Abstract
Up to 10% of acute colonic diverticulitis may necessitate a surgical intervention. Although associated with high morbidity and mortality rates, Hartmann’s procedure (HP) has been considered for many years to be the gold standard for the treatment of generalized peritonitis. To reduce the burden of surgery in these situations and as driven by the accumulated experience in colorectal and minimally-invasive surgery, laparoscopy has been increasingly adopted in the management of abdominal emergencies. Multiple case series and retrospective comparative studies confirmed that with experienced hands, the laparoscopic approach provided better outcomes than the open surgery. This technique applies to all interventions related to complicated diverticular disease, such as HP, sigmoid resection with primary anastomosis (RPA) and reversal of HP. The laparoscopic approach also provided new therapeutic possibilities with the emergence of the laparoscopic lavage drainage (LLD), particularly interesting in the context of purulent peritonitis of diverticular origin. At this stage, however, most of our knowledge in these fields relies on studies of low-level evidence. More than ever, well-built large randomized controlled trials are necessary to answer present interrogations such as the exact place of LLD or the most appropriate sigmoid resection procedure (laparoscopic HP or RPA), as well as to confirm the advantages of laparoscopy in chronic complications of diverticulitis or HP reversal.
Keywords: Diverticulitis, Laparoscopy, Emergent, Lavage, Drainage, Peritonitis, Purulent, Stercoral, Complicated, Perforation
Core tip: With the aim to improve surgery outcomes, laparoscopy has been increasingly performed in complicated diverticulitis. Despite the absence of solid proofs and under the condition of large expertise, it is an appropriate approach for the surgical management of both elective and emergent situations related to complicated diverticulitis. Moreover, the laparoscopic lavage drainage represents a previously unknown modality of treatment of purulent peritonitis. Validation of these data by large-scale randomized controlled trials is mandatory to build future therapeutic algorithms on which general surgeons can rely in their daily practice.
INTRODUCTION
Colonic diverticulosis is mainly an acquired disease with an age-dependent prevalence, ranging from 5% at 30 years to 60% at 80 years[1]. Acute diverticulitis occurs in 4%-25% of cases[2,3] of which 8%-35% present with perforated disease[4]. Generalized peritonitis from colonic diverticulitis (graded as Hinchey 3 and 4[5]) is a life-threatening situation requiring immediate surgical intervention[2,6,7]. Designated by Hartmann’s procedure (HP), resection of the affected diverticular colon segment, closure of the rectal stump and formation of an end colostomy has been considered the treatment of choice for many years[8-13]. However, morbidity and mortality rates of 24% and 19% as well as high risk of permanent stoma[14-18] have pushed general surgeons to look for surgical alternatives with better outcomes.
In colorectal surgery, large-scale prospective studies have confirmed the superiority of laparoscopy over the open approach in terms of lowered postoperative morbidities, reduced postoperative pain, improved respiratory function and shortened hospital stay[19-22]. Based on that, laparoscopy has been considered as the preferred approach for the elective treatment of diverticular disease[1,23,24]. In 2006, however, the European Association of Endoscopic Surgeons[25] and the American Society of Colon and Rectal Surgeons[23] expressed their opposition to the routine usage of laparoscopy in the acute setting. Due to insufficient data confirming validity of the presumed advantages in emergent surgery, the laparoscopic approach was estimated not to be appropriate for the management of complicated perforated diverticulitis.
Since then, worldwide increasing experience in colorectal and minimally invasive surgery has broadened applicability of laparoscopy to abdominal emergencies, hypothesizing that the advantages observed in the elective setting can be translatable to acute situations[26]. Several recent studies claim the benefits of laparoscopy over the open approach when performed by experienced surgeons in selected patients with perforated diverticulitis[25,27-31].
Virtually all procedures for complicated diverticular disease have been achieved under laparoscopy. Since its first description almost twenty years ago[32], the laparoscopic reversal of HP has been progressively performed promising reduced morbidity and mortality[33,34]. Similarly, sigmoid resection and primary anastomosis (RPA) with or without derivating loop ileostomy (DI) has been repeatedly performed in diverticular peritonitis[35]. Furthermore, during the last ten years, we have been observing the emergence of the laparoscopic lavage drainage (LLD), a previously unknown technique for the management of purulent peritonitis[36,37].
In parallel, laparoscopy is being increasingly performed for elective surgeries related to complicated diverticulitis. The most common examples are the reversal of HP and the sigmoidectomy for chronic complications (such as fistula, inflammatory stenosis and phlegmon).
Nonetheless, despite worldwide application, laparoscopic surgery for complicated diverticulitis mostly relies on empirical experience. A precise consensus based on level 1 evidenced data has not yet been established to determine the exact status of laparoscopic techniques in this field.
This review aims to provide a critical appraisal of currently available data concerning the laparoscopic approach in both emergent and elective settings of complicated diverticulitis. We will focus on ongoing randomized controlled studies (RCTs) that are expected to provide clear practical recommendations for emerging techniques. Perspectives for future research will also be suggested to assist tomorrow’s surgeons in their decision making when addressing these situations.
LITERATURE RESEARCH
A bibliographic search was performed in PubMed and Cochrane library for case series and comparative studies published from January 1995 to July 2015. RCTs were recorded from the official web site www.clinicaltrial.gov. The following medical subject heading (MeSH) terms were searched for titles and abstracts in the English or French languages: Diverticulitis; acute; emergent; laparoscopy; lavage; drainage; peritonitis; purulent; stercoral; fecal; complicated; perforation; Hinchey; Hartmann. The “related articles” function was used to enlarge the search. A manual search of the reference lists was also performed to identify additional relevant studies. The first two authors separately classified the selected articles into elective, emergent and future situations. Subsequently, relevant articles were discussed and discrepancies of findings were resolved with agreement of both authors. Overlapping publications were identified and only the most recent paper was selected for the review.
DISCUSSION
Emergent surgery
Laparoscopic surgery for failed medical treatment: Diverticulitis complicated by pericolic and/or pelvis abscess (Hinchey 1 and 2) are most often managed conservatively with intravenous antibiotics more or less combined to percutaneous drainage[1,38,39]. In case of failure, an emergent surgery may be indicated for sepsis control and resection of the diseased colon. Available data are, however, limited to a single-institutional retrospective series[40] which has been recently updated[41]. When comparing outcomes of the laparoscopic approach (24 patients) to those of laparotomy (18 patients), laparoscopy was associated with a 4-fold decrease in overall complication rate, faster bowel movement, shorter hospital stay and comparable rate of RPA despite a longer operative time. In the laproscopy group, RPA could be achieved in all but one patient and conversion to open surgery occurred in 2 patients. In regard to these encouraging results and motivated by the scarcity of data on this specific aspect of colonic diverticular surgery, RCTs are needed to confirm the suggested benefits of laparoscopy in this group of patients.
