Abstract
In the past, the indications for varicocelectomy are primarily for infertility with abnormal semen parameters, testicular hypotrophy/atrophy in adolescents, and/or pain. The surgical treatment of varicocele for hypogonadism is controversial and debated. Recently, multiple reports in the literature have suggested that varicocele is associated with hypogonadism and varicocele repair can increase testosterone levels. Men with hypogonadal symptoms should have at least two serum testosterone levels. Microsurgical varicocelectomy may be beneficial for men with clinically palpable varicoceles with documented hypogonadism. In this review, we summarize the most recent literature linking varicocele to hypogonadism and sexual dysfunction and the impact of repair on serum testosterone levels. We performed a search of the published English literature. The key words used were “varicocele and hypogonadism” and “varicocele surgery and testosterone.” We included published studies after 1998. We, also, evaluated the effect of surgery on the changes in the serum testosterone level regardless of the indication for the varicocele repair.
Keywords: erectile dysfunction, hypogonadism, varicocele, varicocelectomy
INTRODUCTION
Varicocele is dilation of the veins of the pampiniform plexus draining the testicle. Varicoceles are found in 15% of all men. Of those, 19%–41% will present with primary infertility and 45%–81% will present with secondary infertility.1 Varicocele can adversely affect testicular function in a variety of ways. Varicoceles have long been identified as the most common reversible cause of male infertility.2 Varicocele has also been associated with testicular discomfort, testicular atrophy, and even azoospermia in some men.3 The majority of men with varicoceles are asymptomatic and fertile.4 However, among those who are affected, the evidence for the impact of varicocele on male fertility continues to grow. Given the progressive nature of the effects of varicocele on both spermatogenesis and testosterone production,3 early repair can be advocated as it is easier to prevent future infertility and androgen deficiency than to treat it after it has occurred. Growing evidence suggests that the pathophysiology of varicocele might partially involve dysfunction of the hypothalamic–pituitary–gonadal axis at the level of Leydig cells and lead to hormonal dysfunction.5 Therefore, current challenges in the management of varicoceles lie in determining which patients stand to benefit most from surgical correction in setting of low testosterone. Although the prevalence of isolated hypogonadism in men with varicocele is not well defined, the effect of surgical repair on the changes in the serum testosterone level is mainly evaluated in men who underwent surgery for other indications such as infertility. In this review, we summarize the most recent literature linking varicocele to hypogonadism and sexual dysfunction and the ramification of surgical repair on testosterone levels.
In men who present with clear symptoms of low testosterone and suspected of hypogonadism, a thorough physical examination and laboratory work-up are necessary. Serum total testosterone measurement should be obtained on two different occasions between 07:00 and 11:00 in the morning. Total testosterone is the most widely accepted serum levels to establish the presence of hypogonadism. There are no generally accepted lower limits of normal. However, it is a general agreement that total testosterone level above 350 ng dl−1 does not require treatment or intervention. Clinician should be aware of the risk factors for hypogonadism, which include chronic illnesses (including diabetes mellitus, inflammatory arthritic, renal, and HIV), obesity, and metabolic syndrome. Such chronic diseases should be investigated and treated. When pituitary etiology is suspected, measurements of serum LH will differentiate between primary and secondary hypogonadism, and serum prolactin is indicated when the serum testosterone is extremely low.6
VARICOCELE PATHOPHYSIOLOGY
Varicocelectomy was first utilized for the management of infertile men in the late 1950s.7 Since then, multiple studies have associated with varicocele to testicular dysfunction.8 Testicular atrophy is usually associated with the ipsilateral side of the varicocele. Testicular biopsies before and 1 year after the varicocele repair showed significant improvements in the appearance of seminiferous tubules after surgery.9 These testicular milieu and ultrastructure alterations are implicated by the varicocele as a causal factor to these changes, and the improvement of ultrastructural of the testicle following varicocelectomy may argue for varicocele treatment.
