Abstract
In this review, we examine the evolution and application of various diagnostic modalities for varicoceles starting with venography, scintigraphy, and thermography and their role in the evaluation of a varicocele patient. Some of these methods have been supplanted by less invasive and more easily performed diagnostic modalities, especially ultrasound and Doppler examination of the scrotum. Advances in ultrasound and magnetic resonance imaging hold the potential to expand the role of imaging beyond that of visual confirmation and characterization of varicoceles. The ability to identify the early indicators of testicular dysfunction based on imaging findings may have implications for the management of varicoceles in the future.
Keywords: scrotum, testis, varicocele
INTRODUCTION
Varicocele, defined by the dilatation of the venous pampiniform plexus, occurs secondary to retrograde flow via the spermatic vein due to incompetent or absent valves.1 The prevalence of varicocele is estimated at 15%–20% for healthy men, with 35%–40% affected among men seeking infertility treatment.2 Physical examination has long represented the foundation for diagnosing varicoceles. The introduction of radiographic diagnostic studies has allowed for improved detection and further characterization of varicoceles. However, improved detection has generated a subset of subclinical varicoceles which are identified radiographically, but not appreciated on physical examination. Management of these subclinical varicoceles is controversial and, consequently, both the American Society of Reproductive Medicine (ASRM) and American Urological Association (AUA) have recommended against routine radiographic screening with ancillary imaging on patients without a palpable abnormality.3,4 In this review, we will discuss the various modalities utilized in varicocele detection and how they have evolved.
PHYSICAL EXAMINATION
Evaluation for varicocele requires proper room setup, environment, and systematic examination. A warm and comfortable environment for the patient is ideal to allow for relaxed scrotal skin. Cold temperatures and patient distress can result in tightening of the scrotum and preclude identification of a varicocele. It is the authors’ preference to first perform examination in the standing position, both without and with Valsalva maneuvers. Subsequent examination is then repeated in the supine position to evaluate for decompression of the dilated veins. In addition to palpating for pampiniform plexus dilatation, testicular size and consistency should be noted. Grading of varicoceles (Table 1) is based on criteria published by Dubin and Amelar.5
Table 1.
Dubin and Amelar varicocele grading system
The physical examination for varicocele is limited by its subjective nature in addition to patient body habitus. A study involving experienced andrologists and clinicians identified a significant inter- and intra-observer variability in the grading of varicoceles and estimation of testicular size.6 A significant inter-observer error of 16% was found in estimating testicular size, and varicocele grading was inconsistent. In this study, of six clinicians who examined the same patient twice, only two obtained the same results on repeat examination. Compared to venography, physical examination was determined to have a sensitivity of 71% and a specificity of 69%.7 Ultrasound was found to be superior to Prader orchidometers with regards to testicular size estimation.8 However, even ultrasound has been found to suffer from significant inter-institutional variability.9 Despite these limitations, physical examination still represents the gold standard for diagnosing clinically significant varicoceles, which have the clearest indications for repair.3,4
IMAGING MODALITIES
Venography
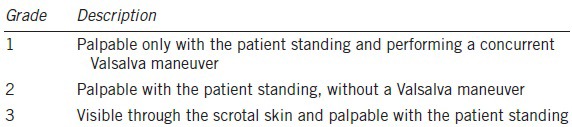
Early reports of retrograde spermatic venography for varicocele were primarily diagnostic in nature and shed light on the mechanism of valvular incompetence or absence.1 Percutaneous access is typically achieved through the right femoral or internal jugular vein, followed by advancement of a catheter to the spermatic vein and retrograde contrast administration (Figure 1).2 Venography is generally considered the most sensitive test, as nearly 100% of individuals with clinically palpable varicocele demonstrate spermatic vein reflux.1
Figure 1.
Venography and embolization of a left-sided grade 3 varicocele.
