Abstract
Varicocele-associated male infertility has classically been managed using surgery or assisted reproductive techniques. With increasing evidence of oxidative stress as a pathophysiological factor in varicocele-associated infertility, medical therapy especially antioxidants might become a treatment option with lower risks. We reviewed the existing literature on the role of various medical agents in the management of male infertility attributed to varicoceles. Medical therapy is typically evaluated in three different situations such as (a) comparison of two drugs or one drug with placebo, (b) comparison of drugs versus surgery, and (c) comparison of drugs as adjuvant therapy with surgery versus drug therapy alone. Due to heterogeneity of data and lack of well-conducted studies, there is insufficient data to recommend routine use of medical therapy for men with varicocele-associated infertility and surgery remains the treatment of choice. Pregnancy and live birth rates are usually not reported in most studies and mere improvement in sperm parameters or antioxidant capacity is insufficient to support its routine use. Antioxidant therapy is a potential option due to its theoretical benefit, data from preclinical studies, and lack of major side effects. Adjuvant therapy with antioxidants after surgical repair of varicocele may improve the outcome and is a potential area for further research.
Keywords: antioxidant therapy, drug therapy, male infertility, varicocele
INTRODUCTION
Even though varicoceles are considered a major cause of male infertility, the fact that not all men with varicoceles are infertile and repairing a varicocele does not always result in improved fertility has fueled the varicocele debate.1,2,3,4 The pathophysiology behind varicocele-induced infertility has been extensively studied but definite mechanisms are unclear. Varicocele-induced oxidative stress, hormonal disturbances, scrotal hyperthermia, reflux of renal and adrenal metabolites, and testicular hypo perfusion are among major mechanisms.5
Oxidative stress appears to be the central mediator of testicular damage in varicoceles, and the exact pathophysiology behind varicocele-induced infertility is yet to be elucidated. Heat stress associated with varicocele is known to induce mitochondrial, plasma membrane, cytoplasmic, and peroxisomal reactive oxygen species including nitrous oxide (NO) and hydrogen peroxide (H2O2).1 Testicular ischemia can also occur due to increased venous hydrostatic pressure in varicocele, which leads to increased expression of cytokines such as Interleukin-1 (IL-1), Interleukin-6 (IL-6), and hormones such as leptin. These agents induce generation of reactive oxygen species and impair fertility.1 Infertile men with or without varicoceles have increased seminal reactive oxygen species but such levels are higher in the former, suggesting that varicoceles exacerbate oxidative stress.5 The grade of varicocele has also been correlated directly with the level of oxidative stress.5 Antioxidant therapy that helps negate oxidative stress could thus improve varicocele-associated infertility.
Surgery remains the mainstay of management of varicocele. Varicocelectomy can be performed with open, laparoscopic, or microsurgical techniques. The procedure can also be done with different approaches including retroperitoneal, inguinal, subinguinal, and scrotal. Percutaneous embolisation is another interventional option. However, all such interventions are associated with complications including potential testicular atrophy and, in the absence of identifiable predictors of success, there is an understandable desire to seek less invasive treatments.6 Assisted reproduction offers an alternative to surgery but is associated with risks, costs, and possible need for repetitive interventions. Medical management, including antioxidants, could offer a potential solution with lower risks given the increasing evidence suggesting the role of oxidative stress in varicocele-induced infertility. In this article, we review the existing literature on the role of various medical agents in male infertility attributed to varicoceles.
MATERIALS AND METHODS
Search strategy
Between March and April 2015, PubMed/Medline® database was searched using the key words such as varicocele, male infertility, treatment, drug therapy, antioxidant therapy, and hormonal therapy for articles published after 1985.
Eligibility criteria
Articles involving human studies were included. Articles published in languages other than English were also considered. Data that were solely published in conference or meeting proceedings, websites, or books were not included. Case reports and reviews were gathered to screen their reference lists for additional relevant articles. For articles published in English, full texts were sought while for articles in languages other than English, only the English language abstracts were accessed.
Study selection
Full texts were retrieved through either the journal access from the library or a request to the author. If full-text access was not accessible, the abstracts were reviewed.
Data collection process and data items
An initial screening of the articles suggested that most studies were performed in one of the three settings such as (a) comparison of two drugs or one with a placebo, (b) comparison of drugs versus surgery, and (c) comparison of drugs as adjuvant after surgery versus surgery or drugs alone. This review looks at these studies in these three different settings.
RESULTS
A total of 25 manuscripts describing clinical impact of various medical agents on varicocele-associated infertility were included in the review. Some manuscripts were included under more than one heading as they were used in multiple settings in the same report. Full texts were retrieved for 14 manuscripts and only abstracts could be retrieved for the remaining 11 studies.
Drugs as sole therapy
Hormonal agents
Varicoceles have been shown to be associated with low testosterone.7 It, therefore, seems logical that therapies that manipulate the hormonal milieu may result in improvement in semen parameters. However, there are little data on androgenic hormones in varicocele-associated infertility (Table 1). In 1999, Radicioni and Schwarzenberg8 treated 20 adolescents and young adults with idiopathic, unilateral left varicocele with purified urinary FSH 75 IU thrice weekly for 3 months and reported a significant improvement in sperm density per ml (from 38 × 106 to 49 × 106), total sperm number per ejaculate with forward motility (37 × 106 to 48 × 106), and a decrease of atypical forms (53% to 49%). They considered nine patients as responders based on increase of total number of sperm per ejaculate >50% after FSH treatment. This is a nonrandomized, uncontrolled study which has only studied seminal parameters after treatment and did not study pregnancy rates. The small sample size and inadequate definition of responders are other limitations of this study.
