Abstract
Objective
Obesity is a heritable condition with well-established risk-reducing behaviours. Studies have shown that beliefs about the causes of obesity are associated with diet and exercise behaviour. Identifying mechanisms linking causal beliefs and behaviours is important for obesity prevention and control.
Design
Cross-sectional multi-level regression analyses of self-efficacy for weight control as a possible mediator of obesity attributions (diet, physical activity, genetic) and preventive behaviours in 487 non-Hispanic White women from South King County, Washington.
Main Outcome Measures
Self-reported daily fruit and vegetable intake and weekly leisure-time physical activity.
Results
Diet causal beliefs were positively associated with fruit and vegetable intake, with self-efficacy for weight control partially accounting for this association. Self-efficacy for weight control also indirectly linked physical activity attributions and physical activity behaviour. Relationships between genetic causal beliefs, self-efficacy for weight control, and obesity-related behaviours differed by obesity status. Self-efficacy for weight control contributed to negative associations between genetic causal attributions and obesity-related behaviours in non-obese, but not obese, women.
Conclusion
Self-efficacy is an important construct to include in studies of genetic causal beliefs and behavioural self-regulation. Theoretical and longitudinal work is needed to clarify the causal nature of these relationships and other mediating and moderating factors.
Keywords: obesity, causal beliefs, self-efficacy, diet behaviour, physical activity, genetic attributions
Introduction
With the number of genetic variants implicated in multifactorial conditions steadily increasing, characterizing genetic causal beliefs’ (genetic attributions; perceptions that a trait is due to genetic factors) impact on health behaviour is important for informing genomics’ integration into health promotion efforts (O'Neill, McBride, Alford, & Kaphingst, 2010). Pressing questions include whether greater attention to the genetic determinants of disease will increase perceptions that diseases are predetermined and change beliefs and behaviours related to prevention and treatment (Henrikson, Bowen, & Burke, 2009; Waters, Muff, & Hamilton, 2014). Messaging about genetic risk factors, including the provision of genetic tests, has been hypothesized to have both beneficial and detrimental effects on risk-management through self-regulation, alternatively motivating and discouraging individuals to initiate and maintain important health behaviours (Carlsten & Burke, 2006). Many health behaviour theories propose that responses to new risk information are influenced by prior beliefs and perceptions (e.g. social cognitive theory, protection motivation theory). Therefore clarifying how causal beliefs influence current behaviour is an important step towards better understanding genetic information's impact on behavioural self-regulation (Bandura, 1986; Floyd & Prentice-Dunn, 2000).
Obesity, defined as a body mass index (BMI) of 30 or more, presents an ideal context for exploring causal beliefs’ influence on risk reducing health behaviour. Obesity prevention and control are major public health priorities due to its increasing prevalence, impact on downstream health outcomes, and associated health care system costs (Flegal, Carrol, Ogden, & Curtin, 2010). Obesity is estimated to be 40-70% heritable and more than seventy five variants have been associated with obesity-related phenotypes in genome-wide association studies (Willyard, 2014). Lifestyle behaviours that decrease obesity risk are well established and rapidly rising rates of obesity suggest that environmental and behavioural factors play a critical causal role (Frazier, Mason, Zhuang, & Beeler, 2008; Hofker & Wijmenga, 2009). Still, genetic risk factors for obesity are increasingly highlighted by the media and recognized by the general public (Persky, Sanderson, & Koehly, 2013).
Prior studies focusing on causal explanations for obesity and their relationship with health behaviour are limited. In a clinical sample of obese men and women seeking genetic testing and counseling for weight control, Hilbert et al. (2009) observed that genetic attributions for obesity were common (endorsed by 86% of women and 59.7% of men), but unrelated to restrained eating and physical activity behaviours over the next six months. Other clinical studies have found that attributing excess weight to a physical origin, like genes, predicted poorer weight management in obese individuals trying to lose weight (Wamsteker et al., 2005). In the general population, Wang and Coups (2010) observed that 72% of respondents to the 2007 Health Information National Trends Survey (HINTS) endorsed the belief that lifestyle behaviours have ‘a lot’ to do with causing obesity, compared to 19% who believed the same of inheritance. Despite a lower prevalence, the belief that obesity is inherited was associated with lower self-reported rates of both physical activity and fruit and vegetable intake, while lifestyle causal beliefs were associated with greater reported levels of physical activity. These findings highlight the need for additional research on the correlates and consequences of causal explanations for obesity. Specifically, there is a need to replicate associations between causal attributions and behaviour in non-clinical populations and to identify potential mechanisms linking existing obesity causal beliefs with risk-reducing behaviours.
Self-efficacy is a key construct in the health promotion literature and a frequent target of obesity-related interventions that modify diet and physical activity behaviours (Olander et al., 2013). First formalized in Bandura's social learning theory, self-efficacy refers to individuals’ beliefs about their capacity to coordinate skills and abilities to attain desired goals in specific domains and circumstances (Bandura, 1977). Self-efficacy has since become a central component of a number of important health behaviour theories including social cognitive theory (Bandura, 1986), protection motivation theory (Maddux & Rogers, 1983), the extended parallel process model (Witte, 1994), and the health belief model developed by Rosenstock, Hochbaum, Kegeles, and Leventhal (Champion & Skinner, 2008). Many of these theories assert that perceived self-efficacy and subsequent attempts at behavioural self-regulation are influenced by past knowledge and explanations for successes and failures, suggesting that self-efficacy could mediate association between causal beliefs and behaviour (Shields, Brawley, & Lindover, 2006). Specifically, it has been hypothesized that attributing obesity to genetic causes may decrease self-efficacy for weight control, diet, and exercise behaviours due to fatalism or a loss of confidence in ability to carry out changes in these behaviours (Hilbert et al., 2009; Sanderson, Persky, & Mitchie, 2009).