However, because of its invasive nature and potential for false-positives,10 contemporary use primarily involves concurrent therapeutic intervention with embolization.11 A retrospective review of salvage varicocele embolization after failed surgical ligation therapy highlighted the importance of venography in identifying persistent collateral veins, specifically at the retroperitoneal or inguinal level.12
Thermography and scintigraphy
Historically, scrotal thermography and scintigraphy were developed as noninvasive alternatives to venography. Thermography is a technique using a flexible film containing heat sensitive liquid crystals, which detects changes in scrotal temperature. Identification of varicoceles was based on the finding of hyperthermia over the region of the pampiniform plexus or testis.13 A more contemporary pilot study evaluating diagnostic criteria defined the presence of varicocele in patients with pampiniform plexus temperature of ≥34°C or a difference in temperature of ≥0.5°C between the left and right pampiniform plexus.20 However, other intratesticular pathologies, such as testicular cancer or infection/inflammation, can also result in ipsilateral hyperthermia, thereby decreasing the diagnostic specificity for identifying varicoceles.14
Labeled blood-pool scintigraphy detects varicoceles by demonstrating pooling of tracer on static images and reflux of tracer on dynamic images.15 Unlike thermography, which can only identify the presence of varicocele, scintigraphy can evaluate and quantify the degree of spermatic vein reflux.16,17 Improved detection of subclinical varicoceles with thermography and scintigraphy has been reported;16,18 however, the variability in technique7,19 and lack of standard diagnostic criteria make widespread practice impractical.20 Both thermography and scintigraphy, however, would be supplanted by the increasing availability and capability of ultrasound imaging.
Ultrasound
Scrotal ultrasound is currently the most established and widely used modality for the study of varicoceles. With the use of high-frequency ultrasound probes and the advent of Doppler technology, scrotal ultrasound has become increasingly easy to perform. It can provide high-resolution images and characterize vascular flow within the testes as well as adjacent structures. Given its high sensitivity and specificity (97% and 94% when compared to venography7), noninvasive nature, and relative ease of performance, scrotal ultrasound with Doppler examination has become the study of choice in evaluating scrotal and testicular pathology.21
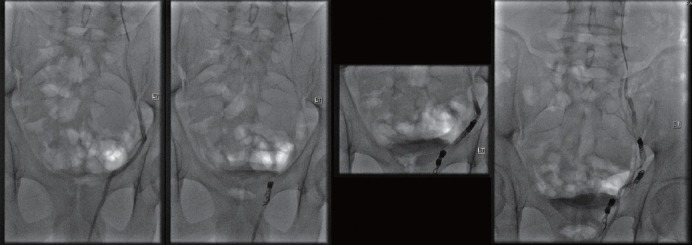
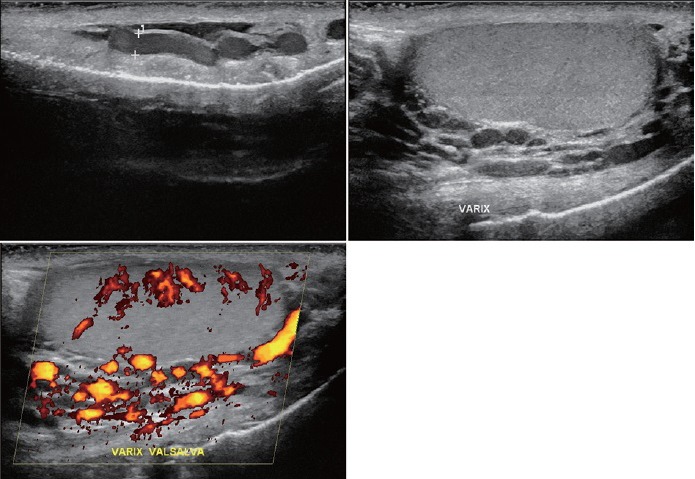
Ultrasound examination of the scrotum is performed with the patient in the supine position. The scrotum is supported with a rolled towel and warmed ultrasound gel is placed on the scrotum. The examination is best performed with high-frequency linear array transducers, usually >7.5 MHz. The examiner should have a low threshold to undertake further study of the varicocele with the patient upright and/or with a Valsalva maneuver.21,22 The characteristic ultrasound appearance of a varicocele is that of “multiple, anechoic, serpiginous, tubular structures,” near the superior and lateral aspects of the testis (Figures 2 and 3).22 Color, power, or spectral Doppler ultrasound with settings optimized for low flow velocities is commonly used to aid in the diagnosis of varicoceles.23 Typical Doppler findings include venous flow at rest with intermittent or continuous flow reversal with Valsalva. Multiple grading systems exist for the purpose of classifying the dynamic sonographic findings of varicocele. The Sarteschi and Dubin classifications as shown in Tables 2 and 3 are among the most commonly used.33,34 A scoring system published by Chiou et al. (Table 4) further improved the sensitivity and specificity of ultrasound in identifying clinically palpable varicoceles.25
Figure 2.
