Supplemental Digital Content is Available in the Text.
Key Words: alcohol consumption, HIV infection, mortality, cardiovascular diseases, cohort study
Abstract
Objectives:
In HIV-negative populations, light-to-moderate alcohol consumption is associated with a lower cardiovascular morbidity and mortality than alcohol abstention. Whether the same holds true for HIV-infected individuals has not been evaluated in detail.
Design:
Cohort study.
Methods:
Adults on antiretroviral therapy in the Swiss HIV Cohort Study with follow-up after August 2005 were included. We categorized alcohol consumption into: abstention or very low (<1 g/d), low (1–9 g/d), moderate (10–29 g/d in women and 10–39 g/d in men), and high alcohol intake. Cox proportional hazards models were used to describe the association between alcohol consumption and cardiovascular disease-free survival (combined endpoint), cardiovascular disease events (CADE) and overall survival. Baseline and time-updated risk factors for CADE were included in the models.
Results:
Among 9741 individuals included, there were 788 events of major CADE or death during 46,719 patient-years of follow-up, corresponding to an incidence of 1.69 events/100 person-years. Follow-up according to alcohol consumption level was 51% no or very low, 20% low, 23% moderate, and 6% high intake. As compared with no or very low alcohol intake, low (hazard ratio 0.79, 95% confidence interval 0.63 to 0.98) and moderate alcohol intakes (0.78, 0.64 to 0.95) were associated with a lower incidence of the combined endpoint. There was no significant association between alcohol consumption and CADE.
Conclusions:
Compared with no or very low alcohol consumption, low and moderate intake associated with a better CADE-free survival. However, this result was mainly driven by mortality and the specific impact of drinking patterns and type of alcoholic beverage on this outcome remains to be determined.
INTRODUCTION
In the general population, episodic intake of large amounts of alcohol increases mortality,1 whereas low-to-moderate alcohol consumption is associated with a lower cardiovascular morbidity and mortality compared with alcohol abstention.2,3 Whether the latter association depends on the type of alcoholic beverage, the frequency of intake or on associated socio-cultural behaviors remains of debate.2,4,5
In HIV-infected individuals, excessive alcohol consumption has been associated with several negative outcomes, including mortality, increased sexual risk behavior, lower adherence to and higher interruptions of antiretroviral therapy (ART), and impaired response to ART.6–9 However, only a few studies have assessed the impact of alcohol consumption on cardiovascular outcomes in this population. Low or moderate alcohol consumption was associated with a low prevalence of cardiovascular disease in an American cross-sectional study10 and a reduced risk of major cardiovascular disease events (CADE) in a prospective multisite French cohort.11 Although the first study did not differentiate between no alcohol intake and low or moderate consumption, the second was limited by a small sample size and a low number of observed cardiovascular events. Importantly, neither study assessed the impact of low and moderate alcohol consumption on CADE-free survival and overall mortality.
We performed a thorough analysis of the association between different levels of alcohol consumption and CADE-free survival and overall mortality in a large, nationwide HIV cohort. To reduce confounding, time-updated data on the quantity and patterns of alcohol consumption and detailed information on all important cardiovascular risk factors and HIV-related clinical parameters were adjusted for.
METHODS
The Swiss HIV Cohort Study
The Swiss HIV Cohort Study (SHCS, www.shcs.ch) is a prospective cohort study with ongoing enrollment of HIV-infected adults in Switzerland since 1988. It covers close to 50% of the cumulative number of HIV infections declared to the Swiss public health authorities and 75% of individuals receiving ART in Switzerland.12 Representativeness remained stable over the years. Detailed information on demographics, mode of HIV acquisition, risk behavior, clinical events, coinfections, comorbidities, and treatment is collected using a standard protocol at registration and then at intervals of 6 months. Local ethical committees of all participating study sites have approved the study and written consent has been obtained from all participants.
Inclusion Criteria and Definitions
We included all adult individuals enrolled in the SHCS, who started ART and had at least 1 follow-up visit with available information on alcohol consumption. We considered individual follow-up starting at the first visit with available alcohol data. The alcohol questionnaire was introduced into the SHCS routine questionnaire in August 2005. Since then, data on self-reported alcohol consumption were collected at 6 months intervals for every patient. The questionnaire captures information on the frequency, quantity, and pattern of alcohol consumption. For this analysis, self-reported alcohol consumption was categorized into: abstention or very low (<1 g/d), low (1–9 g/d), moderate (10–29 g/d in women and 10–39 g/d in men), and high alcohol intake (>39 g/d).
