the age range if the mean age was not available), number of men and women subjects, mean sample total sleep time (min), and estimated year of study. Studies with multiple age groups generated multiple data points for the analyses. When available, separate data points for men and women were used. Since most of the studies recorded sleep in the laboratory, only the laboratory data were used for studies that included both home and laboratory data, except for separate analysis of the actigraphy data.
Table 1.
Polysomnography studies reviewed for the present paper.
| Polysomnography Studies | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Fixed Sleep Schedule | |||||||||
| Authors | Year Published | Estimated Year of Study | Sample Size | Sample Age Years | Gender | Total Sleep Time (± SD) min | Time in Bed (± SD) min | Excluded First Night | Comments |
| Ryback, Lewis | 1971 | 1970 | n= 8 | 18–24 | not stated | 404.5 | 480 | Yes | Baseline data only |
| Brezinova | 1975 | 1974 | n=24 | 42–66 | M-5 F-9 | 484 ± 22 | 540 | Yes | |
| 20–30 | M-6 F-4 | 455 ± 31 | |||||||
| Nicholson, Stone | 1980 | 1978 | n=6 | 24 | not stated | 443.3 | 480 | Not Stated | Placebo data only |
| Okuma et al. | 1982 | 1982 | n= 8 | 21.1 | M-8 | 444.4 | 480 | Not Stated | Baseline data only |
| Bixler et al. | 1984 | 1984 | n=100 | 19–29 | M-10 F-11 | 440.4 | 480 | Yes | |
| 30–49 | M-16 F-21 | 432.4 | |||||||
| 50–80 | M-14 F-28 | 406.6 | |||||||
| Carskadon, Dement | 1985 | 1985 | n= 10 | 69.3 | M-2 F-8 | 467 ± 54 | 600 | Yes | Baseline data only |
| Roehrs et al. | 1986 | 1986 | n= 12 | 28 | M-12 | 433.2 | 480 | Yes | Placebo group only |
| Libert et al. | 1988 | 1988 | n= 6 | 20–29 | M-6 | 444.4 ±19.7 | 480 | Yes | Baseline data only |
| Gillberg, Akerstedt | 1994 | 1993 | n= 7 | 19–21 | No Data | 456 ±6.4 | 480 | Yes | 8-hour treatment data only |
| Walsh et al. | 1994 | 1993 | n= 12 | 23.5 | M-9 F-3 | 465 | 510 | Not Stated | ND (no sleep disruption condition) night two data only |
| Carrier, Dumont | 1995 | 1995 | n= 23 | 22.8 | M-18 F-5 | 463.68 | 480 | Not Stated | Baseline data only |
| Landolt et al. | 1995 | 1995 | n= 9 | 22.4 | M-9 | 452.67 | 480 | Yes | Placebo, baseline night data only |
| Mann et al. | 1996 | 1995 | n= 11 | 24.8 | M-11 | 393.5 ±19 | 480 | Yes | Baseline data only |
| Landolt et al. | 1996 | 1994 | n= 10 | 61.6 | M-10 | 413.4 | 480 | Yes | Baseline data only |
| Landolt et al. | 1996 | 1995 | n=16 | 20–26 | M-8 | 449.7 ±4.7 | 480 | Yes | |
| 57–64 | M-8 | 409.2 ±7.9 | 480 | ||||||
| Cajochen et al. | 1997 | 1995 | n= 8 | 23–32 | M-8 | 443.6 ±10.6 | 480 | Yes | Placebo, pretreatment night data only |
| Martin et al. | 1997 | 1996 | n= 12 | 25 | M-7 | 419.0 ±27.4 | 450 | Yes | Disregarding data from fragmented sleep night |
| Rao et al | 1998 | 1998 | n= 17 | African American 30.9 | M-6 F-11 | 416.9 ±45.7 | 480 | Not Stated | |
| n= 10 | Asian 28.4 | M-6 F-4 | 404.3 ±29.2 | 480 | |||||
| n= 30 | Caucasian 42.2 | M-16 F-14 | 406.4 ±52.5 | 480 | |||||
| n= 16 | Hispanic 27.7 | M-7 F-9 | 440.6 | 480 | |||||
| Harma et al. | 1998 | 1996 | n= 2 | 28.9 | F-2 | 421 ± 24 | 480 | Yes | Controls only |
| Yassouridis et al. | 1999 | 1997 | n= 30 | 27.5 | M-30 | 432.21 ±16.5 | 480 | Yes | |
| Sharkey et al. | 2001 | 2000 | n= 21 | 27 | M-12 F-9 | 459 ± 12 | 480 | Yes | Baseline, placebo data only |
| Onen et al. | 2001 | 2000 | n= 9 | 31 | M-9 | 426.3 ±11.7 | 480 | Yes | Baseline data only |
| Gaudreau et al. | 2001 | 1999 | n=54 | 19–29 | M-10 F-5 | 502.53 ±46.32 | 570 | Yes | > 18 year old data plotted only |
| 36–60 | M-10 F-5 | 439.49 ±34.54 | 480 | ||||||
| Huber et al. | 2002 | 2002 | n= 16 | 22.3 | M-16 | 446.4 ±3 | 480 | Yes | Sham data only |
| Mukai et al. | 2003 | 2001 | n= 8 | 24.5 | M-8 | 456.3 ±15.7 | 480 | Yes | Normal sleepers only |
| Brandenberger et al. | 2003 | 2002 | n= 24 | 21.1 | M-10 F-2 | 449.2 ±4 | 480 | Yes | |
| 64.9 | M-10 F-2 | 409.5 ±85 | |||||||
| Waters et al. | 2003 | 2002 | n= 77 | 26.5 | M-77 | 406.8 | 480 | Yes | Placebo data only |
| LaJambe et al. | 2005 | 2004 | n= 8 | 18–35 | no data per group | 389.6 ±24 | 480 | Yes | Placebo data only |
| Drapeau et al. | 2006 | 2005 | n= 12 | 23.8 | M-6 F-6 | 460 ± 12 | 480 | Yes | Placebo data only |
| n= 12 | 50.3 | M-5 F-7 | 395 ± 15 | ||||||
| Hornyak et al. | 2007 | 2006 | n= 35 | 19–69 | M-16 F-29 | 425.4 ±34.3 | 480 ±30 | Yes | Controls only |
| Wong et al. | 2008 | 2007 | n= 9 | 27.8 | M-9 F-1 | 390 | 480 | Yes | Control data only |
| Schmid et al. | 2008 | 2007 | n= 9 | 24.2 | M-9 | 418 ± 11 | 420 | Not Stated | Seven hour TIB data only |
| Cote et al. | 2009 | 2008 | n= 12 | 21 | M-4 F-13 | 450 | 480 | Yes | Baseline data only |
| Bixler et al. | 2009 | 2007 | n= 66 | 23.5 | M-32 | 432 | 480 | Yes | Baseline data only |
| 24.2 | F-34 | 430 | 480 | ||||||
| Vandekerckhove et al. | 2011 | 2010 | n= 13 | 19–56 | M-6 F-7 | 457.42 ±32.65 | 480 | Yes | Baseline (first data point) neutral data (second data point) |
| 445.46 ±45.77 | |||||||||
| Brower et al. | 2011 | 2010 | n= 10 | 20–40 | no data | 389.3 ±10.3 | 420 | Yes | Baseline data only for healthy control |
| Schmid et al. | 2012 | 2011 | n= 23 | 23.2 | M-23 | 462.1 ±1.3 | 480 | Yes | Sham data only |
| Schmid et al. | 2012 | 2011 | n= 30 | 23 | M-30 | 456.5 ±2.4 | 480 | Screening night included | Sham data only |
| Flausino et al. | 2012 | 2011 | n= 18 | 27.2 | M-18 | 339.1 ±54.9 | 480 | Not Stated | Baseline data only. Data deleted as outlier |
| Holz et al. | 2012 | 2012 | n= 20 | 27.1 | M-10 F-10 | 418.7 | 480 | Yes | Baseline data only |
| Rosipal et al. | 2013 | 2012 | n=148 | 20–86 | M-67 F-81 | 384 | 474 | Yes | Data from two nights; used only 2nd night |
| 408 | 474 | ||||||||
| Tonetti et al. | 2013 | 2012 | n= 11 | 24.75 | M-4 F-7 | 401.18 ±47.96 | 480 | Not Stated | PSG data only, WS device data not included |
| Normal Sleep Schedule | |||||||||
| Feinberg et al. | 1967 | 1966 | n=30 | 19–36 | M-9 F-6 | 393.9 ±28.1 | 420.7 ±2.0 | Yes | Healthy control data only |
| 65–96 | M-9 F-6 | 384.4 ±36.5 | 468.9 ±38.3 | ||||||
| Walker et al. | 1977 | 1975 | n= 10 | 18–22 | M-10 | 441.0 ±27.5 | 478.6 ±3 | Yes | Nonrunner, baseline data only |
| Gaillard | 1978 | 1977 | n= 40 | 19–21 | n=12 | 504 ± 36 | 529 ± 38 | Yes | |
| 22–24 | n=11 | 505 ± 45 | 525 ±38 | ||||||
| 25–27 | n=11 | 491 ±49 | 517 ± 43 | ||||||
| 28–30 | n=6 | 460 ± 49 | 507 ± 40 | ||||||
| Browman | 1980 | 1979 | n= 8 | 19–22 | M-8 | 407.3 ±43.1 | 418.57 ±50.89 | Yes | Baseline data only |
| Adam | 1980 | 1979 | n= 16 | 59 | M-6 F-10 | 455.1±24.8 | Normal Sleep Patterns | Yes | Placebo capsule data |
| Philipson et al. | 1980 | 1978 | n= 46 | 24 | M-37 F-9 | 439.3 | 481.3 | Yes | |
| Coates et al. | 1981 | 1981 | n= 12 | 23–60 | M-6 F-6 | 388 ±55.4 | Normal Sleep Patterns | Yes | Night two data only |
| Montgomery et al. | 1982 | 1982 | n= 12 | 23.3 | M-4 F-4 | 428. 4 | 455.3 | Yes | Unfit subjects, however still fit healthy criteria |
| Trinder et al. | 1982 | 1982 | n= 6 | 22.3 | not stated | 401.4 | 452.3 | Yes | Unfit subjects, however still fit healthy criteria |
| n= 6 | 31.8 | not stated | 420.2 | 449.4 | |||||
| Paxton et al. | 1983 | 1983 | n= 9 | 20.67 | M-9 | 416 | 446 | Yes | Normal, unfit data only. Used average of 2 nights |
| 426 | 454 | ||||||||
| Bunnell et al. | 1983 | 1983 | n= 9 | 25 | M-4 F-5 | 436.2 ± 11.1 | Normal Sleep Patterns | Not Stated | Baseline data only |
| Horne, Staff | 1983 | 1983 | n= 8 | 25.4 | M-8 | 464.5 ± 20.5 | Normal Sleep Patterns | Yes | Baseline data only |
| Matsumoto et al. | 1984 | 1984 | n= 6 | 20–24 | M-6 | 389.0 ± 11.5 | Normal Sleep Patterns | Not Stated | No exercise group |
| Paxton et al. | 1984 | 1984 | n= 17 | 20 | M-17 | 449 ± 49.5 | 489 ± 25.2 | Yes | Non-athlete. Baseline data only |
| Reynolds et al. | 1985 | 1985 | n= 24 | 69.5 | M-8 F-16 | 367.4 ± 45 | Normal Sleep Patterns | Yes | Healthy control data only |
| Bonnet | 1985 | 1985 | n= 11 | 18–32 | not stated | 389 | Normal Sleep Patterns | Yes | Baseline data only |
| Kupfer et al. | 1985 | 1985 | n= 10 | 24.8 | M-10 | 396.6 ± 47.6 | Normal Sleep Patterns | Yes | No exercise group |
| Nakagawa | 1987 | 1987 | n= 6 | 19– 23 | M-6 | 501.8 ± 28.2 | 523.0 ± 30.7 | Yes | Baseline data only |
| Naifeh et al. | 1987 | 1987 | n=23 | 30–40 | M-6 F-6 | 386 ± 40 | 404 ± 46 | Not Stated | |
| 60 + | M-5 F-6 | 364 ± 47 | 422 ± 58 | ||||||
| Hudson et al. | 1988 | 1988 | n=18 | 20–55 | M-8 F-10 | 384.9 ± 30.7 | 421.1 ± 27.5 | Yes | Controls only |
| Schiavi, Schreiner-Engel | 1988 | 1988 | n=40 | 23–29 | M-11 | 404 ± 36 | 441 ± 36 | Yes | |
| 30–39 | M-5 | 411 ± 34 | 448 ± 41 | ||||||
| 40–49 | M-8 | 387 ± 42 | 434 ± 26 | ||||||
| 50–59 | M-7 | 332 ± 51 | 398 ± 39 | ||||||
| 60–73 | M-9 | 317 ± 53 | 397 ± 39 | ||||||
| Hoch et al. | 1988 | 1988 | n=19 | 60–82 | M-9 F-10 | 350.1 ± 64.9 | 467.3 | Yes | |
| 370.9± 29.6 | 455.8 | ||||||||
| Mellman, Uhde | 1989 | 1989 | n=7 | 26–49 | M-5 F-2 | 439.6 ± 45.3 | Normal Sleep Patterns | Yes | Controls only |
| Bonnet | 1989 | 1989 | n=24 | 22 | M-12 | 372 | 411 | Yes | |
| 63 | M-12 | 363 | 430 | ||||||
| Lydiard et al | 1989 | 1989 | n=14 | 30.1 | No Data | 384.9 ± 31.4 | Normal Sleep Patterns | Yes | Controls only |
| Saletu et al | 1990 | 1990 | n=16 | 23–39 | M-8 F-8 | 385.66 ± 78.55 | 426.65 ± 19.4 | Yes | Baseline data only |
| Vitiello et al. | 1990 | 1990 | n= 24 | 63.6 | M-11 F-13 | 385.1 | 456.5 | Yes | Controls only |
| Brendel et al | 1990 | 1990 | n=10 | 83 | M-6 F-4 | 395.5 ± 70.1 | 491.5 ± 55.7 | Yes | Nights two and three |
| n=14 | 23.9 | M-10 F-4 | 429.8 ± 31.4 | 445.0 ± 42.4 | |||||
| Hoch et al | 1990 | 1990 | n=34 | 60–69 | M-21 F-13 | 335.1 ± 62.3 | 430.6 | Yes | |
| n=33 | 70–79 | M-17 F-16 | 328.5 ± 56.4 | 431.9 | |||||
| n=38 | 80–89 | M-19 F-19 | 318.1 ± 81.4 | 437.3 | |||||
| Lauer et al. | 1991 | 1991 | n=13 | 18–24 | M-26 F-25 total Not specified for age groups | 413.9 ± 16 | 422.3 | Not Stated | Controls only |
