Abstract
Background:
Inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) are elevated in end-stage renal disease (ESRD). IL-6 and TNF-α are toxins which deteriorate renal function, and their pathogenic role has been confirmed in cardiovascular and oral diseases. This study was designed to investigate the salivary levels of IL-6 and TNF-α in patients with ESRD undergoing hemodialysis (HD).
Materials and Methods:
Twenty patients with ESRD who were treated with 4 h HD sessions, with low flux membrane were included in this cross-sectional study. Average Kt/V index in patients was 1.19 ± 0.1. Twenty age-sex-matched healthy controls with no infectious diseases during 1 month before saliva sampling were selected. Unstimulated whole saliva was collected and TNF-α and IL-6, concentrations were measured using human IL-6 and TNF-α ELISA kits. Independent t-test was used to analyze the data using SPSS (α = 0.05).
Results:
There was a significant difference between dialysis and control groups regarding the salivary levels of TNF-α (P = 0.034) and IL-6 (P = 0.001).
Conclusion:
Considering the results of this study and reported role of inflammatory cytokines in the pathogenesis of cardiovascular and oral diseases, measurement of salivary IL-6 and TNF-α in HD patients may help in risk stratification of HD patients and in planning pertinent preventive strategies.
Keywords: Cytokine, hemodialysis, renal failure, saliva
INTRODUCTION
Chronic kidney disease (CKD) refers to the progressive loss of renal function.[1] Unfortunately, large numbers of patients have gone undiagnosed at earlier stages of CKD, which increases the risk for development of end stage renal disease (ESRD).[2,3]
Inflammatory response can reflect an underlying systemic disease.[4] Patients with CKD demonstrate activation of inflammatory pathways,[5,6] which is accompanied by increased inflammatory markers like cytokines.[4] The elevated levels of cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) have been shown in ESRD.[7,8,9,10] Furthermore, these inflammatory markers act as toxins[11] that predict kidney function deterioration.[12]
Patients with ESRD are at a greater risk of cardiovascular and oral diseases.[13] It has been shown that inflammatory markers such as IL-6 and TNF-α enhance the risk of cardiovascular mortality.[10] Furthermore, it is confirmed that oral diseases including oral cancer, lichen planus, and periodontal diseases are associated with IL-6 and TNF-α deregulation.[14] According to some previous studies, we can consider the merit of IL-6 measurement as a prognostic indicator and provide a clinical perspective on IL-6-blocking therapies in renal disease.[15]
To the best of our knowledge, little or no research has been performed so far to compare the salivary levels of IL-6 and TNF-α in patients undergoing hemodialysis (HD) with matched controls. Since, the prognostic value and pathogenic role of IL-6 and TNF-α have been confirmed in publications, the present study aimed to investigate the salivary levels of IL-6 and TNF-α in patients with ESRD undergoing HD.
MATERIALS AND METHODS
The study subject population consisted of 20 dialysis patients who were diagnosed with end-stage renal disease caused by diabetic nephropathy and admitted at Nephrology Department of Isfahan University of Medical Sciences. The Ethics Committee of the University approved the study protocol and informed consent obtained prior to participation in this cross-sectional study.
Patient characteristics
The study included 18 years or older patients who were treated with standard 4 h HD sessions, 3 times a week with low flux membrane and were stable by the time the study was conducted. The mean duration of dialysis was 9 ± 2.3 months. The average Kt/V index in patients was 1.19 ± 0.1 and the protein catabolism index was 1.42 ± 0.2 g/kg/day. None of the patients suffered from any symptoms of infection or collagen vascular diseases. In all patients, cardiovascular diseases were assessed on the basis of the history of echocardiographic abnormalities. Patients with previous myocardial infarction, stable angina, stroke, arteriopathy and heavy smoakers were excluded. Patients had not received any medications known to affect immune functions and the time period from the last blood transfusion was not shorter than 6 months. Furthermore, patients with unstimulated whole saliva (UWS) flow rates of <0.1 ml/min were considered as salivary gland hypo-function and excluded from the study.