Outcomes
Our primary outcome was a combined endpoint of either death or CADE (CADE-free survival), whichever occurred first. CADE included myocardial infarction, coronary angioplasty, coronary artery bypass grafting, carotid endarterectomy, procedures on other arteries, cerebral infarction, and cerebral hemorrhage. In the SHCS, data on all cardiovascular events are collected on specific, standardized, case-report forms, using reports from medical hospitalizations and performed surgery to inform and validate the diagnosis.
The secondary endpoints were the separate outcomes: CADE, overall survival, and cardiovascular death.
Statistical Analyses
Baseline characteristics of patients at study inclusion were compared between baseline alcohol consumption levels using Kruskal–Wallis and χ2 tests for continuous and categorical variables, respectively. The distribution of clinical outcomes across categories of alcohol intake was presented as absolute numbers and proportions.
Cox proportional hazards models were used to evaluate the association between time-updated alcohol consumption level and CADE-free survival (combined endpoint) and CADE and overall survival. Follow-up was censored at the time of first major CADE, death, or last recorded visit, whichever occurred first. These models were adjusted for all relevant baseline demographic and clinical characteristics, including sex, ethnicity (black vs. others), education level [low (no or basic education), intermediate (high school), and high (high-level education)], HIV transmission group (heterosexual, men who have sex with men, injection drug users, and others), hepatitis C infection (presence of positive hepatitis C virus RNA), hepatitis B infection (positive hepatitis B surface antigen), center for diseases control stage of infection, and family history of cardiovascular disease (yes/no). Anemia, an important predictor of mortality among HIV-infected patients,13 was included as a binary, time-updated variable (yes/no, cutoff value for women 12 g/dL and for men 14 g/dL) as the prevalence of severe anemia was inferior to 1% in our cohort. Age, body mass index (normal, underweight, or overweight/obese), smoking (packs per day), random cholesterol levels [total cholesterol/high-density lipoprotein (HDL)-cholesterol ratio], diabetes mellitus (yes/no), arterial hypertension (yes, if systolic blood pressure exceeds 140 mm Hg or diastolic blood pressure exceeds 90 mm Hg; no otherwise), CD4 cell count, log HIV viral load, and ART regimens [cumulative exposure to abacavir (ABC), efavirenz, nevirapine, and protease inhibitors] were included as time-varying covariates. We carried forward the last observed value of time-dependent covariates. To describe the overall cardiovascular risk profile of the different comparison groups, we used the Framingham 10-year cardiovascular disease risk score as a summary measure.14 The association between alcohol consumption and CADE-free survival was shown in figures including alcohol as a continuous and categorical variable. Similar figures were reproduced for the associations between alcohol intake and the secondary outcomes.
Sensitivity Analyses
Education level is associated with health seeking behavior and could condition drinking patterns. Thus, to assess the possible link between education level and CADE-free survival, we repeated our analyses after stratification by education level categories and a formal test of interaction was performed. Furthermore, to evaluate the impact of the definition of our main independent variable, self-reported alcohol consumption, on the primary outcome, we compared the results of the main analysis with those of a sensitivity analysis in which current alcohol intake was replaced by time-updated average consumption since the beginning of the follow-up period. Finally, “sick quitters” could have been included into the “no/very low alcohol consumption group” and influenced our results. Thus, we repeated the main analyses after excluding the patients with an aspartate aminotransferase-to-Platelet Ratio Index (APRI) score corresponding to liver cirrhosis (APRI >2.0) from this alcohol use category. All statistical analyses were performed using R Version 2.15.2.
RESULTS
Baseline Characteristics
Of 9764 patients included in the study, 51% reported no or very low alcohol consumption at baseline, whereas 20%, 22%, and 7% had a low, moderate, and high alcohol intake, respectively (Table 1). Individuals with no or very low alcohol intake were more likely to be woman and of black ethnicity. The groups with low or moderate alcohol consumption at baseline had the lowest proportions of injection drug users and the highest proportion of highly educated patients. Cardiovascular disease risk profile differed between groups. Framingham cardiovascular disease 10-year risk score increased with alcohol intake at baseline, reaching 7.3% in the group with high alcohol consumption. Whereas smoking and arterial hypertension were most prevalent in this group, participants with no or very low alcohol intake were most likely to have diabetes mellitus and anemia.
TABLE 1.