LLD: First described in 1996[42,43], the procedure consists of a laparoscopic exploration of the abdominal cavity followed by lavage with heated saline serum and drainage of the diseased colon for the next several days. The need for extensive adhesiolysis in search of the colonic perforation remains controversial[44]. In a prospective multi-institutional study[45], 92 patients underwent laparoscopic peritoneal lavage for Hinchey 2 or 3 diverticulitis. All patients but two had complete clinical resolution. One patient required subsequent colonic resection whereas the other required percutaneous drainage for pelvic abscess. Mortality and morbidity rates were 3% and 4%, respectively. After a median follow-up period of 36 mo, only two patients were readmitted with acute diverticulitis successfully treated with antibiotics. The authors concluded that LLD can be a reasonable alternative to HP for Hinchey 3 perforated diverticulitis. Another prospective study[46] found that LLD offers the advantages of shorter operative time and hospital stay, reduced estimated blood loss and better postoperative outcomes compared with laparoscopic HP. Including all stages of complicated diverticulitis (mainly Hinchey 3), only 2.1% of patients undergoing LLD were converted to open HP, and 6.4% were reoperated for uncontrolled sepsis. Almost half of the patients who received LLD underwent subsequent sigmoid resection, but the reasons were not mentioned. Such favorable results (low morbidity and mortality rates, high chance of sepsis control, avoidance of stoma and bowel salvage) have been constantly reported in case series and systematic reviews[37,44,47-53]. Soon after and despite robust evidence, LLD was cited in national and international scientific committees’ reports as a potential therapeutic option for purulent peritonitis of diverticular origin[1,54,55].
Preliminary results of the DILALA prospective randomized trial have been recently published after complete accrual[56]. Although the primary endpoint (the number of reinterventions) could not be assessed because of incomplete follow-up, this trial showed a higher than usual mortality rate of 7.7% after LLD. This result was comparable to that found in the open HP group. Both procedures provided comparable complication profiles, but LLD resulted in shorter operative time, shorter time in the recovery unit and shorter hospital stay. Recently, the enthusiasm toward LLD has been hindered by the results of the LOLA group within the Ladies trial confronting LLD to sigmoidectomy in Hinchey 3 diverticulitis[57]. This multicenter RCT has been prematurely terminated because of significantly increased in-hospital major morbidity or mortality in the lavage group compared with sigmoidectomy. Surgical reinterventions accounted for most of these adverse events. However, mortality rate was unaltered (9% in the LLD group vs 14% in the sigmoidectomy group), and sepsis was successfully controlled in 76% of cases (vs 90% in the sigmoidectomy group). In the long-term, there was no difference in the incidence of major morbidity or death between the two groups (37% vs 40% in the LLD and sigmoidectomy groups, respectively). LLD allowed salvage of the sigmoid in almost half of the cases and avoided stoma formation in three-quarters of the patients. In contrast to the resection procedure, LLD allows bowel salvage and avoids stoma but requires a multi-step careful surveillance and timely management. The authors conclude that peritoneal lavage cannot be favored over sigmoid resection as a routine intervention for purulent peritonitis of diverticular origin. Instead, it may be an alternative approach to sigmoidectomy with similar length of stay and long-term outcome in select patients. From this standpoint, in the Dutch Collaborative study group[58] as well as in another study[59], age older than 80 years, American Society of Anesthesiologists grade 3 or above, multiple comorbidities, immunosuppression, high C reactive protein and/or high Mannheim peritonitis index were associated with increased risk of failure after LDD. Currently, there are two ongoing RCTs comparing LLD to sigmoidectomy[60,61]. The results are eagerly awaited to provide further evidence about expected outcomes after LLD and to identify criteria for patients who would preferably benefit from each technique.
In contrast to the enthusiasm for LLD in purulent peritonitis, this approach is not commonly admitted for Hinchey 4 diverticulitis. The presence of a visible perforation in the colon has always represented the limit of application of the technique[42,62]. In his prospective study, Myers et al[45] stated that stercoral peritonitis constitutes an indication for conversion to open HP. Conversely, Liang et al[46] reported very encouraging results despite the inclusion of more than 10% of Hinchey 4 peritonitis in his prospective study. Many authors agree that LLD cannot be accepted unless perforation of the colon is formally ruled out[45,53]. Conversely, others propose suturing the colonic hole if stercoral peritonitis is not evident[59]. The diagnosis of stercoral peritonitis on explorative laparoscopy excluded patients from both of the available randomized controlled trials[56,57]. This condition is presumed to significantly modify the results observed with purulent peritonitis. In fact, the high reintervention rate found in the Ladies trial is mostly attributed to the misdiagnosis of stercoral peritonitis. To optimize outcomes after peritoneal lavage, the authors pushed toward a meticulous search for colon perforation. In all cases, the adoption of LLD in emergency settings, abdominal exploration for generalized peritonitis, pelvic dissection in inflammatory conditions and possible suture of a diseased colon require that the surgeon have a minimum of colorectal and minimally invasive skills before he can propose this conservative approach[51,58].
Sigmoidectomy: Primary anastomosis and HP: Supported by considerable improvement in the perioperative care, RPA (without or without DI) has been proposed as an alternative to HP in emergent situations. A comparison of these two techniques has mostly enrolled patients undergoing open procedures before the widespread application of laparoscopy in emergent colorectal surgery. In fact, several comparative studies, systematic reviews and meta-analyses favored RPA over HP in respect to reduced mortality and morbidity rates, shorter cumulative operative time and hospital stay, more frequent stoma reversal and reduced cost[63-76]. Even without DI, RPA was shown to be preferable than HP for purulent peritonitis[70,72,77]. These studies, however, suffer from marked heterogeneity and selection bias with low-risk patients mainly undergoing RPA, whereas HP is offered to high-risk elderly patients[63,74]. A recent RCT showed that for Hinchey 3 and 4 diverticular disease, the main differences between RPA with DI and HP occur during the stage of stoma reversal[78]. When both stages (colonic resection and stoma reversal) were combined, the rates of overall complications, severe complications and mortality (13% in HP vs 9% in PA) were similar in both groups. In contrast, when the reversal procedure was considered alone, HP was associated with lower stoma reversal rate (58% vs 90%), more frequent severe complications (20% vs 0%), and longer operative time and hospital stay. The main flaw of this RCT would be the lack of information about the adopted approach (laparoscopic or open) for the reversal of the stoma. This issue is of paramount importance because laparoscopy has been proved to decrease the morbidity of HP reversal in several case series and systematic reviews[79-86]. The elevated rate of severe complications during stoma closure in the HP group may have been overemphasized by the open approach per se.