Typical ultrasound appearance of a left-sided grade 3 varicocele.
Figure 3.
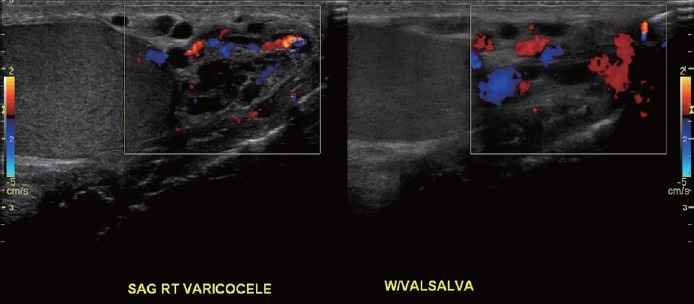
Typical ultrasound appearance of a right-sided grade 3 varicocele.
Table 2.
Sarteschi classification
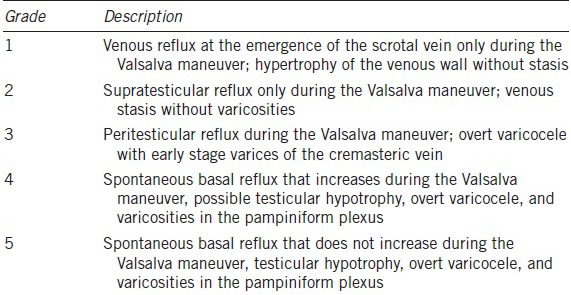
Table 3.
Dubin classification
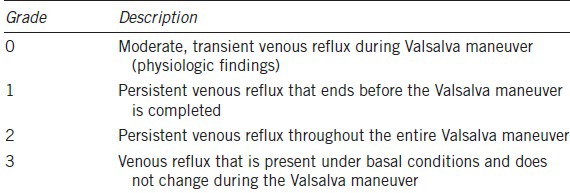
Table 4.
Chiou et al. scoring system
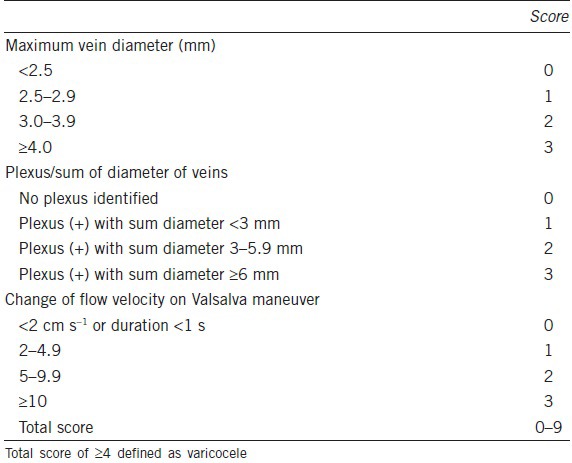
While the general ultrasound appearance of varicoceles is agreed-upon, there are no standardized criteria regarding the extent of venous dilation or reflux that must be present to meet the definition of a varicocele. In a series of 217 men with clinical and subclinical varicoceles, venous diameter of >2.95 mm during Valsalva was associated with sensitivity and specificity of 84% each for clinical varicocele.35 In general, clinicians agree that clinically relevant varicoceles are more than 2.5–3 mm in diameter.24 A scoring system including color Doppler ultrasound findings of vein dilation and flow reversal demonstrated a sensitivity of 93% and a specificity of 85% when compared to physical examination in a series of 127 testes.25 The use of a Doppler stethoscope to detect spermatic vein reflux with a 9 MHz pencil probe has also been described.36 Unfortunately, a series studying 118 patients without clinically palpable varicoceles found that Valsalva-induced reflux occurred on the left in 83% and right in 53%, dampening enthusiasm for the Doppler stethoscope's continued use.40
Until recently, ultrasound evaluation of testicular parenchyma has been relatively simple. Gray-scale ultrasonography can provide a rough estimation of echotexture, calculate testicular volume, and identify parenchymal calcifications or tumors. Doppler ultrasound can provide information about parenchymal flow on a macrovascular level. However, the level of detail afforded by these studies is insufficient to detect varicocele-induced damage to the testicular parenchyma. More recent advances including real-time elastography and contrast-enhanced ultrasonography have demonstrated the potential to correlate the presence of varicoceles to sonographic findings of testicular parenchymal damage and microvascular perfusion defects. Elastography involves postprocessing techniques to quantify testicular tissue stiffness based on measured strain. Contrast-enhanced ultrasound requires intravenous injection of micro-bubbles and allows for superior visualization of both micro- and macro-vasculature.23 Findings such as increased tissue stiffness or loss of microvessel density may suggest early signs of testicular dysfunction. Although still investigational, these technologies may prove to be clinically useful in determining patients that may benefit from varicocele repair based on imaging findings.