Twenty age-sex-matched healthy controls with no infectious diseases during 1 month prior to saliva collection were selected from individuals visiting oral medicine clinic of Isfahan University of Medical Sciences.
Two groups were matched for gingival conditions according to modified gingival index (MGI).[16] MGI eliminates the use of probing or pressure to establish the presence or absence of bleeding. It also makes it possible to detect and record subtle visual changes in gingival inflammation, permits the intra- and inter-calibration of examiners, and is noninvasive upon repeated evaluations.[16]
Saliva sampling
Participants were asked not to eat, drink, or use saliva stimulators such as chewing gum or mint for at least 1 h before sampling. UWS was collected between 10:00 and 11:00 a.m. using the standard technique.[9] Participants were asked to swallow first, and then tilt their head forward and expectorate all saliva into a 50 ml centrifuge tubes for 5 min without swallowing. The saliva samples were frozen at −70°C, until analysis. All samples were centrifuged at 4500 g for 15 min. Supernatants were drawn off and used in the ELISA cytokine assays. TNF-α and IL-6, concentrations were measured using human IL-6 (sensitivity: <0.3 pg/ml) and TNF-α (sensitivity: <1 pg/ml) ELISA kits (Boster Biological Technology Co, CA, USA) according to manufacturer's recommendation.
Statistical analysis
SPSS software version 18 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. Distribution of the variables was examined for normality using Kolmogorov-Smirnov test. Since data were normally distributed, parametric independent t-test was used (α = 0.05).
RESULTS
Forty patients were enrolled in the study. The mean age of the case and control groups were 59 ± 12.4 and 53 ± 10.8 years, respectively. There were 12 and 8 women in the case and control groups, respectively. Two groups were matched for MGI index (12 edentulous patients and 8 patients with score 3). There were no significant gender and age differences between case and control groups.
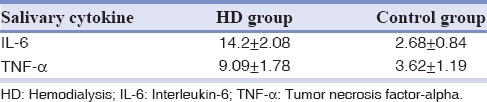
The mean amounts of TNF-α and IL-6 are summarized in Table 1 and Graph 1.
Table 1.
The mean amounts (pg/ml) of TNF-α and IL-6 in HD group and controls
Graph 1.
The mean amounts (pg/ml) of tumor necrosis factor-alpha and interleukin-6 in hemodialysis group and controls.
ELISA analysis of whole unstimulated saliva showed that there was a significant difference between two groups regarding the salivary levels of TNF-α (P = 0.034) and IL-6 (P = 0.001).
DISCUSSION
Cytokines are soluble proteins that play an important role in the initiation and maintenance of inflammatory and immune responses.[14] Many of prior studies have found that inflammatory cytokines such as IL-6 and TNF-α are elevated in ESRD,[17,18,19] and some studies report salivary cytokines and secretion rates are significantly decreased in CKD patients, and recommend further research.[20]
Furthermore, IL-6 and TNF-α are toxins which may deteriorate renal function by triggering endothelial dysfunction and glomerular injury[4] and act as independent risk factors for mortality.
We examined the salivary level of IL-6 and TNF-α in patients with ESRD undergoing HD. Our hypothesis was that there would be a significant difference in the salivary levels of these markers between HD and control groups. The results of the study confirmed our hypothesis. It was shown that salivary levels of IL-6 and TNF-α are significantly higher in patients with ESRD undergoing HD.
Saliva is a safe and low-cost alternative and as a biofluid, has several advantages over blood supporting its use in diagnosis and assessment of diseases.[21] Researches have shown that levels of some serum markers like C-reactive protein, IL-2, IL-6, and TNF-α correlate well with those in saliva.[22,23,24]
Elevated circulating levels of IL-6 in patients with congestive heart failure and active inflammation have been reported.[25,26] Therefore, for this study patients with any signs of cardiovascular diseases or infections were excluded. In this study, patients who received dialysis with low-flux polysulfone membrane were included. It is confirmed that the contact of blood with dialyzer membrane leads to degranulation of polymorphonuclear leukocytes and release of inflammatory mediators.[26,27] Furthermore, different studies assessed the back-leakage of endotoxin from the contaminated dialysate membrane, and it was found that high-flux dialyzers are the proposed mechanisms of monocyte stimulation and elevated inflammatory cytokines.[28,29] Therefore in the present study, patients received dialysis with low-flux polysulfone membrane.