Table 1.
Studies comparing medical agents as sole therapy in management of varicocele-associated infertility
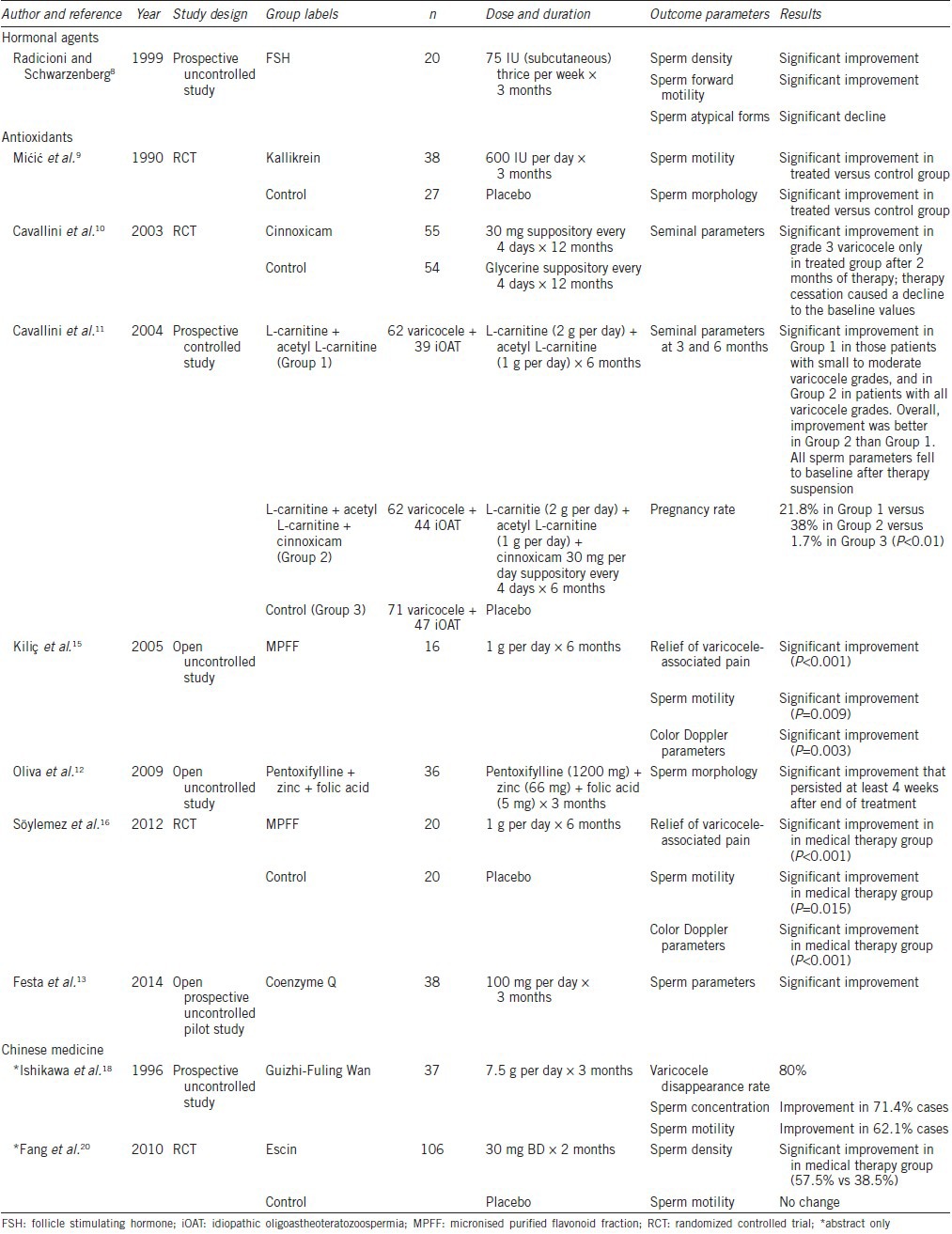
Antioxidants
A multitude of antoxidants has been used in management of varicocele-associated infertility (Table 1). Kallikrein, which is thought to improve intratesticular testosterone and improve sperm maturation, was found to have positive impact on sperm parameters in patients with male infertility and varicocele. Mićić et al., in a randomized controlled study of 65 infertile men with oligoasthenozoospermia and left-sided varicocele, treated 38 men with kallikrein 600 units orally per day for 3 months and the rest with placebo. They reported significant improvements in sperm motility (24% to 35%) and sperm morphology (58% to 71%).9 Cinnoxicam, an anti-inflammatory agent, was observed to significantly improve the seminal parameters in grade 3 varicocele, but cessation of therapy led to decline to baseline values.10 Cavallini et al.,11 in a randomized prospective controlled study of 325 patients suffering from clinical or subclinical varicocele or idiopathic male infertility, compared the effects of combination therapy of carnitine (2 g per day) + L-acetyl carnitine (1 g per day) + cinnoxicam (30 mg suppository every 4 days) with carnitine (2 g per day) +L-acetyl carnitine (1 g per day) for a duration of 6 months. The patients on control arm received starch tablets (500 mg per day) and glycerine suppository every 4 days. There was no improvement in sperm parameters in the control group. The group which received only L-carnitine with L-acetyl carnitine showed significant improvements in sperm concentration, morphology, and total count 3 and 6 months after initiation of the therapy regardless of varicocele grade. The group which received carnitine and cinnoxicam therapy had significant improvements (P < 0.05) in sperm parameters associated with small to moderate varicocele grades but not severe varicocele grade. A significant increase in pregnancy rate with combination therapy (38% vs 21%, P < 0.05) was also observed. However, the seminal parameters returned to baseline after suspension of therapy. They did not report live birth rate and miscarriage/abortion rate. Unfortunately, the study groups were extremely heterogenous including subjects with idiopathic infertility, subclinical varicoceles, and clinical varicoceles. In one group, improvement occurred in patients with subclinical varicocele and not with clinical varicocele.