Baseline Characteristics of Study Population by Level of Alcohol Intake
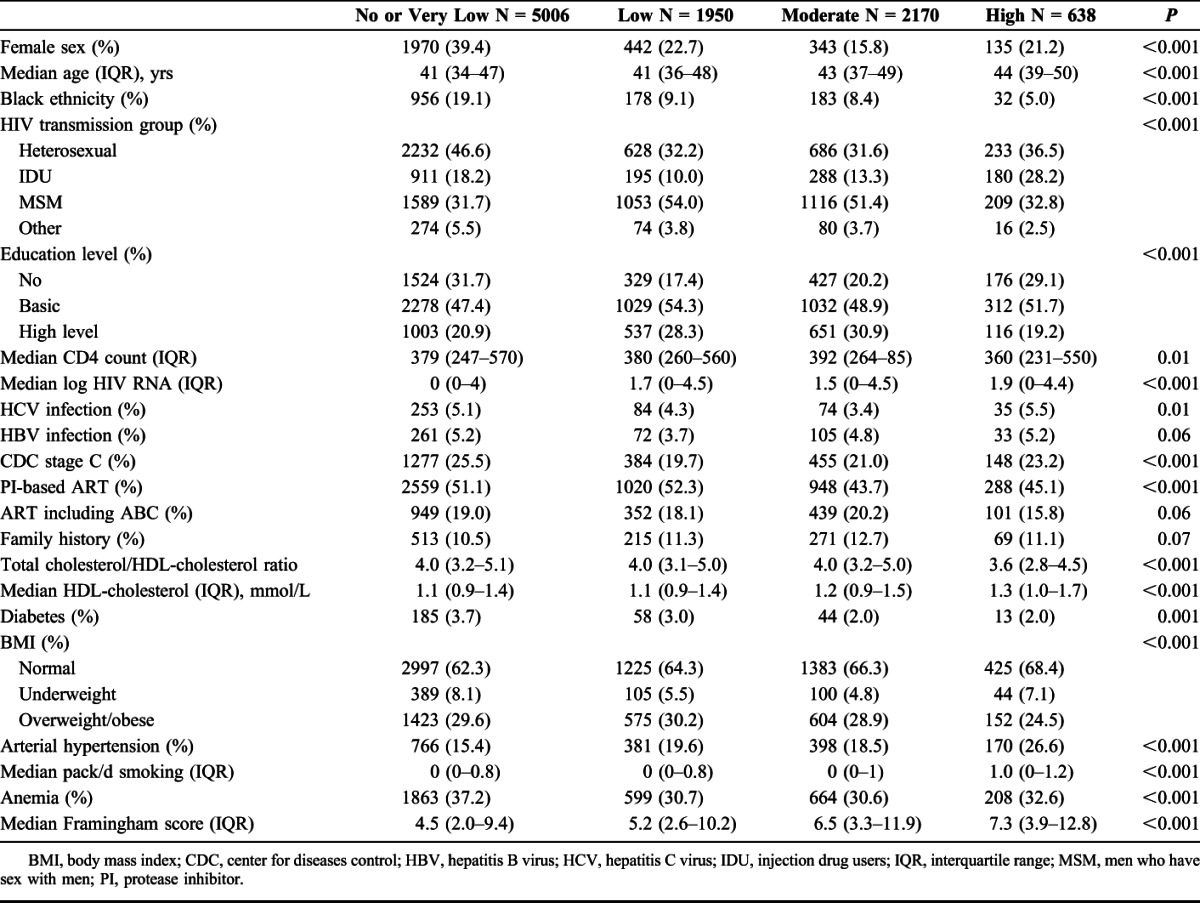
Individual drinking habits remained fairly constant over time: 53% of patients spent at least 80% of their follow-up time in the same drinking category and 92% spent at least 50% of their time in 1 category. The incidence rate of change of alcohol consumption category was 0.44 per person-year (py) of follow-up.
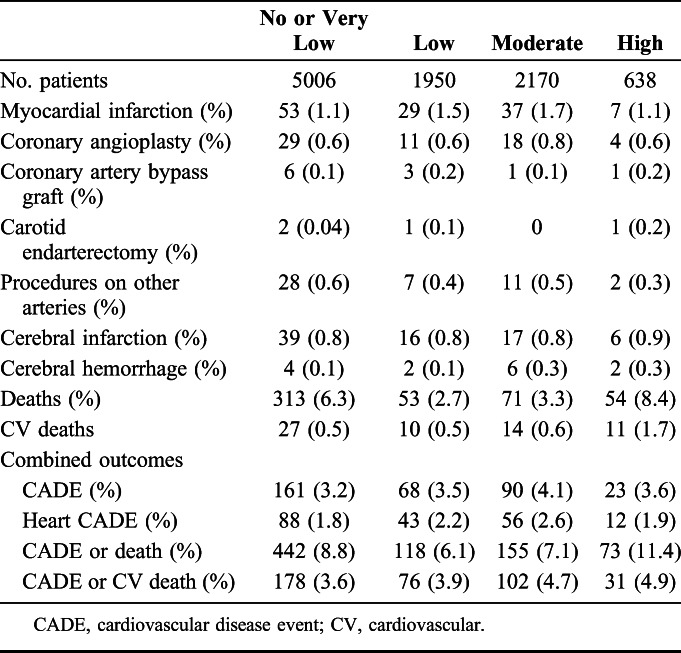
Distribution of CADE and Death According to Alcohol Intake
During 46,719 patient-years of follow-up, 788 individuals either developed a CADE or died; there were 343 CADE and 491 deaths (Table 2). Heart CADE, including myocardial infarction, coronary angioplasty, and coronary artery bypass graft were observed in 199 patients (58% of all CADE). The combined outcome was observed in 442 (8.8%) patients with no or very low alcohol consumption at baseline, whereas 118 (6.1%), 155 (7.1%), and 73 (11.4%) patients with low, moderate, and high alcohol intake developed a CADE or died, respectively. In total, 12.6% of all deaths (62/491) were due to cardiovascular events.