This evidence raises the question whether the laparoscopic HP may offer advantages over the open approach in terms of reduced morbidity and mortality in the acute setting of perforated diverticulitis. To improve the outcome after open HP, we have been among the first to show the feasibility of a laparoscopic two-staged strategy for complicated diverticular disease. Despite conversion in 19% of cases, this approach offered adequate control of sepsis with low rates of mortality (3%) and morbidity (23%)[33]. Similarly, in a small case series, Agaba et al[34] described favorable outcomes after laparoscopic HP for Hinchey 3 and 4 diverticulitis. Recently, a propensity-matched analysis of the ACS NSQIP database failed to show a decrease in postoperative morbidity and mortality when HP was performed under laparoscopy compared with the open approach. This study, however, suffers from substantial imperfections in methodology such as retrospective data acquisition and lack of analysis of pertinent variables that might substantially interfere with the results[26].
To clarify the role of laparoscopy in emergent sigmoidectomy, Mbadiwe et al[87] retrospectively analyzed the ACS NSQIP database. In a total of 11981 patients, a bivariate analysis showed that patients undergoing laparoscopy experienced lower rates of complications with both RPA (14% vs 26%, P < 0.001) and HP (30% vs 37%, P = 0.02). The laparoscopic approach was associated with decreased mortality rate for patients undergoing RPA (0.24% vs 0.79%, P < 0.001). The reduced complication rate after laparoscopic RPA was confirmed in the multivariate analysis[87].
To provide a high level of evidence in the present era of widespread use of laparoscopy for colorectal disease, a well-built RCT is highly desirable comparing laparoscopic RPA (with or without DI) with a two-step laparoscopic HP (sigmoid resection and stoma closure) in perforated complicated diverticulitis. Not only outcomes of both procedures will be clarified but also identification of precise criteria would define the subgroups of patients who will benefit more from each technique. Based on this perspective, the results of the ongoing DIVA section of the Ladies trial are keenly awaited to provide us with level 1 evidence about the preferable laparoscopic attitude in Hinchey 4 complicated diverticulitis[57].
Elective surgery
Based on solid proofs from a large-scale meta-analysis[88] and RCTs[89,90], international committees have adopted laparoscopy as the preferred approach for elective sigmoidectomy after acute diverticulitis[1,23,24]. Compared with an open procedure, the laparoscopic modality offers a significant decrease in major complications and morbidity, less blood loss, fewer analgesic requirements, shorter hospital stay and improved quality of life.
Conversely, in early experience, laparoscopy was contraindicated for the treatment of diverticular chronic complications (stricture, fistula and persistent phlegmon) because severe inflammation and distorted anatomy exposes the patient to high risks of bleeding and adjacent organ trauma (bladder, left ureter, female genital organs)[11,91]. With increasing experience, the laparoscopic approach has been progressively accepted as an alternative to open surgery but its routine usage in chronic complications remains controversial[92].
Because presently available data mostly rely on small retrospective series and case reports, several controversies cannot be fully elucidated. In a descriptive case series, Le Moine et al[93] suggested that chronic complicated diverticulitis increases the risk of conversion to laparotomy in elective laparoscopic sigmoidectomy. This effect has been recently disproved by two comparative studies[94,95] which stated that surgeons’ expertise in minimally invasive and colorectal surgery is the principal determinant of morbidity and conversion rates in complicated cases. This evidence outlines that accumulating experience during the last ten years has inevitably challenged previously accepted knowledge.
Colonic fistula is the most reported late complications of diverticular disease, although available data is scarce and confined to retrospective case series. In recent systematic reviews[96,97], the laparoscopic approach was judged to be feasible and safe for the treatment of colovesical fistulae. However, due to a lack in methodology and/or a limited number of patients, the studies failed to show superiority of laparoscopy over the open approach. Furthermore, the conversion rate could not be determined and the predictive factors of its occurrence were not discussed[96]. This issue has been addressed in a previous case series including 31 patients conducted over 10 years. The overall conversion rate was approximately 30% but declined to 10% during the second half of the study period[98]. This finding is consistent with the statement of Abbass et al[99] that similar rates of conversion, morbidity and mortality can be expected with laparoscopy regardless of the presence of colonic fistula. Therefore, the current surgical management of colonic fistula relies on poor data derived from empirical experiences in open surgery. The most salient example is the adoption of a single-stage procedure as the preferred surgical option despite the absence of solid proofs confirming its superiority[98].
During this study, we noticed a striking lack of high quality papers dedicated to the issues of inflammatory phlegmon and stricture. Information on the most appropriate treatment in these situations is thus absent. If low incidence of such cases is the cause of this shortage, prospective enrollment of patients in large multi-institutional databases might be the solution to build precise therapeutic algorithms on which tomorrow’s general surgeons can use for the treatment of their patients.
Finally, with the emergence of LLD as a conservative modality for complicated perforated diverticulitis, controversies have arisen about the need for systematic elective sigmoidectomy after the diseased organ has been saved. In a recent systematic review[44], rehospitalization was observed in 7% of patients who underwent LLD. More than half of them presented with a new episode of diverticulitis, 21% with generalized peritonitis, 10% with colovesical fistula and 7% with undetected colon cancer. At this stage of experience, the present data lack sufficient proof to know whether LLD can be regarded as a definitive treatment or a bridge to elective laparoscopic sigmoidectomy[100]. If LLD becomes widely admitted, well-built RCTs will be necessary to answer these questions and to determine the best candidates for bowel sparing.