It is now well established that high prevalence of inflammatory cytokines are associated with the high rate of cardiovascular morbidity and mortality in ESRD patients.[30] Increased levels of inflammatory biomarkers in ESRD can promote atherosclerosis and thrombosis.[31] These mechanisms may explain the high prevalence of cardiovascular disease among persons developing ESRD. Therefore, measurement of salivary cytokines levels may be considered as a noninvasive test for cardiac risk stratification in ESRD patients undergoing HD.
A number of oral diseases including lichen planus, oral cancer, and periodontal diseases have been reported to be associated with IL-6 deregulation.[14] Periodontal diseases are prevalent in renal dialysis patients who showed an unacceptable level of oral hygiene and its prevalence increases with the chronicity of the illness.[32] Available literature point toward the important role of IL-6 in the loss of periodontal ligament and alveolar bone through the tissue degradation effects of IL-6 on connective tissue and bone, mediated by metalloproteinase and osteoclasts.[14] According to the results of this study, ELISA analysis of whole unstimulated saliva showed that difference between salivary levels of TNF-α and IL-6 was significant (P < 0.05) and the elevated salivary levels of inflammatory cytokines may necessitate the need of comprehensive professional oral care and self-care instruction in dialysis patients.
One of our restrictions in this study was sample size and in this study the correlation between salivary and serum IL-6 and TNF-α was not investigated; hence, we suggest comparative analysis of salivary and serum cytokines in a larger group of patients.
We would like to suggest that commenting on the viability of saliva over blood is possible only when you do a comparative analysis for both.
Although our findings demonstrated that salivary inflammatory biomarkers are elevated in patients undergoing HD; however, the relation between salivary cytokine levels and the efficacy of HD has not been assessed. Furthermore, it is recommended to conduct further studies to investigate the prognostic value of salivary inflammatory cytokines in cardiovascular and oral diseases.
CONCLUSION
Considering the significant elevation of salivary TNF-α and IL-6 in this study and reported role of inflammatory cytokines in the pathogenesis of cardiovascular and oral disease, our findings support the need for additional studies. If confirmed, measurement of salivary IL-6 and TNF-α in HD patient may be considered as a noninvasive test for cardiac risk stratification to help in risk assessment of HD patients, and in planning pertinent preventive strategies.
Financial support and sponsorship
This study has been funded by Isfahan University of Medical Sciences.
Conflicts of interest:
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
REFERENCES
- 1.Fatahzadeh M. The spectrum of orofacial manifestations in renal osteodystrophy: Diagnostic challenges of an uncommon presentation. Quintessence Int. 2011;42:e78–88. [PubMed] [Google Scholar]
- 2.Kausz AT, Khan SS, Abichandani R, Kazmi WH, Obrador GT, Ruthazer R, et al. Management of patients with chronic renal insufficiency in the Northeastern United States. J Am Soc Nephrol. 2001;12:1501–7. doi: 10.1681/ASN.V1271501. [DOI] [PubMed] [Google Scholar]
- 3.Coresh J, Wei GL, McQuillan G, Brancati FL, Levey AS, Jones C, et al. Prevalence of high blood pressure and elevated serum creatinine level in the United States: Findings from the third National Health and Nutrition Examination Survey (1988-1994) Arch Intern Med. 2001;161:1207–16. doi: 10.1001/archinte.161.9.1207. [DOI] [PubMed] [Google Scholar]