TABLE 2.
Distribution of Outcomes by Level of Alcohol Intake
Incidence of CADE or Death
The incidence of CADE or death (whichever occurred first) was 1.69 events/100 py [95% confidence interval (CI) 1.57 to 1.81]. Overall follow-up time was distributed as follows according to time-updated alcohol consumption: no or very low: 50.6%, low: 20.4%, moderate: 23.3%, and high: 5.7%. Compared with no or very low alcohol intake, low [hazard ratio (HR) 0.79, 95% CI: 0.63 to 0.98] and moderate alcohol intake (0.78, 0.64 to 0.95) were associated with a lower incidence of the combined endpoint, whereas no association was detected for high intake (1.02, 0.78 to 1.34) (Table 3). Figure 1 shows a fitted curve of the association between daily alcohol consumption category or continuous level with the HR of the combined endpoint. The classical cardiovascular risk factors, including age, diabetes mellitus, smoking, total cholesterol/HDL-cholesterol ratio and arterial hypertension, and low CD4 cell count and anemia were significantly associated with a higher hazard of CADE or death. A strong association between education level and the combined outcome was also observed (high vs. low: HR 0.73, 95% CI: 0.59 to 0.95). Finally, a significant association between cumulative treatment with ABC and protease inhibitors and CADE or death could also be shown.
TABLE 3.
Predictors of CADE or Death
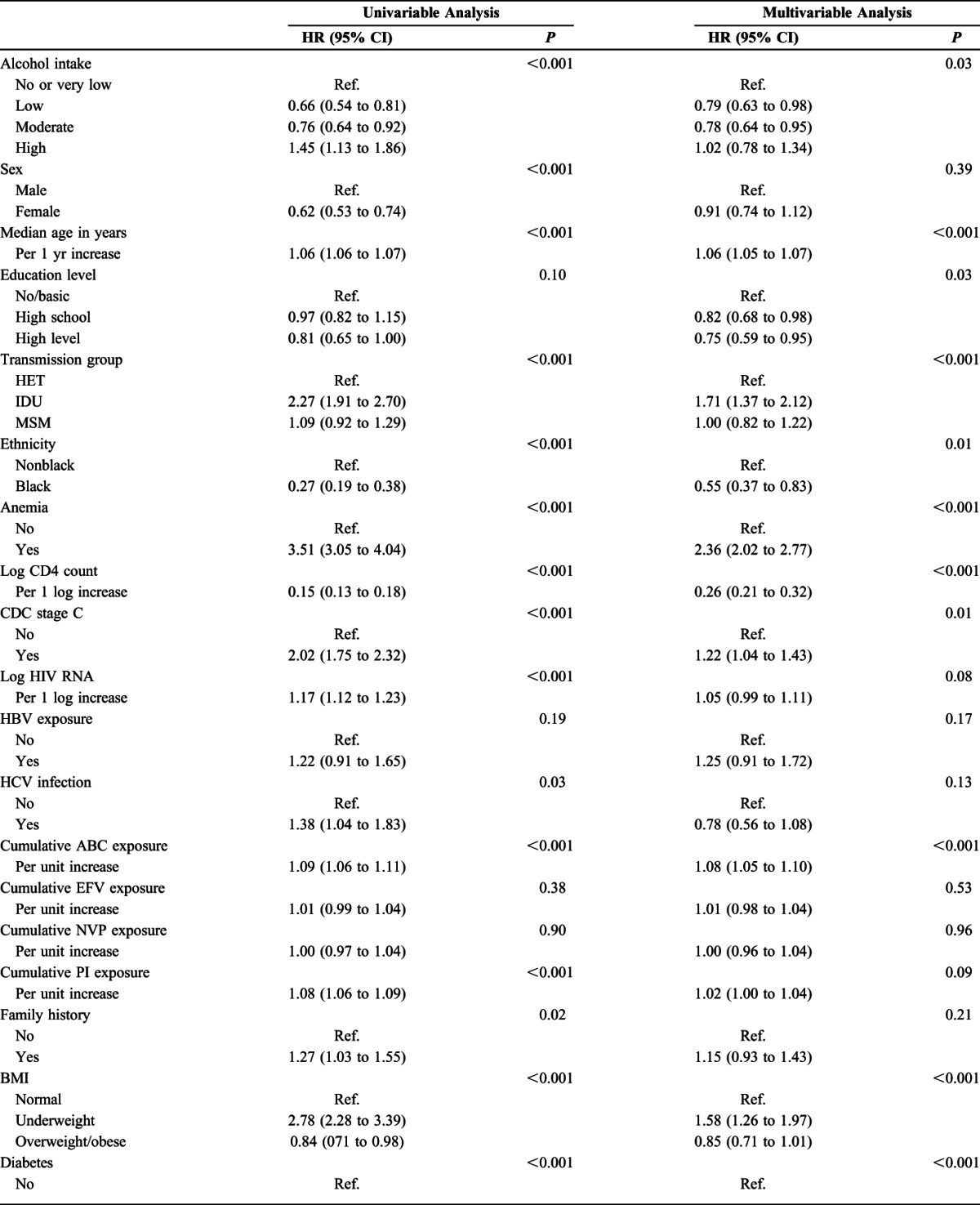