CONCLUSION
In conclusion, accumulated empirical experience during the last two decades shows that laparoscopy is undeniably a promising adjunct in the management of complicated colonic diverticulitis. Analysis of presently available data also highlights the urge to build large-scale prospective RCTs in order to elucidate the exact benefits of laparoscopy and to define patients who are the best candidates for each approach. Like the ongoing trials NCT01019239 and NCT01047462, solid data are particularly awaited in order to clarify the exact place of LLD and to determine the most appropriate sigmoid resection procedure (laparoscopic HP or RPA) in Hinchey 3 and 4 peritonitis. The advantages provided by laparoscopy in chronic complications of diverticulitis and HP reversal also need to be confirmed. In the absence of precise recommendations, we suggest the following algorithm that may assist general surgeons in their decision-making when dealing with complicated colonic diverticulitis (Figure 1).
Figure 1.
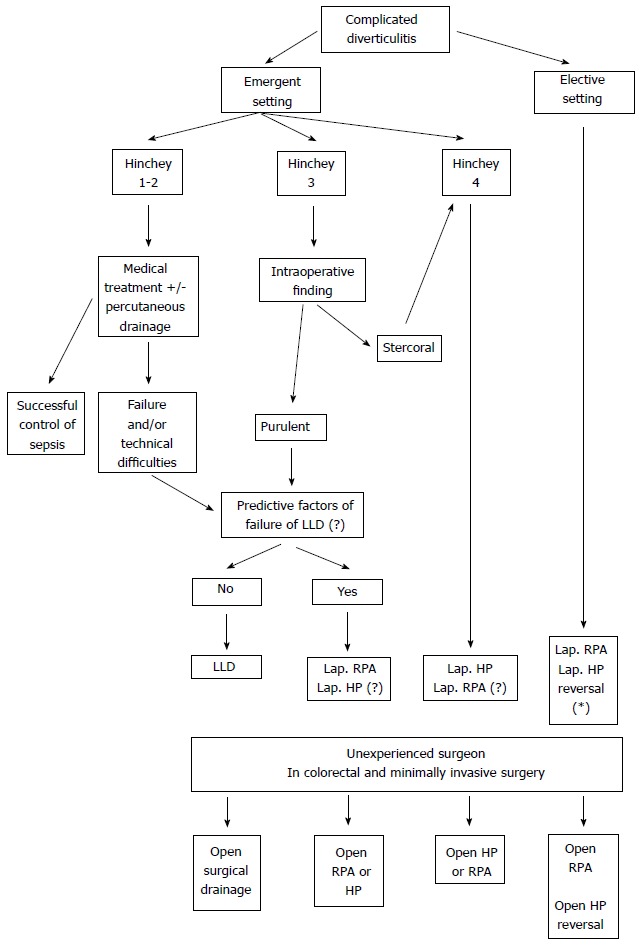
Algorithm for the laparoscopic management of complicated colonic diverticulitis. Lap: Laparoscopic; LLD: Laparoscopic lavage drainage; RPA: Resection with primary anastomosis; HP: Hartmann’s procedure; (?): Data that need to be elucidated in RCTs, (*): Data that need confirmation in RCTs.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 25, 2015
First decision: September 30, 2015
Article in press: December 8, 2015
P- Reviewer: Biondo S, Cordon JP, Lopez LM, Mutter D S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, Støvring J. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C4453. [PubMed] [Google Scholar]
- 2.Parks TG. Natural history of diverticular disease of the colon. Clin Gastroenterol. 1975;4:53–69. [PubMed] [Google Scholar]
- 3.Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R, Agarwal N, Kaneshiro M, Atia M, Sheen V, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11:1609–1613. doi: 10.1016/j.cgh.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li D, Baxter NN, McLeod RS, Moineddin R, Wilton AS, Nathens AB. Evolving practice patterns in the management of acute colonic diverticulitis: a population-based analysis. Dis Colon Rectum. 2014;57:1397–1405. doi: 10.1097/DCR.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 5.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 6.Krukowski ZH, Matheson NA. Emergency surgery for diverticular disease complicated by generalized and faecal peritonitis: a review. Br J Surg. 1984;71:921–927. doi: 10.1002/bjs.1800711202. [DOI] [PubMed] [Google Scholar]
- 7.Berry AR, Turner WH, Mortensen NJ, Kettlewell MG. Emergency surgery for complicated diverticular disease. A five-year experience. Dis Colon Rectum. 1989;32:849–854. doi: 10.1007/BF02554554. [DOI] [PubMed] [Google Scholar]
- 8.Salem L, Anaya DA, Flum DR. Temporal changes in the management of diverticulitis. J Surg Res. 2005;124:318–323. doi: 10.1016/j.jss.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Kronborg O. Treatment of perforated sigmoid diverticulitis: a prospective randomized trial. Br J Surg. 1993;80:505–507. doi: 10.1002/bjs.1800800434. [DOI] [PubMed] [Google Scholar]
- 10.Khan AL, Ah-See AK, Crofts TJ, Heys SD, Eremin O. Surgical management of the septic complications of diverticular disease. Ann R Coll Surg Engl. 1995;77:16–20. [PMC free article] [PubMed] [Google Scholar]
- 11.Köhler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13:430–436. doi: 10.1007/s004649901007. [DOI] [PubMed] [Google Scholar]
- 12.Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110–3121. doi: 10.1111/j.1572-0241.1999.01501.x. [DOI] [PubMed] [Google Scholar]
- 13.Wong WD, Wexner SD, Lowry A, Vernava A, Burnstein M, Denstman F, Fazio V, Kerner B, Moore R, Oliver G, et al. Practice parameters for the treatment of sigmoid diverticulitis--supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 2000;43:290–297. doi: 10.1007/BF02258291. [DOI] [PubMed] [Google Scholar]
- 14.Salem L, Anaya DA, Roberts KE, Flum DR. Hartmann’s colectomy and reversal in diverticulitis: a population-level assessment. Dis Colon Rectum. 2005;48:988–995. doi: 10.1007/s10350-004-0871-x. [DOI] [PubMed] [Google Scholar]
- 15.Seah DW, Ibrahim S, Tay KH. Hartmann procedure: is it still relevant today? ANZ J Surg. 2005;75:436–440. doi: 10.1111/j.1445-2197.2005.03367.x. [DOI] [PubMed] [Google Scholar]
- 16.Maggard MA, Zingmond D, O’Connell JB, Ko CY. What proportion of patients with an ostomy (for diverticulitis) get reversed? Am Surg. 2004;70:928–931. [PubMed] [Google Scholar]
- 17.Chapman J, Davies M, Wolff B, Dozois E, Tessier D, Harrington J, Larson D. Complicated diverticulitis: is it time to rethink the rules? Ann Surg. 2005;242:576–581; discussion 581-583. doi: 10.1097/01.sla.0000184843.89836.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ince M, Stocchi L, Khomvilai S, Kwon DS, Hammel JP, Kiran RP. Morbidity and mortality of the Hartmann procedure for diverticular disease over 18 years in a single institution. Colorectal Dis. 2012;14:e492–e498. doi: 10.1111/j.1463-1318.2012.03004.x. [DOI] [PubMed] [Google Scholar]