Computerized tomography (CT)
Within the scope of varicocele evaluation, cross-sectional imaging is generally reserved for delineation of retroperitoneal anatomy. Approximately, 85%–90% of clinically significant varicoceles are palpated on the left.37 However, a series evaluating 286 infertile men with physical examination, thermography, Doppler sonography, and venography found that inclusion of subclinical varicoceles resulted in 80.7% rate of bilateral disease, suggesting that infertility resulting from varicocele is often from a bilateral process.38 The predisposition of left-sided palpable varicoceles is hypothesized to be a result of increased hydrostatic pressures generated by the perpendicular insertion of the left spermatic vein into the renal vein when compared to the oblique insertion of the right spermatic vein into the vena cava.26 For this reason, classic teaching advises retroperitoneal imaging to rule out renal and retroperitoneal tumors in cases of isolated right-sided varicocele or acute onset of unilateral varicocele in an older patient. However, the overall yield is low, as only 2%–3% of renal tumors present as symptomatic varicoceles.27
The feasibility of varicocele evaluation using CT imaging has been reported but is impractical due to its significant radiation exposure.28 Although lower dosed CT protocols are currently weighed against conventional protocols,29 the low-cost and widespread availability of ultrasound still makes it the preferred initial imaging modality. The increasing resolution of CT imaging, however, has made it an excellent adjunctive modality to study retroperitoneal anatomy. Among a cohort of men identified with a retro-aortic left renal vein on CT imaging, 77% were found to have varicoceles on scrotal ultrasound, which supports the hypothesis of increased hydrostatic pressures resulting in higher incidence of left-sided varicoceles.30 At this time, the role of CT imaging is minimal in diagnosis of varicocele and reserved for clinical scenarios where a retroperitoneal process or malignancy is suspected.