| n= 10 | 25–34 | 417.6 ± 23.6 | 428.8 | ||||||
| n= 10 | 35–44 | 404.6 ± 34.2 | 424.1 | ||||||
| n= 9 | 45–54 | 363.1 ± 44.5 | 397.2 | ||||||
| n= 9 | 55–65 | 350.0 ± 36.3 | 385.8 | ||||||
| Monk et al. | 1991 | 1991 | n=34 | 80–91 | M-16 F-18 | 368 ± 50 | 478 | Yes | |
| n=30 | 21–30 | M-21 F-9 | 426 ± 39 | 507 | |||||
| Van Coevorden et al. | 1991 | 1990 | n= 8 | 20–27 | M-8 | 479 ± 48 | Normal sleep Patterns | Yes | Non-catheter data only |
| n= 8 | 67–84 | M-8 | 454 ± 53 | ||||||
| Wauquier et al. | 1992 | 1992 | n= 7 | 88–102 | F-7 | 438 ± 27.6 | 566 ± 22.8 | Yes | |
| n= 7 | 88–98 | F-7 | 328 ± 14.1 | 462 ± 14.6 | |||||
| Bonnet, Arand | 1992 | 1992 | n= 12 | 18–30 | M-12 | 445 | 472 | Yes | Baseline data only |
| Hudson et al | 1992 | 1992 | n= 19 | 24.5 | M-7 F-12 | 407 ± 35 | 437 ± 32 | Yes | Controls only |
| Monk et al. | 1992 | 1992 | n= 25 | 71–91 | F-25 | 366 ± 37 | Normal Sleep Patterns | Not Stated | |
| n= 20 | 71–97 | M-20 | 338 ± 48 | ||||||
| n= 21 | 19–28 | M-10 F-11 | 415 ± 47 | ||||||
| Buysse et al | 1992 | 1992 | n=45 | > 78 | M-21 F-24 | 365.0 ± 62.0 | Normal Sleep Patterns | Yes | |
| n=33 | 20–30 | M-20 F-13 | 426.5 ± 36.4 | ||||||
| Hirshkowitz et al. | 1992 | 1992 | n=44 | 20–29 | M-44 | 347.3 ± 62.5 | 404.9 ± 44.1 | Yes | |
| n=23 | 30–39 | M-23 | 340.0 ± 70.8 | 393.1 ± 58.2 | |||||
| n=49 | 40–49 | M-49 | 329.4 ± 54.6 | 404.2 ± 49.4 | |||||
| n=41 | 50–59 | M-41 | 331.6 ± 63.6 | 393.0 ± 51.1 | |||||
| n=29 | >60 | M-29 | 298.4 ± 61.3 | 395.7 ± 42.8 | |||||
| Montmayeur, Buguet | 1992 | 1992 | n= 6 | 36 | M-6 | 357.8 ± 16.2 | Normal Sleep Patterns | Not Stated | Data from intermediate temperature only (March) |
| Dijk, Czeisler | 1993 | 1993 | n= 9 | 21–30 | M-9 | 431.8 ± 6.3 | Normal Sleep Patterns | Yes | Baseline data only |
| Hoch et al. | 1994 | 1994 | n=27 | <75 | M-21 F-29 | 378.6 ± 40.5 | Normal Sleep Patterns | Yes | Baseline data |
| n=23 | ≥75 | 363.9 ± 57.4 | |||||||
| Buguet et al. | 1995 | 1994 | n= 6 | 24 | No data | 441.2 ± 4.9 | 489.1 ± 2.3 | Not Stated | Placebo, baseline night data only |
| Hajak et al. | 1996 | 1995 | n= 10 | 25.6 | M-5 | 419.1 ± 62.1 | 483 ± 16 | Yes | Placebo data only |
| 49.4 | M-5 | 389 ± 44.6 | 455 ± 20 min | ||||||
| Carrier et al. | 1996 | 1995 | n= 24 | 82.2 | M-10 F-14 | 370.3 ± 7.9 | 460 | Yes | Baseline data only |
| Vitiello et al. | 1996 | 1995 | n= 68 | 55–80+ | F-68 | 393.2 ± 6 | 465.8 ± 5.9 | Yes | Non-catheter data only |
| n= 45 | 60–80+ | M-45 | 369.8 ± 7.3 | 445.3 ± 8.5 | |||||
| Ehlers, Kupfer | 1997 | 1996 | n=61 | 20–29 | M-18 | 447.83 | 477.58 | Yes | |
| F-14 | 457.71 | 483.43 | |||||||
| 30–40 | M-15 | 413 | 445.57 | ||||||
| F-14 | 415.5 | 439.4 | |||||||
| Haimov, Lavie | 1997 | 1996 | n=17 | 65–75 | M-17 | 330.2 ± 33.4 | Normal Sleep Patterns | Yes | |
| n=8 | 19–26 | M-8 | 354.3 ± 38.4 | ||||||
| Carrier et al. | 1997 | 1997 | n= 39 | 29.99 | M-52 F-58 | 457.73 ± 44.36 | 460.6 ± 4.3 | Yes | |
| n= 37 | 34.79 | 423.05 ± 36.4 | |||||||
| n= 33 | 47.64 | 405.96 ± 37.52 | |||||||
| Edinger et al. | 1997 | 1997 | n=32 | 67.5 | M-16 F-16 | 363.6 (Home) | Normal Sleep Patterns | No | Used only night 2 in the lab |
| 347.5 (Home) | |||||||||
| 371.8 (Lab) | |||||||||
| 361.1 (Lab) | |||||||||
| Cajochen et al. | 1998 | 1997 | n= 10 | 27 | M-10 | 423.5 ± 5 | Normal Sleep Patterns | Yes | Placebo, treatment night data only |
| Lushington et al. | 1999 | 1997 | n= 16 | 65.4 | M-5 F-11 | 449.3 ± 8 | 530 ± 6 | Yes | |
| Armitage et al. | 2000 | 1999 | n=23 | 22–40 | M-15 | 384.5 | Normal Sleep Patterns | Yes | Controls only |
| F-8 | 410.3 | ||||||||
| Carrier et al. | 2001 | 1999 | n=100 | 20–39 | M-31 F-27 | 428.9 | Normal Sleep Patterns | Yes | |
| 40–60 | M-22 F-20 | 404.3 | |||||||
| Nicolas et al. | 2001 | 2000 | n=30 | 20–29 | M-3 F-3 | 433.07 ± 32.99 | Normal Sleep Patterns | Yes | |
| 30–39 | M-3 F-3 | 451.53 ± 47.45 | |||||||
| 40–49 | M-3 F-3 | 431.47 ± 22.09 | |||||||
| 50–59 | M-3 F-3 | 447.65 ± 39.00 | |||||||
| 60–69 | M-2 F-4 | 379.12 ± 41.28 | |||||||
| Edinger et al. | 2001 | 2000 | n= 35 | 40–59 | M-17 F-18 | 377.6 ± 10.5 | Normal Sleep Patterns | Yes | Controls only (Home) |
| Roky et al. | 2001 | 1999 | n= 8 | 20–28 | M-8 | 422 ± 9 | Normal Sleep Patterns | Yes | Baseline data only |
| Means et al. | 2003 | 2002 | n= 49 | 55.4 | M-27 F-22 | 376.9 ± 46.5 (Home) | 452.0 ± 63.3 | Yes | Disregarded insomnia patient data |
| 371.2 ± 41.2 (Lab) | 430.7 ± 45.8 | ||||||||
| Kato et al. | 2004 | 2003 | n= 10 | 24.6 | M-4 F-6 | 452 ± 17 | Normal Sleep Patterns | Yes | Baseline data only |
| Penev | 2007 | 2006 | n=12 | 68.9 | M-12 | 383 ± 58 | 436 | Yes | |
| Carrier et al. | 2007 | 2006 | n= 17 | 37.2 | M-7 F-10 | 426.1 ± 16 | 504 | Not Stated | Placebo data only |
| Peters et al. | 2008 | 2007 | n= 28 | 20.14 | M-7 F-7 | 483.12 ± 35.32 | Normal Sleep Patterns | Yes | Baseline data only |
| 69.79 | M-7 F-7 | 445. 43 ± 71.7 | |||||||
| O'Donnell et al. | 2009 | 2008 | n= 24 | 64 | M-11 F-13 | 377.5 ± 37.6 | Normal Sleep Patterns | Yes | Baseline data only |
| Paterson et al. | 2009 | 2008 | n= 12 | 24.9 | M-12 | 458 ± 12 | Normal Sleep Patterns | Yes | Placebo data only |
| Robillard et al. | 2010 | 2008 | n= 87 | 23.3 | M-26 F-22 | 438 | Normal Sleep Patterns | Not Stated | |
| 51.9 | M-18 F-21 | 404 | |||||||
| Morgan et al. | 2010 | 2008 | n= 12 | 39 | M-12 | 416 ± 15 | Normal Sleep Patterns | Placebo data only | |
| Marzano et al. | 2010 | 2009 | n= 10 | 23.8 | M-10 F-10 | 441.4 ± 38 | 484.8 ± 63 | Yes | Baseline data only |
| Ferri et al. | 2010 | 2009 | n= 15 | 24.6 | M-12 F-3 | 449.6 ± 18.41 | 483.0 ± 16 | Not Stated | |
| Herbst et al | 2010 | 2009 | n= 26 | 39.8 | M-13 F-13 | 386.56 ± 83.95 | Normal Sleep Patterns | Yes | Night one and night two data |
| 395.27 ± 68.49 | |||||||||
| Nissen et al. | 2011 | 2009 | n= 26 | 46.3 | M-14 F-12 | 390.4 | Normal Sleep Patterns | Not Stated | Controls only |
| Hebert et al. | 2011 | 2009 | n= 22 | 60.4 | M-8 F-14 | 376.6 ± 59.6 | Normal Sleep Patterns | No | Controls only |
| Danker-Hopfe et al. | 2011 | 2009 | n= 30 | 25.3 | M-30 | 456.3 ± 16.6 | Normal Sleep Patterns | Yes | Sham data only |
| Marzano et al. | 2011 | 2009 | n= 50 | 24.3 | M-29 F-21 | 443.26 | Normal Sleep Patterns | Yes | Baseline data only |
| Gonzalez et al. | 2011 | 2010 | n= 20 | 28–64 | F-20 | 357.31 ± 41.5 | 420.59 ± 20.74 | Not Stated | Control data only |
| Bianchi et al. | 2012 | 2011 | n= 32 | 18–32 | M-16 F-16 | 474 ± 48 | 516 | Recorded as baseline | Baseline data only |
| n= 12 | 60–76 | M-5 F-7 | 402 ± 48 | 485 | |||||
| Ferri, Bruni et al. | 2012 | 2011 | n= 98 | 29.7 | M-12 F-13 | 393.7 | 438.5 | Not Stated | > 18 year old data only |
| 62.2 | M-4 F-6 | 410.8 | 526.6 | ||||||
| 73.4 | M-3 F-6 | 345.1 | 487.7 | ||||||
| Frey et al. | 2012 | 2011 | n= 8 | 20–31 | F-8 | 446.2 ± 26.9 | Normal Sleep Patterns | Yes | Disregarded depression data, baseline data only. |
| n= 8 | 57–74 | F-8 | 408.5 ± 42.5 | ||||||
| Kobayashi et al. | 2012 | 2011 | n=22 | 22.6 | M-15 F-8 | 373.1 ± 136.2 | Normal Sleep Patterns | Yes | Non-PTSD subjects Only used |
| 408.1 ± 81.7 | |||||||||
| Ferri et al. | 2013 | 2012 | n=18 | 69.4 | M-10 F-8 | 382.5± 53.11 | 517.2 ± 64.31 | Yes | |
| Chellappa et al. | 2013 | 2012 | n= 30 | 25.2 | M-16 F-14 | 390.7 ± 3.1 | Normal Sleep Patterns | Not Stated | Classic light data only |
| Robey et al. | 2013 | 2012 | n= 11 | 26 | M-11 | 410.9 ± 14.3 | 438.9 ± 8 | Yes | Control data only |
| Richards et al. | 2013 | 2012 | n= 43 | 30.39 | M-22 F-21 | 403.66 | Normal Sleep Patterns | Not Stated | Control data only |
| Saxvig et al. | 2013 | 2012 | n= 19 | 21.1 | M-5 F-14 | 507 ± 68.8 | 551 ± 67.2 | Yes | Control data only |
| Sleep Schedule Not Stated | |||||||||
| Kahn et al. | 1970 | 1968 | n=10 | 76.7 | F-10 | 383 ± 46.6 | Not stated | Yes | |
| Williamset al. | 1972 | 1970 | n=10 | 41–46 | M-10 | 376.6 ± 35.7 | Not stated | Yes | |
| Browman, Tepas | 1976 | 1975 | n= 9 | 18.89 | M-9 | 456 | Not stated | Yes | Relaxation data group only |
| Karacan et al. | 1976 | 1975 | n= 18 | 20–30 | M-18 | 416 | Not stated | Yes | Baseline data only |
| Adam | 1982 | 1982 | n= 7 | 58 | M-4 F-3 | 456.5 ± 29.7 | Not stated | Yes | Non-catheter night only |
| Berry, Webb | 1985 | 1985 | n=119 | 50–70 | M-55 | 400.7 | Not stated | Yes | |
| F-64 | 403.8 | ||||||||
| Reynolds et al. | 1986 | 1986 | n= 20 | 70.1 | M-10 | 374 ± 48 | Not stated | Yes | Baseline data only |
| 68.7 | F-10 | 361.8 ± 42.6 | |||||||
| James et al. | 1987 | 1987 | n= 10 | 29.9 | M-7 F-3 | 436.9 ± 32.8 | Not stated | Yes | Placebo group only |
| Stone et al. | 2000 | 1999 | n= 7 | 23.4 | M-7 | 417.0 ± 26.6 | Not stated | Yes | |
| Youngstedt et al. | 2000 | 1998 | n=8 | 24.5 | M-8 | 424.3 ± 14.4 | Not stated | Yes | |
| Crowley et al. | 2002 | 2001 | n=34 | 18–25 | M-8 F-6 | 453.3 ± 92.7 | Not stated | Yes | |
| 74.6 | M-11 | 341.7 ± 65.5 | Not stated | ||||||
| 76.7 | F-9 | ||||||||
| Edinger et al. | 2003 | 2003 | n=34 | 46.5 | M-16 F-18 | 370.5 ± 10.1 (Lab) | Ad Lib | Yes | Normal patient data only |
| 379.6 ± 11.3 (Home) | |||||||||
| De Souza et al. | 2003 | 2001 | n= 21 | 18–33 | M-7 F-14 | 414.8 ± 43.2 | Not stated | Yes | |
| Beaumont et al. | 2004 | 2002 | n= 9 | 35.3 | M-6 F-3 | 395 ± 25 | Not stated | Yes | Placebo data only |
| Mahlberg, Kunz | 2007 | 2006 | n= 29 | 24–86 | M-13 F-16 | 396.8 ± 50.2 | Not stated | Yes | Healthy subject only |
| Bonnet, Arand | 2007 | 2006 | n= 12 | 18–20 | M-3 F-9 | 439 | Not stated | No | Data corrected for arousals associated with limb movements and apnea |
| n= 13 | 21–30 | M-7 F-6 | 446 | ||||||
| n=13 | 31–40 | M-7 F-6 | 403 | ||||||
| n=10 | 41–50 | M-6 F-4 | 395 | ||||||
| n=14 | 51–60 | M-12 F-2 | 358 | ||||||
| n=14 | 61–70 | M-12 F-2 | 350 | ||||||
| Jaehne et al | 2012 | 2011 | n= 44 | 18–52 | M-29 F-15 | 430.5 ± 17.06 | Not stated | Yes | Smoker data disregarded |
Table 2.