Impairments in testicular function resulting from varicocele are thought to be related to increased testicular temperature, leading to detrimental effects on spermatogenesis, impaired Sertoli cell function, abnormal testicular-protein metabolism, and decreased testicular Leydig cell production of testosterone.10 Elevated intratesticular temperature has also been reported in men with varicocele and infertility.11,12 It is also suggested that the dilation of the pampiniform plexus can lead to prolonged testicular exposure to gonadotoxins from reflux of renal and adrenal metabolites.13 Varicocele has been associated with the increase of the reactive oxygen species (ROS) production and decrease of the all over quantitative levels of antioxidant capacity.14 Oxidative stress markers have been measured in internal spermatic venous blood of patients with clinical varicocele, and there was a distinct increase of these markers within the spermatic veins that can cause protein nitration and cytotoxicity via its reaction with various molecular targets. This could explain some of the repercussions on both sperm and testis function, including testosterone production.15,16
In addition to the effect of varicocele on germ cells and the spermatogenesis, varicoceles have a detrimental impact on other testicular cell types as well. Sertoli cell dysfunction can be detected by the decrease in the responsiveness to follicle stimulating hormone (FSH), and by alterations in androgen binding protein (ABP) and inhibin-B.17,18 In the setting of varicocele, 48%–76% of men with elevated FSH will have improvement in these parameters following varicocelectomy.19,20 Inhibin B levels also often improve after varicocelectomy, suggesting a reversible Sertoli cell defect.21,22
Similar to the hypothesis regarding varicocele and its pathophysiological impact on spermatogenesis, increase in the testicular temperature may also negatively affect testosterone synthesis.23 The effect of varicocele on serum testosterone suggests Leydig cells at the epicenter of this phenomenon. Men with varicocele were observed to have Leydig cell structural changes, Leydig cell atrophy, and notable decreases in the quantity of testosterone positive Leydig cells.24 Animal studies have demonstrated marked decrease in the activities of the five enzymes that are pertinent for testosterone biosynthesis pathway, with marked inhibition in the production of androgen by the testis following creation of an experimental varicocele in rats at the 17,20-desmolase step.10 Varicocele has been implicated in altered function of 17 alpha-hydroxyprogesterone aldolase, which converts 17-hydroxyprogesterone to testosterone. The increase in the testicular temperature could have a negative effect on the enzyme's action, thus resulting in decreased testosterone production.25 Other studies have confirmed the alteration of the biosynthesis pathway in men with varicocele with evidence of inhibition of testicular C17–20-lyase activity.26
VARICOCELE AND LOW TESTOSTERONE LEVELS
The progressive negative effect of varicocele on Leydig cell function is evidenced by several reports that demonstrate an association between varicocele repair and increase in serum testosterone levels in humans (Table 1). Retrospective review of the effect of varicocelectomy on testosterone levels in infertile men with varicoceles showed a significant increase in serum levels after repair. Men with at least 1 firm testis preoperatively had the greatest increase in serum testosterone postrepair.27 A significant positive correlation between the improvement of the total testosterone levels and the testicular size was noticed in other studies as well.28,29 This suggests that after varicocelectomy, the testicular tissue will improve in function. Therefore, early varicocelectomy is advocated to prevent progressive loss of testicular volume.30
Table 1.
Summary of the reported literature
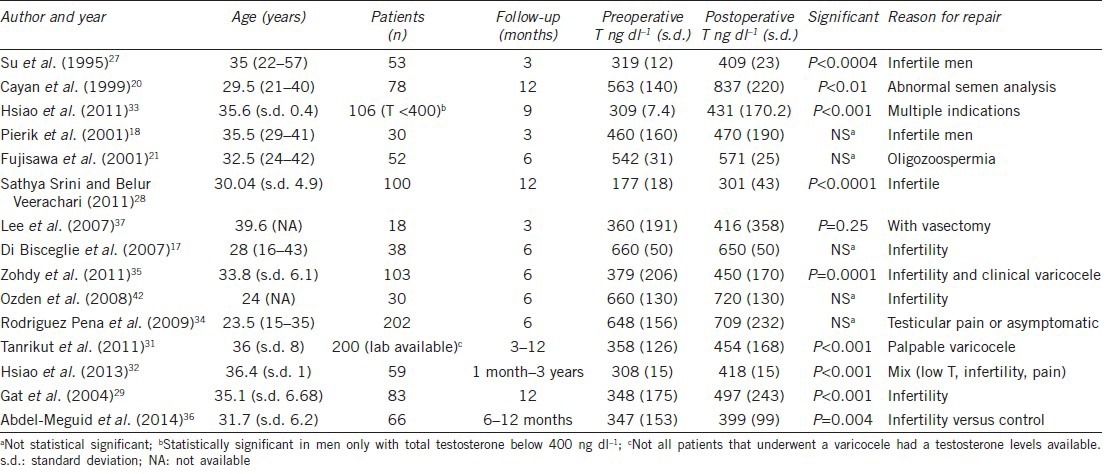
Varicocelectomy leads to improvement in the serum testosterone level in >80% of patients, with a mean increase between 100 and 140 ng dl−1.31,32 Although surgical repair of a greater clinical grade varicocele has been shown to result in greater improvement in semen parameters, clinical grade as well as varicocele vein diameter is not associated with the improvement in serum testosterone level.28,29,32