Oliva et al.12 studied the role of combination therapy of pentoxifylline (1200 mg per day) + zinc (66 mg per day) + folic acid (5 mg per day) administered to 36 men with clinical varicocele-associated infertility and, at least, one abnormal semen parameter for 3 months. The authors found a significant improvement (P < 0.05) in the proportion of morphologically normal sperm that persisted at least for 4 weeks after discontinuation of therapy. This was an open-labeled, uncontrolled study and did not report pregnancy data, thus limiting the value of the results.
Coenzyme Q10 is another antioxidant which has been found to play a role in the management of male infertility. Increased oxidative stress decreases the availability of this coenzyme in oxidative phosphorylation. Hence, exogenous supplementation might increase its content in semen and improve sperm characteristics. Festa et al.13 in an open-labeled, uncontrolled pilot study evaluated the antioxidant capacity of seminal plasma before and after supplementation of coenzyme Q10 100 mg per day for 12 weeks in patients with male infertility associated with low-grade varicocele. They found significant increase in total antioxidant capacity (P < 0.01), significant improvements in sperm density (P = 0.03) and forward sperm motility (P = 0.03). However, they did not measure the persistence of these changes after discontinuation of therapy and did not report any pregnancy owing to the short period of the study.
Bioflavonoid, a plant pigment responsible for coloring of flowers, is another class of antioxidants shown to be effective in varicocele with altered sperm parameters. These agents possibly prolong the activity of peripheral norepinephrine, increase the mechanical tension and calcium sensitivity of contractile apparatus, thus improving venous tone in varicoceles.14 Zampieri et al.14 studied 168 adolescent boys with a subclinical left-sided varicoceles in a longitudinal observational study and demonstrated significantly slower rate of progression of subclinical varicocele to palpable varicocele (11% vs 31%, P = 0.002). The authors also reported higher resolution rate (41% vs 31%, P < 0.05) with cyclical therapy of semisynthetic derivative of bioflavanoid (O-β-hydroxyethyl rutoside) at 1000 mg per day thrice monthly for 1 year. However, the drug had no protective effects against testicular growth arrest.
Another derivative of bioflavanoid in the form of micronized purified flavonoid fraction (MPFF, commonly available as Daflon) was also evaluated to study its effect on pain score, spermiogram, and color Doppler parameters in patients with clinical painful varicocele after treatment for 6 months.15 It was found that medical therapy resulted in significant relief of varicocele-associated pain (P < 0.001), improvement in color Doppler parameters (i.e., decrease in the reflux time of left spermatic vein during Valsalva maneuver; P = 0.003), and improvement in sperm motility (P = 0.009). It did not lead to any improvement in total sperm count, sperm concentration, morphology, and semen volume. Later, the same group16 conducted a placebo-controlled randomized controlled trial to study the effects of MPFF at dose of 1000 mg per day for 6 months in 40 patients with clinical varicocele and sperm concentration >20 million ml−1. They reported significant improvement in pain (P < 0.001), color Doppler parameters (P < 0.001), and sperm motility (P = 0.015) at the end of the treatment. None of these aforementioned studies have looked at varicocele-associated infertility, and their end-points have focused on pain and Doppler parameters.
Chinese medicine
A myriad of Chinese medicines with antioxidant and anti-inflammatory activity have been studied as possible therapeutic agents for management of varicocele and male infertility. Qianjing is a herbal medicine observed to improve epididymal microenvironment and seminal parameters by increasing glutathione peroxidase and decreasing malondialdehyde in seminal plasma in rats.17 Another anti-inflammatory agent and antioxidant, Guizhi Fuling Wan, was shown to improve sperm concentration and sperm motility in patients suffering from varicocele and male infertility.18 Another extensively used Chinese agent, Escin, derived from seed extract of Aesculus hippocastanum, is an anti-inflammatory and anti-edema agent that enhances glucocorticoid and Prostaglandin F-2α (PGF-2α) activity and decreases Nuclear Factor-kappa β (NF-κβ) expression.19 Fang et al.20 compared 106 patients with clinical or subclinical varicocele-associated infertility who received escin 60 mg d-1 for two months with controls. All the patients received composite medicines favorable for sperm quality. They found significant improvements in sperm density (57.5% vs 38.5%, P < 0.05) and sperm motility (55.7% vs 46.2%, P < 0.05). They also reported better improvements in these sperm parameters in patients with moderate grade of varicocele as compared to severe grade.