- 19.Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;(3):CD003145. doi: 10.1002/14651858.CD003145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braga M, Vignali A, Gianotti L, Zuliani W, Radaelli G, Gruarin P, Dellabona P, Di Carlo V. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg. 2002;236:759–766; disscussion 767. doi: 10.1097/01.SLA.0000036269.60340.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delaney CP, Chang E, Senagore AJ, Broder M. Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg. 2008;247:819–824. doi: 10.1097/SLA.0b013e31816d950e. [DOI] [PubMed] [Google Scholar]
- 22.Forgione A, Leroy J, Cahill RA, Bailey C, Simone M, Mutter D, Marescaux J. Prospective evaluation of functional outcome after laparoscopic sigmoid colectomy. Ann Surg. 2009;249:218–224. doi: 10.1097/SLA.0b013e318195c5fc. [DOI] [PubMed] [Google Scholar]
- 23.Rafferty J, Shellito P, Hyman NH, Buie WD. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–944. doi: 10.1007/s10350-006-0578-2. [DOI] [PubMed] [Google Scholar]
- 24.Fozard JB, Armitage NC, Schofield JB, Jones OM. ACPGBI position statement on elective resection for diverticulitis. Colorectal Dis. 2011;13 Suppl 3:1–11. doi: 10.1111/j.1463-1318.2010.02531.x. [DOI] [PubMed] [Google Scholar]
- 25.Sauerland S, Agresta F, Bergamaschi R, Borzellino G, Budzynski A, Champault G, Fingerhut A, Isla A, Johansson M, Lundorff P, et al. Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2006;20:14–29. doi: 10.1007/s00464-005-0564-0. [DOI] [PubMed] [Google Scholar]
- 26.Turley RS, Barbas AS, Lidsky ME, Mantyh CR, Migaly J, Scarborough JE. Laparoscopic versus open Hartmann procedure for the emergency treatment of diverticulitis: a propensity-matched analysis. Dis Colon Rectum. 2013;56:72–82. doi: 10.1097/DCR.0b013e3182749cf5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vermeulen J, Lange JF. Treatment of perforated diverticulitis with generalized peritonitis: past, present, and future. World J Surg. 2010;34:587–593. doi: 10.1007/s00268-009-0372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stocchi L. Current indications and role of surgery in the management of sigmoid diverticulitis. World J Gastroenterol. 2010;16:804–817. doi: 10.3748/wjg.v16.i7.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stulberg JJ, Champagne BJ, Fan Z, Horan M, Obias V, Marderstein E, Reynolds H, Delaney CP. Emergency laparoscopic colectomy: does it measure up to open? Am J Surg. 2009;197:296–301. doi: 10.1016/j.amjsurg.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chand M, Siddiqui MR, Gupta A, Rasheed S, Tekkis P, Parvaiz A, Mirnezami AH, Qureshi T. Systematic review of emergent laparoscopic colorectal surgery for benign and malignant disease. World J Gastroenterol. 2014;20:16956–16963. doi: 10.3748/wjg.v20.i45.16956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaertner WB, Kwaan MR, Madoff RD, Willis D, Belzer GE, Rothenberger DA, Melton GB. The evolving role of laparoscopy in colonic diverticular disease: a systematic review. World J Surg. 2013;37:629–638. doi: 10.1007/s00268-012-1872-x. [DOI] [PubMed] [Google Scholar]
- 32.Anderson CA, Fowler DL, White S, Wintz N. Laparoscopic colostomy closure. Surg Laparosc Endosc. 1993;3:69–72. [PubMed] [Google Scholar]
- 33.Chouillard E, Maggiori L, Ata T, Jarbaoui S, Rivkine E, Benhaim L, Ghiles E, Etienne JC, Fingerhut A. Laparoscopic two-stage left colonic resection for patients with peritonitis caused by acute diverticulitis. Dis Colon Rectum. 2007;50:1157–1163. doi: 10.1007/s10350-006-0851-4. [DOI] [PubMed] [Google Scholar]
- 34.Agaba EA, Zaidi RM, Ramzy P, Aftab M, Rubach E, Gecelter G, Ravikumar TS, DeNoto G. Laparoscopic Hartmann’s procedure: a viable option for treatment of acutely perforated diverticultis. Surg Endosc. 2009;23:1483–1486. doi: 10.1007/s00464-009-0380-z. [DOI] [PubMed] [Google Scholar]
- 35.Regenbogen SE, Hardiman KM, Hendren S, Morris AM. Surgery for diverticulitis in the 21st century: a systematic review. JAMA Surg. 2014;149:292–303. doi: 10.1001/jamasurg.2013.5477. [DOI] [PubMed] [Google Scholar]
- 36.Bretagnol F, Pautrat K, Mor C, Benchellal Z, Huten N, de Calan L. Emergency laparoscopic management of perforated sigmoid diverticulitis: a promising alternative to more radical procedures. J Am Coll Surg. 2008;206:654–657. doi: 10.1016/j.jamcollsurg.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 37.Alamili M, Gögenur I, Rosenberg J. Acute complicated diverticulitis managed by laparoscopic lavage. Dis Colon Rectum. 2009;52:1345–1349. doi: 10.1007/DCR.0b013e3181a0da34. [DOI] [PubMed] [Google Scholar]
- 38.Wieghard N, Geltzeiler CB, Tsikitis VL. Trends in the surgical management of diverticulitis. Ann Gastroenterol. 2015;28:25–30. [PMC free article] [PubMed] [Google Scholar]
- 39.Moore FA, Catena F, Moore EE, Leppaniemi A, Peitzmann AB. Position paper: management of perforated sigmoid diverticulitis. World J Emerg Surg. 2013;8:55. doi: 10.1186/1749-7922-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Letarte F, Hallet J, Drolet S, Charles Grégoire R, Bouchard A, Gagné JP, Thibault C, Bouchard P. Laparoscopic emergency surgery for diverticular disease that failed medical treatment: a valuable option? Results of a retrospective comparative cohort study. Dis Colon Rectum. 2013;56:1395–1402. doi: 10.1097/DCR.0b013e3182a760b6. [DOI] [PubMed] [Google Scholar]