The prevalence of varicocele increases with age since venous valves become less competent due to changes with aging walls. It is also well-documented that the prevalence of hypogonadism increases with age. In older men who develop a varicocele and hypogonadism, the benefit of varicocelectomy on serum testosterone levels is related to patient age. Men in the fifth and sixth decades of life who underwent varicocelectomy for low serum total testosterone improved as much as younger men. Men with total T <400 had larger changes in serum testosterone levels than in men with more normal testosterone levels.33
Although multiple studies have demonstrated that varicocelectomy improves Leydig cell function and serum testosterone levels, some studies did not find significant increases in testosterone level after surgery.34 Although some studies observed a significant association between testosterone levels, semen analysis profile, and testicular volume, these associations were not always consistently reported.34 After varicocele repair, an increase in serum testosterone was associated with a significant decrease in the mean serum FSH levels, reflecting improved Sertoli and Leydig cell functions.29 In some studies, the varicocele treatment did not show any marked changes in the serum total testosterone levels, but an increase in the serum inhibin B levels was demonstrated, indicating improvement in spermatogenesis and Sertoli cell function.17,18 The preoperative serum inhibin B concentration did not reliably predict a response to varicocelectomy. However, the changes in serum inhibin B concentration after varicocelectomy might be helpful in evaluating improvement in seminiferous tubules function before and after varicocelectomy.21
The magnitude of the increase in the serum testosterone levels after varicocelectomy is usually not the same in all men. Hypogonadal men with total testosterone <300 ng dl−1 seemed to have more significant increase, whereas this trend was not observed in men with total testosterone >300 ng dl−1, despite the considerable improvement in sperm parameters in this subgroup.27,29,31,35,36 These observations suggest that improved spermatogenesis might have a mechanism other than increased testosterone production, such us changes in the inhibin-B and FSH as discussed earlier. Moreover, classification of men based on their preoperative total testosterone may explain variation in the testosterone levels improvement between different studies. Many studies that failed to demonstrate the positive change in the serum testosterone level following varicocelectomy did not characterize patients with low preoperative serum testosterone.
A study compared men with varicocele and infertility who underwent repair to infertile men with varicocele without treatment, men with varicocele but were fertile, and normal men (no varicocele no infertility). At a 6-month follow-up, testosterone levels were improved significantly after varicocele repair compared with no repair. The postvaricocelectomy men demonstrated levels comparable to those of fertile men with varicocele. The latter finding raises a question as to whether improved serum testosterone is related to improved fertility potential. However, the improved postvaricocelectomy testosterone levels did not achieve levels comparable with those of normal fertile men without varicoceles,36 suggesting that some of the testicular damage and decrease in the function might not be reversible and early detection and repair might be important in these patients.
Men with varicocele and hypogonadism should be offered surgical repair, even when future fertility is not an issue, such as men seen for vasectomy.37 A discussion should include all treatment options, including testosterone replacement, anti-estrogens, and aromatase inhibitors. The risks associated with testosterone replacement therapy should be discussed.38 The treatment options should be considered in the framework of the cost and the patient's preference, the need for future testosterone replacement therapy (TRT), and desire for future fertility. Although varicocelectomy might not increase the testosterone levels in certain men, especially in men with total testosterone over 300 ng dl−1, it will preserve testicular function and prevent the decline in testosterone levels. Men with varicocele should also be counseled after surgical repair that they might still require testosterone supplementation to help alleviated symptoms of testosterone deficiency.