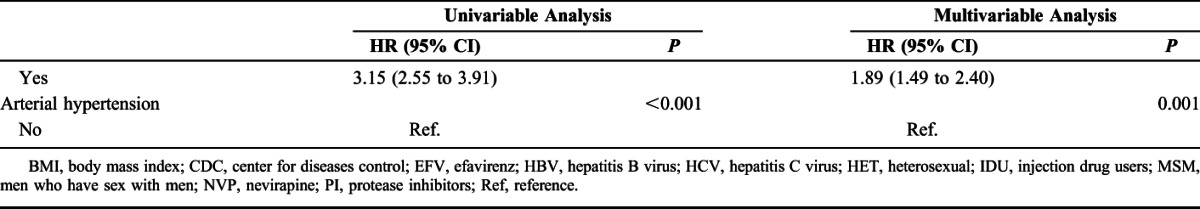
FIGURE 1.
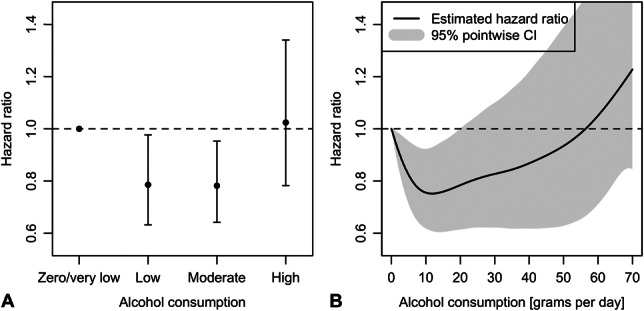
Impact of daily alcohol consumption category (A) and continuous level (B) on the combined endpoint (CADE or death). CI, confidence interval.
Secondary Outcomes
The level of alcohol intake predicted overall survival. We observed 491 deaths during 48,000 py of follow-up, which corresponds to an incidence of 1.03/100 py (95% CI: 0.94 to 1.12). A J-curve similar to the one for the combined outcome could be shown (Fig. 2). Compared with very low alcohol consumption, low (HR 0.57, 95% CI: 0.42 to 0.78) and moderate alcohol intake (0.60, 0.46 to 0.80) were associated with a lower incidence of death. Again, there was no association between high alcohol intake and death (HR 1.02, 0.74 to 1.42). Education level and all classical cardiovascular risk factors were associated with mortality, whereas no specific antiretroviral drug was associated with this outcome. During 47,000 py of follow-up, 343 CADE were noted, which corresponded to an incidence of 0.73/100 py (95% CI: 0.66 to 0.82). However, low (HR 1.09, 95% CI: 0.81 to 1.47) or moderate (1.02, 0.77 to 1.35) alcohol consumption were not associated with a lower hazard of CADE, as shown in Figure 2. Similarly, low (HR 1.05, 95% CI: 0.50 to 2.22) or moderate (HR 1.03, 95% CI: 0.51 to 2.05) alcohol consumption did not seem to be associated with lower hazard for cardiovascular death.
FIGURE 2.