Actigraphic studies reviewed for the present paper.
| Actigraphic Studies | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Fixed Sleep Schedule | |||||||||
| Authors | Year Published | Estimated Year of Study | Sample Size | Sample Age Years | Gender | Total Sleep Time (± SD) min | Time in Bed (± SD) min | Excluded First Night | Comments |
| Blagrove et al. | 1998 | 1996 | n= 9 | 20 | F-9 | 421 ± 12.2 | 480 | Yes | |
| Hindmarch et al. | 2000 | 1998 | n= 30 | 27.3 | M-15 F-15 | 441.6 | 510 | Yes | Placebo data only |
| Jean-Louis et al. | 2001 | 1999 | n= 11 | 25.36 | M-4 F-7 | 441 | 480 | Yes | |
| Jean-Louis et al. | 2001 | 1999 | n=5 | 25 | no data | 449 ± 19 | 480 | Yes | |
| Baskett et al. | 2003 | 2001 | n= 20 | 71.7 | M-4 F-16 | 443 | 480 | Yes | Baseline data only |
| Yoon et al. | 2003 | 2002 | n=133 | 18–32 | M-26 F-47 | 420.8 ± 48.2 | 474.5 ± 54.5 | Yes | |
| 60–75 | M-22 F-38 | 366.1 ± 53.2 | 475.9 ± 64.3 | ||||||
| O’Hare et al. | 2014 | 2013 | n=20 | 30 | M-11 F-9 | 391 ± 49 | 450 | Not Stated | |
| Normal Sleep Schedule | |||||||||
| Jean-Louis et al. | 1996 | 1996 | n= 20 | 29.95 | M-11 F-9 | 391 ± 57 | Normal Sleep Patterns | Not Stated | Validation night only |
| Hume et al. | 1998 | 1997 | n= 190 | 20–34 | M-39 F-23 | 458 ± 54 | Normal Sleep Patterns | Yes | |
| 35–49 | M-22 F-42 | 422 ±60 | |||||||
| 50–70 | M-26 F-38 | 412 ± 55 | |||||||
| Pires et al. | 2001 | 2000 | n= 6 | 22–24 | M-6 | 558.7 ±73 | Normal Sleep Patterns | Yes | Placebo data only. Data from PSG |
| 511.5 ± 101 | |||||||||
| 517.7 ± 39 | |||||||||
| Youngstedt et al. | 2003 | 2002 | n= 71 | 18–75 | no data | 380.95 ± 5.8 | Not stated | No, because at home | |
| Benson et al. | 2004 | 2003 | n= 20 | 35.35 | M-7 F-13 | 383.93 ±70.29 | Normal Sleep Patterns | No, because at home | |
| Monk et al | 2006 | 2005 | n= 128 | 70–92 | M-65 F-63 | 413 ± 83 | 449 ± 76 | Not Stated | |
| Robertson et al. | 2007 | 2006 | n= 15 | 27.7 | M-7 F-8 | 374 ± 56.8 | Normal Sleep Patterns | Not Stated | Normal sleepers only. |
| Rahman et al. | 2011 | 2010 | n=15 | 35.6 | M-5 F-10 | 486 ±54 | Normal Sleep Patterns | Control data only. | |
| Kogure et al. | 2011 | 2010 | n= 45 | 50.2 | M-16 F-17 | 436 ± 69 | Normal Sleep Patterns | No, because at home | |
| 83.8 | F-12 | 410 ± 72.9 | |||||||
| Myllymäki et al. | 2011 | 2010 | n= 11 | 25 | M-7 F-4 | 437.7 ± 45 | 486 | Yes | Control data only |
| Scatena et al. | 2012 | 2011 | n= 25 | 44.3 | M-13 F-12 | 736.7 ± 121.8 | Normal Sleep Patterns | Not Stated | Data deleted as outlier |
| Robertson et al. | 2013 | 2012 | n= 19 | 20–30 | M-19 | 369 ± 40.5 | Not stated | Not Stated | Baseline data only. |
| Petersen et al. | 2013 | 2012 | n= 28 | 41 | M-7 F-21 | 381.81 ± 11.3 | 491 | Yes | Low sensitivity, low stress data only |
| Sleep Schedule Not Stated | |||||||||
| Naylor et al. | 2000 | 1999 | n= 14 | 75.2 | M-5 F-9 | 337.6 ± 19.5 | Not stated | Yes | Controls only |
| Gooneratne et al. | 2011 | 2009 | n= 100 | 72.5 | M-37 F-63 | 371.1 | Not stated | Yes | > 18 year old data only |
| Wulff et al. | 2012 | 2010 | n= 21 | 37.5 | M-13 F-8 | 364.8 ± 37.2 | Not stated | Not Stated | Control data only. |
| Shambroom et al. | 2012 | 2010 | n=26 | 38 | M-13 F-13 | 324.6 ± 11.2 | Not stated | Yes | |
| Ju et al | 2013 | 2012 | n=142 | 65.6 | M-58 F-84 | 402.6±44.6 | 486.4 ±49.8 | Not Stated | |
| Winser et al. | 2013 | 2012 | n=39 | 26.5 | M-12 | 428 ± 55.2 | Not Stated | Not stated | |
| 27.9 | F-27 | 434.1 ± 40 | |||||||
| Lombardi et al | 2013 | 2012 | n= 23 | 40.6 | M-23 | 420 | Not Stated | Not stated | Sea level data only |
| n= 14 | 36.1 | F-14 | |||||||
Since the year of publication of a study often differed from the year in which a study was conducted, the following rules were used to estimate the year that a study had been conducted. 1) Year of study was estimated by subtracting 10 months from the posted date of journal receipt of the manuscript for studies with <50 subjects, 14 months for studies with 50–99 subjects, 18 months for studies with 100–149 subjects, and 22 months for studies with ≥150 subjects. 2) If information was available regarding the date a paper was accepted, but not the date that it was received, the median across-the-literature duration in months between date received and date accepted (4 months) was subtracted from the date of publication, and Rule 1 was followed. 3) If neither date accepted nor date received information was available, the median number of months between date received and date published (11 months) was subtracted from the date of publication, and Rule 1 was followed.
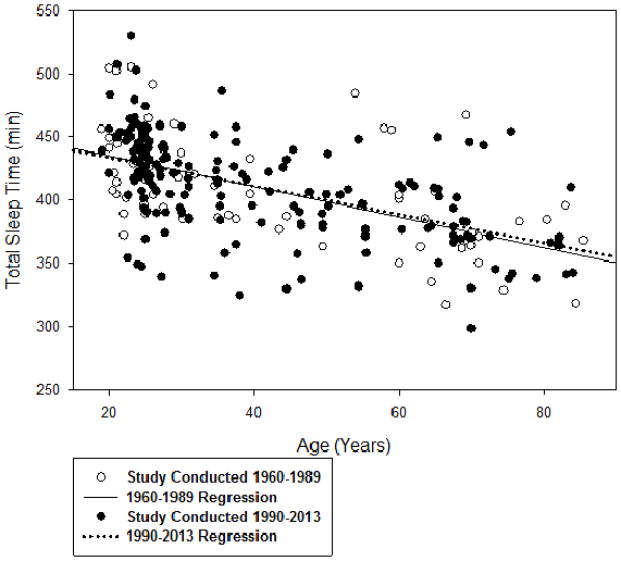
The TST data were first assessed by comparing the intercepts of the regression lines of age vs. TST for studies conducted between 1960–1989 vs. 1990–2013. We chose this split to obtain a more balanced number of data points across the years split. Another reason for the1989/1990 split was that it has been posited that the obesity epidemic, which started shortly after this time, can be partly attributed to declines in sleep. Examining the intercepts allowed an assessment of temporal differences in TST across all data points (without adjustment for age). A temporal decline in TST would be revealed by a smaller intercept for the 1990–2013 studies compared with the 1960–1989 studies. Another rationale for the1989/1990 split was that it has been posited that the obesity epidemic, which started shortly after this time, can be partly attributed to declines in sleep [21].
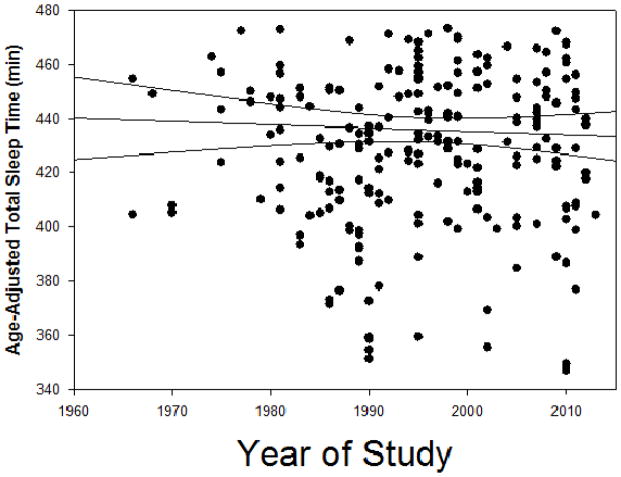
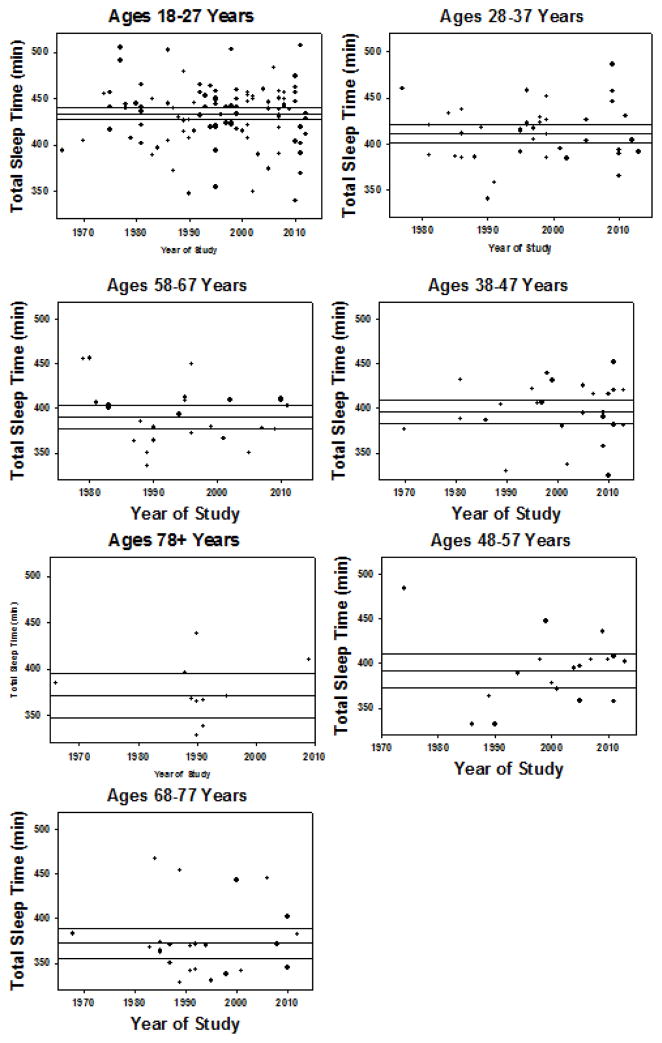
To further assess a temporal trend of TST across all data points, a linear regression analysis of year of study (weighted for sample size) and participants’ age vs. TST was calculated. To plot these data, age-adjusted TST was determined based on the slope of the linear regression between TST and age across all data points. An a priori decision was made to remove outlying samples, for which mean age-adjusted TST was ≥ 2 standard deviations from the mean value across the literature. Two data points were removed based on this criterion. Weighted linear regression analyses were also conducted for year of study vs. TST across 10-year age categories (e.g, ages 18–27 years, 28–37 years, etc.).
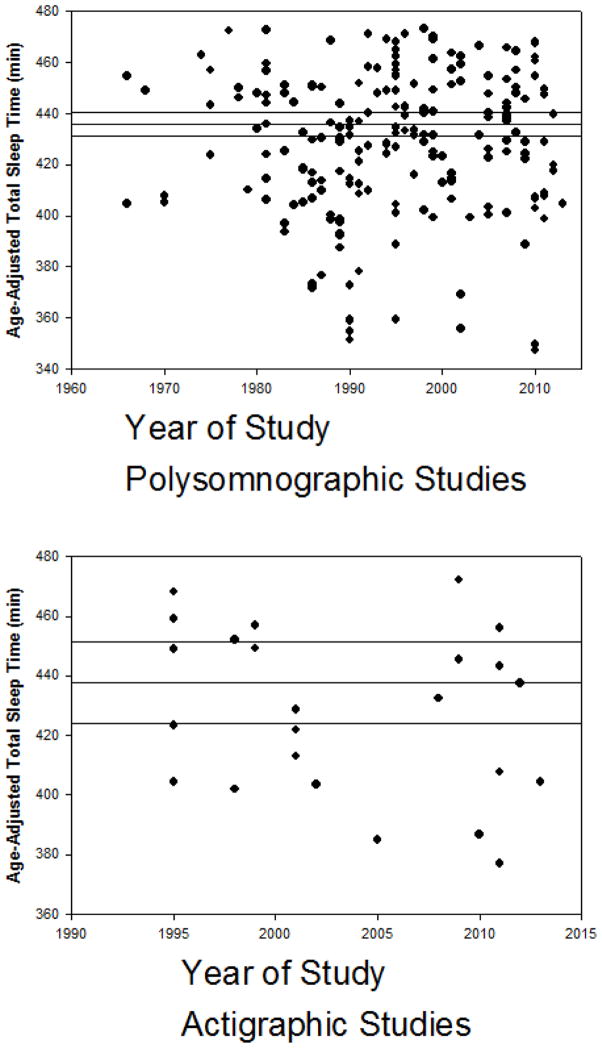
Separate weighted linear regression analyses were conducted for data from studies in which participants followed their usual sleep schedules and for studies involving a fixed sleep period; for polysomnographic and actigraphic data; and for data involving men only and women only. Plots of year of study vs. age-adjusted TST were performed for each of these analyses.