VARICOCELE AND ERECTILE FUNCTION
Very few studies have evaluated the association of varicocele and erectile dysfunction (ED). In a study that performed a population-based analysis to evaluate these associations after stratifying by age, the youngest men with ED were found to have the strongest magnitudes of association with varicocele (OR: 5.2, CI: 3.27–8.28; P < 0.001). Increasing age demonstrated a decreasing trend in the magnitude of association when compared with matched controls, except for those aged between 60 and 69 and those over 69 years. Men who underwent a varicocelectomy still shared an association with ED (OR: 1.92, CI: 1.52–2.43), but the magnitude of that association was significantly weaker than it was for untreated varicocele patients (OR: 3.09, CI: 2.67–3.49; P < 0.001).39 Similar studies observed an increase in the International Index of Erectile Function (IIEF-5) score in patients with varicocele and serum testosterone lower than 300 ng dl−1. After varicocelectomy, there was a significant positive correlation between the mean change in total testosterone and the mean change in IIEF-5 (r = 0.629, P < 0.0001).35
Some studies have reported premature ejaculation to be significantly associated with varicocele (29.2% vs 24.9% in subjects with or without varicocele, respectively; P < 0.05).40 In addition, 60%–70% of men with varicocele and infertility reported hypoactive sexual desire,35,40 and this can be attributed to low serum testosterone associated with varicocele. With this association, one also has to keep in mind the negative impact of infertility on sexual desire and sexual function.41 The associations detected in this study between varicocele, varicocelectomy, and sexual function can be explained through overlapping elements of the pathogenesis of varicocele and its subsequent morphologic changes, and the etiologic and prognostic factors of ED. Perhaps the strongest factor contributing to the association between ED and varicocele is the varicocele-generated perturbation of the hypothalamic–pituitary–gonadal axis.
CONCLUSION
Accumulating evidence suggests that varicocele is a risk factor for androgen deficiency. The exact pathophysiology of the negative effects of varicocele on Leydig cell function is not well understood. A review of the literature demonstrates that microsurgical varicocelectomy improves testosterone levels in men with varicocele.
AUTHOR CONTRIBUTIONS
Both AAD and MG performed literature search, prepared manuscript, edited the manuscript, and reviewed and approved the final copy.
COMPETING INTERESTS
None of the authors declared competing financial interests.
REFERENCES
- 1.Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70:532–8. doi: 10.1016/j.urology.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 2.WHO Task Force on the Diagnosis and Treatment of Infertility. The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. World Health Organization. Fertil Steril. 1992;57:1289–93. [PubMed] [Google Scholar]
- 3.Schlegel PN, Goldstein M. Alternate indications for varicocele repair: non-obstructive azoospermia, pain, androgen deficiency and progressive testicular dysfunction. Fertil Steril. 2011;96:1288–93. doi: 10.1016/j.fertnstert.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 4.Wein AJ, Kavoussi LR, Campbell MF, Walsh PC, Goldstein M, et al. 10th ed. Philadelphia, PA: Elsevier Saunders; 2012. Campbell-Walsh Urology; pp. 636–7. [Google Scholar]
- 5.Li F, Yue H, Yamaguchi K, Okada K, Matsushita K, et al. Effect of surgical repair on testosterone production in infertile men with varicocele: a meta-analysis. Int J Urol. 2012;19:149–54. doi: 10.1111/j.1442-2042.2011.02890.x. [DOI] [PubMed] [Google Scholar]
- 6.Wang C, Nieschlag E, Swerdloff RS, Behre H, Hellstrom WJ, et al. ISA, ISSAM, EAU, EAA and ASA recommendations: investigation, treatment and monitoring of late-onset hypogonadism in males. Aging Male. 2009;12:5–12. doi: 10.1080/13685530802389628. [DOI] [PubMed] [Google Scholar]