The relationship between obesity causal beliefs and self-efficacy remains unclear. In clinical samples of obese individuals trying to lose weight, genetic causal attributions for obesity were unrelated to generalized self-efficacy (Hilbert et al., 2009) and eating self-efficacy did not differ between individuals informed of their genetic risk for obesity based on their b3-adrenergic receptor (b3AR) status (Harvey-Berino et al., 2001). However in a non-obese sample, Frosch et al. (2005) found that receiving a hypothetical genetic test result indicating high obesity risk lowered confidence in ability to maintain a healthy diet, though a similar study found no association between obesity risk information, genetic or otherwise, and diet self-efficacy (Sanderson, Persky, & Mitchie, 2009). A better understanding of self-efficacy as a potential mediator linking obesity causal beliefs and health behaviour will help inform future obesity prevention and control interventions, including those designed to alter or reinforce existing causal beliefs to facilitate behaviour change. This motivated the current analysis.
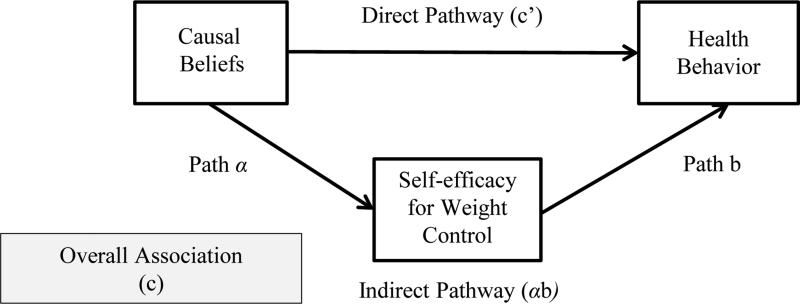
Drawing on prior research and theory we tested the relationship between causal beliefs and obesity-related health behaviours and hypothesized that this relationship would be partially explained by self-efficacy for weight control (Figure 1). We defined self-efficacy for weight control as a domain-specific efficacy expectation that encompasses an individuals’ judgment of their capacity to successfully control their weight. To help guide future longitudinal mediation analyses we tested the following hypotheses using baseline data from a cohort of 30-50 year old non-Hispanic White women living in South King County, WA:
-
(1)
Diet causal beliefs will be associated with greater fruit and vegetable intake. The link between diet causal beliefs and behaviour will be partially explained by self-efficacy for weight control, where diet causal beliefs are associated with higher self-efficacy.
-
(2)
Physical activity causal beliefs will be associated with greater weekly leisure-time physical activity. The link between physical activity causal beliefs and behaviour will be partially explained by self-efficacy for weight control, where physical activity causal beliefs are associated with higher self-efficacy.
-
(3)
Genetic causal beliefs will be inversely associated with fruit and vegetable intake and weekly leisure-time physical activity. Links between genetic causal beliefs and these behaviours will be partially explained by self-efficacy for weight control, where genetic causal beliefs are associated with lower self-efficacy.
Figure 1.
Conceptual model depicting relationships between obesity causal beliefs, self-efficacy for weight control, and obesity-related behaviours.
Method
Participants and procedures
Data was drawn from the baseline visit of the Socioeconomic Status and Obesity Study (SESO)—a longitudinal cohort study designed to evaluate individual- and area-level mechanisms linking socioeconomic status and obesity in Hispanic and non-Hispanic White women living in South King County, Washington. Women were recruited door-to-door beginning in 2010 using a population-based multi-stage sampling method adapted from the Los Angeles Family and Neighborhood Survey (Sastry, Ghosh-Dastidar, Adams, & Pebley, 2006). Groups of houses in 143 randomly chosen census block-groups with a high representation of Hispanic, low education, and low income households (as determined by 2000 census data) were approached by female study interviewers to determine residency of an eligible women. Eligible women self-identified as Hispanic or non-Hispanic White and were aged 30-50 years, fluent in English or Spanish, and planning to remain in the area over the next 2 years. To achieve a spread of educational levels for SESO's main analyses, all Hispanic women and all non-Hispanic White women who had completed high school or earned a GED were invited to participate, while only a subset of non-Hispanic White women with more than a high school degree were randomly selected to join the study. For households with more than one eligible woman the respondent with the most recent birthday was invited. Women who agreed to participate and provided written informed consent completed a baseline pen and paper survey in English or Spanish and had their height and weight measured. A total of 1,018 women (515 Hispanic, 506 Caucasian) were confirmed eligible and enrolled in the cohort, for a final response rate of 34.1% (The American Association for Public Opinion Research, 2008). All SESO procedures were approved by the University of Washington Institutional Review Board.
Analyses for the present study were confined to non-Hispanic White women who were not currently pregnant and had complete information on education, height, and weight (N=487). Hispanic women, who were largely Spanish-speaking and almost exclusively of Mexican origin, were excluded from the present study based on an a priori hypothesis that relationships between obesity causal beliefs and health behaviours may differ by ethnicity and degree of US acculturation and warranted separate study (Allan, 1998; New, Xiao, & Ma, 2013).
Measures
Demographics were measured as follows. Participants self-identified their race from a list of options (White; Black or African American; Asian; Hawaiian or other Pacific Islander; American Indian, Native American, or Alaskan Native) and self-reported Hispanic origin during screening. Participants also self-reported their date of birth and highest level of education from a list of options, ranging from one (no schooling completed) to 16 (doctorate degree), which were categorized into the follow five groups for analysis: at least some high school; at least some college; college graduate or baccalaureate degree; college or professional degree after college graduation; and master's or doctoral degree. Body mass index (BMI) was calculated from height and weight measured by interviews at study enrollment. Individuals were categorized into three groups based on National Institutes of Health (NIH) BMI classifications: underweight/normal weight; overweight; and obese/morbidly obese (National Heart Lung and Blood Institute, 1998).