- 41.Letarte F, Hallet J, Drolet S, Boulanger-Gobeil C, Bouchard A, Grégoire RC, Gagné JP, Thibault C, Bouchard P. Laparoscopic versus open colonic resection for complicated diverticular disease in the emergency setting: a safe choice? A retrospective comparative cohort study. Am J Surg. 2015;209:992–998. doi: 10.1016/j.amjsurg.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 42.O’Sullivan GC, Murphy D, O’Brien MG, Ireland A. Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg. 1996;171:432–434. doi: 10.1016/S0002-9610(97)89625-0. [DOI] [PubMed] [Google Scholar]
- 43.Rizk N, Champault G. Laparoscopic treatment in two operative stages of perforated sigmoid diverticulitis: 2 cases. Ann Chir. 1996;50:283. [PubMed] [Google Scholar]
- 44.Cirocchi R, Trastulli S, Vettoretto N, Milani D, Cavaliere D, Renzi C, Adamenko O, Desiderio J, Burattini MF, Parisi A, et al. Laparoscopic peritoneal lavage: a definitive treatment for diverticular peritonitis or a “bridge” to elective laparoscopic sigmoidectomy?: a systematic review. Medicine (Baltimore) 2015;94:e334. doi: 10.1097/MD.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97–101. doi: 10.1002/bjs.6024. [DOI] [PubMed] [Google Scholar]
- 46.Liang S, Russek K, Franklin ME. Damage control strategy for the management of perforated diverticulitis with generalized peritonitis: laparoscopic lavage and drainage vs. laparoscopic Hartmann’s procedure. Surg Endosc. 2012;26:2835–2842. doi: 10.1007/s00464-012-2255-y. [DOI] [PubMed] [Google Scholar]
- 47.Toorenvliet BR, Swank H, Schoones JW, Hamming JF, Bemelman WA. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a systematic review. Colorectal Dis. 2010;12:862–867. doi: 10.1111/j.1463-1318.2009.02052.x. [DOI] [PubMed] [Google Scholar]
- 48.Rogers AC, Collins D, O’Sullivan GC, Winter DC. Laparoscopic lavage for perforated diverticulitis: a population analysis. Dis Colon Rectum. 2012;55:932–938. doi: 10.1097/DCR.0b013e31826178d0. [DOI] [PubMed] [Google Scholar]
- 49.White SI, Frenkiel B, Martin PJ. A ten-year audit of perforated sigmoid diverticulitis: highlighting the outcomes of laparoscopic lavage. Dis Colon Rectum. 2010;53:1537–1541. doi: 10.1007/DCR.0b013e3181f2ee2a. [DOI] [PubMed] [Google Scholar]
- 50.Edeiken SM, Maxwell RA, Dart BW, Mejia VA. Preliminary experience with laparoscopic peritoneal lavage for complicated diverticulitis: a new algorithm for treatment? Am Surg. 2013;79:819–825. [PubMed] [Google Scholar]
- 51.McDermott FD, Collins D, Heeney A, Winter DC. Minimally invasive and surgical management strategies tailored to the severity of acute diverticulitis. Br J Surg. 2014;101:e90–e99. doi: 10.1002/bjs.9359. [DOI] [PubMed] [Google Scholar]
- 52.Afshar S, Kurer MA. Laparoscopic peritoneal lavage for perforated sigmoid diverticulitis. Colorectal Dis. 2012;14:135–142. doi: 10.1111/j.1463-1318.2011.02606.x. [DOI] [PubMed] [Google Scholar]
- 53.Rossi GL, Mentz R, Bertone S, Ojea Quintana G, Bilbao S, Im VM, Vaccaro CA. Laparoscopic peritoneal lavage for Hinchey III diverticulitis: is it as effective as it is applicable? Dis Colon Rectum. 2014;57:1384–1390. doi: 10.1097/DCR.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 54.Agresta F, Ansaloni L, Baiocchi GL, Bergamini C, Campanile FC, Carlucci M, Cocorullo G, Corradi A, Franzato B, Lupo M, et al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2012;26:2134–2164. doi: 10.1007/s00464-012-2331-3. [DOI] [PubMed] [Google Scholar]
- 55.Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–294. doi: 10.1097/DCR.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 56.Angenete E, Thornell A, Burcharth J, Pommergaard HC, Skullman S, Bisgaard T, Jess P, Läckberg Z, Matthiessen P, Heath J, et al. Laparoscopic Lavage Is Feasible and Safe for the Treatment of Perforated Diverticulitis With Purulent Peritonitis: The First Results From the Randomized Controlled Trial DILALA. Ann Surg. 2016;263:117–122. doi: 10.1097/SLA.0000000000001061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, Belgers EH, van Geloven AA, Gerhards MF, Govaert MJ, van Grevenstein WM, et al. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet. 2015;386:1269–1277. doi: 10.1016/S0140-6736(15)61168-0. [DOI] [PubMed] [Google Scholar]
- 58.Swank HA, Mulder IM, Hoofwijk AG, Nienhuijs SW, Lange JF, Bemelman WA. Early experience with laparoscopic lavage for perforated diverticulitis. Br J Surg. 2013;100:704–710. doi: 10.1002/bjs.9063. [DOI] [PubMed] [Google Scholar]
- 59.Radé F, Bretagnol F, Auguste M, Di Guisto C, Huten N, de Calan L. Determinants of outcome following laparoscopic peritoneal lavage for perforated diverticulitis. Br J Surg. 2014;101:1602–166; discussion 1606. doi: 10.1002/bjs.9621. [DOI] [PubMed] [Google Scholar]
- 60.St Vincent’s University Hospital, Ireland LapLAND Laparoscopic Lavage for Acute Non-Faeculant Diverticulitis. In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US) Available from: https://clinicaltrials.gov/ct2/show/NCT01019239 NLM Identifier: NCT01019239.
- 61.University Hospital, Akershus Scandinavian Diverticulitis Trial (SCANDIV). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US) Available from: https://clinicaltrials.gov/ct2/show/NCT01047462 NLM Identifier: NCT01047462.