- 7.Tulloch WS. Varicocele in subfertility; results of treatment. BMJ. 1955;2:356–8. doi: 10.1136/bmj.2.4935.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipshultz LI, Corriere JN., Jr Progressive testicular atrophy in the varicocele patient. J Urol. 1977;117:175–6. doi: 10.1016/s0022-5347(17)58387-1. [DOI] [PubMed] [Google Scholar]
- 9.Johnsen SG, Agger P. Quantitative evaluation of testicular biopsies before and after operation for varicocele. Fertil Steril. 1978;29:58–63. doi: 10.1016/s0015-0282(16)43038-4. [DOI] [PubMed] [Google Scholar]
- 10.Rajfer J, Turner TT, Rivera F, Howards SS, Sikka SC. Inhibition of testicular testosterone biosynthesis following experimental varicocele in rats. Biol Reprod. 1987;36:933–7. doi: 10.1095/biolreprod36.4.933. [DOI] [PubMed] [Google Scholar]
- 11.Zorgniotti AW, Macleod J. Studies in temperature, human semen quality, and varicocele. Fertil Steril. 1973;24:854–63. [PubMed] [Google Scholar]
- 12.Goldstein M, Eid JF. Elevation of intratesticular and scrotal skin surface temperature in men with varicocele. J Urol. 1989;142:743–5. doi: 10.1016/s0022-5347(17)38874-2. [DOI] [PubMed] [Google Scholar]
- 13.Ozbek E, Yurekli M, Soylu A, Davarci M, Balbay MD. The role of adrenomedullin in varicocele and impotence. BJU Int. 2000;86:694–8. doi: 10.1046/j.1464-410x.2000.00853.x. [DOI] [PubMed] [Google Scholar]
- 14.Nallella KP, Allamaneni SS, Pasqualotto FF, Sharma RK, Thomas AJ, et al. Relationship of interleukin-6 with semen characteristics and oxidative stress in patients with varicocele. Urology. 2004;64:1010–3. doi: 10.1016/j.urology.2004.05.045. [DOI] [PubMed] [Google Scholar]
- 15.Romeo C, Ientile R, Santoro G, Impellizzeri P, Turiaco N, et al. Nitric oxide production is increased in the spermatic veins of adolescents with left idiophatic varicocele. J Pediatr Surg. 2001;36:389–93. doi: 10.1053/jpsu.2001.20724. [DOI] [PubMed] [Google Scholar]
- 16.Romeo C, Ientile R, Impellizzeri P, Turiaco N, Teletta M, et al. Preliminary report on nitric oxide-mediated oxidative damage in adolescent varicocele. Hum Reprod. 2003;18:26–9. doi: 10.1093/humrep/deg004. [DOI] [PubMed] [Google Scholar]
- 17.Di Bisceglie C, Bertagna A, Baldi M, Lanfranco F, Tagliabue M, et al. Varicocele sclerotherapy improves serum inhibin B levels and seminal parameters. Int J Androl. 2007;30:531–6. doi: 10.1111/j.1365-2605.2007.00747.x. [DOI] [PubMed] [Google Scholar]
- 18.Pierik FH, Abdesselam SA, Vreeburg JT, Dohle GR, De Jong FH, et al. Increased serum inhibin B levels after varicocele treatment. Clin Endocrinol. 2001;54:775–80. doi: 10.1046/j.1365-2265.2001.01302.x. [DOI] [PubMed] [Google Scholar]
- 19.Hudson RW. The endocrinology of varicoceles. Fertil Steril. 1988;49:199–208. doi: 10.1016/s0015-0282(16)59700-3. [DOI] [PubMed] [Google Scholar]
- 20.Cayan S, Kadioglu A, Orhan I, Kandirali E, Tefekli A, et al. The effect of microsurgical varicocelectomy on serum follicle stimulating hormone, testosterone and free testosterone levels in infertile men with varicocele. BJU Int. 1999;84:1046–9. doi: 10.1046/j.1464-410x.1999.00353.x. [DOI] [PubMed] [Google Scholar]
- 21.Fujisawa M, Dobashi M, Yamasaki T, Kanzaki M, Okada H, et al. Significance of serum inhibin B concentration for evaluating improvement in spermatogenesis after varicocelectomy. Hum Reprod. 2001;16:1945–9. doi: 10.1093/humrep/16.9.1945. [DOI] [PubMed] [Google Scholar]
- 22.Blevrakis E, Chatzidarellis E, Anyfantakis D, Sakellaris G, Raissaki M, et al. Impact of varicocele on biological markers of gonadal function. Hernia. 2015 doi: 10.1007/s10029-015-1361-x. doi: 10.1007/s10029-015-1361-x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Raboch J, Starka L. Hormonal testicular activity in men with a varicocele. Fertil Steril. 1971;22:152–5. doi: 10.1016/s0015-0282(16)34150-4. [DOI] [PubMed] [Google Scholar]
- 24.Sirvent JJ, Bernat R, Navarro MA, Rodriguez Tolra J, Guspi R, et al. Leydig cell in idiopathic varicocele. Eur Urol. 1990;17:257–61. doi: 10.1159/000464051. [DOI] [PubMed] [Google Scholar]
- 25.Ando S, Giacchetto C, Colpi G, Panno ML, Beraldi E, et al. Plasma levels of 17-OH-progesterone and testosterone in patients with varicoceles. Acta Endocrinol. 1983;102:463–9. doi: 10.1530/acta.0.1020463. [DOI] [PubMed] [Google Scholar]