- 4.Cachofeiro V, Goicochea M, de Vinuesa SG, Oubiña P, Lahera V, Luño J. Oxidative stress and inflammation, a link between chronic kidney disease and cardiovascular disease. Kidney Int Suppl. 2008;111:S4–9. doi: 10.1038/ki.2008.516. [DOI] [PubMed] [Google Scholar]
- 5.Stenvinkel P, Heimbürger O, Tuck CH, Berglund L. Apo(a)-isoform size, nutritional status and inflammatory markers in chronic renal failure. Kidney Int. 1998;53:1336–42. doi: 10.1046/j.1523-1755.1998.00880.x. [DOI] [PubMed] [Google Scholar]
- 6.Stenvinkel P, Heimbürger O, Paultre F, Diczfalusy U, Wang T, Berglund L, et al. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 1999;55:1899–911. doi: 10.1046/j.1523-1755.1999.00422.x. [DOI] [PubMed] [Google Scholar]
- 7.Landray MJ, Wheeler DC, Lip GY, Newman DJ, Blann AD, McGlynn FJ, et al. Inflammation, endothelial dysfunction, and platelet activation in patients with chronic kidney disease: The chronic renal impairment in Birmingham (CRIB) study. Am J Kidney Dis. 2004;43:244–53. doi: 10.1053/j.ajkd.2003.10.037. [DOI] [PubMed] [Google Scholar]
- 8.De Vinuesa SG, Goicoechea M, Kanter J, Puerta M, Cachofeiro V, Lahera V, et al. Insulin resistance, inflammatory biomarkers, and adipokines in patients with chronic kidney disease: Effects of angiotensin II blockade. J Am Soc Nephrol. 2006;17(12 Suppl 3):S206–12. doi: 10.1681/ASN.2006080916. [DOI] [PubMed] [Google Scholar]
- 9.Goicoechea M, de Vinuesa SG, Lahera V, Cachofeiro V, Gómez-Campderá F, Vega A, et al. Effects of atorvastatin on inflammatory and fibrinolytic parameters in patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(12 Suppl 3):S231–5. doi: 10.1681/ASN.2006080938. [DOI] [PubMed] [Google Scholar]
- 10.Stenvinkel P. New insights on inflammation in chronic kidney disease-genetic and non-genetic factors. Nephrol Ther. 2006;2:111–9. doi: 10.1016/j.nephro.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Vanholder R, De Smet R, Glorieux G, Argilés A, Baurmeister U, Brunet P, et al. Review on uremic toxins: Classification, concentration, and interindividual variability. Kidney Int. 2003;63:1934–43. doi: 10.1046/j.1523-1755.2003.00924.x. [DOI] [PubMed] [Google Scholar]
- 12.Fried L, Solomon C, Shlipak M, Seliger S, Stehman-Breen C, Bleyer AJ, et al. Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J Am Soc Nephrol. 2004;15:3184–91. doi: 10.1097/01.ASN.0000146422.45434.35. [DOI] [PubMed] [Google Scholar]
- 13.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 14.Nibali L, Fedele S, D'Aiuto F, Donos N. Interleukin-6 in oral diseases: A review. Oral Dis. 2012;18:236–43. doi: 10.1111/j.1601-0825.2011.01867.x. [DOI] [PubMed] [Google Scholar]
- 15.Jones SA, Fraser DJ, Fielding CA, Jones GW. Interleukin-6 in renal disease and therapy. Nephrol Dial Transplant. 2015;30:564–74. doi: 10.1093/ndt/gfu233. [DOI] [PubMed] [Google Scholar]
- 16.Lobene RR, Weatherford T, Ross NM, Lamm RA, Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986;8:3–6. [PubMed] [Google Scholar]
- 17.Owen WF, Lowrie EG. C-reactive protein as an outcome predictor for maintenance hemodialysis patients. Kidney Int. 1998;54:627–36. doi: 10.1046/j.1523-1755.1998.00032.x. [DOI] [PubMed] [Google Scholar]
- 18.Bologa RM, Levine DM, Parker TS, Cheigh JS, Serur D, Stenzel KH, et al. Interleukin-6 predicts hypoalbuminemia, hypocholesterolemia, and mortality in hemodialysis patients. Am J Kidney Dis. 1998;32:107–14. doi: 10.1053/ajkd.1998.v32.pm9669431. [DOI] [PubMed] [Google Scholar]