Drugs versus surgery
Hormonal agents
Antiestrogens and gonadotropins enhance spermatogenesis stimulation and have been compared to varicocelectomy (Table 2). Unal et al.21 randomized 42 infertile men with left subclinical varicocele to either clomiphene citrate 50 mg per day for 6 months or surgical management. Surgical management involved open ligation of spermatic vein (subinguinal varicocelectomy). They reported that varicocelectomy led to significant improvements in terms of sperm density and motility (P < 0.05), but there was no significant difference between medical or surgical management in terms of sperm density (P = 0.66), sperm morphology (P = 0.37), and sperm motility (P = 0.31) 6 months after surgery or initiation of medical therapy. Pregnancy was recorded in two cases of the surgical group while only one case in medical group (12.5% vs 6.7%, P = 0.58). They concluded no statistical difference in overall outcome in medical or surgical management of varicocele-associated infertility. De Rose et al.22 compared gonadotropins in the form of menotropin (hMG, human menopausal gonadotropin) versus varicocelectomy in a small trial to assess spermatogenesis stimulation. Twenty patients received menotropin for 3 months while 20 patients underwent subinguinal varicocelectomy. There was a significant improvement in sperm characteristics in the medical therapy group after 12 months follow-up. In term of pregnancy rate, 47% cases in medical therapy group reported pregnancy compared with 27.7% in the surgical group in a follow-up of 12 months (P < 0.05).
Table 2.
Studies comparing roles of medical agents versus surgery in management of varicocele-associated infertility
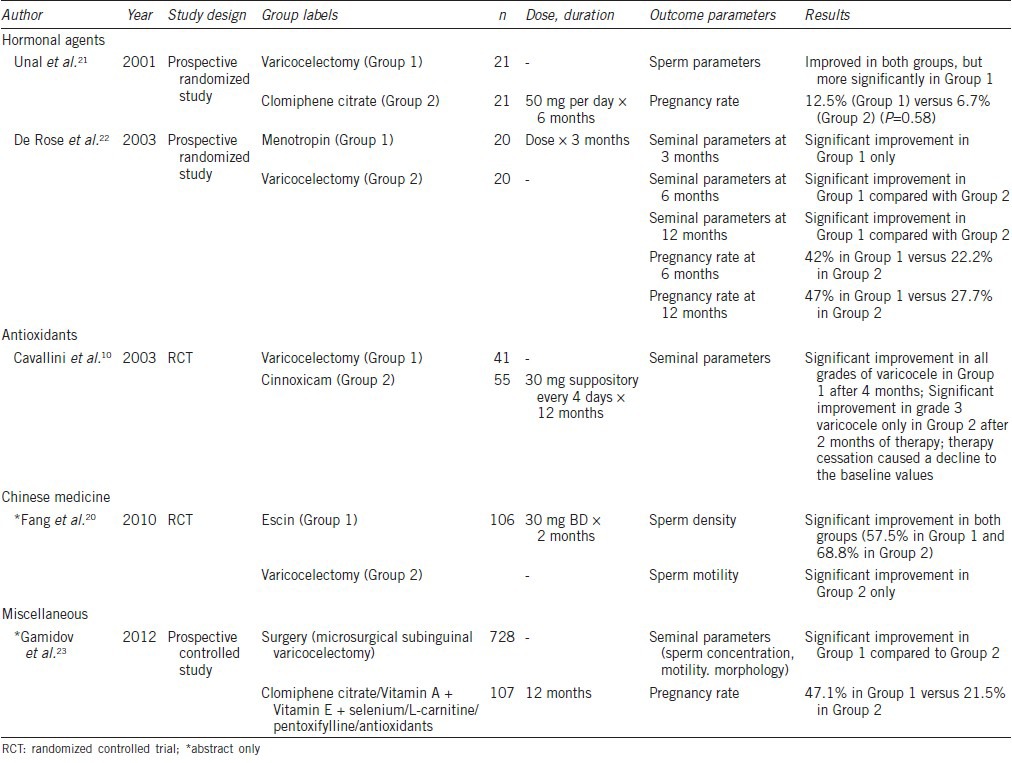
Antioxidants
Cinnoxicam, an anti-inflammatory agent, inhibits reactive oxygen species and prostaglandin synthesis which are often raised in varicocele. Cavallini et al.10 compared 41 patients with clinical or subclinical varicocele-associated infertility receiving cinnoxicam treatment at a dose of 30 mg suppository every 4 days for 12 months with 61 similar patients undergoing microsurgical subinguinal venous ligation. Surgery significantly improved sperm values in men with moderate to severe varicocele within 4 months. Cinnoxicam significantly improved sperm quality in patients with moderate varicocele only. The improvement in medical group declined to baseline after cessation of therapy. They did not report pregnancy rate in either group.
In another study including a large cohort of infertile men with varicocele, Gamidov et al.23 treated 728 patients with bilateral microsurgical subinguinal varicocelectomy and 107 with antioxidant combinations (clomiphene citrate, Vitamins A and E, selenium, L-carnitine, pentoxifylline, and antioxidants) for 3–6 months and 56 patients served as untreated controls. Within a follow-up of 3–12 months, they reported an increase in sperm concentration after both surgery and drug therapy (70% patients vs 30% patients). Natural pregnancy was recorded in 47% of the patients in the surgery group and 21% in the medical therapy compared with 3.6% in the untreated group.