Results
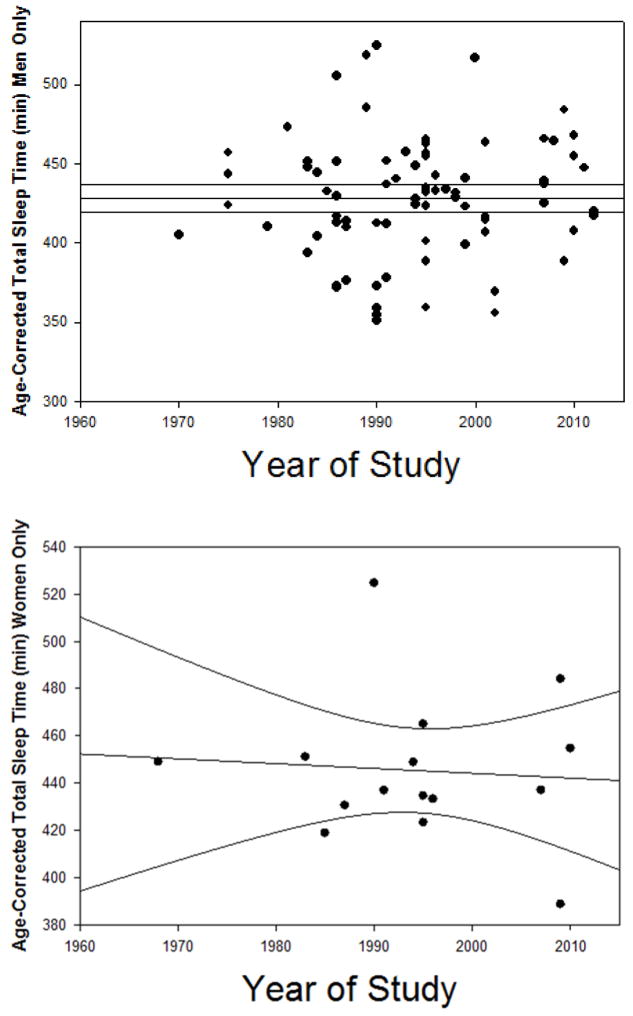
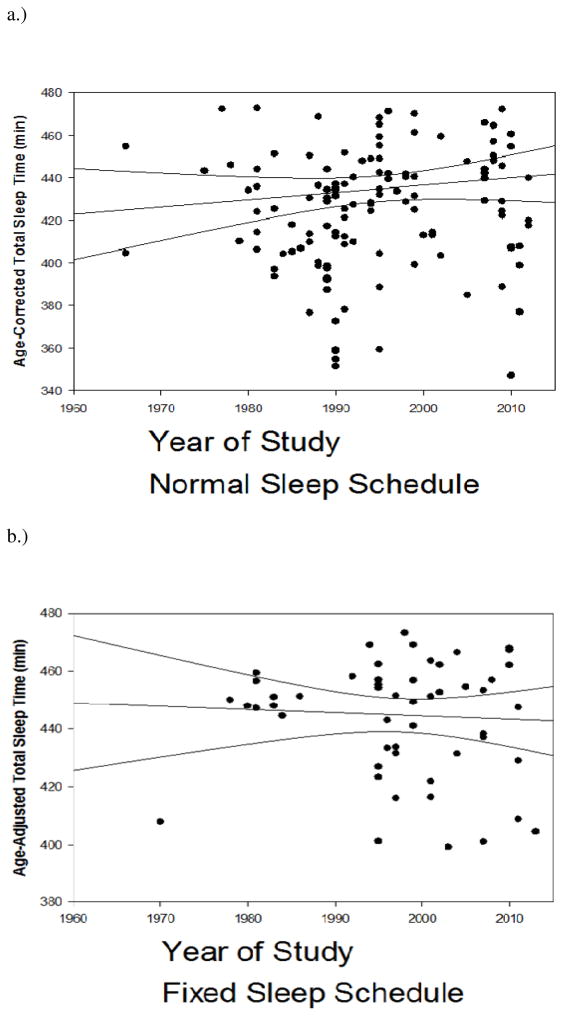
The intercepts and slopes of the regression lines of age vs. TST did not differ for studies conducted between 1960–1989 and 1990–2013 (Figure 1). In the regression analysis across all data points (n=257), there was no significant association of year of study with TST (b=.03, p=0.56) (Figure 2), nor was there a significant association of study year with TST for any of the 10-year age categories (Figure 3) (p=0.40–0.92). Likewise, there was no significant association of year of study in analyses restricted to PSG (n=225) (b=0.03, p=0.63) or to actigraphic data (n=32) (b=−0.17, p=0.38) (Figure 4); or in analyses involving only men (n=71) or only women (n=17) (Figure 5). Finally, there was no significant association in analyses derived from studies in which subjects followed their usual sleep periods (n=154) (b=0.13, p=0.10) or a fixed sleep period (n=68) (b=−0.14, p=0.24) (Figure 6).
Figure 1.
Association of mean age of participants with total sleep time (min) for studies conducted between 1960–1989 (open circles) and 1990–2013 (closed circles).
Figure 2.
Association of year of study with age-adjusted total sleep time (min) for all data points. The regression line and 95% confidence intervals are displayed.
Figure 3.
Association of year of study with total sleep time (with regression line and 95% confidence intervals) for participants ages 18–27 years (a), 28–37 years (b), 38–47 years (c), 48–57 years (d), 58–67 years (e), 68–77 years (f), and ≥78 years (g).
Figure 4.
Association of year of study with age-adjusted total sleep time (min) for polysomnographic data (a) and actigraphic data (b). The regression line and 95% confidence intervals are displayed.
Figure 5.
Association of year of study with age-adjusted total sleep time (min) for women subjects only. The regression line and 95% confidence intervals are displayed.
Figure 6.
Association of year of study with age-adjusted total sleep time (min) for studies in which subjects followed their usual sleep schedule (a), and for studies in which subjects followed a fixed sleep schedule of 470–480 min (b). The regression line and 95% confidence intervals are displayed.
Discussion
The results indicate relative stability of objectively-recorded sleep durations in healthy sleepers assessed over the last half-century. Similar results were found across all age groups; in both men and women; for both PSG and actigraphic data; and under conditions of fixed sleep periods and participants’ usual sleep schedules. These data are consistent with recent comprehensive reviews that found no consistent or compelling evidence of significant decrements in self-reported sleep duration and/or prevalence of short sleep over a similar range of years [11–15]. Together, these data cast doubt on the notion of a modern epidemic of insufficient sleep.
There were several limitations of the literature, which might have confounded demonstration of temporal changes in sleep duration. First, although virtually all of the studies failed to describe the racial/ethnic composition of the samples, it is a reasonable assumption that participants in most of these studies were not representative of the population. Recent research has suggested that the prevalence of short sleep is relatively high among Blacks, and that this prevalence might be increasing more among Blacks than among Whites [22]. Furthermore, most of the studies either excluded women or failed to report separate data for women and men. Thus, there was an insufficient number of data points (n=17) to adequately assess whether there was a temporal decline in women’s sleep duration, which might have occurred as more women have entered the workforce over the past 50 years [11, 15]. Study samples have also likely been unrepresentative of the population in other factors which have been associated with sleep duration, including employment status, education, occupation, and socioeconomic status.
A second limitation is that most of the studies assessed sleep with PSG in the laboratory, a process that can result in curtailed sleep duration. The confound was reduced in most of the PSG studies by disregarding data obtained during the first night of laboratory recording (eliminating “first night effects”) [23]. Interestingly, in a post-hoc assessment of studies that measured sleep objectively both at home and in the laboratory, the median difference between home and laboratory TST was only 3.2 min (Table 3). However, the use of PSG recording could have inhibited sleep, and sleep might have been more disrupted in earlier PSG studies due to greater novelty associated with PSG, as well as less technologically advanced methods, such as the use of collodion for securing electrodes.
Table 3.
Studies located which assessed sleep objectively both at home and in the laboratory.
| Authors /Year | n | Home TST | Lab TST | Comments |
|---|---|---|---|---|
| Coates et al., 1979 | 8 | 380.8 | 364.1 | |
| Riley, Peterson, 1983 | 10 | 378 | 408 | |
| Edinger et al. 1997 | 32 | Nt 2,3: 371.8 | Nights 2–3: 361.1 | |
| Edinger et al., 2001 | 35 | Nt 2,3: 377.6 | Nights2–3: 376.5 | |
| Edinger et al, 2003 | 35 | 379.6 | 370.5 | |
| Means et al, 2003 | 49 | 376.6 | 371.2 | |
| Penev, 2007 | 12 | 381 | 383 | |
| Kobayashi, et al., 2012 | 22 | 373.1 | 403.7 | Actigraphy home PSG lab |
Constraints of PSG recording might not capture a decline in nighttime sleep that has occurred at home when people are more able to follow their customary habits, which might involve staying up later. Roenneberg et al.’s surveys of thousands of adults assessed from 2002–2010 have found a decline of approximately 30 min in reported sleep duration on weekdays [24]. However, the present review did not find a similar change in home actigraphic sleep duration over the past 10–20 years. Likewise, a recent study by Gubelmann et al. found no decline in reported time in bed from 2005–2011 among a large Swiss sample (n=3,853) [25].
A third limitation is that studies with fixed sleep periods (usually 8 h) could have resulted in sleep restriction for some individuals, particularly if the timing of the sleep periods was not consistent with the participants’ usual sleep schedule. This restriction could have been generally greater in earlier studies if sleep duration truly had declined. However, a similar age-adjusted mean TST was observed for studies involving fixed (443.3±31.7 min) and habitual sleep schedules (435.1±37.4 min), and there was a similar absence of a significant secular trend in TST for fixed and habitual sleep schedules (Figure 6). Figure 6A might reflect a societally-imposed or custom-imposed 8-hr ceiling in how long people usually spend sleeping. It is also possible that PSG technicians have been reluctant to extend the night shift beyond 8 h.
A fourth limitation is that compared with more recent studies, it is possible that earlier studies did not screen as well for absence of sleep apnea and other sleep disorders; this difference in screening methods might have resulted in lower estimates of sleep duration. However among adults above middle age, a small amount of sleep apnea or periodic limb movements is so common that it might be considered normal. Relatively more drug studies in recent years could have contributed to more extensive participant screening of normal sleepers, resulting in samples that sleep longer than population norms. However, a similar absence of a decline in sleep duration was found in the 18–27 year old adults, for whom the prevalence of sleep apnea and other health problems is relatively low. Also contrary to the hypothesis that more recent studies have had more homogenous samples of good sleepers, a post-hoc analysis showed no significant correlation between year of study and sample standard deviation of TST (r=−0.01).
A fifth limitation is that mean nighttime sleep duration data for a sample might not reflect temporal changes in the prevalence of short or long sleep, nor changes in 24-hr sleep duration which might have occurred. Interestingly, Figures 1–3 suggest a higher prevalence of sleep of ≤6 h over the last 20 years, particularly among 18–27 year old participants.
In recent decades, the siesta tradition has waned considerably in some countries [26]. Without corresponding increases in nighttime sleep, this could have resulted in a temporal decline in 24-h sleep in these countries. Partial support for this hypothesis was provided by Bin et al., who found in a meta-analysis that 24-h sleep duration decreased by 22 min from 1989–2002 in Italy [13], whereas there was not a decline in 24-h sleep in 8 of the other 9 countries assessed, none of which has had a notable siesta tradition (Australia, Canada, Finland, Germany, Netherlands, Norway, Sweden, United Kingdom, United States).
However, there has been limited empirical investigation of temporal trends in napping. Wolf-Meyer traces a historical decline in napping to the industrial revolution, increased structure of the work day, and the origins of sleep medicine which has promoted a theoretical need for 8 hours of sleep at night [27, 28]. Thus, through much of the 20th century, napping in many industrialized countries was regarded as a sign of laziness [28]. However, attitudes and practices of napping have apparently changed over the past 10–20 years, as evidenced by formal sanctioning of work-day napping and commercial napping services in some cities.
Napping is relatively more common among older adults who have less nighttime sleep and less consolidation of the sleep-wake cycle than young adults. Compared with previous older cohorts, some factors could have resulted in less napping in contemporary seniors, such as later retirement age, more physically and socially active lifestyles, and greater rates of residence in senior living facilities.
Nonetheless, the present review is the first to explore historical patterns of objective sleep duration, which has long been regarded as the gold standard for defining sleep duration [18]. Further, the findings have several implications. Although historically 8 h of sleep was thought to be optimal for health and well-being, an extensive epidemiologic literature has indicated that 7 h of self-reported sleep is associated with the lowest health risks [29], with progressively higher risks associated with shorter as well as longer reported sleep. However, since objectively-recorded sleep duration is generally 30–60 min less than self-reported sleep, optimal objective sleep duration for longevity and health might be only 6–6.5 h. For example, Kripke et al. recently found 5–6.5 h of actigraphic sleep was associated with lower mortality than <5 h and > 6.5 h [30]. The present review adds to recent reviews of self-reported data, which have also indicated no decline in sleep duration over the last 50 years. If the optimal duration of objective sleep is indeed between 6–6.5 hours, the review also suggests that more participants in these studies might be at risk due to long sleep than to short sleep.
Had sleep duration truly declined by 1–2 hours over the last 50 years, as many sleep researchers have claimed, the signal to detect this would be at least as great as that associated with age, which shows only a decline of about 1 h from young adulthood to the elderly (Figure 1). The results also contradict the hypothesis that such a decline in sleep is a probable culprit in modern epidemics of obesity and diabetes [21].
Notwithstanding these findings, assumptions about a steady decline in sleep duration over the past few decades persist, and could be explained by many factors. First, increased public awareness about sleep and the dangers of inadequate sleep, coinciding with an exponential increase in sleep disorders diagnoses with the emergence of sleep medicine [31], could have partly shaped these perceptions. Greater knowledge about sleep, perhaps especially a greater ability to distinguish between sleep and time spent in bed, could lead to perceptions of less sleep.
Second, sleep is commonly considered in the context of leisure time and being a respite from daily stressors [32]. In what seems to many to be an increasingly fast-paced and stressful world, there is a perception of having less free time for “rest.” Third, evidence indicates that the prevalence of depression has increased over time [33], and depression is associated with reports of poor or inadequate sleep [34].
Fourth, self-reported behavior is influenced by perceived social norms [26, 35], and the perception that we have become a sleep-deprived society has likely been shaped partly by promotion of this message in the popular media and by sleep scientists. However, much of the narrative regarding an epidemic of declining sleep has been based on arguments which have not been well-supported by empirical data. We address some of these arguments in the following section, although much of this discussion is also not well-supported by empirical observations.
Decline of Sleep in Children?
A particularly poignant argument for an epidemic of insufficient sleep is that sleep among children and adolescents has declined, due to many factors, including greater use of electronic media at night and reduced parental enforcement of bedtimes. The fear that children are sleeping less has apparently existed for over a century [36], and in recent years this fear may have contributed to the increased rates of hypnotic prescriptions for children [37].
A recent empirical review by Matricciani et al. found that reported sleep duration of children and adolescents has declined by an average of 70 min per night since 1895 [38]. However, these data should be considered within the context of the tremendous difference in physical activity levels of modern children compared with children of over a century ago who were required to work on family farms, and for 60 h per week in mines, sweatshops, factories, etc. [39]. The Matricciani et al. review found that reported sleep duration of children and adolescents has declined by only about 15 min per night since 1970 [38], and this difference could also be partly explained by dramatic declines in children’s physical activity levels during this period of time, as walking/cycling to school and playing outdoors have been largely replaced by car rides and sedentary indoor activities [40]. Changes in reported sleep duration of children should be verified with a review of objective sleep data analogous to the present review.
Twenty-four hour society?
The cliché of an ever-expanding 24/7 society [41] is not well-supported by empirical evidence, at least not over the past 50 years. For example, evidence suggests that the prevalence of shift-work has remained stable at about 15–20% over this interval of years [42, 43]. Such data might seem counterintuitive in light of the increased number of 24-h services and businesses. However, while many of these businesses (e.g, restaurants and convenience stores) can operate all-night with just a few employees, over the past half-century there has been a dramatic disappearance of factories which once employed thousands of shift-workers. Moreover, over the past 10–20 years, protective regulations and practices which limit shift-work and sleep deprivation and/or better accommodate individual’s preferences (e.g,. flex time and telecommuting), have been implemented for various occupations, including medical residents, truck drivers, and transportation workers [44, 45].
A Decline in Sleep Over the Centuries?