- 62.Mutter D, Bouras G, Forgione A, Vix M, Leroy J, Marescaux J. Two-stage totally minimally invasive approach for acute complicated diverticulitis. Colorectal Dis. 2006;8:501–505. doi: 10.1111/j.1463-1318.2006.01011.x. [DOI] [PubMed] [Google Scholar]
- 63.Salem L, Flum DR. Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Dis Colon Rectum. 2004;47:1953–1964. doi: 10.1007/s10350-004-0701-1. [DOI] [PubMed] [Google Scholar]
- 64.Schilling MK, Maurer CA, Kollmar O, Büchler MW. Primary vs. secondary anastomosis after sigmoid colon resection for perforated diverticulitis (Hinchey Stage III and IV): a prospective outcome and cost analysis. Dis Colon Rectum. 2001;44:699–703; discussion 703-5. doi: 10.1007/BF02234569. [DOI] [PubMed] [Google Scholar]
- 65.Gooszen AW, Gooszen HG, Veerman W, Van Dongen VM, Hermans J, Klien Kranenbarg E, Tollenaar RA. Operative treatment of acute complications of diverticular disease: primary or secondary anastomosis after sigmoid resection. Eur J Surg. 2001;167:35–39. doi: 10.1080/110241501750069792. [DOI] [PubMed] [Google Scholar]
- 66.Vermeulen J, Coene PP, Van Hout NM, van der Harst E, Gosselink MP, Mannaerts GH, Weidema WF, Lange JF. Restoration of bowel continuity after surgery for acute perforated diverticulitis: should Hartmann’s procedure be considered a one-stage procedure? Colorectal Dis. 2009;11:619–624. doi: 10.1111/j.1463-1318.2008.01667.x. [DOI] [PubMed] [Google Scholar]
- 67.Toro A, Mannino M, Reale G, Cappello G, Di Carlo I. Primary anastomosis vs Hartmann procedure in acute complicated diverticulitis. Evolution over the last twenty years. Chirurgia (Bucur) 2012;107:598–604. [PubMed] [Google Scholar]
- 68.Abbas S. Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis. 2007;22:351–357. doi: 10.1007/s00384-005-0059-4. [DOI] [PubMed] [Google Scholar]
- 69.Constantinides VA, Tekkis PP, Athanasiou T, Aziz O, Purkayastha S, Remzi FH, Fazio VW, Aydin N, Darzi A, Senapati A. Primary resection with anastomosis vs. Hartmann’s procedure in nonelective surgery for acute colonic diverticulitis: a systematic review. Dis Colon Rectum. 2006;49:966–981. doi: 10.1007/s10350-006-0547-9. [DOI] [PubMed] [Google Scholar]
- 70.Constantinides VA, Heriot A, Remzi F, Darzi A, Senapati A, Fazio VW, Tekkis PP. Operative strategies for diverticular peritonitis: a decision analysis between primary resection and anastomosis versus Hartmann’s procedures. Ann Surg. 2007;245:94–103. doi: 10.1097/01.sla.0000225357.82218.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zorcolo L, Covotta L, Carlomagno N, Bartolo DC. Safety of primary anastomosis in emergency colo-rectal surgery. Colorectal Dis. 2003;5:262–269. doi: 10.1046/j.1463-1318.2003.00432.x. [DOI] [PubMed] [Google Scholar]
- 72.Breitenstein S, Kraus A, Hahnloser D, Decurtins M, Clavien PA, Demartines N. Emergency left colon resection for acute perforation: primary anastomosis or Hartmann’s procedure? A case-matched control study. World J Surg. 2007;31:2117–2124. doi: 10.1007/s00268-007-9199-8. [DOI] [PubMed] [Google Scholar]
- 73.Alizai PH, Schulze-Hagen M, Klink CD, Ulmer F, Roeth AA, Neumann UP, Jansen M, Rosch R. Primary anastomosis with a defunctioning stoma versus Hartmann’s procedure for perforated diverticulitis--a comparison of stoma reversal rates. Int J Colorectal Dis. 2013;28:1681–1688. doi: 10.1007/s00384-013-1753-2. [DOI] [PubMed] [Google Scholar]
- 74.Cirocchi R, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Liu L. Treatment of Hinchey stage III-IV diverticulitis: a systematic review and meta-analysis. Int J Colorectal Dis. 2013;28:447–457. doi: 10.1007/s00384-012-1622-4. [DOI] [PubMed] [Google Scholar]
- 75.Binda GA, Karas JR, Serventi A, Sokmen S, Amato A, Hydo L, Bergamaschi R. Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis. 2012;14:1403–1410. doi: 10.1111/j.1463-1318.2012.03117.x. [DOI] [PubMed] [Google Scholar]
- 76.Tadlock MD, Karamanos E, Skiada D, Inaba K, Talving P, Senagore A, Demetriades D. Emergency surgery for acute diverticulitis: which operation? A National Surgical Quality Improvement Program study. J Trauma Acute Care Surg. 2013;74:1385–1391; quiz 1610. doi: 10.1097/TA.0b013e3182924a82. [DOI] [PubMed] [Google Scholar]
- 77.Regenet N, Pessaux P, Hennekinne S, Lermite E, Tuech JJ, Brehant O, Arnaud JP. Primary anastomosis after intraoperative colonic lavage vs. Hartmann’s procedure in generalized peritonitis complicating diverticular disease of the colon. Int J Colorectal Dis. 2003;18:503–507. doi: 10.1007/s00384-003-0512-1. [DOI] [PubMed] [Google Scholar]
- 78.Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger P, Buchli C, Grieder F, Gelpke H, Decurtins M, Tempia-Caliera AA, et al. A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg. 2012;256:819–826; discussion 826-827. doi: 10.1097/SLA.0b013e31827324ba. [DOI] [PubMed] [Google Scholar]
- 79.Toro A, Ardiri A, Mannino M, Politi A, Di Stefano A, Aftab Z, Abdelaal A, Arcerito MC, Cavallaro A, Cavallaro M, et al. Laparoscopic Reversal of Hartmann’s Procedure: State of the Art 20 Years after the First Reported Case. Gastroenterol Res Pract. 2014;2014:530140. doi: 10.1155/2014/530140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mazeh H, Greenstein AJ, Swedish K, Nguyen SQ, Lipskar A, Weber KJ, Chin EH, Divino CM. Laparoscopic and open reversal of Hartmann’s procedure--a comparative retrospective analysis. Surg Endosc. 2009;23:496–502. doi: 10.1007/s00464-008-0052-4. [DOI] [PubMed] [Google Scholar]