Obesity causal beliefs were assessed with three separate questions, modeled on those used in the HINTS 2007 survey, but measuring beliefs about diet and exercise with separate items (Cantor et al., 2009). To assess genetic causal beliefs, individuals were asked, ‘To what extent do you believe that obesity is inherited,’ with the response options ranging on a four-point Likert-type scale from ‘not at all’ to ‘a lot’. Beliefs about lifestyle behaviours were measured in the same way, asking, ‘To what extent do you believe that obesity is caused by not eating a healthy diet’ and ‘To what extent do you believe that obesity is caused by not exercising regularly’. Throughout the baseline survey, a ‘healthy diet’ was defined as eating plenty of fruits and vegetables and not too much sugar or fatty foods and ‘exercising regularly’ was defined as exercising at least three times a week.
Self-efficacy for weight control was assessed with the question: ‘How sure are you that you will control your weight next year.’ Response options fell on a zero to 9 scale ranging from ‘not sure’ to ‘very sure’. A similar measure has been used previously to examine the effects of perceived self-efficacy for weight control on diet and exercise behaviours in older adults (Grembowski et al., 1993).
Daily fruit and vegetable intake was measured with a single item that showed quantities of different fruits and vegetables that count as one serving and then asked participants to report the number of servings of fruits and vegetables they eat each day, with response options ranging from zero to 11 servings or more. Participants were asked to mark only one answer and give their best guess (Beresford, Thompson, Feng, Christianson, McLerran, & Patrick, 2001).
Physical activity was measured using a modified Godin Leisure-Time Exercise Questionnaire (Godin & Shephard, 1985). Individuals reported how many times per week they completed more than 10 minutes of strenuous, moderate, and mild physical activity. Examples of different types of activities falling into each category, as well as definitions, were provided. Weekly frequencies of each category of exercise were weighted using approximate metabolic equivalents (METs) of nine, five, and three, respectively. Given that mild activity contributes minimally to many health outcomes, we calculated a total weekly leisure activity score based on the contributions of moderate and strenuous activity only, in accordance with Godin's updated recommendations (2011). For women who did not indicate a response for a specific category, it was assumed that they did no activity within that category. As such, an overall score was calculated using zero frequency for missing responses.
Statistical analyses
To determine if self-efficacy for weight control accounts for relationships between obesity causal beliefs and health behaviours we conducted multilevel regression analyses following the methods of Krull and MacKinnon (2001) for situations where predictors, mediators, and outcomes are all individual level variables. Multilevel methods were needed to account for the data structure created by sampling women within select census block groups. Maximum likelihood estimation (MLE) was used to generate estimates from a series of mixed-effects linear regression equations. For each of the regression models described in hypotheses 1-3 we first determined the association between the predictor variable (Xij = genetic, diet, or physical activity beliefs) and the behavioural outcome of interest (Yij = fruit and vegetable intake or physical activity) to provide an estimate of the overall influence (c) of causal beliefs on behaviour (Equation 1, Level 1: Yij = β0j + βcXij + rij). We then determined the association between obesity causal beliefs and self-efficacy for weight control (Mij) (Equation 2, Level 1: Mij = β0j + βαXij + rij) and the impact of obesity causal beliefs on the behavioural outcome while controlling for self-efficacy (Equation 3, Level 1: Yij = β0j + βc’Xij + βbMij + rij). All regressions accounted for study design factors by including census block group as a random effect and education as fixed-effect covariates and also adjusted for BMI. We tested for effect modification by BMI and conducted stratified analyses as needed. Sensitivity analyses adjusting competing causal beliefs as fixed-effect covariates were conducted to explore the robustness of the findings.
To ensure that the same individuals were used throughout the analyses we created an analytic data set for each model that excluded women missing data for the specific predictor and outcome of interest. Coefficients from Equations 2 and 3 were used to calculate indirect (α*b) and direct (c’) pathways for each model following the product of coefficients method. We estimated the standard error of the indirect and direct pathways and nonparametrically tested their significance by constructing bias-corrected bootstrap confidence intervals (1,000 replications) (Mackinnon, Warsi, & Dwyer, 1995; Preacher & Hayes, 2004). All statistical analyses were conducted using Stata 12 software (StataCorp, 2011).
Results
Descriptives
Descriptive characteristic for the study sample are given in Table 1. Table 2 provides means and correlations for all study variables. Means for the diet and physical activity causal beliefs were similar, 3.35 (SD=0.73) and 3.33 (SD=0.72), respectively, but were lower for genetic causal attributions (2.49, SD=0.74), indicating more women believed that obesity is caused by not eating a healthy diet and not exercising regularly than believed that obesity is inherited. Overall, women consumed approximately three and half servings of fruits and vegetables a day (SD: 1.85). The mean Godin score was 29.43, which meets the Surgeon General's recommendations for weekly exercise, but the range of reported physical activity was large (SD: 21.96). Education was positively correlated with diet and physical activity causal beliefs, self-efficacy for weight control, and fruit and vegetable intake, but was not correlated with genetic causal beliefs or weekly physical activity scores. Age was not correlated with either behavioural outcome. BMI was negatively correlated with self-efficacy for weight control and both behavioural outcomes as well as positively correlated with genetic causal beliefs. Women from 118 different census block groups were included in the sample, with approximately four women representing each block group, providing adequate sample size at the group level for the multilevel analyses (Krull & MacKinnon, 2001).
Table 1.