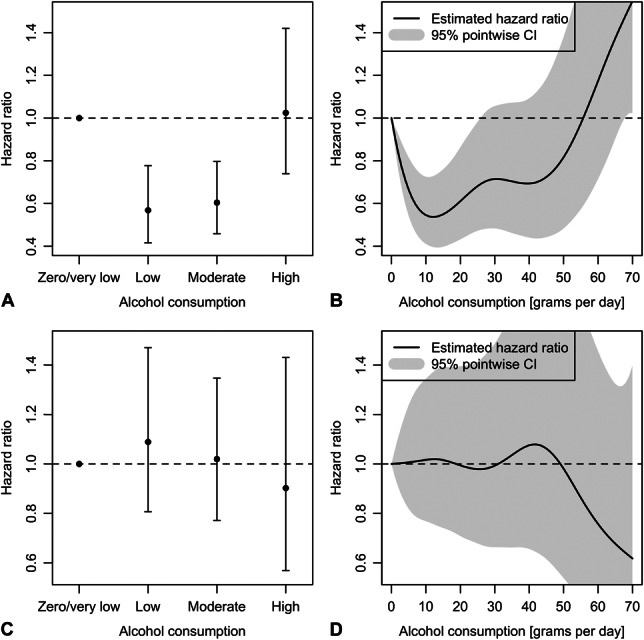
Impact of daily alcohol consumption category and continuous level on separate endpoints (A and B: death; C and D: CADE). CI, confidence interval.
Sensitivity Analyses
In stratified analyses, the J-shaped curve of the association between low/moderate alcohol intake and the combined outcome remained statistically significant for the groups of participants with low or intermediate education levels (see Figure S1, Supplemental Digital Content, http://links.lww.com/QAI/A757). This was not the case for high education level, but the number of patients in this category reporting high alcohol consumption was low. There was no evidence of an interaction between alcohol consumption and education levels in their association with CADE or death (P = 0.64). Replacing time-updated alcohol consumption by average intake as the main independent variable did not change the association between low/moderate alcohol intake and the combined outcome (see Figure S2, Supplemental Digital Content, http://links.lww.com/QAI/A757). Finally, the results of the main analyses obtained after the exclusion of potential sick quitters did not vary significantly from the original results (data not shown).
DISCUSSION
Compared with abstention or very low consumption, low and moderate alcohol intakes were associated with a better CADE-free survival and overall survival in participants of the SHCS receiving ART. These observations persisted after adjustment for a wide range of classical baseline and time-updated cardiovascular risk factors and other known predictors of mortality such as CD4 cell count and anemia. However, the incidence of CADE seemed to be lower with increasing alcohol consumption, possibly because of competing risks. The J-shaped association between alcohol consumption and mortality shown previously in the general population also seems to hold true in HIV-infected individuals on ART.
Of nearly 10,000 individuals included in this study, 51% were alcohol abstainers or had very low consumption at enrollment. Similar proportions have been shown in several studies reporting on the proportion of alcohol abstainers in HIV-infected individuals.15,16 However, in 2 recent publications on the association between alcohol consumption and cardiovascular events in HIV-infected individuals, American veterans and French patients had much lower proportions of abstainers.10,11 Estimates on low or moderate alcohol consumption, the categories of primary interest in this study, are not consistently reported across publications. In our study, approximately 42% of patients were classified into these categories at baseline and the proportion of participants who remained in these groups over time was fairly constant. In comparison, previous landmark studies on the association between moderate alcohol consumption and decreased risk of cardiovascular events in HIV-infected and uninfected individuals had much higher proportions of individuals with moderate alcohol intake.2,11 This is of importance as drinking patterns often carry socio-cultural and behavioral characteristics along, which vary widely across settings and are themselves linked to comorbidities and health seeking behavior.17
We found a moderate association between low or moderate alcohol consumption and CADE-free and overall survival, after adjustment for all relevant cardiovascular risk factors and parameters of advanced HIV disease. The impact of alcohol intake on these outcomes was consistent across strata of education level and did not change significantly whether alcohol was considered as a time-varying covariate or an average estimate. Furthermore, these J-shaped associations could be shown in analyses including alcohol intake as a categorical or continuous variable and the magnitude was similar to published analyses from studies in HIV-uninfected patients.18,19 These findings confirm the results of larger studies in the general population, where a causal link between moderate alcohol consumption and mortality has become evident, including the biological plausibility.3,20 Although HDL-cholesterol levels increased with higher alcohol intake in our study, there was no difference between abstainers and patients with low alcohol intake. Thus, the potential protective effect of HDL-cholesterol linked to the consumption of red wine could not be shown.