It is a widely repeated hyperbole that never before in human history have we faced such challenges to our sleep [46]. It has been hypothesized that industrialization, urbanization, and technological advances have caused us to ignore or override our natural tendency to sleep more, and we do so at great costs to our health and quality of life. Wolf-Meyer has noted that this “fall from grace” sentiment can be traced back at least as far as the pioneering work of Nathaniel Kleitman [27, 28]. However, historical accounts belie the myth that people slept longer or better centuries ago, when sleep was compromised by pestilence, fear of night marauders, poorer ability to control ambient temperature or treat illnesses, etc. [28, 47]. By Ekirch’s estimation, sleep centuries ago typically occurred in two nighttime in-bed periods, with each period lasting approximately 3–4 h, suggesting that average sleep duration probably did not exceed 7 h (personal communication) [48].
The light bulb has been blamed for sleep loss [49]. However, recent anthropologic studies of people in societies with little or no electricity have failed to indicate that these people sleep more than people in industrialized societies [50, 51].
In summary, it is beyond dispute that disrupted and inadequate sleep are highly prevalent and associated with significant risks, and that experimental sleep deprivation has myriad negative effects [52, 53]. Thus, the notion of a recent epidemic of insufficient sleep, and speculation that this is a primary contributor to modern epidemics of obesity, diabetes, metabolic syndrome, etc., rests largely on the question of whether sleep duration has declined in the last few decades. Consistent with recent reviews of subjective data [11–15, 54], this review does not support this notion, at least not in healthy sleepers
Practice Points.
Systematic reviews of the literature have generally not shown that average self-reported sleep duration has declined, nor that the prevalence of short sleep duration (< 6 h) has increased over the past few decades [11–15].
Limitations of the objective-recording literature include unrepresentative samples; assessment of sleep mostly with PSG under laboratory conditions; and almost no studies of 24-hr sleep patterns.
The data indicate no significant change in objective TST over the last 50+ years.
Reasons for persistent assumptions about a temporal decline in societal sleep duration could include greater knowledge about sleep and the risks of inadequate sleep; increased prevalence of depression; misperceptions about population norms; and persistent claims in the popular and scientific literature regarding a so-called modern epidemic of insufficient sleep.
Research Agenda.
A similar analysis of temporal trends in objective sleep duration in children and adolescents should be undertaken. A recent review indicated a decline in reported sleep duration of about 70 min per night among children and adolescents over the last century [38], which should be confirmed with objective data.
A similar analysis of temporal changes in other measures of objective sleep, such as sleep latency and sleep efficiency, should be conducted to address whether the quality of sleep has changed over time.
Further historical studies focused specifically on sleep duration and other sleep variables might uncover more information about sleep changes over time.
Future large-scale prospective, representative, multi-national studies of objective sleep (using actigraphy) could address whether there are future population changes in sleep.
Acknowledgments
This manuscript is dedicated to Dr. Richard R. Bootzin, our dear friend and colleague who passed away on December 4, 2014. Dr. Bootzin contributed to earlier drafts of this manuscript. Research supported by RO1-HL095799; R01-MD007716; R01-AG034588; R01-AG026364; R01-CA160245; R01-DA032922 the Cousins Center for Psychoneuroimmunology. Susan Noh assisted with this study.
List of Abbreviations
- PSG
polysomnography
- TIB
time in bed
- TST
total sleep time
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National center for health statistics. Quick-Stats: percentage of adults who reported an average of ≤ 6 hours of sleep per 24-hour period, by sex and age group—United States, 1985 and 2004. MMWR Morb Mortal Wkly Rep. 2005;54:933. [Google Scholar]
- 2.Kronholm E, Partonen T, Laatikainen T, Peltonen M, Härmä M, Hublin C, et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. J Sleep Res. 2008;17:54–62. doi: 10.1111/j.1365-2869.2008.00627.x. [DOI] [PubMed] [Google Scholar]
- 3.Jean-Louis G, Williams NJ, Sarpong D, Pandey A, Youngstedt S, Zizi F, et al. Associations between inadequate sleep and obesity in the US population: Analysis of national health interview survey (1977–2009) BMC Public Health. 2014;14:290. doi: 10.1186/1471-2458-14-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ford ES, Cunningham TJ, Croft JB. Trends in self-reported sleep duration among US adults from 1985 to 2012. SLEEP. 2015;38(5):829–832. doi: 10.5665/sleep.4684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *5.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall MH, Smagula SF, Boudreau RM, Ayonayon HN, Goldman SE, Harris TB, et al. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: The health, aging and body composition study. Sleep. 2015 doi: 10.5665/sleep.4394. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *7.Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, et al. Sleep duration and mortality: A prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2014 doi: 10.5665/sleep.4564. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dettoni JL, Consolim-Colombo FM, Drager LF, Rubira MC, Souza SB, Irigoyen MC, et al. Cardiovascular effects of partial sleep deprivation in healthy volunteers. J Appl Physiol. 2012;113:232–236. doi: 10.1152/japplphysiol.01604.2011. [DOI] [PubMed] [Google Scholar]
- 9.Ablin JN, Clauw DJ, Lyden AK, Ambrose K, Williams DA, Gracely RH, et al. Effects of sleep restriction and exercise deprivation on somatic symptoms and mood in healthy adults. Clin Exp Rheumatol. 2013;31(6 Suppl 79):S53–9. [PubMed] [Google Scholar]
- 10.Robertson MD, Russell-Jones D, Umpleby AM, Dijk DJ. Effects of three weeks of mild sleep restriction implemented in the home environment on multiple metabolic and endocrine markers in healthy young men. Metabolism. 2013;62:204–211. doi: 10.1016/j.metabol.2012.07.016. [DOI] [PubMed] [Google Scholar]
- *11.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bin YS, Marshall NS, Glozier N. Secular trends in adult sleep duration: a systematic review. Sleep Med Rev. 2012;16(3):223–230. doi: 10.1016/j.smrv.2011.07.003. [DOI] [PubMed] [Google Scholar]
- *13.Bin YS, Marshall NS, Glozier N. Sleeping at the limits: the changing prevalence of short and long sleep durations in 10 countries. Am J Epidemiol. 2013;177:826–833. doi: 10.1093/aje/kws308. [DOI] [PubMed] [Google Scholar]
- *14.Rowshan Ravan A, Bengtsson C, Lissner L, Lapidus L, Björkelund C. Thirty-six-year secular trends in sleep duration and sleep satisfaction, and associations with mental stress and socioeconomic factors--results of the Population Study of Women in Gothenburg, Sweden. J Sleep Res. 2010;19:496–503. doi: 10.1111/j.1365-2869.2009.00815.x. [DOI] [PubMed] [Google Scholar]
- *15.Bonke J. Trends in short and long sleep in Denmark from 1964 to 2009, and the associations with employment, SES (socioeconomic status) and BMI. Sleep Med. 2015 doi: 10.1016/j.sleep.2014.10.021. in press. [DOI] [PubMed] [Google Scholar]
- 16.Matricciani L. Subjective reports of children’s sleep duration: Does the question matter? A literature review Sleep Med. 2013;14:303–311. doi: 10.1016/j.sleep.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Lauderdale DS. Survey questions about sleep duration: does asking separately about weekdays and weekends matter? Behav Sleep Med. 2014 Mar 4;12(2):158–168. doi: 10.1080/15402002.2013.778201. [DOI] [PubMed] [Google Scholar]
- 18.Means MK, Edinger JD, Glenn DM, Fins AI. Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Medicine. 2003;4:285–296. doi: 10.1016/s1389-9457(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 19.Orff HJ, Drummond SPA, Nowakowski S, Perlis ML. Discrepancy between subjective symptomatology and objective neuropsychological performance in insomnia. Sleep. 2007;30(9):1205–1211. doi: 10.1093/sleep/30.9.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 21.Van Cauter E1, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008;159(Suppl 1):S59–66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: Role of racial/ethnic differences. Sleep Med Rev. 2013;17:255–262. doi: 10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kis A, Szakadát S, Simor P, Gombos F, Horváth K, Bódizs R. Objective and subjective components of the first-night effect in young nightmare sufferers and healthy participants. Behav Sleep Med. 2014;12:469–80. doi: 10.1080/15402002.2013.829062. [DOI] [PubMed] [Google Scholar]
- 24.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–43. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 25.Gubelmann C, Guessous I, Theler JM, Haba-Rubio J, Gaspoz JM, Marques-Vidal P. Trends and determinants of time in bed in Geneva, Switzerland. J Clin Sleep Med. 2014;15:1129–1135. doi: 10.5664/jcsm.4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moore M. Mexicans must say adios to the 3-hour siesta. Washington Post. 1999;23 [Google Scholar]
- 27.Wolf-Meyer M. Where have all our naps gone? Or Nathaniel Kleitman, the consolidation of sleep, and the historiography of emergence. Anthropology of Consciousness. 2013;24:96–116. [Google Scholar]
- *28.Wolf-Meyer MJ. Sleep, Medicine, and Modern American Life. University of Minnesota Press; Minneapolis, MN: 2012. The Slumbering Masses. [Google Scholar]
- 29.Youngstedt SD, Kripke DF. Sleep duration and mortality: Rationale for sleep restriction. Sleep Med Rev. 2004;8:159–174. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 30.Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Med. 2011;12:28–33. doi: 10.1016/j.sleep.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moloney ME1, Konrad TR, Zimmer CR. The medicalization of sleeplessness: a public health concern. Am J Public Health. 2011;101:1429–1433. doi: 10.2105/AJPH.2010.300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson C, Horne JA. Do we really want more sleep? A population-based study evaluating the strength of desire for more sleep. Sleep Med. 2008;9(2):184–7. doi: 10.1016/j.sleep.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 33.Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:10. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meerlo P, Havekes R, Steiger A. Chronically restricted or disrupted sleep as a causal factor in the development of depression. Curr Top Behav Neurosci. 2015 doi: 10.1007/7854_2015_367. in press. [DOI] [PubMed] [Google Scholar]
- 35.Perkins HW, Berkowitz AD. Perceiving the community norms of alcohol use among students: Some research implications for campus alcohol education programming. Int J Addict. 1986;21(9 & 10):961–976. doi: 10.3109/10826088609077249. [DOI] [PubMed] [Google Scholar]
- 36.Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT. Never enough sleep: A brief history of sleep recommendations for children. Pediatrics. 2012;129(3):548–56. doi: 10.1542/peds.2011-2039. [DOI] [PubMed] [Google Scholar]
- 37.Hartz I1, Furu K, Bratlid T, Handal M, Skurtveit S. Hypnotic drug use among 0–17 year olds during 2004–2011: a nationwide prescription database study. Scand J Public Health. 2012;40(8):704–711. doi: 10.1177/1403494812464446. [DOI] [PubMed] [Google Scholar]
- *38.Matricciani L, Olds T, Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012;16(3):203–11. doi: 10.1016/j.smrv.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 39.Children’s Lives at the Turn of the Twentieth Century. [Accessed 13th February 2015];Library of Congress Teaching with Primary Sources. [Online] Available from: http://www.loc.gov/teachers/classroommaterials/primarysourcesets/childrens-lives/pdf/teacher_guide.pdf.
- 40.Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: What are the contributors? Annual Review of Public Health. 2005;26:421–443. doi: 10.1146/annurev.publhealth.26.021304.144437. [DOI] [PubMed] [Google Scholar]
- 41.http://www.huffingtonpost.com/susan-steinbrecher/why-our-247-connected-society-is-driving-us-farther-apart_b_5185925.html. Posted: 04/28/2014 6:50 pm EDT. Updated: 06/28/2014 5:59 am EDT
- 42.Gordon NP, Cleary PD, Parker CE, Czeisler CA. The prevalence and health impact of shiftwork. Am J Public Health. 1986;76:1225–12288. doi: 10.2105/ajph.76.10.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McMenamin TM. A time to work. Recent trends in shiftwork and flexible schedules. Mon Labor Rev. 2007;130:3–15. [Google Scholar]
- 44.Harris JD, Staheli G, LeClere L, Andersone D, McCormick F. What effects have resident work-hour changes had on education, quality of life, and safety? A systematic review. Clin Orthop Relat Res. 2014 doi: 10.1007/s11999-014-3968-0. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Federal Motor Carrier Safety Administration. [Accessed 13th February 2015];Hours of Service. [Online] Available from: http://www.fmcsa.dot.gov/regulations/hours-of-service.
- 46.http://www.cnn.com/2009/HEALTH/03/04/sleep.stress.economy/ Why We’re Sleeping Less. updated 4:08 p.m. EST, Fri March 6, 2009
- *47.Ekirch AR. At Day’s Close: Night in Times Past. W. W. Norton & Company; New York, NY: 2006. [Google Scholar]
- 48.Ekirch AR. Email sent to: Alexandria M Reynolds. Jun 24, 2014.