Sample characteristics.
| N, % | ||
|---|---|---|
| Overall | 487 | |
| Number of block group clusters | 118 | |
| Age | ≥ 40 (Range 30-50) | 228, 46.8 |
| Education | At least some high school | 102, 20.9 |
| At least some college | 144, 29.6 | |
| College graduate or baccalaureate degree | 116, 23.8 | |
| College or professional degree after college graduation | 27, 5.5 | |
| Master's or doctoral degree | 98, 20.1 | |
| BMI | Underweight or normal weight | 184, 37.8 |
| Overweight | 106, 21.8 | |
| Obese or morbidly obese | 197, 40.5 | |
| Gen. beliefs | Don't believe at all | 29, 6.0 |
| Believe a little | 235, 48.3 | |
| Believe quite a bit | 177, 36.3 | |
| Believe a lot | 44, 9.0 | |
| Missing | 2, 0.4 | |
| Diet beliefs | Don't believe at all | 10, 2.1 |
| Believe a little | 43, 8.8 | |
| Believe quite a bit | 199, 40.9 | |
| Believe a lot | 233, 47.8 | |
| Missing | 2, 0.4 | |
| PA beliefs | Don't believe at all | 6, 1.2 |
| Believe a little | 54, 11.1 | |
| Believe quite a bit | 199, 40.9 | |
| Believe a lot | 227, 46.6 | |
| Missing | 1, 0.2 | |
| SE | ≥ 5 (Range 0-9) | 378, 77.6 |
| Missing | 1, 0.2 | |
| FV | ≥ 5 fruits or vegetables a day | 129, 26.5 |
| Missing | 3, 0.6 | |
| PA | < 14 METS (7 kcal/kg/week) | 104, 21.4 |
| 14-23 METS (7-13.9 kcal/kg/week) | 100, 20.5 | |
| > 23 METS (13.9 kcals/kg/week) | 269, 55.2 | |
| Missing | 14, 2.9 | |
Notes: BMI = body mass index, Gen. = genetic, PA = physical activity, SE = self-efficacy for weight control, FV = daily fruit and vegetable intake, PA = weekly leisure-time physical activity, METS = metabolic equivalents, kcal = kilocalorie, kg= kilogram. Numbers may not sum to 100 due to rounding error.
Table 2.
Means and intercorrelations for study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | −1.73*** | 0.11* | 0.04 | −0.12** | −0.05 | −0.08 | −0.09 | −0.03 | |
| 2. Education | −0.29*** | −0.04 | 0.13** | 0.14** | 0.17*** | 0.30*** | 0.08 | ||
| 3. BMI | 0.17*** | −0.09 | 0.01 | −0.43*** | −0.20*** | −0.12** | |||
| 4. Gen. beliefs | −0.04 | −0.05 | −0.12** | −0.09* | 0.05 | ||||
| 5. Diet beliefs | 0.37*** | 0.15** | 0.15*** | 0.01 | |||||
| 6. PA beliefs | 0.09 | 0.15** | 0.06 | ||||||
| 7. SE | 0.23*** | 0.20*** | |||||||
| 8. FV | 0.25*** | ||||||||
| 9. PA | |||||||||
| Mean | 39.90 | 2.74 | 2.03 | 2.49 | 3.35 | 3.33 | 6.15 | 3.51 | 29.43 |
| SD | 6.04 | 1.39 | 0.89 | 0.74 | 0.73 | 0.72 | 2.34 | 1.85 | 21.96 |
Notes: N=487, Non-Hispanic White women aged 30-50. BMI = body mass index, Gen. = genetic, PA = physical activity, SE = self-efficacy for weight control, FV = daily fruit and vegetable intake, PA = weekly leisure-time physical activity.
p < 0.05
p < 0.01
p<0.001.
Diet and physical activity causal beliefs and obesity-related behaviours
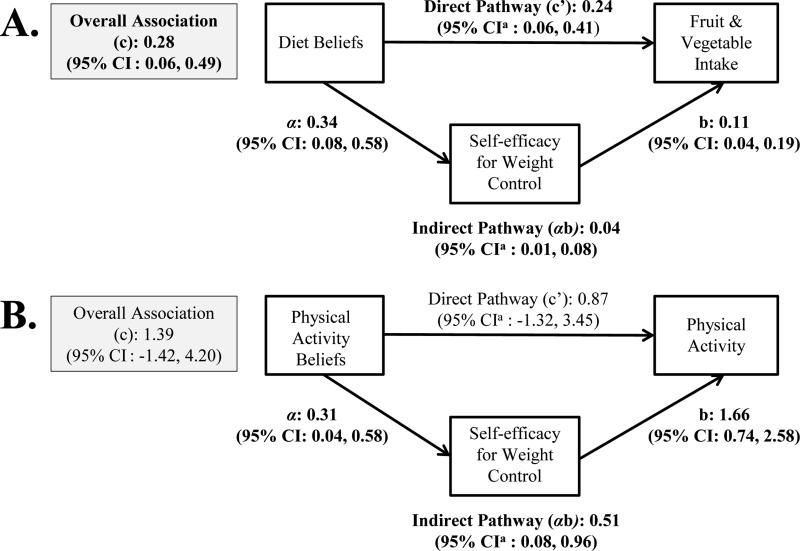
Figure 2 summarizes the results of the regression analyses for the two models considering diet and physical activity causal beliefs and the corresponding obesity-related behaviours, adjusted for education and BMI. Diet causal beliefs were positively associated with daily fruit and vegetable intake (Figure 2A: c = 0.28, 95% CI: 0.06, 0.49). An indirect pathway through self-efficacy for weight control was also present in this model (Figure 2A: αb = 0.04, 95% CI: 0.01, 0.08). Controlling for self-efficacy for weight control, the association between diet beliefs and daily fruit and vegetable intake remained positive and significant (Figure 2A: c’ = 0.24, 95% CI: 0.06, 0.41). Physical activity causal beliefs were not associated with weekly leisure-time physical activity in our sample. Still, an indirect pathway through self-efficacy for weight control linked physical activity attributions and exercise behaviour in this model (Figure 2B: (αb = 0.51, 95% CI: 0.08, 0.096).