- 19.Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999;55:648–58. doi: 10.1046/j.1523-1755.1999.00273.x. [DOI] [PubMed] [Google Scholar]
- 20.Thorman R, Lundahl J, Yucel-Lindberg T, Hylander B. Inflammatory cytokines in saliva: Early signs of metabolic disorders in chronic kidney disease. A controlled cross-sectional study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:597–604. doi: 10.1016/j.tripleo.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Nishanian P, Aziz N, Chung J, Detels R, Fahey JL. Oral fluids as an alternative to serum for measurement of markers of immune activation. Clin Diagn Lab Immunol. 1998;5:507–12. doi: 10.1128/cdli.5.4.507-512.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byrne ML, O'Brien-Simpson NM, Reynolds EC, Walsh KA, Laughton K, Waloszek JM, et al. Acute phase protein and cytokine levels in serum and saliva: A comparison of detectable levels and correlations in a depressed and healthy adolescent sample. Brain Behav Immun. 2013;34:164–75. doi: 10.1016/j.bbi.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Wang PL, Ohura K, Fujii T, Oido-Mori M, Kowashi Y, Kikuchi M, et al. DNA microarray analysis of human gingival fibroblasts from healthy and inflammatory gingival tissues. Biochem Biophys Res Commun. 2003;305:970–3. doi: 10.1016/s0006-291x(03)00821-0. [DOI] [PubMed] [Google Scholar]
- 24.Giannopoulou C, Kamma JJ, Mombelli A. Effect of inflammation, smoking and stress on gingival crevicular fluid cytokine level. J Clin Periodontol. 2003;30:145–53. doi: 10.1034/j.1600-051x.2003.300201.x. [DOI] [PubMed] [Google Scholar]
- 25.Carrero JJ, Park SH, Axelsson J, Lindholm B, Stenvinkel P. Cytokines, atherogenesis, and hypercatabolism in chronic kidney disease: A dreadful triad. Semin Dial. 2009;22:381–6. doi: 10.1111/j.1525-139X.2009.00585.x. [DOI] [PubMed] [Google Scholar]
- 26.Gabay C. Interleukin-6 and chronic inflammation. Arthritis Res Ther. 2006;8(Suppl 2):S3. doi: 10.1186/ar1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rysz J, Banach M, Cialkowska-Rysz A, Stolarek R, Barylski M, Drozdz J, et al. Blood serum levels of IL-2, IL-6, IL-8, TNF-alpha and IL-1beta in patients on maintenance hemodialysis. Cell Mol Immunol. 2006;3:151–4. [PubMed] [Google Scholar]
- 28.Panichi V, De Pietro S, Andreini B, Migliori M, Tessore V, Taccola D, et al. Cytokine production in haemodiafiltration: A multicentre study. Nephrol Dial Transplant. 1998;13:1737–44. doi: 10.1093/ndt/13.7.1737. [DOI] [PubMed] [Google Scholar]
- 29.Panichi V, Tetta C, Rindi P, Palla R, Lonnemann G. Plasma C-reactive protein is linked to backfiltration associated interleukin-6 production. ASAIO J. 1998;44:M415–7. doi: 10.1097/00002480-199809000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Himmelfarb J, Stenvinkel P, Ikizler TA, Hakim RM. The elephant in uremia: Oxidant stress as a unifying concept of cardiovascular disease in uremia. Kidney Int. 2002;62:1524–38. doi: 10.1046/j.1523-1755.2002.00600.x. [DOI] [PubMed] [Google Scholar]
- 31.Shlipak MG, Fried LF, Crump C, Bleyer AJ, Manolio TA, Tracy RP, et al. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation. 2003;107:87–92. doi: 10.1161/01.cir.0000042700.48769.59. [DOI] [PubMed] [Google Scholar]
- 32.Hamissi J, Porsamimi J, Naseh MR, Mosalaei S. Oral hygiene and periodontal status of hemodialyzed patients with chronic renal failure in Qazvin, Iran. East Afr J Public Health. 2009;6:108–11. doi: 10.4314/eajph.v6i1.45759. [DOI] [PubMed] [Google Scholar]