In contrast to the study by Carrieri et al,11 we did not find a significant association between alcohol intake and CADE, despite having a much larger sample size and a 7-fold higher number of major CADE, resulting in very similar overall incidence estimates [0.73 (0.66 to 0.82) per 100 patient-years in our study vs. 0.75 (0.57 to 0.99) in Carrieri et al11]. There are several potential explanations for these divergent results. First, there was a large group of patients with very low consumption in the study by Carrieri et al and only few abstainers. Unfortunately, in our study, we were not able to distinguish abstainers from patients with very low alcohol consumption (less than 1 drink per week). Thus, the category no or very low alcohol consumption could have included patients with good cardiovascular profile (as shown by the low Framingham cardiovascular risk score in this group) and a smaller group of less healthy individuals (eg, sick quitters). However, in a sensitivity analyses performed after the exclusion of abstainers with possible liver cirrhosis, we did not find significant differences in the association between alcohol consumption and the main outcomes. Second, we may have over corrected our model by including clinical and laboratory CADE risk factors which may have been on the causal pathway between alcohol consumption and protection of CADE. However, a forward step-wise adjustment strategy did not confirm this potential explanation. Finally, the difference in the results between the 2 studies might have occurred because of the use of time-updated covariates in our analyses.
All main cardiovascular risk factors, including age, smoking, arterial hypertension, diabetes mellitus and hyperlipidemia, and anemia, were associated with the hazard of CADE, CADE-free survival, and death. This strengthens the validity of our model and shows the need to rely on high-quality data on these confounders when analyzing the impact of alcohol on long-term clinical outcomes. The impact of several antiretroviral drugs on cardiovascular events has been much debated in recent years. ABC has been in the forefront of these discussions, as several large-scale observational studies had shown its potential impact on myocardial infarction.21,22 In our study, time spent on ABC was a significant risk factor of CADE and CADE-free survival but not of overall survival. However, the point estimates were close to 1 and we did not adjust our analyses for renal dysfunction, which has been shown to be a potential confounder in such analyses.22
This is the first study to assess the impact of different alcohol consumption levels on cardiovascular disease-free survival in a nationwide population of HIV-infected individuals. Taking advantage of the systematic and repeated collection of detailed information on alcohol consumption within the framework of the SHCS, we were able to determine each patient's intake over time and to classify all individuals into one of the main alcohol consumption categories. Furthermore, dedicated ascertainment of cardiovascular events and reasons of death and the availability of information on all classical cardiovascular risk factors over time allowed us to study the impact of baseline and time-updated alcohol intake on several long-term outcomes in detail. The main limitations of our study are the self-reported nature of individual alcohol consumption, which might have led to some degree of reporting bias and the lack of information on the type of alcoholic beverage consumed. Thus, we were not able to disentangle the relationship between specific types of alcohol, for example wine in the “French paradox,” and long-term outcomes. However, it has been suggested that the type of alcohol might not play such an important role as the beverage most widely consumed seems to be the one most likely to have a protective effect on the risk of cardiovascular events and death.5
Our study underlines the protective effect of low and moderate alcohol consumption on cardiovascular event-free survival and overall survival. Thus, there is no signal that low-to-moderate alcohol consumption should be avoided by HIV-infected persons on ART. However, the main reasons for this association are still unclear. In this regard, the role played by different types of alcoholic beverages, drinking patterns, and social and behavioral characteristics linked to them need to be further explored. Furthermore, these findings warrant more detailed analyses of causes of death besides cardiovascular events to inform public health strategies and guidance on the benefits and risks of low and moderate alcohol consumption.
ACKNOWLEDGMENTS
The authors thank all patients, doctors, and nurses associated with the Swiss HIV Cohort Study (SHCS). The members of the Swiss HIV Cohort Study are: Aubert V, Barth J, Battegay M, Bernasconi E, Böni J, Bucher HC, Burton-Jeangros C, Calmy A, Cavassini M, Egger M, Elzi L, Fehr J, Fellay J, Francioli P, Furrer H (Chairman of the Clinical and Laboratory Committee), Fux CA, Gorgievski M, Günthard H (President of the SHCS), Haerry D (deputy of “Positive Council”), Hasse B, Hirsch HH, Hirschel B, Hösli I, Kahlert C, Kaiser L, Keiser O, Kind C, Klimkait T, Kovari H, Ledergerber B, Martinetti G, Martinez de Tejada B, Metzner K, Müller N, Nadal D, Pantaleo G, Rauch A (Chairman of the Scientific Board), Regenass S, Rickenbach M (Head of Data Center), Rudin C (Chairman of the Mother & Child Substudy), Schmid P, Schultze D, Schöni-Affolter F, Schüpbach J, Speck R, Taffé P, Tarr P, Telenti A, Trkola A, Vernazza P, Weber R, and Yerly S.
Footnotes
Supported by the framework of the Swiss HIV Cohort Study, supported by the Swiss National Science Foundation (SNF Grant number 33CSC0-108787, SHCS project number 733). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the article.
Presented in part at the 21st Conference on Retroviruses and Opportunistic Infections (CROI), March 3–6, 2014, Boston, MA.