Figure 2.
Associations between diet and physical activity causal beliefs, self-efficacy for weight control, and obesity-related behaviours.
A. N=482
B. N=471
Notes: These analyses are adjusted for education and BMI. Estimates are bolded when confidence interval excludes zero.
aBias-corrected confidence interval generated via bootstrapping.
Genetic causal beliefs and fruit and vegetable intake
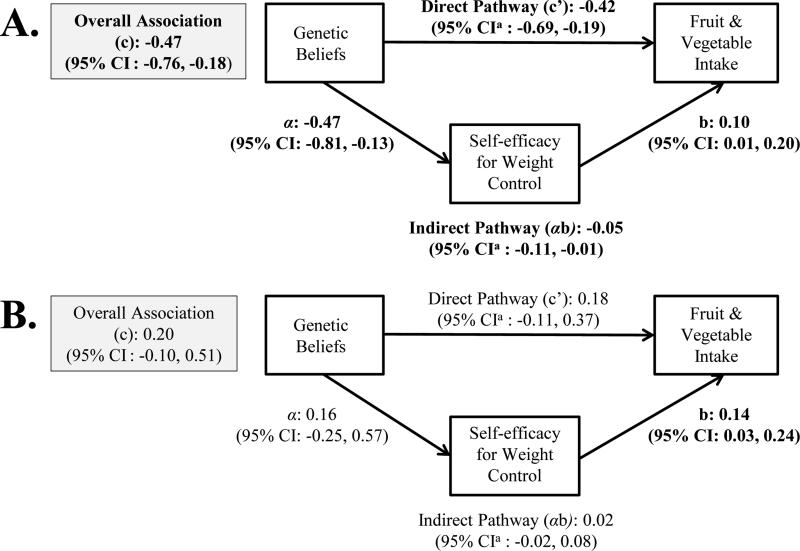
There was evidence of effect modification by BMI in the models considering genetic causal beliefs about obesity, self-efficacy for weight control, and obesity-related behaviours. Specifically, associations between genetic causal beliefs and daily fruit and vegetable intake as well as genetic causal beliefs and self-efficacy for weight control differed significantly by BMI. Thus, hypothesis 3 was evaluated separately in non-obese and obese women. Figure 3 summarizes the results of the regression analyses considering genetic causal beliefs and daily fruit and vegetable intake, adjusted for education, by obesity status. In non-obese women, genetic causal beliefs were negatively associated with daily fruit and vegetable intake (Figure 3A: α = −0.47, 95% CI: −0.76, −0.18). A negative indirect pathway through self-efficacy for weight control was present (Figure 3A: αb = −0.05, 95% CI: −0.11, −0.01) and the direct association between genetic beliefs and fruit and vegetable intake remained negative and significant when controlling for self-efficacy for weight control (Figure 3A: c’ = −0.42, 95% CI: −0.69, −0.19). These relationships were not present in obese women; genetic causal beliefs were not associated with either fruit and vegetable intake or self-efficacy for weight control (Figure 3B).
Figure 3.
Associations between genetic causal beliefs, self-efficacy for weight control, and daily fruit and vegetable intake by obesity status.
A. N=286 non-obese women
B. N=195 obese women
Notes: These analyses are adjusted for education. Estimates are bolded when confidence interval excludes zero.
aBias-corrected confidence interval generated via bootstrapping.
Genetic causal beliefs and physical activity
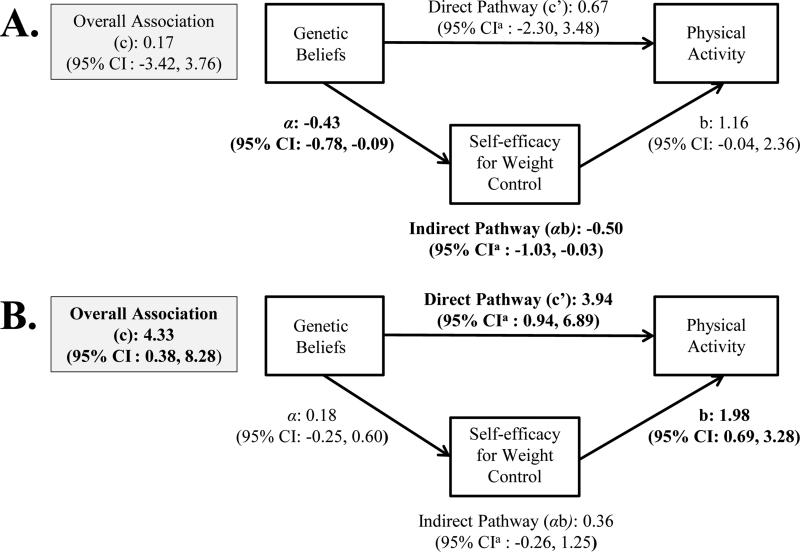
Figure 4 summarizes the results for the regression analyses considering genetic causal beliefs and weekly leisure-time physical activity, adjusted for education, by obesity status. In non-obese women, genetic causal beliefs were not associated with physical activity, though a negative indirect pathway through self-efficacy for weight control was present in this model (Figure 4A: αb = −0.05, 95% CI: −1.03, −0.03). In contrast, genetic causal beliefs were positively associated with weekly leisure-time physical activity in obese women (Figure 4B: c = 4.33, 95% CI: 0.38, 8.28). This association remained positive and significant when adjusting for self-efficacy for weight control (Figure 4B: c’ = 3.94, 95% CI: 0.94, 6.89).
Figure 4.
Associations between genetic causal beliefs, self-efficacy for weight control, and weekly leisure-time physical activity by obesity status.