- 49.http://www.huffingtonpost.com/2013/06/01/electric-light-sleep-circadian-rhythm-cycle_n_3332920.html. How Electric Light Is Harming Our Normal Sleep Cycles. Posted: 06/01/2013 11:03 am EDT. Updated: 06/01/2013 11:03 am EDT
- 50.Worthman CM, Brown RA. Sleep budgets in a globalizing world: Biocultural interactions influence sleep sufficiency among Egyptian families. Soc Sci Med. 2013;79:31–39. doi: 10.1016/j.socscimed.2012.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *51.Knutson KL. Sleep duration, quality, and timing and their associations with age in a community without electricity in Haiti. Am J Hum Biol. 2014;26(1):80–86. doi: 10.1002/ajhb.22481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Irwin MR. Why sleep is important for health: psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143–72. doi: 10.1146/annurev-psych-010213-115205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiat. doi: 10.1016/j.biopsych.2015.05.014. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robinson JP, Michelson W. Sleep as a victim of the “time crunch” – a multinational analysis. Int J Time Use Res (electronic) 2010;7:61–72. [Google Scholar]
- 55.Feinberg I, Keresko RL, Heller N. EEG sleep patterns as a function of normal and pathological aging in man. J Psychiatr Res. 1967;5(2):107–44. doi: 10.1016/0022-3956(67)90027-1. [DOI] [PubMed] [Google Scholar]
- 56.Kahn E, Fisher C, Lieberman L. Sleep characteristics of the human aged female. Compr Psychiatry. 1970;11(3):274–8. doi: 10.1016/0010-440x(70)90174-4. [DOI] [PubMed] [Google Scholar]
- 57.Ryback RS, Lewis OF. Effects of prolonged bed rest on EEG sleep patterns in young, healthy volunteers. Electroencephalogr Clin Neurophysiol. 1971;31(4):395–9. doi: 10.1016/0013-4694(71)90235-5. [DOI] [PubMed] [Google Scholar]
- 58.Williams RL, Karacan I, Thornby JI, Salis PJ. The electroencephalogram sleep patterns of middle-aged males. J Nerv Ment Dis. 1972;154:22–30. doi: 10.1097/00005053-197201000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Brezinova V. The number and duration of the episodes of the various EEG stages of sleep in young and older people. Electroencephalogr Clin Neurophysiol. 1975;39(3):273–8. doi: 10.1016/0013-4694(75)90149-2. [DOI] [PubMed] [Google Scholar]
- 60.Browman CP, Tepas DI. The effects of presleep activity on all-night sleep. Psychophysiology. 1976;13(6):536–40. doi: 10.1111/j.1469-8986.1976.tb00876.x. [DOI] [PubMed] [Google Scholar]
- 61.Karacan I, Thornby JI, Anch M, et al. Dose-related sleep disturbances induced by coffee and caffeine. Clin Pharmacol Ther. 1976;20(6):682–9. doi: 10.1002/cpt1976206682. [DOI] [PubMed] [Google Scholar]
- 62.Walker JM, Floyd TC, Fein G, et al. Effects of exercise on sleep. J Appl Physiol Respir Environ Exerc Physiol. 1978;44(6):945–51. doi: 10.1152/jappl.1978.44.6.945. [DOI] [PubMed] [Google Scholar]
- 63.Gaillard JM. Chronic primary insomnia: Possible physiopathological involvement of slow wave sleep deficiency. Sleep. 1978;1(2):133–47. doi: 10.1093/sleep/1.2.133. [DOI] [PubMed] [Google Scholar]
- 64.Browman CP. Sleep following sustained exercise. Psychophysiology. 1980;17(6):577–80. doi: 10.1111/j.1469-8986.1980.tb02300.x. [DOI] [PubMed] [Google Scholar]
- 65.Adam K. Dietary habits and sleep after bedtime food drinks. Sleep. 1980;3(1):47–58. doi: 10.1093/sleep/3.1.47. [DOI] [PubMed] [Google Scholar]
- 66.Philipson L, Risberg AM, Ingvar DH. Normal sleep pattern analyzed statistically and studied by color “dormograms”. Sleep. 1980;2(4):437–51. doi: 10.1093/sleep/2.4.437. [DOI] [PubMed] [Google Scholar]
- 67.Nicholson AN, Stone BM. Heterocyclic amphetamine derivatives and caffeine on sleep in man. Br J Clin Pharmacol. 1980;9(2):195–203. doi: 10.1111/j.1365-2125.1980.tb05833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Coates TJ, George JM, Killen JD, et al. First night effects in good sleepers and sleep-maintenance insomniacs when recorded at home. Sleep. 1981;4(3):293–8. doi: 10.1093/sleep/4.3.293. [DOI] [PubMed] [Google Scholar]
- 69.Montgomery I, Trinder J, Paxton SJ. Energy expenditure and total sleep time: Effect of physical exercise. Sleep. 1982;5(2):159–68. doi: 10.1093/sleep/5.2.159. [DOI] [PubMed] [Google Scholar]
- 70.Trinder J, Bruck D, Paxton SJ, Montgomery I, Bowling A. Physical fitness, exercise, age and human sleep. Australian Journal of Psychology. 1982;34(2):131–138. [Google Scholar]
- 71.Adam K. Sleep is changed by blood sampling through an indwelling venous catheter. Sleep. 1982;5(2):154–8. [PubMed] [Google Scholar]
- 72.Okuma T, Matsuoka H, Matsue Y, Toyomura K. Model insomnia by methylphenidate and caffeine and use in the evaluation of temazepam. Psychopharmacology (Berl) 1982;76(3):201–8. doi: 10.1007/BF00432545. [DOI] [PubMed] [Google Scholar]
- 73.Paxton SJ, Trinder J, Montgomery I. Does aerobic fitness affect sleep? Psychophysiology. 1983;20(3):320–4. doi: 10.1111/j.1469-8986.1983.tb02162.x. [DOI] [PubMed] [Google Scholar]
- 74.Bunnell DE, Bevier W, Horvath SM. Effects of exhaustive exercise on the sleep of men and women. Psychophysiology. 1983;20(1):50–8. doi: 10.1111/j.1469-8986.1983.tb00900.x. [DOI] [PubMed] [Google Scholar]
- 75.Horne JA, Staff LH. Exercise and sleep: Body-heating effects. Sleep. 1983;6(1):36–46. doi: 10.1093/sleep/6.1.36. [DOI] [PubMed] [Google Scholar]
- 76.Bixler EO, Kales A, Jacoby JA, Soldatos CR, Vela-Bueno A. Nocturnal sleep and wakefulness: Effects of age and sex in normal sleepers. Int J Neurosci. 1984;23(1):33–42. doi: 10.3109/00207458408985343. [DOI] [PubMed] [Google Scholar]
- 77.Matsumoto K, Saito Y, Abe M, Furumi K. The effects of daytime exercise on night sleep. J Hum Ergol (Tokyo) 1984;13(1):31–6. [PubMed] [Google Scholar]
- 78.Paxton SJ, Trinder J, Shapiro CM, et al. Effect of physical fitness and body composition on sleep and sleep-related hormone concentrations. Sleep. 1984;7(4):339–46. doi: 10.1093/sleep/7.4.339. [DOI] [PubMed] [Google Scholar]
- 79.Reynolds CF, 3rd, Kupfer DJ, Taska LS, et al. Slow wave sleep in elderly depressed, demented, and healthy subjects. Sleep. 1985;8(2):155–9. doi: 10.1093/sleep/8.2.155. [DOI] [PubMed] [Google Scholar]
- 80.Bonnet MH. Effect of sleep disruption on sleep, performance, and mood. Sleep. 1985;8(1):11–9. doi: 10.1093/sleep/8.1.11. [DOI] [PubMed] [Google Scholar]
- 81.Kupfer DJ, Sewitch DE, Epstein LH, et al. Exercise and subsequent sleep in male runners: Failure to support the slow wave sleep-mood-exercise hypothesis. Neuropsychobiology. 1985;14(1):5–12. doi: 10.1159/000118193. [DOI] [PubMed] [Google Scholar]
- 82.Carskadon MA, Dement WC. Sleep loss in elderly volunteers. Sleep. 1985;8(3):207–21. doi: 10.1093/sleep/8.3.207. [DOI] [PubMed] [Google Scholar]
- 83.Berry DT, Webb WB. Sleep and cognitive functions in normal older adults. J Gerontol. 1985;40(3):331–5. doi: 10.1093/geronj/40.3.331. [DOI] [PubMed] [Google Scholar]
- 84.Reynolds CF, 3rd, Kupfer DJ, Hoch CC, et al. Sleep deprivation in healthy elderly men and women: Effects on mood and on sleep during recovery. Sleep. 1986;9(4):492–501. doi: 10.1093/sleep/9.4.492. [DOI] [PubMed] [Google Scholar]
- 85.Roehrs T, Kribbs N, Zorick F, Roth T. Hypnotic residual effects of benzodiazepines with repeated administration. Sleep. 1986;9(2):309–16. doi: 10.1093/sleep/9.2.309. [DOI] [PubMed] [Google Scholar]
- 86.Nakagawa Y. Sleep disturbances due to exposure to tone pulses throughout the night. Sleep. 1987;10(5):463–72. doi: 10.1093/sleep/10.5.463. [DOI] [PubMed] [Google Scholar]
- 87.James SP, Mendelson WB, Sack DA, Rosenthal NE, Wehr TA. The effect of melatonin on normal sleep. Neuropsychopharmacology. 1987;1(1):41–4. doi: 10.1016/0893-133x(87)90008-x. [DOI] [PubMed] [Google Scholar]
- 88.Naifeh KH, Severinghaus JW, Kamiya J. Effect of aging on sleep related changes in respiratory variables. Sleep. 1987;10(2):160–71. doi: 10.1093/sleep/10.2.160. [DOI] [PubMed] [Google Scholar]
- 89.Libert JP, Di Nisi J, Fukuda H, et al. Effect of continuous heat exposure on sleep stages in humans. Sleep. 1988;11(2):195–209. doi: 10.1093/sleep/11.2.195. [DOI] [PubMed] [Google Scholar]
- 90.Hudson J, Lipinski J, Frankenburg F, Grochocinski V, Kupfer D. Electroencephaolgraphic sleep in mania. Arch Gen Psychiatry. 1988;45(3):267–73. doi: 10.1001/archpsyc.1988.01800270085010. [DOI] [PubMed] [Google Scholar]
- 91.Schiavi RC, Schreiner-Engel P. Nocturnal penile tumescence in healthy aging men. J Gerontol. 1988;43(5):M146–50. doi: 10.1093/geronj/43.5.m146. [DOI] [PubMed] [Google Scholar]
- 92.Hoch CC, Reynolds CF, 3rd, Kupfer DJ, Berman SR. Stability of EEG sleep and sleep quality in healthy seniors. Sleep. 1988;11(6):521–7. doi: 10.1093/sleep/11.6.521. [DOI] [PubMed] [Google Scholar]
- 93.Mellman T, Uhde T. Electroencephalographic sleep in panic disorder. A focus on sleep-related panic attacks. Arch Gen Psychiatry. 1989;46(2):178–84. doi: 10.1001/archpsyc.1989.01810020080013. [DOI] [PubMed] [Google Scholar]
- 94.Bonnet M. The effect of sleep fragmentation on sleep and performance in younger and older subjects. Neurobiol Aging. 1989;10(1):21–5. doi: 10.1016/s0197-4580(89)80006-5. [DOI] [PubMed] [Google Scholar]
- 95.Lydiard R, Zealberg J, Laraia M, et al. Electroencephalography during sleep of patients with panic disorder. J of Neuropsychiatry. 1989;1(4):372–76. doi: 10.1176/jnp.1.4.372. [DOI] [PubMed] [Google Scholar]
- 96.Saletu B, Frey R, Grunberger J, et al. Sleep laboratory studies on single does effects of suriclone. Br J Clin Pharmacol. 1990;30(5):703–10. doi: 10.1111/j.1365-2125.1990.tb03839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vitiello M, Prinz P, Avery D, et al. Sleep is undisturbed in elderly, depressed individuals who have not sought health care. Biol Psychiatry. 1990;27(4):431–40. doi: 10.1016/0006-3223(90)90553-e. [DOI] [PubMed] [Google Scholar]
- 98.Brendel DH, Reynolds CF, III, Jennings JR, et al. Sleep stage physiology, mood, and vigilance responses to total sleep deprivation in healthy 80-year-olds and 20-year-olds. Psychophysiology. 1990;27(6):677–8. doi: 10.1111/j.1469-8986.1990.tb03193.x. [DOI] [PubMed] [Google Scholar]
- 99.Hoch CC, Reynolds CF, III, Monk TH, et al. Comparison of sleep disordered breathing among healthy elderly in the seventh, eighth, and ninth decades of life. Sleep. 1990;13(6):502–11. doi: 10.1093/sleep/13.6.502. [DOI] [PubMed] [Google Scholar]
- 100.Van Coevorden A, Mockel J, Laurent E, et al. Neuroendocrine rhythms and sleep in aging men. Am J Physiol. 1991;260(4 Pt 1):E651–61. doi: 10.1152/ajpendo.1991.260.4.E651. [DOI] [PubMed] [Google Scholar]
- 101.Lauer CJ, Riemann D, Wiegand M, Berger M. From early to late adulthood changes in EEG sleep of depressed patients and healthy volunteers. Biol Psychiatry. 1991;29(10):979–93. doi: 10.1016/0006-3223(91)90355-p. [DOI] [PubMed] [Google Scholar]
- 102.Monk TH, Reynolds CF, III, Buysee DJ, et al. Circadian characteristics of healthy 80-year-olds and their relationship to objectively recorded sleep. J Gerontol. 1991;46(5):M171–5. doi: 10.1093/geronj/46.5.m171. [DOI] [PubMed] [Google Scholar]
- 103.Wauquier A, van Sweden B, Lagaay AM, Kemp B, Kamphuisen HA. Ambulatory monitoring of sleep-wakefulness patterns in healthy elderly males and females (greater than 88 years): The “Senieur” protocol. J Am Geriatr Soc. 1992;40(2):109–14. doi: 10.1111/j.1532-5415.1992.tb01928.x. [DOI] [PubMed] [Google Scholar]
- 104.Bonnet MH, Arand DL. Caffeine use as a model of acute and chronic insomnia. Sleep. 1992;15(6):526–36. [PubMed] [Google Scholar]
- 105.Hudson J, Lipinski J, Keck j, et al. Polysomnographic characteristics of young manic patients. Arch Gen Psychiatry. 1992;49(5):378–83. doi: 10.1001/archpsyc.1992.01820050042006. [DOI] [PubMed] [Google Scholar]
- 106.Monk TH, Reynolds CF, 3rd, Machen MA, Kupfer DJ. Daily social rhythms in the elderly and their relation to objectively recorded sleep. Sleep. 1992;15(4):322–9. doi: 10.1093/sleep/15.4.322. [DOI] [PubMed] [Google Scholar]
- 107.Buysse DJ, Browman KE, Monk TH, et al. Napping and 24-hour sleep/wake patterns in healthy elderly and young adults. J Am Geriatr Soc. 1992;40(8):779–86. doi: 10.1111/j.1532-5415.1992.tb01849.x. [DOI] [PubMed] [Google Scholar]
- 108.Hirshkowitz M, Moore CA, Hamilton CR, 3rd, Rando KC, Karacan I. Polysomnography of adults and elderly: Sleep architecture, respiration, and leg movement. J Clin Neurophysiol. 1992;9(1):56–62. [PubMed] [Google Scholar]
- 109.Montmayeur A, Buguet A. Sleep patterns of European expatriates in a dry tropical climate. J Sleep Res. 1992;1(3):191–196. doi: 10.1111/j.1365-2869.1992.tb00037.x. [DOI] [PubMed] [Google Scholar]
- 110.Dijk DJ, Czeisler CA. Body temperature is elevated during the rebound of slow-wave sleep following 40-h of sleep deprivation on a constant routine. J Sleep Res. 1993;2(3):117–120. doi: 10.1111/j.1365-2869.1993.tb00073.x. [DOI] [PubMed] [Google Scholar]
- 111.Hoch CC, Dew MA, Reynolds CF, 3rd, et al. A longitudinal study of laboratory- and diary-based sleep measures in healthy “old old” and “young old” volunteers. Sleep. 1994;17(6):489–96. doi: 10.1093/sleep/17.6.489. [DOI] [PubMed] [Google Scholar]
- 112.Gillberg M, Åkerstedt T. Sleep restriction and SWS-suppression: Effects on daytime and night-time recovery. J Sleep Res. 1994;3(3):144–151. doi: 10.1111/j.1365-2869.1994.tb00121.x. [DOI] [PubMed] [Google Scholar]