H.F. grew up in a farm in Zurich “Wyland,” which included a vineyard. His brother produces and sells his own red wine. G.W. was supported by an Ambizione-PROSPER fellowship from the Swiss National Science Foundation (PZ00P3_154730). The remaining authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
G.W. and H.F. designed the study. D.K. performed the statistical analyses. G.W., D.K., and H.F. wrote the first draft of the article. All authors contributed to the interpretation of the results and to the final version of the article. G.W., D.K., and H.F. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. G.W. and D.K. contributed equally to this article.
REFERENCES
- 1.Kauhanen J, Kaplan GA, Goldberg DE, et al. Beer binging and mortality: results from the kuopio ischaemic heart disease risk factor study, a prospective population based study. BMJ. 1997;315:846–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mukamal KJ, Conigrave KM, Mittleman MA, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348:109–118. [DOI] [PubMed] [Google Scholar]
- 3.Ronksley PE, Brien SE, Turner BJ, et al. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Renaud S, de Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet. 1992;339:1523–1526. [DOI] [PubMed] [Google Scholar]
- 5.Marques-Vidal P, Ducimetiere P, Evans A, et al. Alcohol consumption and myocardial infarction: a case-control study in France and Northern Ireland. Am J Epidemiol. 1996;143:1089–1093. [DOI] [PubMed] [Google Scholar]
- 6.Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. J Acquir Immune Defic Syndr. 2006;43:411–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conen A, Wang Q, Glass TR, et al. Association of alcohol consumption and HIV surrogate markers in participants of the Swiss HIV cohort study. J Acquir Immune Defic Syndr. 2013;64:472–478. [DOI] [PubMed] [Google Scholar]
- 8.Braithwaite RS, Conigliaro J, Roberts MS, et al. Estimating the impact of alcohol consumption on survival for HIV+ individuals. AIDS Care. 2007;19:459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrieri MP, Protopopescu C, Raffi F, et al. Low alcohol consumption as a predictor of higher CD4+ cell count in HIV-treated patients: a French paradox or a proxy of healthy behaviors? The ANRS APROCO-COPILOTE CO-08 cohort. J Acquir Immune Defic Syndr. 2014;65:e148–e150. [DOI] [PubMed] [Google Scholar]
- 10.Freiberg MS, McGinnis KA, Kraemer K, et al. The association between alcohol consumption and prevalent cardiovascular diseases among HIV-infected and HIV-uninfected men. J Acquir Immune Defic Syndr. 2010;53:247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carrieri MP, Protopopescu C, Le Moing V, et al. Impact of immunodepression and moderate alcohol consumption on coronary and other arterial disease events in an 11-year cohort of HIV-infected patients on antiretroviral therapy. BMJ Open. 2012;2:e001155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schoeni-Affolter F, Ledergerber B, Rickenbach M, et al. Cohort profile: the Swiss HIV Cohort study. Int J Epidemiol. 2010;39:1179–1189. [DOI] [PubMed] [Google Scholar]
- 13.Lundgren JD, Mocroft A. Anemia and survival in human immunodeficiency virus. Clin Infect Dis. 2003;37(suppl 4):S297–S303. [DOI] [PubMed] [Google Scholar]
- 14.D'Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. [DOI] [PubMed] [Google Scholar]
- 15.Galvan FH, Bing EG, Fleishman JA, et al. The prevalence of alcohol consumption and heavy drinking among people with HIV in the United States: results from the HIV Cost and Services Utilization Study. J Stud Alcohol. 2002;63:179–186. [DOI] [PubMed] [Google Scholar]
- 16.Kowalski S, Colantuoni E, Lau B, et al. Alcohol consumption and CD4 T-cell count response among persons initiating antiretroviral therapy. J Acquir Immune Defic Syndr. 2012;61:455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rimm EB. Alcohol consumption and coronary heart disease: good habits may be more important than just good wine. Am J Epidemiol. 1996;143:1094–1098; discussion 1099. [DOI] [PubMed] [Google Scholar]
- 18.Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, et al. Alcohol consumption, heavy drinking, and mortality: rethinking the j-shaped curve. Alcohol Clin Exp Res. 2014;38:471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellavia A, Bottai M, Wolk A, et al. Alcohol consumption and mortality: a dose-response analysis in terms of time. Ann Epidemiol. 2014;24:291–296. [DOI] [PubMed] [Google Scholar]
- 20.Brien SE, Ronksley PE, Turner BJ, et al. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruciani M, Zanichelli V, Serpelloni G, et al. Abacavir use and cardiovascular disease events: a meta-analysis of published and unpublished data. AIDS. 2011;25:1993–2004. [DOI] [PubMed] [Google Scholar]
- 22.Costagliola D, Lang S, Mary-Krause M, et al. Abacavir and cardiovascular risk: reviewing the evidence. Curr HIV/AIDS Rep. 2010;7:127–133. [DOI] [PubMed] [Google Scholar]