Magnetic resonance imaging (MRI)
Though not common in the literature, there have been some published studies regarding the use of magnetic resonance imaging (MRI) for the diagnosis and imaging of varicoceles. Proposed benefits of MRI in comparison to other existing imaging modalities include most notably, lack of operator dependency, and highly detailed delineation of the retroperitoneal anatomy. When a retroperitoneal cause of varicocele is suspected, MRI may play a role in confirming and further evaluating this cause. In particular, MR angiography has been proposed to study varicoceles secondary to nutcracker syndrome.31
Current areas of research include the use of MRI to evaluate the sequelae of varicoceles, providing important prognostic information to be weighed in considering management options. Diffusion-weighted MRI of the testes was evaluated in a cross-sectional study of 25 subjects with clinically apparent varicoceles and 25 healthy control subjects. Apparent diffusion coefficient (ADC) values were significantly lower in patients with varicocele compared to healthy controls. Based on ADC values, the series demonstrated 90% sensitivity and 96% specificity for the diagnosis of these varicoceles while potentially providing the ability to detect fibrosis of the testicular parenchyma.32
CONCLUSIONS
The introduction of radiographic modalities has vastly improved the ability to detect or confirm the presence of varicoceles. The use of imaging in varicocele has the potential to evolve if early signs of testicular dysfunction can be identified to assist in selection of patients for varicocele repair. Thermography and scintigraphy are of increasingly historic significance while venography and cross-sectional imaging still offer additional information in complex varicocele cases. Ultrasound has emerged as the de facto adjunct to clinical examination due to its inexpensive, widespread, and noninvasive characteristics. The most recent AUA and ASRM guidelines do not recommend the routine use of scrotal ultrasound to diagnose varicoceles. Instead, the role of scrotal ultrasound is reserved for situations in which physical examination is inconclusive, such as patients with large body habitus or thick scrotal skin precluding accurate examination.3,4 On the contrary, the European Association of Urology (EAU) recommends confirmation by color Duplex ultrasound after the diagnosis of varicocele is made by clinical examination.39 The widespread use of scrotal ultrasound, however, has resulted in increased detection of subclinical varicoceles. The question of whether subclinical varicoceles should be repaired is discussed elsewhere in this issue.
AUTHORS CONTRIBUTIONS
All authors had equal contribution to the conception, research, writing of, and review/approval of the manuscript.
COMPETING INTERESTS
None of the authors declared competing financial interests.
REFERENCES
- 1.Ahlberg NE, Bartley O, Chidekel N, Fritjofsson A. Phlebography in varicocele scroti. Acta Radiol Diagn (Stockh) 1966;4:517–28. doi: 10.1177/028418516600400506. [DOI] [PubMed] [Google Scholar]
- 2.Masson P, Brannigan RE. The varicocele. Urol Clin North Am. 2014;41:129–44. doi: 10.1016/j.ucl.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Jarow JP, Sharlip ID, Belker AM, Lipshultz LI, Sigman M, et al. Best practice policies for male infertility. J Urol. 2002;167:2138–44. [PubMed] [Google Scholar]
- 4.Practice Committee of the American Society for Reproductive Medicine, Society for Male Reproduction and Urology. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2014;102:1556–60. doi: 10.1016/j.fertnstert.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970;21:606–9. doi: 10.1016/s0015-0282(16)37684-1. [DOI] [PubMed] [Google Scholar]
- 6.Carlsen E, Andersen AG, Buchreitz L, Jorgensen N, Magnus O, et al. Inter-observer variation in the results of the clinical andrological examination including estimation of testicular size. Int J Androl. 2000;23:248–53. doi: 10.1046/j.1365-2605.2000.00240.x. [DOI] [PubMed] [Google Scholar]