Chinese medicine
In a three-armed randomized controlled study of 219 subjects, Escin in a dose of 60 mg per day for 2 months was compared with surgery and controls who received no treatment. There was an improvement in sperm density in all the three groups: 69% of the cases undergoing surgery, 57% of those receiving medical therapy, and 38% of the controls. Similarly, motility improvements were 77% for surgery, 55% for drug, and 46% for controls. Surgery was superior to control and drug treatments in both parameters.20
Adjuvant drug therapy
Medical therapy as adjuvant to surgical management of varicocele is often used to maximize benefits of both modalities. Multiple studies have compared adjuvant therapy after surgery with medical therapy or surgery alone. Table 3 lists studies comparing adjuvant medical therapy with medical therapy alone.
Table 3.
Studies comparing adjuvant medical therapy versus medical therapy alone in management of varicocele-associated infertility
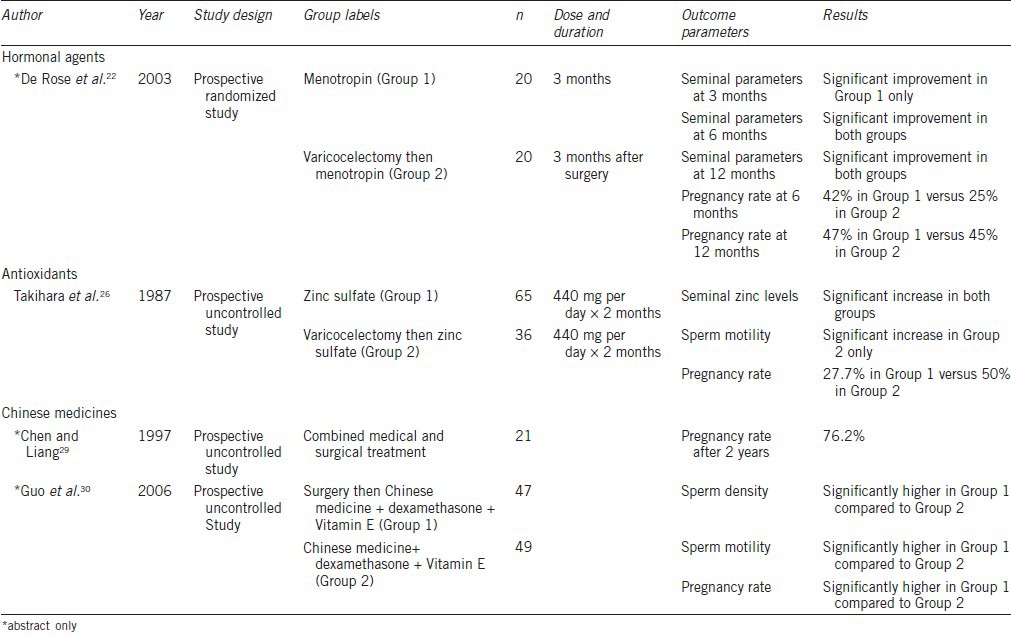
Hormonal agents
Gonadotropins and antiestrogens have been used as adjuvant therapy after varicocelectomy. In a controlled trial of 60 men divided into three arms, Menotropin use after surgery was found to be superior to either Menotropin or subinguinal varicocelectomy alone.22 Combined therapy not only significantly improved sperm concentration, motility, and morphology 6 months and 12 months after surgery (P < 0.05) but also led to significantly higher pregnancy rate (45% with combination therapy vs 42% with medical therapy and 27.7% with varicocelectomy alone; P < 0.05). Kadioglu et al.24 studied the role of tamoxifen 20 mg per day for 6 months as adjuvant therapy for spermatogenesis stimulation after varicocelectomy in 84 infertile patients with clinical varicoceles. The authors showed significant increase in sperm concentration from 13.5 to 18 million ml−1 in normogonadotropic patients.
Antioxidants
Antioxidants are commonly used as adjuvant therapy after surgical management of varicocele. Paradiso Galatioto et al.25 conducted a randomized controlled trial involving 42 patients who had undergone retrograde embolisation for clinical varicocele and persisted with oligozoospermia 6 months after surgery. Twenty patients were allocated in the treatment arm receiving antioxidant therapy (including N-acetyl cysteine 600 mg per day with vitamins and minerals) for 3 months while 22 patients were included in the control arm receiving placebo. At the end of 3 months, the sperm count in the treatment arm significantly improved from 14 to 32 million ml−1 (P = 0.009) while no significant improvement occurred in the control arm. No statistical difference in progressive motility (P = 0.752) and typical forms (P = 0.926) were found. Further analysis suggested a 20 times higher chance of improving sperm counts after antioxidant therapy compared to controls. However, this improvement did not translate into a higher pregnancy rate when the patients were followed up for 12 months after cessation of therapy.