- 81.Chouillard E, Pierard T, Campbell R, Tabary N. Laparoscopically assisted Hartman’s reversal is an efficacious and efficient procedure: a case control study. Minerva Chir. 2009;64:1–8. [PubMed] [Google Scholar]
- 82.Di Carlo I, Toro A, Pannofino O, Patane E, Pulvirenti E. Laparoscopic versus open restoration of intestinal continuity after Hartmann procedure. Hepatogastroenterology. 2010;57:232–235. [PubMed] [Google Scholar]
- 83.Huynh H, Trottier DC, Soto CM, Moloo H, Poulin EC, Mamazza J, Boushey RP. Laparoscopic colostomy reversal after a Hartmann procedure: a prospective series, literature review and an argument against laparotomy as the primary approach. Can J Surg. 2011;54:133–137. doi: 10.1503/cjs.013510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leroy J, Costantino F, Cahill RA, D’Agostino J, Wu WH, Mutter D, Marescaux J. Technical aspects and outcome of a standardized full laparoscopic approach to the reversal of Hartmann’s procedure in a teaching centre. Colorectal Dis. 2011;13:1058–1065. doi: 10.1111/j.1463-1318.2010.02389.x. [DOI] [PubMed] [Google Scholar]
- 85.De’angelis N, Brunetti F, Memeo R, Batista da Costa J, Schneck AS, Carra MC, Azoulay D. Comparison between open and laparoscopic reversal of Hartmann’s procedure for diverticulitis. World J Gastrointest Surg. 2013;5:245–251. doi: 10.4240/wjgs.v5.i8.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zimmermann M, Hoffmann M, Laubert T, Meyer KF, Jungbluth T, Roblick UJ, Bruch HP, Schlöricke E. Laparoscopic versus open reversal of a Hartmann procedure: a single-center study. World J Surg. 2014;38:2145–2152. doi: 10.1007/s00268-014-2507-1. [DOI] [PubMed] [Google Scholar]
- 87.Mbadiwe T, Obirieze AC, Cornwell EE, Turner P, Fullum TM. Surgical management of complicated diverticulitis: a comparison of the laparoscopic and open approaches. J Am Coll Surg. 2013;216:782–788; discussion 788-790. doi: 10.1016/j.jamcollsurg.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 88.Siddiqui MR, Sajid MS, Qureshi S, Cheek E, Baig MK. Elective laparoscopic sigmoid resection for diverticular disease has fewer complications than conventional surgery: a meta-analysis. Am J Surg. 2010;200:144–161. doi: 10.1016/j.amjsurg.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 89.Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES, Bemelman WA, Heres P, Lacy AM, Engel AF, et al. Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg. 2009;249:39–44. doi: 10.1097/SLA.0b013e31818e416a. [DOI] [PubMed] [Google Scholar]
- 90.Gervaz P, Inan I, Perneger T, Schiffer E, Morel P. A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg. 2010;252:3–8. doi: 10.1097/SLA.0b013e3181dbb5a5. [DOI] [PubMed] [Google Scholar]
- 91.Vargas HD, Ramirez RT, Hoffman GC, Hubbard GW, Gould RJ, Wohlgemuth SD, Ruffin WK, Hatter JE, Kolm P. Defining the role of laparoscopic-assisted sigmoid colectomy for diverticulitis. Dis Colon Rectum. 2000;43:1726–1731. doi: 10.1007/BF02236858. [DOI] [PubMed] [Google Scholar]
- 92.Collins D, Winter DC. Laparoscopy in diverticular disease: Controversies. Best Pract Res Clin Gastroenterol. 2014;28:175–182. doi: 10.1016/j.bpg.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 93.Le Moine MC, Fabre JM, Vacher C, Navarro F, Picot MC, Domergue J. Factors and consequences of conversion in laparoscopic sigmoidectomy for diverticular disease. Br J Surg. 2003;90:232–236. doi: 10.1002/bjs.4035. [DOI] [PubMed] [Google Scholar]
- 94.De Magistris L, Azagra JS, Goergen M, De Blasi V, Arru L, Facy O. Laparoscopic sigmoidectomy in moderate and severe diverticulitis: analysis of short-term outcomes in a continuous series of 121 patients. Surg Endosc. 2013;27:1766–1771. doi: 10.1007/s00464-012-2676-7. [DOI] [PubMed] [Google Scholar]
- 95.Pendlimari R, Touzios JG, Azodo IA, Chua HK, Dozois EJ, Cima RR, Larson DW. Short-term outcomes after elective minimally invasive colectomy for diverticulitis. Br J Surg. 2011;98:431–435. doi: 10.1002/bjs.7345. [DOI] [PubMed] [Google Scholar]
- 96.Cirocchi R, Cochetti G, Randolph J, Listorti C, Castellani E, Renzi C, Mearini E, Fingerhut A. Laparoscopic treatment of colovesical fistulas due to complicated colonic diverticular disease: a systematic review. Tech Coloproctol. 2014;18:873–885. doi: 10.1007/s10151-014-1157-5. [DOI] [PubMed] [Google Scholar]
- 97.Laurent SR, Detroz B, Detry O, Degauque C, Honoré P, Meurisse M. Laparoscopic sigmoidectomy for fistulized diverticulitis. Dis Colon Rectum. 2005;48:148–152. doi: 10.1007/s10350-004-0745-2. [DOI] [PubMed] [Google Scholar]
- 98.Engledow AH, Pakzad F, Ward NJ, Arulampalam T, Motson RW. Laparoscopic resection of diverticular fistulae: a 10-year experience. Colorectal Dis. 2007;9:632–634. doi: 10.1111/j.1463-1318.2007.01268.x. [DOI] [PubMed] [Google Scholar]
- 99.Abbass MA, Tsay AT, Abbas MA. Laparoscopic resection of chronic sigmoid diverticulitis with fistula. JSLS. 2013;17:636–640. doi: 10.4293/108680813X13693422520512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sorrentino M, Brizzolari M, Scarpa E, Malisan D, Bruschi F, Bertozzi S, Bernardi S, Petri R. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a definitive treatment? Retrospective analysis of 63 cases. Tech Coloproctol. 2015;19:105–110. doi: 10.1007/s10151-014-1258-1. [DOI] [PubMed] [Google Scholar]