- 7.Trum JW, Gubler FM, Laan R, van der Veen F. The value of palpation, varicoscreen contact thermography and colour Doppler ultrasound in the diagnosis of varicocele. Hum Reprod. 1996;11:1232–5. doi: 10.1093/oxfordjournals.humrep.a019362. [DOI] [PubMed] [Google Scholar]
- 8.Sakamoto H, Saito K, Oohta M, Inoue K, Ogawa Y, et al. Testicular volume measurement: comparison of ultrasonography, orchidometry, and water displacement. Urology. 2007;69:152–7. doi: 10.1016/j.urology.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Sorokin I, Welliver C, Elebyjian L, Feustel PJ, McCullough A. Interinstitutional variability in testicular volumes and varicocele presence by ultrasound: surprising discrepancies and implications for clinical decision making. Urology. 2015;85:1079–84. doi: 10.1016/j.urology.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Nadel SN, Hutchins GM, Albertsen PC, White RI., Jr Valves of the internal spermatic vein: potential for misdiagnosis of varicocele by venography. Fertil Steril. 1984;41:479–81. doi: 10.1016/s0015-0282(16)47733-2. [DOI] [PubMed] [Google Scholar]
- 11.Kwak N, Siegel D. Imaging and interventional therapy for varicoceles. Curr Urol Rep. 2014;15:399. doi: 10.1007/s11934-014-0399-0. [DOI] [PubMed] [Google Scholar]
- 12.Rais-Bahrami S, Montag S, George AK, Rastinehad AR, Palmer LS, et al. Angiographic findings of primary versus salvage varicoceles treated with selective gonadal vein embolization: an explanation for surgical treatment failure. J Endourol/Endourol Soc. 2012;26:556–60. doi: 10.1089/end.2011.0387. [DOI] [PubMed] [Google Scholar]
- 13.Comhaire F, Monteyne R, Kunnen M. The value of scrotal thermography as compared with selective retrograde venography of the internal spermatic vein for the diagnosis of “subclinical” varicocele. Fertil Steril. 1976;27:694–8. doi: 10.1016/s0015-0282(16)41901-1. [DOI] [PubMed] [Google Scholar]
- 14.Gold RH, Ehrlich RM, Samuels B, Dowdy A, Young RT. Scrotal thermography. Radiology. 1977;122:129–32. doi: 10.1148/122.1.129. [DOI] [PubMed] [Google Scholar]
- 15.Freund J, Handelsman DJ, Bautovich GJ, Conway AJ, Morris JG. Detection of varicocele by radionuclide blood-pool scanning. Radiology. 1980;137:227–30. doi: 10.1148/radiology.137.1.7422850. [DOI] [PubMed] [Google Scholar]
- 16.Geatti O, Gasparini D, Shapiro B. A comparison of scintigraphy, thermography, ultrasound and phlebography in grading of clinical varicocele. J Nucl Med: official Publication Soc Nucl Med. 1991;32:2092–7. [PubMed] [Google Scholar]
- 17.Paz A, Melloul M. Comparison of radionuclide scrotal blood-pool index versus gonadal venography in the diagnosis of varicocele. J Nucl Med: official Publication Soc Nucl Med. 1998;39:1069–74. [PubMed] [Google Scholar]
- 18.Hamm B, Fobbe F, Sorensen R, Felsenberg D. Varicoceles: combined sonography and thermography in diagnosis and posttherapeutic evaluation. Radiology. 1986;160:419–24. doi: 10.1148/radiology.160.2.3523594. [DOI] [PubMed] [Google Scholar]
- 19.Nogueira FE, Medeiros F, Barroso LV, Miranda EP, de Castro JD, et al. Infrared digital telethermography: a new method for early detection of varicocele. Fertil Steril. 2009;92:361–2. doi: 10.1016/j.fertnstert.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 20.Kulis T, Kolaric D, Karlovic K, Knezevic M, Antonini S, et al. Scrotal infrared digital thermography in assessment of varicocele – pilot study to assess diagnostic criteria. Andrologia. 2012;44(Suppl 1):780–5. doi: 10.1111/j.1439-0272.2011.01265.x. [DOI] [PubMed] [Google Scholar]
- 21.Dogra VS, Gottlieb RH, Oka M, Rubens DJ. Sonography of the scrotum. Radiology. 2003;227:18–36. doi: 10.1148/radiol.2271001744. [DOI] [PubMed] [Google Scholar]