- 113.Walsh JK, Hartman PG, Schweitzer PK. Slow-wave sleep deprivation and waking function. J Sleep Res. 1994;3(1):16–25. doi: 10.1111/j.1365-2869.1994.tb00099.x. [DOI] [PubMed] [Google Scholar]
- 114.Carrier J, Dumont M. Sleep propensity and sleep architecture after bright light exposure at three different times of day. J Sleep Res. 1995;4(4):202–211. doi: 10.1111/j.1365-2869.1995.tb00171.x. [DOI] [PubMed] [Google Scholar]
- 115.Buguet A, Montmayeur A, Pigeau R, Naitoh P. Modafinil, d-amphetamine and placebo during 64 hours of sustained mental work. II. Effects on two nights of recovery sleep. J Sleep Res. 1995;4(4):229–241. doi: 10.1111/j.1365-2869.1995.tb00173.x. [DOI] [PubMed] [Google Scholar]
- 116.Landolt HP, Werth E, Borbély AA, Dijk DJ. Caffeine intake (200 mg) in the morning affects human sleep and EEG power spectra at night. Brain Res. 1995;675(1–2):67–74. doi: 10.1016/0006-8993(95)00040-w. [DOI] [PubMed] [Google Scholar]
- 117.Hajak G, Rodenbeck A, Bandelow B, et al. Nocturnal plasma melatonin levels after flunitrazepam administration in healthy subjects. Eur Neuropsychopharmacol. 1996;6(2):149–53. doi: 10.1016/0924-977x(96)00005-3. [DOI] [PubMed] [Google Scholar]
- 118.Mann K, Bauer H, Hiemke C, et al. Acute, subchronic and discontinuation effects of zopiclone on sleep EEG and nocturnal melatonin secretion. Eur Neuropsychopharmacol. 1996;6(3):163–8. doi: 10.1016/0924-977x(96)00014-4. [DOI] [PubMed] [Google Scholar]
- 119.Jean-Louis G, von Gizycki H, Zizi F, et al. Determination of sleep and wakefulness with the actigraph data analysis software (ADAS) Sleep. 1996;19(9):739–43. [PubMed] [Google Scholar]
- 120.Carrier J, Monk TH, Buysse DJ, Kupfer DJ. Inducing a 6-hour phase advance in the elderly: Effects on sleep and temperature rhythms. J Sleep Res. 1996;5(2):99–105. doi: 10.1046/j.1365-2869.1996.00015.x. [DOI] [PubMed] [Google Scholar]
- 121.Landolt HP, Roth C, Dijk DJ, Borbély AA. Late-afternoon ethanol intake affects nocturnal sleep and the sleep EEG in middle-aged men. J Clin Psychopharmacol. 1996;16(6):428–36. doi: 10.1097/00004714-199612000-00004. [DOI] [PubMed] [Google Scholar]
- 122.Landolt HP, Dijk DJ, Achermann P, Borbély AA. Effect of age on the sleep EEG: Slow-wave activity and spindle frequency activity in young and middle-aged men. Brain Res. 1996;738(2):205–12. doi: 10.1016/s0006-8993(96)00770-6. [DOI] [PubMed] [Google Scholar]
- 123.Vitiello MV, Larsen LH, Moe KE, et al. Objective sleep quality of healthy older men and women is differentially disrupted by nighttime periodic blood sampling via indwelling catheter. Sleep. 1996;19(4):304–11. doi: 10.1093/sleep/19.4.304. [DOI] [PubMed] [Google Scholar]
- 124.Ehlers CL, Kupfer DJ. Slow-wave sleep: Do young adult men and women age differently? J Sleep Res. 1997;6:211–5. doi: 10.1046/j.1365-2869.1997.00041.x. [DOI] [PubMed] [Google Scholar]
- 125.Haimov I, Lavie P. Circadian characteristics of sleep propensity function in healthy elderly: A comparison with young adults. Sleep. 1997;20(4):294–300. doi: 10.1093/sleep/20.4.294. [DOI] [PubMed] [Google Scholar]
- 126.Carrier J, Monk TH, Buysse DJ, Kupfer DJ. Sleep and morningness-eveningness in the ‘middle’ years of life (20–59 y) J Sleep Res. 1997;6(4):230–7. doi: 10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- 127.Cajochen C, Kräuchi K, Möri D, Graw P, Wirz-Justice A. Melatonin and S-20098 increase REM sleep and wake-up propensity without modifying NREM sleep homeostasis. Am J Physiol. 1997;272(4 Pt 2):R1189–96. doi: 10.1152/ajpregu.1997.272.4.R1189. [DOI] [PubMed] [Google Scholar]
- 128.Edinger JD, Fins AI, Sullivan RJ, Jr, Marsh GR, Dailey DS, Hope TV, et al. Sleep in the laboratory and sleep at home: Comparisons of older insomniacs and normal sleepers. Sleep. 1997;20(12):1119–26. doi: 10.1093/sleep/20.12.1119. [DOI] [PubMed] [Google Scholar]
- 129.Martin SE, Wraith PK, Deary IJ, Douglas NJ. The effect of nonvisible sleep fragmentation on daytime function. Am J Respir Crit Care Med. 1997;155(5):1596–601. doi: 10.1164/ajrccm.155.5.9154863. [DOI] [PubMed] [Google Scholar]
- 130.Hume KI, Van F, Watson A. A field study of age and gender differences in habitual adult sleep. J Sleep Res. 1998;7(2):85–94. doi: 10.1046/j.1365-2869.1998.00103.x. [DOI] [PubMed] [Google Scholar]
- 131.Cajochen C, Kräuchi K, Danilenko KV, Wirz-Justice A. Evening administration of melatonin and bright light: interactions on the EEG during sleep and wakefulness. J Sleep Res. 1998;7(3):145–57. doi: 10.1046/j.1365-2869.1998.00106.x. [DOI] [PubMed] [Google Scholar]
- 132.Blagrove M, Owens DS, MacDonald I, et al. Time of day effects in, and the relationship between, sleep quality and movement. J Sleep Res. 1998;7(4):233–9. doi: 10.1046/j.1365-2869.1998.00119.x. [DOI] [PubMed] [Google Scholar]
- 133.Härmä M, Suvanto S, Popkin S, et al. A dose-response study of total sleep time and the ability to maintain wakefulness. J Sleep Res. 1998;7(3):167–74. doi: 10.1046/j.1365-2869.1998.00115.x. [DOI] [PubMed] [Google Scholar]
- 134.Yassouridis A, Steiger A, Klinger A, Fahrmeir L. Modelling and exploring human sleep with event history analysis. J Sleep Res. 1999;8(1):25–36. doi: 10.1046/j.1365-2869.1999.00133.x. [DOI] [PubMed] [Google Scholar]
- 135.Rao U, Poland RE, Lutchmansingh P, et al. Relationship between ethnicity and sleep patterns in normal controls: Implications for psychopathology and treatment. J Psychiatr Res. 1999;33(5):419–26. doi: 10.1016/s0022-3956(99)00019-9. [DOI] [PubMed] [Google Scholar]
- 136.Lushington K, Dawson D, Kennaway DJ, Lack L. The relationship between 6-sulphatoxymelatonin rhythm phase and age in self-reported good sleeping controls and sleep maintenance insomniacs aged 55–80 years. Psychopharmacology (Berl) 1999;147(1):111–2. doi: 10.1007/s002130051150. [DOI] [PubMed] [Google Scholar]
- 137.Stone BM, Turner C, Mills SL, Nicholson AN. Hypnotic activity of melatonin. Sleep. 2000;23(5):663–9. [PubMed] [Google Scholar]
- 138.Naylor E, Penev PD, Orbeta L, et al. Daily social and physical activity increases slow-wave sleep and daytime neuropsychological performance in the elderly. Sleep. 2000;23(1):87–95. [PubMed] [Google Scholar]
- 139.Hindmarch I, Rigney U, Stanley N, et al. A naturalistic investigation of the effects of day-long consumption of tea, coffee and water on alertness, sleep onset and sleep quality. Psychopharmacology (Berl) 2000;149(3):203–16. doi: 10.1007/s002130000383. [DOI] [PubMed] [Google Scholar]
- 140.Youngstedt SD, O’Connor PJ, Crabbe JB, Dishman RK. The influence of acute exercise on sleep following high caffeine intake. Physiol Behav. 2000;68(4):563–70. doi: 10.1016/s0031-9384(99)00213-9. [DOI] [PubMed] [Google Scholar]
- 141.Armitage R, Hoffmann R, Fitch T, Trivedi M, Rush AJ. Temporal characteristics of delta activity during NREM sleep in depressed outpatients and healthy adults: Group and sex effects. Sleep. 2000;23(5):607–17. [PubMed] [Google Scholar]
- 142.Carrier J, Land S, Buysse DJ, Kupfer DJ, Monk TH. The effects of age and gender on sleep EEG power spectral density in the middle years of life (ages 20–60 years old) Psychophysiology. 2001;38(2):232–42. [PubMed] [Google Scholar]
- 143.Nicolas A, Petit D, Rompre S, Montplaisir J. Sleep spindle characteristics in healthy subjects of different age groups. Clin Neurophysiol. 2001;112(3):521–7. doi: 10.1016/s1388-2457(00)00556-3. [DOI] [PubMed] [Google Scholar]
- 144.Edinger J, Glenn M, Bastain L, et al. Sleep in the laboratory and sleep at home II: Comparison of middle-aged insomnia sufferers and normal sleepers. Sleep. 2001;24(7):761–70. doi: 10.1093/sleep/24.7.761. [DOI] [PubMed] [Google Scholar]
- 145.Pires ML, Benedito-Silva AA, Pinto L, et al. Acute effects of low doses of melatonin on the sleep of young healthy subjects. J Pineal Res. 2001;31(4):326–32. doi: 10.1034/j.1600-079x.2001.310407.x. [DOI] [PubMed] [Google Scholar]
- 146.Roky R, Chapotot F, Hakkou F, Benchekroun MT, Buguet A. Sleep during Ramadan intermittent fasting. J Sleep Res. 2001;10(4):319–27. doi: 10.1046/j.1365-2869.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- 147.Sharkey KM, Fogg LF, Eastman CI. Effects of melatonin administration on daytime sleep after simulated night shift work. J Sleep Res. 2001;10(3):181–92. doi: 10.1046/j.1365-2869.2001.00256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Onen SH, Alloui A, Gross A, Eschallier A, Dubray C. The effects of total sleep deprivation, selective sleep interruption and sleep recovery on pain tolerance thresholds in healthy subjects. J Sleep Res. 2001;10(1):35–42. doi: 10.1046/j.1365-2869.2001.00240.x. [DOI] [PubMed] [Google Scholar]
- 149.Jean-Louis G, Kripke DF, Cole RJ, Assmus JD, Langer RD. Sleep detection with an accelerometer actigraph: comparisons with polysomnography. Physiol Behav. 2001;72(1–2):21–8. doi: 10.1016/s0031-9384(00)00355-3. [DOI] [PubMed] [Google Scholar]
- 150.Jean-Louis G, Kripke DF, Mason WJ, Elliott JA, Youngstedt SD. Sleep estimation from wrist movement quantified by different actigraphic modalities. J Neurosci Methods. 2001;105(2):185–91. doi: 10.1016/s0165-0270(00)00364-2. [DOI] [PubMed] [Google Scholar]
- 151.Gaudreau H, Carrier J, Montplaisir J. Age-related modifications of NREM sleep EEG: From childhood to middle age. J Sleep Res. 2001;10(3):165–72. doi: 10.1046/j.1365-2869.2001.00252.x. [DOI] [PubMed] [Google Scholar]
- 152.Crowley K, Trinder J, Kim Y, Carrington M, Colrain IM. The effects of normal aging on sleep spindle and K-complex production. Clin Neurophysiol. 2002;113(10):1615–22. doi: 10.1016/s1388-2457(02)00237-7. [DOI] [PubMed] [Google Scholar]
- 153.Huber R, Treyer V, Borbély AA, et al. Electromagnetic fields, such as those from mobile phones, alter regional cerebral blood flow and sleep and waking EEG. J Sleep Res. 2002;11(4):289–95. doi: 10.1046/j.1365-2869.2002.00314.x. [DOI] [PubMed] [Google Scholar]
- 154.Baskett JJ, Broad JB, Wood PC, et al. Does melatonin improve sleep in older people? A randomised crossover trial. Age Ageing. 2003;32(2):164–70. doi: 10.1093/ageing/32.2.164. [DOI] [PubMed] [Google Scholar]
- 155.Mukai J, Uchida S, Miyazaki S, Nishihara K, Honda Y. Spectral analysis of all-night human sleep EEG in narcoleptic patients and normal subjects. J Sleep Res. 2003;12(1):63–71. doi: 10.1046/j.1365-2869.2003.00331.x. [DOI] [PubMed] [Google Scholar]
- 156.Brandenberger G, Viola AU, Ehrhart J, et al. Age-related changes in cardiac autonomic control during sleep. J Sleep Res. 2003;12(3):173–80. doi: 10.1046/j.1365-2869.2003.00353.x. [DOI] [PubMed] [Google Scholar]
- 157.Waters WF, Magill RA, Bray GA, et al. A comparison of tyrosine against placebo, phertermine, caffeine, and D-amphetamine during sleep deprivation. Nutr Neurosci. 2003;6(4):221–35. doi: 10.1080/1028415031000120543. [DOI] [PubMed] [Google Scholar]
- 158.Yoon IY, Kripke DF, Youngstedt SD, Elliott JA. Actigraphy suggests age-related differences in napping and nocturnal sleep. J Sleep Res. 2003;12(2):87–93. doi: 10.1046/j.1365-2869.2003.00345.x. [DOI] [PubMed] [Google Scholar]
- 159.Means M, Edinger J, Glenn DM, Fins A. Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med. 2003;4(4):285–96. doi: 10.1016/s1389-9457(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 160.Edinger JD, Glenn DM, Bastian LA, Marsh GR, Dailey D, Hope TV, et al. Daytime testing after laboratory or home-based polysomnography: Comparisons of middle-aged insomnia sufferers and normal sleepers. J Sleep Res. 2003;12(1):45–52. doi: 10.1046/j.1365-2869.2003.00335.x. [DOI] [PubMed] [Google Scholar]
- 161.de Souza L, Benedito-Silva AA, Pires ML, et al. Further validation of actigraphy for sleep studies. Sleep. 2003;26(1):81–5. doi: 10.1093/sleep/26.1.81. [DOI] [PubMed] [Google Scholar]
- 162.Youngstedt SD, Perlis ML, O’Brien PM, et al. No association of sleep with total daily physical activity in normal sleepers. Physiol Behav. 2003;78(3):395–401. doi: 10.1016/s0031-9384(03)00004-0. [DOI] [PubMed] [Google Scholar]
- 163.Kato T, Montplaisir JY, Lavigne GJ. Experimentally induced arousals during sleep: A cross-modality matching paradigm. J Sleep Res. 2004;13(3):229–38. doi: 10.1111/j.1365-2869.2004.00409.x. [DOI] [PubMed] [Google Scholar]
- 164.Benson K, Friedman L, Noda A, et al. The measurement of sleep by actigraphy: Direct comparison of 2 commercially available actigraphs in a nonclinical population. Sleep. 2004;27(5):986–9. doi: 10.1093/sleep/27.5.986. [DOI] [PubMed] [Google Scholar]
- 165.Beaumont M, Batéjat D, Piérard C, et al. Caffeine or melatonin effect on sleep and sleepiness after rapid eastward transmeridian travel. J Appl Physiol (1985) 2004;96(1):50–8. doi: 10.1152/japplphysiol.00940.2002. [DOI] [PubMed] [Google Scholar]
- 166.LaJambe CM, Kamimori GH, Belenky G, Balkin TJ. Caffeine effects on recovery sleep following 27 h total sleep deprivation. Aviat Space Environ Med. 2005;76(2):108–13. [PubMed] [Google Scholar]
- 167.Drapeau C, Hamel-Hébert I, Robillard R, et al. Challenging sleep in aging: The effects of 200 mg of caffeine during the evening in young and middle-aged moderate caffeine consumers. J Sleep Res. 2006;15(2):133–41. doi: 10.1111/j.1365-2869.2006.00518.x. [DOI] [PubMed] [Google Scholar]
- 168.Monk T, Thompson W, Buysse D, et al. Sleep in healthy seniors: A diary study of the relation between bedtime and the amount of sleep obtained. J Sleep Res. 2006;15(3):256–60. doi: 10.1111/j.1365-2869.2006.00534.x. [DOI] [PubMed] [Google Scholar]