Zinc and folic acid are also used as adjuvant therapies.26,27,28 Takihara et al.26 treated 65 infertile men with or without varicocele with zinc therapy (440 mg daily) and 36 infertile men postsubinguinal varicocelectomy with similar zinc adjuvant therapy for a variable period of 2 months to 2 years. The postvaricocelectomy group showed significant improvement in sperm motility (P < 0.05) at 2 months and 12 months of therapy. Twenty-eight percentage of men who received only zinc therapy impregnated their wives compared with 50% of the postvaricocelectomy group. Zinc was thus concluded to play some role in improvement in seminal parameters postvaricocelectomy. Azizollahi et al.27 randomized 102 infertile patients after varicocelectomy used to repair clinical grade 3 varicocele into four groups such as 32 receiving zinc sulfate 66 mg per day alone, 26 receiving folic acid (5 mg per day) alone, 29 receiving combination therapy, and 25 receiving placebo for 6 months starting immediately after surgery. There was mild improvement in control arm. Patients receiving zinc sulfate therapy showed significant improvement in only sperm morphology (percentage of normal sperms increased from 40% to 53%, P < 0.05) while those receiving folic acid showed significant improvement only in sperm concentration (27 million ml−1 to 49 million ml−1, P < 0.05). Patients receiving combination therapy showed significantly improved sperm concentration (30 million ml−1 to 47 million ml−1, P < 0.05), morphology (percentage normal sperm increased from 46% to 57%, P < 0.05), and motility (percentage of sperm with forward progressive motility increased from 28.7% to 43.0%, P < 0.05) at the end of 6-month treatment. Further analysis on hormonal parameters and seminal plasma biomarkers showed significant increase in blood Inhibin B levels (from 127.9 to 190.1 pg ml−1, P < 0.05) after combination therapy. Seminal superoxide dismutase (SOD) activity showed significant improvement in groups receiving zinc therapy alone (63.3% to 71.4%, P < 0.05) and combination therapy (58.8% to 68.4%, P < 0.05) for 6 months. No significant change in nitrous oxide concentration and total antioxidant capacity of seminal plasma was noted. In conclusion, zinc and folic acid combination therapy does seem to have a positive impact on seminal parameters after surgery, but its clinical implication in terms of pregnancy outcome is still unclear.
Chinese medicine
In 1997, Chen and Liang29 reported the combined role of surgery followed by Chinese medicine in the management of male infertility with varicocele. The authors recorded pregnancy rates as high as 72%. Guo et al.30 compared surgery followed by Chinese medicine with dexamethasone and Vitamin E combined found significantly higher sperm parameters and pregnancy rates with surgery and drug combination than medical therapy alone. Yan et al.31 studied Jingling oral liquid in a randomized controlled study as an adjuvant therapy after varicocelectomy and compared it with hCG in 60 patients. They reported a significant improvement in seminal parameters, seminal superoxide dismutase and zinc levels and higher pregnancy rate in the Chinese medicine group compared with hCG group.
Miscellaneous
Ketotifen, a tricyclic benzocycloheptatiophene, a mast cell stabilizer, is thought to counteract the ability of mast cells to trigger inflammatory response, thereby improving sperm quality. Azadi et al.32 randomized 103 patients with clinical varicocele and infertility subjected to varicocelectomy to two groups such as 51 patients received ketotifen 2 mg per day for 3 months and 52 patients received no drug. Assessment of seminal parameters 3 months after surgery revealed marked improvement in seminal parameters in both groups, the treatment group (P < 0.01) and control group (P < 0.05). On comparing the seminal parameters between the two groups, there was no significant difference in sperm density (P = 0.95), sperm morphology (P = 0.1) before surgery. Three months after surgery, the treatment group which received adjuvant ketotifen showed marked improvement in sperm density (P = 0.004) and sperm morphology (P = 0.001) compared to control group. The impact on sperm motility was not significant. On follow-up of these groups for 9 months, pregnancy rate was significantly higher in the group which received adjuvant ketotifen (41% vs 21%, P < 0.05).
DISCUSSION
Similar to the problem with empirical drug therapy for idiopathic male infertility, empirical drug therapy for varicocele-associated infertility suffers from a lack of well-conducted studies that could offer high levels of evidence.33 The problem stems from an unclear target of therapy, poorly designed studies, small numbers, varying drug combinations, and inadequate outcome measures. In the absence of live birth data, surrogates such as change in oxidative stress levels, sperm parameter improvements, and even pregnancy rates are insufficient evidence to support prescriptions. Some of the studies reviewed in this article have shown sperm parameter improvement rates with placebo to be as high as 38%–46%.20 In view of such data, unless large prospective trials are conducted, most such therapies will remain empirical.
A number of studies reviewed in this manuscript provide a “proof of concept” or rationale for medical therapy to men with varicocele but fall short of providing true evidence. This is particularly true for antioxidants which are associated with a lack of harm and, therefore, seem to be the best candidates for both research and clinical use.
Since there is high-level evidence to suggest that in the appropriate patient, varicocelectomy results in improvement of outcomes,34 treating infertile men with a varicocele with drugs alone cannot be recommended. However, success after surgical intervention for varicocelectomy is not universal. Many such men will have persistent oligoasthenoteratozoospermia and will fall into the category of idiopathic seminal abnormalities since the identifiable surgical cause, namely the varicocele, has already been corrected. They are thus candidates for empirical treatment similar to their counterparts who never had a surgically correctable cause. Antioxidants are the most commonly prescribed drugs in this patient population both due to theoretical benefits, preclinical studies, and lack of significant harm.35 This may be a group where empirical drug therapy, primarily with antioxidants, plays a role.