- 22.Sommers D, Winter T. Ultrasonography evaluation of scrotal masses. Radiol Clin North Am. 2014;52:1265–81. doi: 10.1016/j.rcl.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 23.Schurich M, Aigner F, Frauscher F, Pallwein L. The role of ultrasound in assessment of male fertility. Eur J Obstet Gynecol Reprod Biol. 2009;144(Suppl 1):S192–8. doi: 10.1016/j.ejogrb.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 24.Stahl P, Schlegel PN. Standardization and documentation of varicocele evaluation. Curr Opin Urol. 2011;21:500–5. doi: 10.1097/MOU.0b013e32834b8698. [DOI] [PubMed] [Google Scholar]
- 25.Chiou RK, Anderson JC, Wobig RK, Rosinsky DE, Matamoros A, Jr, et al. Color Doppler ultrasound criteria to diagnose varicoceles: correlation of a new scoring system with physical examination. Urology. 1997;50:953–6. doi: 10.1016/S0090-4295(97)00452-4. [DOI] [PubMed] [Google Scholar]
- 26.Shafik A, Bedeir GA. Venous tension patterns in cord veins. I. In normal and varicocele individuals. J Urol. 1980;123:383–5. doi: 10.1016/s0022-5347(17)55945-5. [DOI] [PubMed] [Google Scholar]
- 27.El-Saeity NS, Sidhu PS. “Scrotal varicocele, exclude a renal tumour”. Is this evidence based? Clin Radiol. 2006;61:593–9. doi: 10.1016/j.crad.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 28.Karcaaltincaba M. Demonstration of normal and dilated testicular veins by multidetector computed tomography. Jpn J Radiol. 2011;29:161–5. doi: 10.1007/s11604-010-0527-9. [DOI] [PubMed] [Google Scholar]
- 29.Kim K, Kim YH, Kim SY, Kim S, Lee YJ, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012;366:1596–605. doi: 10.1056/NEJMoa1110734. [DOI] [PubMed] [Google Scholar]
- 30.Arslan H, Etlik O, Ceylan K, Temizoz O, Harman M, et al. Incidence of retro-aortic left renal vein and its relationship with varicocele. Eur Radiol. 2005;15:1717–20. doi: 10.1007/s00330-004-2563-2. [DOI] [PubMed] [Google Scholar]
- 31.Gulleroglu K, Gulleroglu B, Baskin E. Nutcracker syndrome. World J Nephrol. 2014;3:277–81. doi: 10.5527/wjn.v3.i4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karakas E, Karakas O, Cullu N, Badem OF, Boyaci FN, et al. Diffusion-weighted MRI of the testes in patients with varicocele: a preliminary study. AJR Am J Roentgenol. 2014;202:324–8. doi: 10.2214/AJR.13.10594. [DOI] [PubMed] [Google Scholar]
- 33.Valentino M, Bertolotto M, Derchi L, Pavlica P. Children and adults varicocele: diagnostic issues and therapeutical strategies. J Ultrasound. 2014;17:185–93. doi: 10.1007/s40477-014-0088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pauroso S, Di Leo N, Fulle I, Di Segni M, Alessi S, et al. Varicocele: ultrasonographic assessment in daily clinical practice. J Ultrasound. 2011;14:199–204. doi: 10.1016/j.jus.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pilatz A, Altinkilic B, Köhler E, Marconi M, Weidner W. Color Doppler ultrasound imaging in varicoceles: is the venous diameter sufficient for predicting clinical and subclinical varicocele? World J Urol. 2011;29:645–50. doi: 10.1007/s00345-011-0701-4. [DOI] [PubMed] [Google Scholar]
- 36.Greenberg SH, Lipshultz LI, Wein AJ. A preliminary report of “subclinical varicocele”: diagnosis by Doppler ultrasonic stethoscope. Examination and initial results of surgical therapy. J Reprod Med. 1979;22:77–81. [PubMed] [Google Scholar]
- 37.Skoog SJ, Roberts KP, Goldstein M, Pryor JL. The adolescent varicocele: what's new with an old problem in young patients? Pediatrics. 1997;100:112–21. doi: 10.1542/peds.100.1.112. [DOI] [PubMed] [Google Scholar]
- 38.Gat Y, Bachar GN, Zukerman Z, Belenky A, Gornish M. Varicocele: a bilateral disease. Fertil Steril. 2004;81:424–9. doi: 10.1016/j.fertnstert.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 39.Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, et al. European Association of Urology Working Group on Male Infertility. European Association of Urology guidelines on Male Infertility: the 2012 update. Eur Urol. 2012;62:324–32. doi: 10.1016/j.eururo.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 40.Hirsh AV, Cameron KM, Tyler JP, Simpson J, Pryor JP. The Doppler assessment of varicoceles and internal spermatic vein reflux in infertile men. Br J Urol. 1980;52:50–6. doi: 10.1111/j.1464-410x.1980.tb02919.x. [DOI] [PubMed] [Google Scholar]