- 26.Takeyama M, Honjoh M, Kodama M, Sakaguchi H, Koh E, et al. Testicular steroids in spermatic and peripheral veins after single injection of hCG in patients with varicocele. Arch Androl. 1990;24:207–13. doi: 10.3109/01485019008986881. [DOI] [PubMed] [Google Scholar]
- 27.Su LM, Goldstein M, Schlegel PN. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. J Urol. 1995;154:1752–5. [PubMed] [Google Scholar]
- 28.Sathya Srini V, Belur Veerachari S. Does varicocelectomy improve gonadal function in men with hypogonadism and infertility?. Analysis of a prospective study. Int J Endocrinol 2011. 2011:916380. doi: 10.1155/2011/916380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gat Y, Gornish M, Belenky A, Bachar GN. Elevation of serum testosterone and free testosterone after embolization of the internal spermatic vein for the treatment of varicocele in infertile men. Hum Reprod. 2004;19:2303–6. doi: 10.1093/humrep/deh443. [DOI] [PubMed] [Google Scholar]
- 30.Diamond DA, Zurakowski D, Bauer SB, Borer JG, Peters CA, et al. Relationship of varicocele grade and testicular hypotrophy to semen parameters in adolescents. J Urol. 2007;178:1584–8. doi: 10.1016/j.juro.2007.03.169. [DOI] [PubMed] [Google Scholar]
- 31.Tanrikut C, Goldstein M, Rosoff JS, Lee RK, Nelson CJ, et al. Varicocele as a risk factor for androgen deficiency and effect of repair. BJU Int. 2011;108:1480–4. doi: 10.1111/j.1464-410X.2010.10030.x. [DOI] [PubMed] [Google Scholar]
- 32.Hsiao W, Rosoff JS, Pale JR, Powell JL, Goldstein M. Varicocelectomy is associated with increases in serum testosterone independent of clinical grade. Urology. 2013;81:1213–7. doi: 10.1016/j.urology.2013.01.060. [DOI] [PubMed] [Google Scholar]
- 33.Hsiao W, Rosoff JS, Pale JR, Greenwood EA, Goldstein M. Older age is associated with similar improvements in semen parameters and testosterone after subinguinal microsurgical varicocelectomy. J Urol. 2011;185:620–5. doi: 10.1016/j.juro.2010.09.114. [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez Pena M, Alescio L, Russell A, Lourenco da Cunha J, Alzu G, et al. Predictors of improved seminal parameters and fertility after varicocele repair in young adults. Andrologia. 2009;41:277–81. doi: 10.1111/j.1439-0272.2009.00919.x. [DOI] [PubMed] [Google Scholar]
- 35.Zohdy W, Ghazi S, Arafa M. Impact of varicocelectomy on gonadal and erectile functions in men with hypogonadism and infertility. J Sex Med. 2011;8:885–93. doi: 10.1111/j.1743-6109.2010.01974.x. [DOI] [PubMed] [Google Scholar]
- 36.Abdel-Meguid TA, Farsi HM, Al-Sayyad A, Tayib A, Mosli HA, et al. Effects of varicocele on serum testosterone and changes of testosterone after varicocelectomy: a prospective controlled study. Urology. 2014;84:1081–7. doi: 10.1016/j.urology.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 37.Lee RK, Li PS, Goldstein M. Simultaneous vasectomy and varicocelectomy: indications and technique. Urology. 2007;70:362–5. doi: 10.1016/j.urology.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 38.Grech A, Breck J, Heidelbaugh J. Adverse effects of testosterone replacement therapy: an update on the evidence and controversy. Ther Adv Drug Saf. 2014;5:190–200. doi: 10.1177/2042098614548680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Keller JJ, Chen YK, Lin HC. Varicocele is associated with erectile dysfunction: a population-based case-control study. J Sex Med. 2012;9:1745–52. doi: 10.1111/j.1743-6109.2012.02736.x. [DOI] [PubMed] [Google Scholar]
- 40.Lotti F, Corona G, Mancini M, Biagini C, Colpi GM, et al. The association between varicocele, premature ejaculation and prostatitis symptoms: possible mechanisms. J Sex Med. 2009;6:2878–87. doi: 10.1111/j.1743-6109.2009.01417.x. [DOI] [PubMed] [Google Scholar]
- 41.Wischmann T. Sexual disorders in infertile couples: an update. Curr Opin Obstet Gynecol. 2013;25:220–2. doi: 10.1097/GCO.0b013e328360e507. [DOI] [PubMed] [Google Scholar]
- 42.Ozden C, Ozdal OL, Bulut S, Guzel O, Koyuncu HH, et al. Effect of varicocelectomy on serum inhibin B levels in infertile patients with varicocele. Scand J Urol Nephrol. 2008;42:441–3. doi: 10.1080/00365590802028141. [DOI] [PubMed] [Google Scholar]