CONCLUSIONS
Current evidence cannot support recommendation of medical therapy alone to infertile males with abnormal seminal parameters and clinically palpable varicocele. Surgery remains the treatment of choice. Since surgery for varicoceles does not always result in success, adjuvant therapy after surgery may be an acceptable option. Adjuvant therapy with antioxidants may provide additional benefit. Research using valid end-points such as pregnancy is required before these therapies can become a standard treatment option.
AUTHOR CONTRIBUTIONS
HG is responsible for data acquisition, manuscript first draft, manuscript critical revision, and approval of final draft; RK is responsible concept design, data acquisition, manuscript critical revision, approval of final draft, and overall supervision.
COMPETING INTEREST
The authors declared no competing interests.
REFERENCES
- 1.Agarwal A, Hamada A, Esteves SC. Insight into oxidative stress in varicocele associated male infertility: part 1. Nat Rev Urol. 2012;9:678–902. doi: 10.1038/nrurol.2012.197. [DOI] [PubMed] [Google Scholar]
- 2.Madgar I, Weissenberg R, Lunenfeld B, Karasik A, Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril. 1995;63:120–4. doi: 10.1016/s0015-0282(16)57306-3. [DOI] [PubMed] [Google Scholar]
- 3.Witt MA, Lipshultz LI. Varicocele: a progressive or static lesion? Urology. 1993;42:541–3. doi: 10.1016/0090-4295(93)90268-f. [DOI] [PubMed] [Google Scholar]
- 4.Sylora JA, Pryor JL. Varicocele. Curr Ther Endocrinol Metab. 1994;5:309–14. [PubMed] [Google Scholar]
- 5.Hamada A, Esteves SC, Agarwal A. Insight into oxidative stress in varicocele associated male infertility: part 2. Nat Rev Urol. 2013;10:26–37. doi: 10.1038/nrurol.2012.198. [DOI] [PubMed] [Google Scholar]
- 6.Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, et al. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011;108:1157–72. doi: 10.1111/j.1464-410X.2010.09959.x. [DOI] [PubMed] [Google Scholar]
- 7.Fisch H, Hyun G. Varicocele repair for low testosterone. Curr Opin Urol. 2012;22:495–8. doi: 10.1097/MOU.0b013e328358e0fb. [DOI] [PubMed] [Google Scholar]
- 8.Radicioni A, Schwarzenberg TL. The use of FSH in adolescents and young adults with idiopathic, unilateral, left varicocele not undergoing surgical intervention. Preliminary study. Minerva Endocrinol. 1999;24:63–8. [PubMed] [Google Scholar]
- 9.Miæiæ S, Tuliæ C, Dotliæ R. Kallikrein therapy of infertile men with varicocele and impaired sperm motility. Andrologia. 1990;22:179–83. doi: 10.1111/j.1439-0272.1990.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 10.Cavallini G, Biagiotti G, Ferraretti AP, Gianaroli L, Vitali G. Medical therapy of oligoasthenospermia associated with left varicocele. BJU Int. 2003;91:513–8. doi: 10.1046/j.1464-410x.2003.04136.x. [DOI] [PubMed] [Google Scholar]
- 11.Cavallini G, Ferraretti AP, Gianaroli L, Biagiotti G, Vitali G. Cinnoxicam and L-carnitine/acetyl carnitine treatment for idiopathic and varicocele associated oligoasthenospermia. J Androl. 2004;25:761–70. doi: 10.1002/j.1939-4640.2004.tb02853.x. [DOI] [PubMed] [Google Scholar]
- 12.Oliva A, Dotta A, Multigner L. Pentoxifylline and antioxidants improve sperm quality in male patients with varicocele. Fertil Steril. 2009;91:1536–9. doi: 10.1016/j.fertnstert.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 13.Festa R, Giacchi E, Raimondo S, Tiano L, Zuccarelli P, et al. Coenzyme Q10 supplementation in infertile men with low-grade varicocele: an open, uncontrolled pilot study. Andrologia. 2014;46:805–7. doi: 10.1111/and.12152. [DOI] [PubMed] [Google Scholar]
- 14.Zampieri N, Pellegrino M, Ottolenghi A, Camoglio FS. Effects of bioflavonoids in the management of subclinical varicocele. Pediatr Surg Int. 2010;26:505–8. doi: 10.1007/s00383-010-2574-9. [DOI] [PubMed] [Google Scholar]
- 15.Kiliç S, Güneº A, Ipek D, Dusak A, Güneº G, et al. Effects of micronised purified flavonoid fraction on pain, spermiogram and scrotal color Doppler parameters in patients with painful varicocele. Urol Int. 2005;74:173–9. doi: 10.1159/000083290. [DOI] [PubMed] [Google Scholar]
- 16.Söylemez H, Kiliç S, Atar M, Penbegül N, Sancaktutar AA, et al. Effects of micronised purified flavonoid fraction on pain, semen analysis and scrotal color Doppler parameters in patients with painful varicocele; results of a randomized placebo controlled study. Int Urol Nephrol. 2012;44:401–8. doi: 10.1007/s11255-011-0038-3. [DOI] [PubMed] [Google Scholar]