C. N=283 non-obese women
D. N=187 obese women
Notes: These analyses are adjusted for education. Estimates are bolded when confidence interval excludes zero.
aBias-corrected confidence interval generated via bootstrapping.
Sensitivity analyses
Adjusting for competing obesity causal beliefs had little influence on our results. Assessing hypotheses (1) and (2) among individuals with comparable genetic causal attributions and hypothesis (3) among those with comparable diet and physical activity causal attributions gave slightly different estimates, but the results of the regression analyses were qualitatively unchanged.
Discussion
The goal of this study was to clarify relationships between obesity casual attributions and diet and physical activity behaviour while exploring self-efficacy for weight control as a potential explanatory mechanism. We hypothesized that behavioural causal beliefs would be associated with increased performance of obesity risk-reducing behaviours, driven by positive associations between beliefs and self-efficacy for weight control (hypotheses 1 & 2), while genetic causal beliefs would be associated with decreased performance, driven by inverse associations between genetic causal beliefs and self-efficacy for weight control (hypothesis 3). Multi-level regression methods were used to test these hypotheses in a cohort of middle-aged Non-Hispanic White women.
Our hypotheses about diet and physical activity causal beliefs and obesity-related behaviours were mostly supported. Diet causal beliefs and fruit and vegetable intake were positively related, as predicted in hypothesis 1. Self-efficacy for weight control accounted for approximately 14.3% of the association between these variables (Figure 2A). Physical activity causal beliefs were not associated with weekly leisure-time physical activity as predicted in hypothesis 2. But, an indirect pathway through self-efficacy for weight control was still present in this model (Figure 2B), illustrating that indirect effects may still be present without a significant overall association due to small effect sizes or the presence of multiple mediators with competing effects (Shrout & Bolger, 2002). In addition to suggesting a mediating role for self-efficacy for weight control, these results highlight the importance of measuring and analyzing behavioural causal beliefs independently. The HINTS survey, which is the primary source of representative data on causal beliefs for multifactorial conditions in the United States (US), most recently measured behavioural attributions with a single question (Waters, Muff, & Hamilton, 2014, pg. 2), limiting this resource's usefulness.
Our findings related to hypothesis 3 were less straightforward, as the regression results differed by BMI. Genetic causal beliefs were inversely associated with fruit and vegetable intake in non-obese women and self-efficacy for weight control accounted for approximately 10.6% of the negative association between these variables (Figure 3A), as hypothesized. But, genetic beliefs and fruit and vegetable intake were unrelated in obese women (Figure 3B). Also contradicting hypothesis 3, genetic causal attributions and weekly leisure-time physical activity were not associated in non-obese women (Figure 4A) and were positively associated in obese women (Figure 4B). But, a significant indirect pathway linking genetic causal attributions and leisure-time physical activity was found in the non-obese women (Figure 4 A), supporting a possible mediating role for self-efficacy for weight control in this subgroup.
Overall, our results help to clarify some aspects of the literature on obesity causal attributions and preventive health behaviour and provide directions for future research. First, it appears that relationships between genetic causal beliefs, self-efficacy for weight control, and obesity-related behaviour may differ by body mass index—at least in middle-aged women. These results help explain previous conflicting findings about self-efficacy's role linking genetic causal beliefs and self-regulation behaviours in clinical samples (e.g. Hilbert et al. 2009) versus the general population (e.g. Wang & Coups, 2010). Despite the fact that obese individuals are more likely to endorse genetic causes of obesity, it does not appear that these beliefs lead to lower self-efficacy for weight control in the same way that they do in the non-obese. Discerning why this may be deserves considerable attention in future research. It should be noted that inverse associations between genetic causal beliefs and obesity-related behaviours did not differ significantly by BMI in the 2007 HINTS data (Wang & Coups, 2010). It is possible that BMI's moderating effects may be more pronounced in women, who are more likely to attribute obesity to genetics and are also more likely to suffer psychologically from obesity, and engage in weight control efforts than men (Hilbert et al., 2009; White, O'Neil, Kolotkin, & Byrne, 2004).
Second, additional theoretical and longitudinal work is needed to clarify and unify conceptual models of how obesity causal beliefs affect obesity-related behaviours. Our results indicate that there are other mechanisms linking obesity causal attributions and self-regulation behaviours in addition to self-efficacy for weight control, some with completing negative and positive effects. Complete mediation by self-efficacy for weight control—a scenario where a signal factor accounts for the association between the predictor and the outcome—would be unlikely given the complex determinants of these behaviours. More accurate conceptual models will be important for guiding future longitudinal mediation analyses using statistical techniques that allow for moderated-mediation, mediated-moderation, and feedback loops between variables (Borsboom & Cramer, 2013; Hayes, 2013). To inform covariate selection for formal mediation analyses the internal and external determinants of obesity causal beliefs also need to be better understood. The proportion of respondents reporting strong genetic causal beliefs was 9% in our sample compared to 19% in the 2007 HINTS data (Wang & Coups, 2010) and 38% in a sample of community health center patrons in Suffolk County, New York (Ashida et al., 2011). Some of this variation could be due to item wording, e.g. asking about genes versus inheritance, but could also be a function of demographic factors that are also strongly predictive of health behaviour.
Finally, the relationship between obesity causal beliefs and self-efficacy remains unclear, in part due to the inconsistent ways in which genetic fatalism and determinism have been discussed and operationalized in the literature. Much of the social and behavioural literature has focused on the relationship between genetic risk feedback and perceived control over disease risk, with the limited evidence suggesting that it has little impact (Collins, Wright, & Marteau, 2011). Though the difference is nuanced, perceived control over risk of obesity is not the same as self-efficacy for weight control, which specifically refers to an individuals’ assessment of their ability to successfully control their weight—in our case over the next year. Inconsistent use of these constructs in the literature has led to confusion about how genetic determinism is cognitively manifested and how to best measure it and its downstream consequences. Qualitative work could be used to explore whether lowered self-efficacy is a more potent byproduct of genetic determinism than decreased personal control and if genetic causal beliefs are an indicator of genetic determinism. Our results suggest that this is a useful line of research to pursue and that the results could be informative for understanding how to apply existing self-efficacy theory to genetic and genomic health promotion interventions.