- 169.Penev PD. Association between sleep and morning testosterone levels in older men. Sleep. 2007;30(4):427–32. doi: 10.1093/sleep/30.4.427. [DOI] [PubMed] [Google Scholar]
- 170.Hornyak M, Feige B, Voderholzer U, Philipsen A, Riemann D. Polysomnography finding in patients with restless legs syndrome and in healthy controls: A comparative observational study. Sleep. 2007 Jul;30(7):861–5. doi: 10.1093/sleep/30.7.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Robertson JA, Broomfield NM, Espie CA. Prospective comparison of subjective arousal during the pre-sleep period in primary sleep-onset insomnia and normal sleepers. J Sleep Res. 2007;16(2):230–8. doi: 10.1111/j.1365-2869.2007.00579.x. [DOI] [PubMed] [Google Scholar]
- 172.Carrier J, Fernandez-Bolanos M, Robillard R, et al. Effects of caffeine are more marked on daytime recovery sleep than on nocturnal sleep. Neuropsychopharmacology. 2007;32(4):964–72. doi: 10.1038/sj.npp.1301198. [DOI] [PubMed] [Google Scholar]
- 173.Mahlberg R, Kunz D. Melatonin excretion levels and polysomnographic sleep parameters in healthy subjects and patients with sleep-related disturbances. Sleep Med. 2007;8(5):512–6. doi: 10.1016/j.sleep.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 174.Bonnet M, Arand D. EEG arousal norms by age. J Clin Sleep Med. 2007;3(3):271–4. [PMC free article] [PubMed] [Google Scholar]
- 175.Peters KR, Ray L, Smith V, Smith C. Changes in the density of stage 2 sleep spindles following motor learning in young and older adults. J Sleep Res. 2008;17(1):23–33. doi: 10.1111/j.1365-2869.2008.00634.x. [DOI] [PubMed] [Google Scholar]
- 176.Wong KK, Marshall NS, Grunstein RR, Dodd MJ, Rogers NL. Comparing the neurocognitive effects of 40 h sustained wakefulness in patients with untreated OSA and healthy controls. J Sleep Res. 2008;17(3):322–30. doi: 10.1111/j.1365-2869.2008.00665.x. [DOI] [PubMed] [Google Scholar]
- 177.Schmid SM, Hallschmid M, Jauch-Chara K, Born J, Schultes B. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res. 2008;17(3):331–4. doi: 10.1111/j.1365-2869.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 178.O’Donnell D, Silva EJ, Münch M, et al. Comparison of subjective and objective assessments of sleep in healthy older subjects without sleep complaints. J Sleep Res. 2009;18(2):254–63. doi: 10.1111/j.1365-2869.2008.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Cote KA, Milner CE, Smith BA, et al. CNS arousal and neurobehavioral performance in a short-term sleep restriction paradigm. J Sleep Res. 2009;18(3):291–303. doi: 10.1111/j.1365-2869.2008.00733.x. [DOI] [PubMed] [Google Scholar]
- 180.Bixler EO, Papaliaga MN, Vgontzas AN, et al. Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: Effects of age and menopause. J Sleep Res. 2009;18(2):221–8. doi: 10.1111/j.1365-2869.2008.00713.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Paterson LM, Nutt DJ, Ivarsson M, Hutson PH, Wilson SJ. Effects on sleep stages and microarchitecture of caffeine and its combination with zolpidem or trazodone in healthy volunteers. J Psychopharmacol. 2009;23(5):487–94. doi: 10.1177/0269881109104852. [DOI] [PubMed] [Google Scholar]
- 182.Robillard R, Massicotte-Marquez J, Kawinska A, et al. Topography of homeostatic sleep pressure dissipation across the night in young and middle-aged men and women. J Sleep Res. 2010;19(3):455–65. doi: 10.1111/j.1365-2869.2010.00820.x. [DOI] [PubMed] [Google Scholar]
- 183.Morgan PT, Kehne JH, Sprenger KJ, Malison RT. Retrograde effects of triazolam and zolpidem on sleep-dependent motor learning in humans. J Sleep Res. 2010;19(1 Pt 2):157–64. doi: 10.1111/j.1365-2869.2009.00757.x. [DOI] [PubMed] [Google Scholar]
- 184.Marzano C, Ferrara M, Curcio G, De Gennaro L. The effects of sleep deprivation in humans: Topographical electroencephalogram changes in non-rapid eye movement (NREM) sleep versus REM sleep. J Sleep Res. 2010;19(2):260–8. doi: 10.1111/j.1365-2869.2009.00776.x. [DOI] [PubMed] [Google Scholar]
- 185.Ferri R, Drago V, Arico D, et al. The effects of experimental sleep fragmentation on cognitive processing. Sleep Med. 2010;11(4):378–85. doi: 10.1016/j.sleep.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Herbst E, Metzler T, Lenoci M, et al. Adaptation effects to sleep studies in participants with and without chronic posttraumatic stress disorder. Psychophysiology. 2010;47(6):1127–33. doi: 10.1111/j.1469-8986.2010.01030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Vandekerckhove M, Weiss R, Schotte C, et al. The role of presleep negative emotion in sleep physiology. Psychophysiology. 2011;48(12):1738–44. doi: 10.1111/j.1469-8986.2011.01281.x. [DOI] [PubMed] [Google Scholar]
- 188.Brower K, Hoffmann R, Conroy D, Arnedt JT, Armitage R. Sleep homeostasis in alcohol-dependent, depressed and healthy control men. Eur Arch Psychiatry Clin Neurosci. 2011;261(8):559–66. doi: 10.1007/s00406-011-0195-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Rahman K, Burton A, Galbraith S, Lloyd A, Vollmer-Conna U. Sleep-wake behavior in chronic fatigue syndrome. Sleep. 2011;34(5):671–8. doi: 10.1093/sleep/34.5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kogure T, Shirakawa S, Shimokawa M, Hosokawa Y. Automatic sleep/wake scoring from body motion in bed: Validation of a newly developed sensor placed under a mattress. J Physiol Anthropol. 2011;30(3):103–9. doi: 10.2114/jpa2.30.103. [DOI] [PubMed] [Google Scholar]
- 191.Myllymäki T, Kyröläinen H, Savolainen K, et al. Effects of vigorous late-night exercise on sleep quality and cardiac autonomic activity. J Sleep Res. 2011;20(1 Pt 2):146–53. doi: 10.1111/j.1365-2869.2010.00874.x. [DOI] [PubMed] [Google Scholar]
- 192.Gooneratne NS, Bellamy SL, Pack F, et al. Case-control study of subjective and objective differences in sleep patterns in older adults with insomnia symptoms. J Sleep Res. 2011;20(3):434–44. doi: 10.1111/j.1365-2869.2010.00889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Nissen C, Kloepfer C, Feige B, et al. Sleep-related memory consolidation in primary insomnia. J Sleep Res. 2011;20(1 Pt 2):129–36. doi: 10.1111/j.1365-2869.2010.00872.x. [DOI] [PubMed] [Google Scholar]
- 194.Hébert S, Fullum S, Carrier J. Polysomnographic and quantitative electroencephalographic correlates of subjective sleep complaints in chronic tinnitus. J Sleep Res. 2011;20(1 Pt 1):38–44. doi: 10.1111/j.1365-2869.2010.00860.x. [DOI] [PubMed] [Google Scholar]
- 195.Danker-Hopfe H, Dorn H, Bahr A, Anderer P, Sauter C. Effects of electromagnetic fields emitted by mobile phones (GSM 900 and WCDMA/UMTS) on the macrostructure of sleep. J Sleep Res. 2011;20(1 Pt 1):73–81. doi: 10.1111/j.1365-2869.2010.00850.x. [DOI] [PubMed] [Google Scholar]
- 196.Marzano C, De Simoni E, Tempesta D, Ferrara M, De Gennaro L. Sleep deprivation suppresses the increase of rapid eye movement density across sleep cycles. J Sleep Res. 2011;20(3):386–94. doi: 10.1111/j.1365-2869.2010.00886.x. [DOI] [PubMed] [Google Scholar]
- 197.Gonzalez JLB, Fernandez TVS, Rodriguez LA, et al. Sleep architecture in patients with fibromyalgia. Psicothema. 2011;23(3):368–73. [PubMed] [Google Scholar]
- 198.Bianchi M, Wang W, Klerman E. Sleep misperception in healthy adults: Implications for insomnia diagnosis. J Clin Sleep Med. 2012;8(5):547–54. doi: 10.5664/jcsm.2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Schmid MR, Murbach M, Lustenberger C, et al. Sleep EEG alterations: Effects of pulsed magnetic fields versus pulse-modulated radio frequency electromagnetic fields. J Sleep Res. 2012;21(6):620–9. doi: 10.1111/j.1365-2869.2012.01025.x. [DOI] [PubMed] [Google Scholar]
- 200.Ferri R, Bruni O, Fulda S, Zucconi M, Plazzi G. A quantitative analysis of the submentalis muscle electromyographic amplitude during rapid eye movement sleep across the lifespan. J Sleep Res. 2012;21(3):257–63. doi: 10.1111/j.1365-2869.2011.00958.x. [DOI] [PubMed] [Google Scholar]
- 201.Jaehne A, Unbehaun T, Feige B, et al. How smoking affects sleep: A polysomnographical analysis. Sleep Med. 2012;13(10):1286–92. doi: 10.1016/j.sleep.2012.06.026. [DOI] [PubMed] [Google Scholar]
- 202.Frey S, Birchler-Pedross A, Hofstetter M, et al. Challenging the sleep homeostat: Sleep in depression is not premature aging. Sleep Med. 2012;13(7):933–45. doi: 10.1016/j.sleep.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 203.Schmid MR, Loughran SP, Regel SJ, et al. Sleep EEG alterations: Effects of different pulse-modulated radio frequency electromagnetic fields. J Sleep Res. 2012;21(1):50–8. doi: 10.1111/j.1365-2869.2011.00918.x. [DOI] [PubMed] [Google Scholar]
- 204.Wulff K, Dijk DJ, Middleton B, Foster R, Joyce E. Sleep and circadian rhythm disruption in schizophrenia. Br J Psychiatry. 2012;200(4):308–16. doi: 10.1192/bjp.bp.111.096321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Scatena M, Dittoni S, Maviglia R, et al. An integrated video-analysis software system designed for movement detection and sleep analysis. Validation of a tool for the behavioural study of sleep. Clin Neurophysiol. 2012;123(2):318–23. doi: 10.1016/j.clinph.2011.07.026. [DOI] [PubMed] [Google Scholar]
- 206.Flausino NH, Da Silva Prado JM, de Queiroz SS, Tufik S, de Mello MT. Physical exercise performed before bedtime improves the sleep pattern of healthy young good sleepers. Psychophysiology. 2012;49(2):186–92. doi: 10.1111/j.1469-8986.2011.01300.x. [DOI] [PubMed] [Google Scholar]
- 207.Kobayashi I, Huntley E, Lavela J, Mellman TA. Subjectively and objectively measured sleep with and without posttraumatic stress disorder and trauma exposure. Sleep. 2012;35(7):957–65. doi: 10.5665/sleep.1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Shambroom JR, Fábregas SE, Johnstone J. Validation of an automated wireless system to monitor sleep in healthy adults. J Sleep Res. 2012;21(2):221–30. doi: 10.1111/j.1365-2869.2011.00944.x. [DOI] [PubMed] [Google Scholar]
- 209.Holz J, Piosczyk H, Feige B, et al. EEG Σ and slow-wave activity during NREM sleep correlate with overnight declarative and procedural memory consolidation. J Sleep Res. 2012;21(6):612–9. doi: 10.1111/j.1365-2869.2012.01017.x. [DOI] [PubMed] [Google Scholar]
- 210.Robertson MD, Russell-Jones D, Umpleby AM, Dijk DJ. Effects of three weeks of mild sleep restriction implemented in the home environment on multiple metabolic and endocrine markers in healthy young men. Metabolism. 2013;62(2):204–11. doi: 10.1016/j.metabol.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 211.Rosipal R, Lewandowski A, Dorffner G. In search of objective components for sleep quality indexing in normal sleep. Biol Psychol. 2013;94(1):210–20. doi: 10.1016/j.biopsycho.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Ferri R, Zucconi M, Marelli S, et al. Effects of long-term use of clonazepam on nonrapid eye movement sleep patterns in rapid eye movement sleep behavior disorder. Sleep Med. 2013;14(5):399–406. doi: 10.1016/j.sleep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 213.Chellappa SL, Steiner R, Oelhafen P, et al. Acute exposure to evening blue-enriched light impacts on human sleep. J Sleep Res. 2013;22(5):573–80. doi: 10.1111/jsr.12050. [DOI] [PubMed] [Google Scholar]
- 214.Ju Y, McLeland J, Toedebusch C, et al. Sleep quality and preclinical Alzheimer disease. JAMA Neurol. 2013;70(5):587–93. doi: 10.1001/jamaneurol.2013.2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Winser MA, McBean AL, Montgomery-Downs HE. Minimum duration of actigraphy-defined nocturnal awakenings necessary for morning recall. Sleep Med. 2013;14(7):688–91. doi: 10.1016/j.sleep.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 216.Lombardi C, Meriggi P, Agostoni P, et al. High-altitude hypoxia and periodic breathing during sleep: Gender-related differences. J Sleep Res. 2013;22(3):322–30. doi: 10.1111/jsr.12012. [DOI] [PubMed] [Google Scholar]
- 217.Robey E, Dawson B, Halson S, et al. Effect of evening postexercise cold water immersion on subsequent sleep. Med Sci Sports Exerc. 2013;45(7):1394–402. doi: 10.1249/MSS.0b013e318287f321. [DOI] [PubMed] [Google Scholar]
- 218.Petersen H, Kecklund G, D’Onofrio P, Nilsson J, Åkerstedt T. Stress vulnerability and the effects of moderate daily stress on sleep polysomnography and subjective sleepiness. J Sleep Res. 2013;22(1):50–7. doi: 10.1111/j.1365-2869.2012.01034.x. [DOI] [PubMed] [Google Scholar]
- 219.Richards A, Metzler TJ, Ruoff LM, et al. Sex differences in objective measures of sleep in post-traumatic stress disorder and healthy control subjects. J Sleep Res. 2013;22(6):679–87. doi: 10.1111/jsr.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Saxvig IW, Wilhelmsen-Langeland A, Pallesen S, et al. Objective measures of sleep and dim light melatonin onset in adolescents and young adults with delayed sleep phase disorder compared to healthy controls. J Sleep Res. 2013;22(4):365–72. doi: 10.1111/jsr.12030. [DOI] [PubMed] [Google Scholar]
- 221.Tonetti L, Cellini N, de Zambotti M, et al. Polysomnographic validation of a wireless dry headband technology for sleep monitoring in healthy young adults. Physiol Behav. 2013;118:185–188. doi: 10.1016/j.physbeh.2013.05.036. [DOI] [PubMed] [Google Scholar]
- 222.O’Hare E, Flanagan D, Penzel T, et al. A comparison of radio-frequency biomotion sensors and actigraphy versus polysomnography for the assessment of sleep in normal subjects. Sleep Breath. 2014 doi: 10.1007/s11325-014-0967-z. in press. [DOI] [PubMed] [Google Scholar]