- 17.Qu XW, Shan ZJ, Han QH, Hu JT, Zhang PH, et al. Effects of Qiangjing Capsule on the oxidative and antioxidative system in the epididymis of varicocele in rats. Zhonghua Nan Ke Xue. 2011;17:1039–42. [PubMed] [Google Scholar]
- 18.Ishikawa H, Ohashi M, Hayakawa K, Kaneko S, Hata M. Effects of Guizhi-Fuling-Wan on male infertility with varicocele. Am J Chin Med. 1996;24:327–31. doi: 10.1142/S0192415X96000396. [DOI] [PubMed] [Google Scholar]
- 19.Wang H, Zhang L, Jiang N, Wang Z, Chong Y, et al. Anti-inflammatory effects of escin are correlated with the glucocorticoid receptor/NF-κB signaling pathway, but not the COX/PGF2α signaling pathway. Exp Ther Med. 2013;6:419–22. doi: 10.3892/etm.2013.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fang Y, Zhao L, Yan F, Xia X, Xu D, et al. Escin improves sperm quality in male patients with varicocele associated infertility. Phytomedicine. 2010;17:192–6. doi: 10.1016/j.phymed.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Unal D, Yeni E, Verit A, Karatas OF. Clomiphene citrate versus varicocelectomy in treatment of subclinical varicocele: a prospective randomized study. Int J Urol. 2001;8:227–30. doi: 10.1046/j.1442-2042.2001.00289.x. [DOI] [PubMed] [Google Scholar]
- 22.De Rose AF, Gallo F, Giglio M, Parisini B, Carmignani G. Early use of menotropin in the treatment of varicocele. Arch Ital Urol Androl. 2003;75:53–7. [PubMed] [Google Scholar]
- 23.Gamidov CI, Ovchinnikov RI, Popova AIu, Tkhagapsoeva RA, Izhbaev SKh. Current approach to therapy for male infertility in patients with varicocele. Ter Arkh. 2012;84:56–61. [PubMed] [Google Scholar]
- 24.Kadioglu TC, Köksal IT, Tunç M, Nane I, Tellaloglu S. Treatment of idiopathic and post varicocelectomy oligozoospermia with oral tamoxifen citrate. BJU Int. 1999;83:646–8. doi: 10.1046/j.1464-410x.1999.00976.x. [DOI] [PubMed] [Google Scholar]
- 25.Paradiso Galatioto G, Gravina GL, Angelozzi G, Sacchetti A, Innominato PF, et al. May antioxidant therapy improve sperm parameters of men with persistent oligospermia after retrograde embolization for varicocele? World J Urol. 2008;26:97–102. doi: 10.1007/s00345-007-0218-z. [DOI] [PubMed] [Google Scholar]
- 26.Takihara H, Cosentino MJ, Cockett AT. Zinc sulfate therapy for infertile male with or without varicocelectomy. Urology. 1987;29:638–41. doi: 10.1016/0090-4295(87)90111-7. [DOI] [PubMed] [Google Scholar]
- 27.Azizollahi G, Azizollahi S, Babaei H, Kianinejad M, Baneshi MR, et al. Effects of supplement therapy on sperm parameters, protamine content and acrosomal integrity of varicocelectomized subjects. J Assist Reprod Genet. 2013;30:593–9. doi: 10.1007/s10815-013-9961-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baneshi MR, Safari Z, Azizollahi S. Effect of folic acid and zinc sulphate on endocrine parameters and seminal antioxidant level after varicocelectomy. Andrologia. 2014;46:240–5. doi: 10.1111/and.12067. [DOI] [PubMed] [Google Scholar]
- 29.Chen C, Liang P. Pathogenesis and combined treatment of sterility in men with varicocele. Zhonghua Wai Ke Za Zhi. 1997;35:168–9. [PubMed] [Google Scholar]
- 30.Guo YJ, Wang ZJ, Cao M, Kang GJ. An integrated method works well on varicocele. Zhonghua Nan Ke Xue. 2006;12:800–2. [PubMed] [Google Scholar]
- 31.Yan LF, Jiang MF, Shao RY. Clinical observation on effect of Jingling oral liquid in treating infertile patients with varicocele after varicocelectomy. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2004;24:220–2. [PubMed] [Google Scholar]
- 32.Azadi L, Abbasi H, Deemeh MR, Tavalaee M, Arbabian M, et al. Zaditen (Ketotifen), as mast cell blocker, improves sperm quality, chromatin integrity and pregnancy rate after varicocelectomy. Int J Androl. 2011;34:446–52. doi: 10.1111/j.1365-2605.2010.01112.x. [DOI] [PubMed] [Google Scholar]
- 33.Kumar R, Gautam G, Gupta NP. Drug therapy for idiopathic male infertility: rationale versus evidence. J Urol. 2006;176:1307–12. doi: 10.1016/j.juro.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 34.Practice Committee of the American Society for Reproductive Medicine; Society for Male Reproduction and Urology. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2014;102:1556–60. doi: 10.1016/j.fertnstert.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Garg H, Kumar R. Empirical drug therapy for idiopathic male infertility: what is the new evidence? Urology. 2015;86:1065–75. doi: 10.1016/j.urology.2015.07.030. [DOI] [PubMed] [Google Scholar]