Strengths and limitations
This study's primary strength is that it expanded on prior research by identifying and testing self-efficacy for weight control as a possible mechanism accounting for previously observed relationships between obesity causal beliefs and risk-reducing behaviours, while providing an opportunity to replicate these associations in a second sample. The results add to the limited literature on associations between causal beliefs about obesity, related cognitions, and current diet and exercise behaviours in the general population and provide important groundwork for future longitudinal mediation analyses using the full SESO cohort. The study also has a number of limitations that are important to note. First, the sample has limited diversity with respect to age, gender, and racial/ethnic identity and was conducted in a single county within Washington State. This limits the generalizability of our results to subpopulations that may (or may not) have different beliefs about the causes of obesity, including those who live outside this region and outside of the US. Extending our findings to the Hispanic women who participated in SESO is an important next step. Second, these analyses were cross-sectional, which does not allow us to definitively verify the assumptions of temporal and causal ordering of the predictor, mediator, and outcome made in causal mediation analysis (MacKinnon, 2007). Asking about current causal beliefs and behaviours, but having participants to gauge their confidence in their ability to control their weight during the next year, in particular, could have influenced our findings and makes it difficult to fully understand self-efficacy's possible mediating role. Thus, our results should be interpreted with caution and considered descriptive and not implying causal effects. Feedback loops between behaviours and cognitions are possible and were not accounted for in our analyses, potentially biasing our estimates (Brewer, Weinstein, Cuite, & Harrington, 2004). Future longitudinal studies are critical to substantiating associations between obesity attributions, self-efficacy for weight control, and health behaviour. Finally, we used single item measures of obesity causal beliefs, self-efficacy for weight control, and fruit and vegetable intake, which shortened the length of our survey instruments, but brought the limitation of incalculable alphas.
Conclusions
The results of this study provide initial evidence that inverse associations between genetic attributions and diet and physical activity behaviour may be partially due to lowered confidence in ability to control one's weight, particularly in non-obese women. Our findings should be contextualized in light of the mounting evidence that despite substantial excitement, DNA-based risk estimates appear to have little to no effect on future behaviour (Marteau et al., 2010). It will be important to understand how causal beliefs developed over the lifespan are different than short-term attributions—for example, causal beliefs after receiving a real or hypothetical genetic test result—and the implications for research and practice. In addition to perceived control over risk, self-efficacy is a distinct and important construct to consider when studying genetic causal belief and behavioural self-regulation. Obesity prevention and control efforts should consider how portraying the underlying causes of obesity may influence individuals’ perceptions of their ability to successfully control their weight and pilot test messages about genetic, behavioural, and environmental risk factors in obese and non-obese individuals to avoid unintended effects.
Footnotes
Disclosures: The authors have no conflicts of interest to disclose.
References
- The American Association for Public Opinion Research . Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 5th edition AAPOR; Lenexa, Kansas: 2008. [Google Scholar]
- Allan JD. Explanatory models of overweight among African American, Euro-American, and Mexican American women. Western Journal of Nursing Research. 1998;20:45–66. doi: 10.1177/019394599802000104. [DOI] [PubMed] [Google Scholar]
- Ashida S, Goodman M, Pandya C, Koehly LM, Lachanc C, Stafford J, Kaphingst KA. Age differences in genetic knowledge, health literacy, and causal beliefs for health conditions. Public Health Genomics. 2011;14:307–316. doi: 10.1159/000316234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioural change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action. Prentice-Hall; New York: 1986. [Google Scholar]
- Beresford SAA, Thompson B, Feng Z, Christianson A, McLerran D, Patrick D. Seattle 5 a Day worksite program to increase fruit and vegetable consumption. Preventive Medicine. 2001;32:230–238. doi: 10.1006/pmed.2000.0806. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Weinstein ND, Cuite CL, Herrington JE. Risk perceptions and their relation to risk behaviour. Annals of Behavioural Medicine. 2004;27:125–130. doi: 10.1207/s15324796abm2702_7. [DOI] [PubMed] [Google Scholar]
- Cantor D, Coa K, Crystal-Mansour S, Davis T, Dipko S, Sigman R. Health Information National Trends Study (HINTS) 2007: Final report. 2009 Retrieved from http://hints.cancer.gov/docs/HINTS2007FinalReport.pdf.
- Carlsten C, Burke W. Potential for genetics to promote public health: Genetics research on smoking suggests caution about expectations. JAMA. 2006;269:2480–2482. doi: 10.1001/jama.296.20.2480. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CG. The Health Belief Model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behaviour and health education: theory, research, and practice. 4th ed. Jossey-Bass; San Francisco, CA: 2008. pp. 45–62. [Google Scholar]
- Collins RE, Wright AJ, Marteau TM. Impact of communicating personalized genetic risk information on perceived control over the risk: A systematic review. Genetics in Medicine. 2011;13:273–277. doi: 10.1097/GIM.0b013e3181f710ca. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Floyd D, Prentice-Dunn S. A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology. 2000;30:407–429. [Google Scholar]
- Frazier CRM, Mason P, Zhuang X, Beeler JA. Sucrose exposure in early life alters adult motivation and weight gain. PLoS ONE. 2008;3:e3221. doi: 10.1371/journal.pone.0003221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frosch DL, Mello P, Lerman C. Behavioural consequences of testing for obesity risk. Cancer Epidemiology, Biomarkers & Prevention. 2005;14:1485–1489. doi: 10.1158/1055-9965.EPI-04-0913. [DOI] [PubMed] [Google Scholar]
- Godin G. The Godin-Shephard leisure-time physical activity questionnaire. Health and Fitness Journal of Canada. 2011;4:18–22. [Google Scholar]
- Godin G, Shephard RJ. A simple method to assess exercise behaviour in the community. Canadian Journal of Applied Sports Science. 1985;10:141–146. [PubMed] [Google Scholar]
- Grembowski D, Patrick D, Diehr P, Durham M, Beresford S, Kay E, Hecht J. Self-efficacy and health behaviour among older adults. Journal of Health and Social Behaviour. 1993;34:89–104. [PubMed] [Google Scholar]
- Harvey-Berino J, Gold EC, West DS, Shuldiner RA, Walston J, Starling RD, Poehlman ET. Does genetic testing for obesity influence confidence in the ability to lose weight? A pilot investigation. Journal of the American Dietetic Association. 2001;101:1351–1353. doi: 10.1016/S0002-8223(01)00323-6. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. The Guilford Press; New York: 2013. [Google Scholar]
- Henrikson NB, Bowen D, Burke W. Does genomic risk information motivate people to change their behaviour? Genome Medicine. 2009;1:1–3. doi: 10.1186/gm37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Dierk J, Conradt M, Schlumberger P, Hinney A, Hebebrand J, Rief W. Causal attributions of obese men and women in genetic testing: Implications of genetic/biological attributions. Psychology and Health. 2009;24:749–761. doi: 10.1080/08870440801947787. [DOI] [PubMed] [Google Scholar]
- Hofker M, Wijmenga C. A supersized list of obesity genes. Nature Genetics. 2009;41:139–140. doi: 10.1038/ng0209-139. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioural Research. 2001;36:249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Erlbaum; Mahwah: 2007. [Google Scholar]
- Mackinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behavioural Research. 1995;30:41. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddux JE, Rogers RW. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. Journal of Experimental Social Psychology. 1983;19:469–479. [Google Scholar]
- Marteau TM, French DP, Griffin SJ, Prevost AT, Sutton S, Watkinson C, Attwood S, Hollands GF. Effects of communicating DNA-based disease risk estimates on risk-reducing behaviours. Cochrane Database of Systematic Reviews. 2010;10:1–27. doi: 10.1002/14651858.CD007275.pub2. [DOI] [PubMed] [Google Scholar]
- National Heart Lung and Blood Institute . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults, NIH Publication No. 98-4083. National Institutes of Health; Bethesda: 1998. [Google Scholar]
- New C, Xiao L, Ma J. Acculturation and overweight-related attitudes and behaviour among obese Hispanic adults in the United States. Obesity. 2013;21:2396–2404. doi: 10.1002/oby.20146. [DOI] [PubMed] [Google Scholar]
- Olander EK, Fletcher H, Williams S, Atkinson L, Turner A, French DP. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: a systematic review. International Journal of Behavioural Nutrition and Physical Activity. 2013;10(29):1–11. doi: 10.1186/1479-5868-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neil SC, McBride CM, Alford SH, Kaphingst KA. Preferences for genetic and behavioural health information: the impact of risk factors and disease attributions. Annals of Behavioural Medicine. 2010;40:127–137. doi: 10.1007/s12160-010-9197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Sanderson SC, Koehly LM. Online communication about genetics and body weight: implications for health behaviour and internet-based education. Journal of Health Communication. 2013;18:241–249. doi: 10.1080/10810730.2012.727951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes A. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behaviour Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Sanderson SC, Persky S, Michie S. Psychological and behavioural responses to genetic test results indicating increased risk of obesity: Does the causal pathway from gene to obesity matter? Public Health Genomics. 2009;13:34–47. doi: 10.1159/000217794. [DOI] [PubMed] [Google Scholar]
- Sastry N, Ghosh-Dastidar B, Adams J, Pebley AT. The design of a multilevel survey of children, families, and communities: the Los Angeles Family and Neighborhood Survey. Social Science Research. 2006;35:1000–1024. [Google Scholar]
- Shields CA, Brawley LR, Lindover TI. Self-efficacy as a mediator of the relationship between causal attributions and exercise behaviour. Journal of Applied Social Psychology. 2006;36:2785–2802. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 12. StataCorp LP.; College Station, TX: 2011. [Google Scholar]
- Wamsteker EW, Geenen R, Iestra J, Larsen JK, Zelissen PMJ, van Staveren WA. Obesity-related beliefs predict weight loss after an 8-week low-calorie diet. Journal of the American Dietetic Association. 2005;105:441–444. doi: 10.1016/j.jada.2004.12.031. [DOI] [PubMed] [Google Scholar]
- Wang C, Coups EJ. Causal beliefs about obesity and associated health behaviours: Results from a population-based survey. International Journal of Behavioural Nutrition and Physical Activity. 2010;7:19. doi: 10.1186/1479-5868-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters EA, Muff J, Hamilton JG. Multifactorial beliefs about the role of genetics and behaviour in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviours. Genetics in Medicine. 2014 doi: 10.1038/gim.2014.49. Advance online publication. doi: 10.1038/gim.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White MA, O'Neil PM, Kolotkin RL, Byrne TK. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obesity Research. 2004;12:949–955. doi: 10.1038/oby.2004.116. [DOI] [PubMed] [Google Scholar]
- Willyard C. The family roots of obesity. Nature. 2014;508:S58–S60. doi: 10.1038/508S58a. [DOI] [PubMed] [Google Scholar]
- Witte K. Fear control and danger control: a test of the Extended Parallel Process Model (EPPM). Communication Monographs. 1994;61:113–134. [Google Scholar]